Abstract
The unique neuroanatomical underpinnings of internalizing symptoms and impulsivity during childhood are not well understood. In this study, we examined associations of brain structure with anxiety, depression, and impulsivity in children and adolescents. Participants were 7- to 21-year-olds (N = 328) from the Pediatric Imaging, Neurocognition, and Genetics (PING) study who completed high-resolution, 3-Tesla, T1-weighted MRI and self-report measures of anxiety, depression, and/or impulsivity. Cortical thickness and surface area were examined across cortical regions-of-interest (ROIs), and exploratory whole-brain analyses were also conducted. Gray matter volume (GMV) was examined in subcortical ROIs. When considered separately, higher depressive symptoms and impulsivity were each significantly associated with reduced cortical thickness in ventromedial PFC/medial OFC, but when considered simultaneously, only depressive symptoms remained significant. Higher impulsivity, but not depressive symptoms, was associated with reduced cortical thickness in the frontal pole, rostral middle frontal gyrus, and pars orbitalis. No differences were found for regional surface area. Higher depressive symptoms, but not impulsivity, were significantly associated with smaller hippocampal GMV and larger pallidal GMV. There were no significant associations between anxiety symptoms and brain structure. Depressive symptoms and impulsivity may be linked with cortical thinning in overlapping and distinct regions during childhood and adolescence.
Keywords: Anxiety, Depression, Impulsivity, Cortical thickness, Subcortical volume
Highlights
-
•
Internalizing problems and impulsivity may have shared and distinct neuroanatomical substrates in childhood.
-
•
Higher depressive symptoms were uniquely associated with reduced cortical thickness in vmPFC/medial OFC.
-
•
Higher impulsivity was uniquely associated with reduced cortical thickness in lateral PFC regions.
-
•
Higher depressive symptoms were associated with smaller hippocampal volume and larger pallidal volume.
-
•
These shared and distinct neuroanatomical correlates may inform the design of prevention and intervention strategies.
1. Introduction
Although numerous studies have examined the neuroanatomical correlates of specific psychiatric disorders, fewer have compared brain morphometry across multiple types of psychopathology (Gold et al., 2016). Given that comorbidity among psychiatric disorders is common, there is a particular need for research comparing brain structure across disorders to identify unique and shared neurobiology. The NIMH Research Domain Criteria (RDoC) framework suggests that such investigations use a dimensional approach, which includes focusing on levels of psychopathology and symptoms found across multiple psychiatric disorders (Insel et al., 2010).
High levels of internalizing symptoms and impulsivity may have both shared and distinct neural substrates. Internalizing problems have core features of anxiety and/or depression, which often co-occur and have shared genetic risk factors (Cummings et al., 2014). In contrast, impulsivity refers to the tendency to react quickly without considering the broader consequences of one's actions. On the one hand, their neural mechanisms may differ given that impulsivity has primarily been associated with externalizing rather than internalizing disorders (Beauchaine et al., 2017; Holmes et al., 2016; Mackey et al., 2017). On the other hand, shared neurobiology is suggested by the prevalence of heterotypic comorbidity, which refers to cases of co-occurring internalizing and externalizing disorders (Zisner and Beauchaine, 2016). For example, up to half of children diagnosed with ADHD experience a comorbid mood disorder (Zisner and Beauchaine, 2016). In addition, a core feature across high levels of both internalizing symptoms and impulsivity is reduced top-down control over emotions and reward-related behavior, suggesting that differences in overlapping regions in the prefrontal cortex (PFC) may underlie both domains. Understanding which neural structures are associated with which symptom dimensions can help identify neural mechanisms that may be similar and distinct across multiple psychiatric disorders.
In general, most neuroimaging studies that have examined these questions have focused on adults and compared patient populations diagnosed with one or more psychiatric disorders to controls. Relatively fewer studies have investigated these associations during childhood, when neural mechanisms may differ from those in adulthood. Furthermore, it is crucial that we understand the neural correlates of continuous variability in these symptoms within or closer to the normal range. As such, in the current study, we examined differences in neural structure associated with continuous variability in anxiety symptoms, depressive symptoms, and impulsivity in children and adolescents. Given that anxiety and depression differ in important ways (D'Avanzato et al., 2013), they were examined separately to account for differences in the similarity of their underlying neuroanatomy to that of impulsivity.
1.1. Structural neuroimaging of anxiety symptoms
Previous studies of pediatric anxiety problems have indicated structural differences in PFC regions, including ventromedial PFC (vmPFC) and anterior cingulate cortex (ACC) (see Supplementary Table S1). Although many structural MRI studies of psychiatric disorders have focused on cortical volume, this measure represents a composite of cortical thickness (CT) and surface area (SA), which are genetically, developmentally, and phenotypically independent (Raznahan et al., 2011; Winkler et al., 2010). These findings have given rise to studies of surface-based morphometry, which is the approach we use here. Some studies of anxiety disorders have indicated decreased CT in PFC regions (Newman et al., 2015) whereas others have indicated increased CT in PFC regions (Gold et al., 2017; Strawn et al., 2014). Differences in SA have also been found, although they have been less frequently examined. In a study using the same sample as that used here, children with higher levels of GAD symptoms were found to have decreased SA in vmPFC (Newman et al., 2015).
Some studies have reported smaller amygdala volumes in youth with mixed anxiety disorders (Milham et al., 2005; Mueller et al., 2013; Strawn et al., 2015), whereas others have found larger amygdala volumes in youth with GAD (De Bellis et al., 2000) and higher anxiety (Qin et al., 2014). In addition, smaller hippocampal volumes have been found for youth with mixed anxiety disorders (Gold et al., 2017; Mueller et al., 2013). It should be noted that most of these studies were conducted with small samples, potentially contributing to some of the inconsistencies in results across studies.
1.2. Structural neuroimaging of depressive symptoms
In adults, major depressive disorder (MDD) tends to be linked with decreased CT in PFC regions, although areas of thickening have been found (Lener et al., 2016; Peterson et al., 2009; Schmaal et al., 2016; Tu et al., 2012; van Eijndhoven et al., 2013). Similarly, some studies of pediatric MDD have indicated decreased CT in PFC regions (Marrus et al., 2015; Peterson et al., 2009) (see Supplementary Table S2). In addition, in a longitudinal neuroimaging study, greater depressive symptoms or an MDD diagnosis at 3–6 years of age was associated with an increased rate of global cortical thinning across middle childhood and into early adolescence (Luby et al., 2016). However, other studies have indicated increased CT in PFC regions (Reynolds et al., 2014) or have failed to find differences in CT for adolescents with MDD (Schmaal et al., 2016; Whittle et al., 2014). In terms of SA, a large meta-analysis found that adolescents with MDD had reduced SA in the medial OFC and superior frontal gyrus (Schmaal et al., 2016).
Studies of youth with MDD have also revealed structural alterations in limbic areas, including the hippocampus and amygdala. More specifically, these studies have indicated smaller hippocampal volumes (Blom et al., 2015; Caetano et al., 2007; Jaworska et al., 2016; MacMaster et al., 2014) and smaller amygdala volumes (Rosso et al., 2005). However, other studies of adolescents with MDD have not found differences in hippocampal volume (Rosso et al., 2005; Shad et al., 2012; Vulser et al., 2015) or amygdala volume (Caetano et al., 2007). Finally, depression in children and adolescents has also been associated with volumetric differences in the dorsal (Matsuo et al., 2008; Shad et al., 2012; Vulser et al., 2015) and ventral striatum (Whittle et al., 2014), and functional differences in the pallidum (Dennison et al., 2016).
Some evidence suggests that anxiety and depression may differ in their correlations with brain structure. For example, two prior studies of pediatric anxiety disorders found thicker cortex in PFC regions, specifically the ventromedial and ventrolateral PFC (Gold et al., 2017; Strawn et al., 2014), whereas studies of pediatric MDD have indicated more mixed results with regard to CT, showing increased, decreased, or no differences in CT (Marrus et al., 2015; Reynolds et al., 2014; Schmaal et al., 2016; Whittle et al., 2014). Thus, in this study, anxiety and depression were examined separately.
1.3. Structural neuroimaging of impulsivity
Impulsivity has been strongly associated with ADHD, which is linked with morphometric differences in PFC regions as well as other cortical regions (Nakao et al., 2011; Valera et al., 2007). In addition, studies have directly addressed the associations between brain structure and impulsivity (see Supplementary Table S3). Higher levels of impulsivity have been linked with smaller GMV in PFC regions in children and adolescents (Boes et al., 2009; Mackey et al., 2017). Few studies using surface-based morphometry have focused on children. In adults, higher impulsivity is linked with reduced CT in PFC regions, including the OFC, ACC, and middle frontal gyrus (Bernhardt et al., 2014; Holmes et al., 2016; Schilling et al., 2012; Tu et al., 2017). One large-scale study of adolescents found that higher levels of impulsivity were associated with decreased CT in superior frontal cortex (Schilling et al., 2013). In fMRI research, impulsivity has been correlated with greater activity in the ventral striatum during reward processing tasks (Forbes et al., 2009). Similarly, higher levels of impulsivity have also been associated with larger GMV in the striatum in youth (Mackey et al., 2017) and adults (Tschernegg et al., 2015).
1.4. Patterns of structural brain development
Associations of internalizing symptoms and impulsivity with brain structure may vary by age. Brain structure develops across childhood and adolescence, with evidence indicating that SA and CT develop in distinct nonlinear patterns. SA expands through childhood and early adolescence and then decreases through middle adulthood (Shaw et al., 2008; Wierenga et al., 2014). CT decreases rapidly in childhood and early adolescence, followed by a more gradual thinning, and ultimately plateauing in early- to mid-adulthood (Mutlu et al., 2013; Raznahan et al., 2011; Schnack et al., 2015; Zhou et al., 2015). These developmental changes in CT and SA are thought to relate to synaptic pruning and increases in white matter myelination (Schnack et al., 2015; Shaw et al., 2008). Patterns of CT and SA development vary across cortical regions, with some regions exhibiting more nonlinear patterns of development than others (Mutlu et al., 2013).
A few studies have indicated differences in associations between internalizing symptoms and CT by age. For example, one study found an interaction between internalizing symptoms and age, such that internalizing symptoms were negatively associated with CT at younger ages (<9 years), but positively associated with CT at older ages (15–22 years) (Ducharme et al., 2014). Thus, we explored interactions of anxiety, depression, and impulsivity with age and age2 for CT, SA, and subcortical volume.
1.5. Current study
In this study, we examined differences in gray matter morphometry associated with anxiety symptoms, depressive symptoms, and impulsivity in children and adolescents. Participants were 7- to 21-year-olds from the Pediatric Imaging, Neurocognition, and Genetics (PING) study for whom high-resolution, 3-Tesla, T1-weighted MRI and self-report measures of anxiety, depression, and impulsivity were available (Jernigan et al., 2016). We used both region-of-interest (ROI) and exploratory whole-brain approaches to identify CT, SA, and subcortical GMV differences based on the level of anxiety, depression, or impulsivity.
Based on previous research (Ducharme et al., 2014; Holmes et al., 2016; Marrus et al., 2015; Newman et al., 2015; Schilling et al., 2013; Schmaal et al., 2016; Strawn et al., 2014), ROIs included 11 PFC regions and 6 subcortical regions (e.g., amygdala, hippocampus, striatum; see Table 2 for the full list of ROIs). High levels of both internalizing symptoms and impulsivity are linked with reduced top-down control over emotions and reward-related behavior (Aldao et al., 2016), suggesting that differences in overlapping regions in the prefrontal cortex (PFC) may underlie both domains. Coupled with direct evidence of PFC involvement in anxiety, depression, and impulsivity (Boes et al., 2009; Gold et al., 2017), these findings point to PFC regions as the most likely cortical regions to be shared across domains.
Table 2.
Associations of CT in PFC regions and subcortical ROI GMV with levels of anxiety, depression, and impulsivity.
| Anxiety symptoms |
Depressive symptoms |
Impulsivity |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| β | p | FDR-corrected p | β | p | FDR-corrected p | β | p | FDR-corrected p | |
| Cortical ROI | |||||||||
| Ventromedial PFC/medial OFC | −0.08 | 0.0219 | 0.1205 | −0.12 | 0.0012 | 0.0132 | −0.10 | 0.0147 | 0.0404 |
| Lateral OFC | −0.07 | 0.0521 | 0.1433 | −0.07 | 0.0359 | 0.0744 | −0.08 | 0.0459 | 0.0631 |
| Frontal pole | −0.03 | 0.5358 | 0.5894 | −0.09 | 0.0343 | 0.0744 | −0.13 | 0.0059 | 0.0325 |
| Rostral ACC | −0.06 | 0.1529 | 0.2812 | −0.07 | 0.1002 | 0.1378 | −0.06 | 0.1853 | 0.2265 |
| Caudal ACC | −0.05 | 0.2428 | 0.3339 | −0.04 | 0.3909 | 0.3909 | −0.05 | 0.3365 | 0.3365 |
| Rostral middle frontal gyrus | −0.04 | 0.2057 | 0.3232 | −0.07 | 0.0406 | 0.0744 | −0.10 | 0.0039 | 0.0325 |
| Caudal middle frontal gyrus | −0.08 | 0.0204 | 0.1205 | −0.04 | 0.2142 | 0.2618 | −0.08 | 0.0322 | 0.0572 |
| Pars orbitalis | −0.09 | 0.0451 | 0.1433 | −0.09 | 0.0394 | 0.0744 | −0.12 | 0.0125 | 0.0404 |
| Pars opercularis | −0.03 | 0.5313 | 0.5894 | −0.04 | 0.3799 | 0.3909 | −0.10 | 0.0364 | 0.0572 |
| Pars triangularis | −0.02 | 0.5967 | 0.5967 | −0.07 | 0.0650 | 0.1021 | −0.05 | 0.2623 | 0.2885 |
| Superior frontal gyrus | −0.05 | 0.1534 | 0.2812 | −0.08 | 0.0125 | 0.0688 | −0.08 | 0.0237 | 0.0521 |
| Subcortical ROI | |||||||||
| Amygdala | −0.05 | 0.1257 | 0.2514 | −0.07 | 0.0296 | 0.0592 | −0.06 | 0.1113 | 0.2638 |
| Hippocampus | −0.08 | 0.0568 | 0.2514 | −0.11 | 0.0145 | 0.0435 | −0.07 | 0.1319 | 0.2638 |
| Caudate | −0.04 | 0.4119 | 0.6179 | −0.04 | 0.4472 | 0.6479 | 0.04 | 0.4624 | 0.4624 |
| Putamen | −0.002 | 0.9590 | 0.9590 | 0.01 | 0.7228 | 0.7228 | 0.05 | 0.2962 | 0.3884 |
| Nucleus accumbens | −0.003 | 0.9408 | 0.9590 | −0.02 | 0.5399 | 0.6479 | 0.04 | 0.3237 | 0.3884 |
| Pallidum | 0.07 | 0.1011 | 0.2514 | 0.10 | 0.0121 | 0.0435 | 0.10 | 0.0244 | 0.1464 |
Note. Multiple regression analyses tested associations with anxiety, depression, and impulsivity, adjusting for age, age2, sex, GAFs, and scanner model. Analyses of subcortical GMV additionally corrected for whole brain volume.
CT, cortical thickness; ROI, region-of-interest; PFC, prefrontal cortex; OFC, orbitofrontal cortex; GMV, gray matter volume.
High levels of internalizing symptoms and impulsivity may have unique and shared neuroanatomical correlates. Based on previous studies (Boes et al., 2009; Newman et al., 2015), we hypothesized that they would be associated with CT in vmPFC and ACC, but only impulsivity would be associated with CT in lateral PFC regions. Medial PFC regions connect directly with the amygdala to support emotion regulation, whereas lateral PFC regions have been closely linked with top-down control more generally (Holmes et al., 2016). We tentatively predicted that higher impulsivity would be linked to cortical thinning as opposed to thickening, but for anxiety and depression, no specific predictions were made about direction, based on the available research (Gold et al., 2017; Schmaal et al., 2016). At the subcortical level, we expected that both depressive symptoms and impulsivity would be associated with striatal volume, potentially in opposite directions, given the multiple roles of the striatum, which include reward-related processing and involvement in pleasure and anhedonia (Forbes et al., 2009; Zisner and Beauchaine, 2016). In addition, only internalizing symptoms were expected to be associated with smaller amygdala and hippocampal volume, given their primary role in emotional reactivity and memory as well as mediating physiological stress responses (Koolschijn et al., 2013).
We also explored whether associations of anxiety, depression, and impulsivity with brain morphometry varied by age. Given developmental changes in brain structure, these symptom domains may relate to brain structure differently depending on age. In addition, due to the nonlinear patterns of structural brain development across childhood and adolescence (Ostby et al., 2009), we also examined the quadratic term for age as a moderator.
To our knowledge, only one prior study using PING data has examined associations between dimensions of psychopathology and gray matter morphometry, and this study focused on GAD symptoms (Newman et al., 2015). Thus, the current study is the first to provide a comprehensive picture of associations of anxiety symptoms, depressive symptoms, and impulsivity with gray matter morphometry in the PING study sample.
2. Methods
2.1. Participants
The PING study recruited 3- to 21-year-old participants through a combination of web-based and community advertising at nine university-based data collection sites located in or around Los Angeles, San Diego, New Haven, Sacramento, Boston, Baltimore, Honolulu, and New York (http://pingstudy.ucsd.edu/) (Jernigan et al., 2016; Newman et al., 2015). Exclusionary criteria included neurological disorder; history of head trauma; preterm birth; autism spectrum disorder, bipolar disorder, schizophrenia, or intellectual disability; and contraindications for MRI. Written informed consent was provided by parents for all participants <18 years of age and by the participants themselves if they were ≥ 18 years of age. In addition, child assent was obtained for 7- to 17-year-old participants. Each site's Institutional Review Board approved the study.
Analyses for this study focused on the participants who completed web-based, self-report assessments of anxiety, depression, and impulsivity from the PhenX Toolkit (http://www.phenxtoolkit.org) (see Table 1 for sample characteristics) (Jernigan et al., 2016). This study uses all the data available in the PING sample regarding these constructs. Six of the nine PING sites chose to administer these assessments, which were given to participants ≥8 years of age. In total, 328 participants completed the anxiety and depression measures, and 254 participants completed the impulsivity measure. After accounting for the nesting of participants within site, there were no significant differences in age, sex, genetic ancestry, or parental education between this subsample and the participants who were eligible but did not complete these PhenX questionnaires. However, participants who completed these PhenX questionnaires came from higher income families compared to those who did not. Also, the PhenX questionnaires were often completed after neuroimaging. The time between when participants completed neuroimaging to when they completed the PhenX battery (M = 1.33 years; SD = 0.56) was not a significant covariate in any of the analyses.
Table 1.
Descriptive statistics for sample characteristics.
| M (SD) or n (%) | Range | |
|---|---|---|
| Age at neuroimaging (years) | 13.65 (3.62) | 7.08–21.00 |
| Age at PhenX completion (years) | 14.80 (3.91) | 8.25–22.67 |
| Sex (male) | 172 (52.44%) | – |
| Family income (U.S. dollars) | 104,287.54 (76,810.78) | 4500.00-325,000.00 |
| Parental education (years) | 15.05 (2.26) | 6.00–18.00 |
| Genetic ancestry factor (GAF) | ||
| African | 0.11 (0.25) | 0.00–1.00 |
| American Indian | 0.06 (0.14) | 0.00–0.80 |
| Central Asian | 0.03 (0.13) | 0.00–1.00 |
| East Asian | 0.20 (0.34) | 0.00–1.00 |
| European | 0.59 (0.38) | 0.00–1.00 |
| Oceanic | 0.01 (0.03) | 0.00–0.23 |
| Scanner model | ||
| Philips Achieva | 24 (8.11%) | |
| GE Discovery | 36 (12.16%) | |
| GE Signa | 47 (15.88%) | |
| Siemens TrioTim | 189 (63.85%) | |
| Anxiety | 28.82 (17.36) | 0.00–100.32 |
| SCARED-R total score ≥ 33a | 121 (36.89%) | – |
| Depression | 13.51 (10.08) | 0.00–59.00 |
| CES-DC total score ≥ 15b | 125 (38.11%) | – |
| Impulsivity | 129.22 (23.00) | 76.70–192.93 |
Note. Sample size is 328 for demographics, anxiety, and depression; 313 for GAFs; 296 for scanner model; and 254 for impulsivity. Anxiety, depression, and impulsivity total scores are presented. SCARED-R, Screen for Child Anxiety Related Emotional Disorders-Revised; CES-DC, Center for Epidemiologic Studies Depression Scale for Children.
The recommended clinical-range cutoff score (Bodden et al., 2009).
The recommended clinical-range cutoff score (Fendrich et al., 1990).
2.2. Image acquisition and processing
As described previously (Brown et al., 2012; Jernigan et al., 2016), each site administered a standardized high-resolution structural MRI protocol (see Supplementary Table S4 for scanner models and parameters); images were acquired on 3T scanners. T1-weighted imaging data included in this study passed standardized quality control procedures, including visual inspection ratings by trained imaging technicians and automated quality control algorithms. There was no manual editing of data that were deemed acceptable for inclusion. Morphometric analysis of structural MRI data was performed using a specialized processing stream in FreeSurfer (version 4.5) (http://surfer.nmr.mgh.harvard.edu/). CT was calculated as the shortest distance between the white and pial surfaces (Fischl et al., 2004). ROI labels for 11 PFC regions were derived from the Desikan-Killiany Atlas using FreeSurfer's automated parcellation procedures (Desikan et al., 2006; Fischl et al., 2004) (see Supplemental Materials for details). Subcortical structures were labeled using FreeSurfer's automated, atlas-based, volumetric segmentation procedure (Jernigan et al., 2016).
2.3. Measures
2.3.1. Internalizing symptoms
Participants completed the Screen for Child Anxiety Related Emotional Disorders-Revised (SCARED-R) (Bodden et al., 2009), a 66-item self-report measure of anxiety disorder symptoms. Participants rated how frequently they experience each item on a 3-point scale, ranging from 0 (almost never) to 2 (often). The total score was used in this study. The SCARED-R has demonstrated high reliability and validity (Bodden et al., 2009).
Participants also completed the Center for Epidemiologic Studies Depression Scale for Children (CES-DC) (Fendrich et al., 1990), a 20-item self-report measure. Participants rate each item in terms of frequency during the last week using a 4-point scale, ranging from 0 (not at all) to 3 (a lot). The CES-DC has strong psychometric properties (Fendrich et al., 1990). The SCARED-R total score and CES-DC total score were strongly correlated (r = 0.56, p < .0001), consistent with the high comorbidity of anxiety and depressive disorders (Cummings et al., 2014).
2.3.2. Impulsivity
Participants completed the 59-item UPPS-P Impulsive Behavior Scale (Whiteside and Lynam, 2001), which includes the Lack of Premeditation/Planning (11 items), Negative Urgency (12 items), Sensation Seeking (12 items), Lack of Perseverance (10 items), and Positive Urgency (14 items) subscales. Items on these subscales are rated on a 4-point scale ranging from 1 (strongly agree) to 4 (strongly disagree). The UPPS-P total score was used in this study. The strong psychometric properties of the UPPS-P have been well documented (Whiteside and Lynam, 2001).
2.3.3. Genetic ancestry factors (GAFs)
GAFs were calculated to estimate the degree of genetic similarity of the participant to each of six reference populations (Jernigan et al., 2016). More specifically, GAFs estimated the proportion of European, African, American Indian, East Asian, Central Asian, and Oceanic ancestry for each participant. Previous PING studies have shown strong correlations between genetically-determined and self-reported ancestry (Jernigan et al., 2016).
2.4. Statistical analysis
Based on previous studies (Ducharme et al., 2014; Holmes et al., 2016; Marrus et al., 2015; Newman et al., 2015; Schilling et al., 2013; Strawn et al., 2014), a priori ROIs included 11 PFC regions (vmPFC/medial OFC, lateral OFC, rostral ACC, caudal ACC, pars orbitalis, pars opercularis, pars triangularis, rostral middle frontal gyrus, caudal middle frontal gyrus, superior frontal gyrus, and frontal pole) and six subcortical regions (amygdala, hippocampus, putamen, caudate, nucleus accumbens, and pallidum). Multiple regression analyses tested associations with anxiety symptoms, depressive symptoms, and impulsivity, separately, in each ROI. Age, age2, sex, GAFs, and scanner model were also included in the regression models; subcortical GMV analyses additionally controlled for whole brain volume. We first examined interactions of anxiety/depression/impulsivity with age and age2 for CT, SA, and subcortical volume. None of these interactions were significant. Also, there were no significant interactions of anxiety, depression, or impulsivity with sex. Family socioeconomic status (family income, parental education) was associated with SA but not CT, and thus these variables were included as covariates in analyses of SA but not CT (Noble et al., 2015). To control for multiple comparisons, a false discovery rate (FDR) correction was applied to the CT, SA, and subcortical GMV analyses, separately (α = 0.05). Exploratory, whole-brain, vertex-wise analyses were conducted using the PING portal (10 mm smoothing kernel) (http://pingstudy.ucsd.edu/).
3. Results
3.1. Associations of regional CT with anxiety, depression, and impulsivity
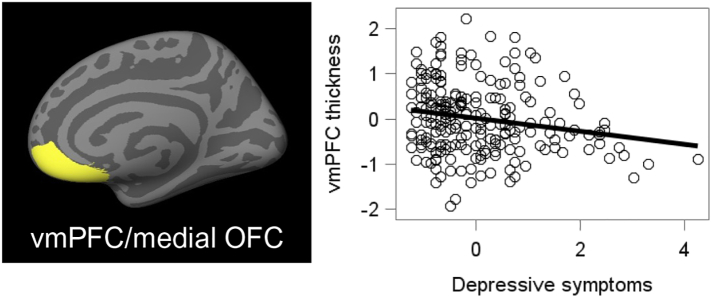
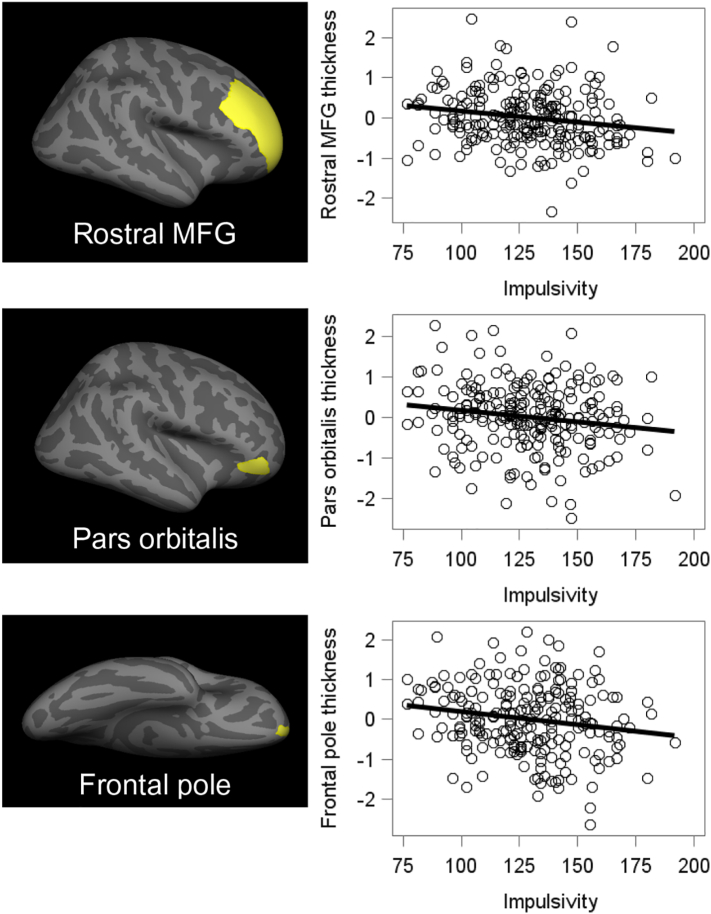
As shown in Table 2, higher levels of both depressive symptoms and impulsivity were significantly associated with reduced CT in vmPFC/medial OFC. Given that depressive symptoms and impulsivity were significantly correlated, r = 0.33, p < .001, we then conducted analyses in which they were entered simultaneously into the same model. As shown in Fig. 1, higher levels of depressive symptoms remained significantly associated with decreased CT in vmPFC/medial OFC, β = −0.09, p = .0196, but impulsivity did not, β = −0.06, p = .1204. Higher levels of impulsivity, but not anxiety or depression, were significantly associated with reduced CT in the frontal pole, rostral middle frontal gyrus, and pars orbitalis (see Table 2 and Fig. 2). After excluding youth with a parent- or self-reported history of ADHD (n = 19; 8.52%), results remained significant.
Fig. 1.
Cortical thickness ROI showing associations with depressive symptoms. Values on the Y axis were adjusted for age, age2, sex, GAFs, and scanner model. Although the right hemisphere is depicted here, analyses averaged across right and left hemispheres. Depression scores are average item scores on the CES-DC.
vmPFC, ventromedial prefrontal cortex.
OFC, orbitofrontal cortex.
Fig. 2.
Cortical thickness ROIs showing associations with impulsivity. Values on the Y axis were adjusted for age, age2, sex, GAFs, and scanner model. Although right hemispheres are depicted here, analyses averaged across right and left hemispheres.
MFG, middle frontal gyrus.
3.2. Associations of regional SA with anxiety, depression, and impulsivity
There were no significant associations of anxiety symptoms, depressive symptoms, or impulsivity with SA in any of the ROIs.
3.3. Associations of subcortical GMV with anxiety, depression, and impulsivity
As shown in Table 2, higher levels of depressive symptoms were significantly associated with smaller hippocampal volume and larger pallidum volume. Anxiety symptoms and impulsivity were not significantly associated with volume of any of the subcortical ROIs.
3.4. Exploratory whole-brain analyses
Using the PING portal to focus on CT and SA, no significant clusters emerged for anxiety symptoms, depressive symptoms, or impulsivity (p < .05, FDR-corrected) after adjusting for age, age2, sex, GAFs, and scanner model. However, CT in medial PFC regions was associated with depressive symptoms at an uncorrected p-value of 0.001 (see Fig. S1).
3.5. Supplemental categorical analyses
Data on formal diagnosis of depressive or anxiety disorders were not available. However, we also employed a categorical approach by comparing youth above and below the clinical-range cut-off for an anxiety disorder and/or MDD (see Table 1) in terms of CT, SA, and subcortical GMV. The results were the same, with similar sized effects (see Supplementary Table S5).
4. Discussion
The goal of this study was to examine associations of cortical surface anatomy and subcortical GMV with continuous variability in anxiety and depressive symptoms and impulsivity in children and adolescents. Impulsivity has been more commonly associated with externalizing rather than internalizing disorders (Zisner and Beauchaine, 2016) and thus was predicted to differ from anxiety and depression in its neural substrates. At the same time, heterotypic comorbidity is common in youth, and difficulties with self-regulatory control are shared across internalizing problems and impulsive behavior. Thus, some neural mechanisms may be shared across internalizing symptoms and impulsivity. Findings indicated that in separate models, higher levels of both depressive symptoms and impulsivity were linked with reduced CT in vmPFC/medial OFC, but when considered simultaneously, only depressive symptoms were uniquely associated with reduced CT in this region. Higher impulsivity, but not anxiety or depressive symptoms, was significantly associated with reduced CT in the frontal pole, rostral middle frontal gyrus, and pars orbitalis.
These findings are consistent with research linking the vmPFC/medial OFC with depression (Lener et al., 2016; Peterson et al., 2009; Tu et al., 2012; van Eijndhoven et al., 2013). In fact, in a recent meta-analysis of neuroimaging studies of MDD, the medial OFC showed the largest effect sizes (Schmaal et al., 2016). A core feature of affective disorders is difficulty with the regulation of negative emotions, skills that depend in part on the vmPFC. Through direct connections with the amygdala, the vmPFC/medial OFC plays a critical role in dampening reactivity to negative emotional stimuli (Ducharme et al., 2014; Guyer et al., 2008; Marrus et al., 2015; Newman et al., 2015; Vulser et al., 2015). The vmPFC/medial OFC has also been implicated in reward-related decision-making and self-report measures of impulsivity (Boes et al., 2009), and thus may have dual roles in terms of involvement in internalizing symptoms and impulsivity (Luking et al., 2016). Findings from this study are partially consistent with this notion, and point to this region as the most likely to relate to both symptom domains.
Lateral PFC regions, such as the rostral middle frontal gyrus and pars orbitalis, have been associated with cognitive control. The construct of impulsivity, including how it is operationalized here, is strongly tied to regulatory skills or cognitive control, regardless of the emotional or motivational significance of the context. Certainly, impulsivity describes approach-related behaviors in the context of reward, but it may also capture these tendencies outside of the reward context as well. This conceptual link between impulsivity and cognitive control may explain these associations with lateral PFC.
In this study, increased depressive symptoms and impulsivity were associated with thinner rather than thicker PFC. For impulsivity, this direction of association is consistent with prior studies of CT in children and adolescents (Schilling et al., 2013) and adults (Holmes et al., 2016; Schilling et al., 2012; Tu et al., 2017). Similarly, studies of adult MDD generally report cortical thinning, especially in the medial OFC (Lener et al., 2016; Peterson et al., 2009; Schmaal et al., 2016; van Eijndhoven et al., 2013). Studies of adolescent MDD have reported increased, decreased, or no differences in CT (Luby et al., 2016; Peterson et al., 2009; Reynolds et al., 2014; Schmaal et al., 2016; Shad et al., 2012). Although we did not find any interactions with age for CT, more attention to potentially modifying factors such as age, timing, or duration of symptoms may explain differences in the direction of association, especially given evidence of divergent patterns for first-episode compared to recurring MDD (Frodl et al., 2003).
Higher levels of depressive symptoms and impulsivity could be linked with altered developmental trajectories of cortical thinning during childhood. In typical development, CT decreases rapidly in childhood and early adolescence, followed by a more gradual thinning, and ultimately plateauing in early- to mid-adulthood (Brown et al., 2012; Raznahan et al., 2011). Early exposure to chronic stress, which often precedes elevations in internalizing symptoms, has been linked with accelerated brain development in both animal models and human studies (Mackey et al., 2017). In addition, a longitudinal neuroimaging study of early-onset depression revealed an increased rate of global cortical thinning into early adolescence (Luby et al., 2016). Similarly, another recent longitudinal study found accelerated frontal lobe cortical thinning in adolescents who developed depression by early adulthood (Bos et al., 2018). Our results linking higher levels of depressive symptoms with reduced CT in vmPFC/medial OFC are consistent with a pattern of accelerated maturation. However, this interpretation is speculative as longitudinal data were not available for this sample. In addition, other interpretations are also possible, including the possibility of excessive cortical thinning that is age invariant.
It should also be noted that prior work has suggested developmental delays in cortical thinning in children with ADHD (Shaw et al., 2011) and internalizing problems (Ducharme et al., 2014). Of course, longitudinal studies are needed to formally test whether developmental trajectories of CT vary with symptomatology, and fortunately a growing number of these studies are being published (Bos et al., 2018; Ducharme et al., 2014; Luby et al., 2016; Shaw et al., 2011; Whittle et al., 2014).
At the subcortical level, higher levels of depressive symptoms, but not impulsivity, were significantly associated with smaller hippocampal volume. These results are consistent with previous studies (Blom et al., 2015; Jaworska et al., 2016; Tschernegg et al., 2015), including a longitudinal study indicating that adolescents who were later diagnosed with MDD showed attenuated growth of the hippocampus (Whittle et al., 2014). One possibility is that these effects could be due to stress-induced chronic hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis. Indeed, the hippocampus has a high density of glucocorticoid receptors and plays a key role in the negative feedback loop of the HPA axis. Chronically elevated HPA activity could lead to neuronal atrophy or inhibition of neurogenesis in the hippocampus (Blom et al., 2015).
Higher depressive symptoms were also associated with larger volume in the pallidum, part of the basal ganglia involved in reward-processing and hedonic experience (Smith et al., 2009). This finding could be due to symptoms of anhedonia, which have been linked with structural and functional differences in the pallidum (Dennison et al., 2016). Studies of adults have tended to link MDD with smaller pallidal volume (Kempton et al., 2011; Onyewuenyi et al., 2014), although anhedonia has been associated with larger pallidal volume (Wang et al., 2014).
It is not clear why associations with cortical SA were not found. Reduced SA in PFC regions has been linked with MDD (Schmaal et al., 2016) and higher GAD symptoms in children and adolescents (Newman et al., 2015). We did not find any interactions with age or age2 for SA, precluding the possibility that the lack of findings for SA reflect a failure to account for the linear and quadratic developmental patterns in SA. Additionally, none of the associations between brain structure and anxiety symptoms survived correction for multiple comparisons. This is possibly due to aggregating across types of anxiety, and future studies should delve deeper into specific types of anxiety in this sample.
Strengths of this study include the large sample size, use of a youth sample closer to the normal range of symptoms (as compared to case-control designs), rigorous quality control and standardized processing of MRI data, and conservative statistical procedures that accounted for multiple comparisons. Findings from this study should also be interpreted taking into account several limitations. This study employed a cross-sectional, correlational design, precluding our ability to make causal inferences about development (Kraemer et al., 2000). The broad age range is another limitation given that it spans puberty, as well as the continued development of brain structure and symptomatology throughout adolescence. Of note, there were no significant interactions of anxiety, depression, or impulsivity with age or age2 for CT, SA, or subcortical volume. In addition, the measurement of anxiety/depression symptoms and impulsivity via self-report may have inflated the correlation between them to some degree, although it was only in the small to medium range (r = 0.17–0.33). Relatedly, another limitation is the lack of psychiatric interviews. Finally, the primary analytic approach of this study was consistent with comparing brain morphometry across internalizing and externalizing dimensions (although we examined anxiety and depression separately). Although data were not available on externalizing behaviors such as aggression and rule-breaking behavior, impulsivity has been put forth as a key symptom dimension underlying externalizing disorders (Beauchaine et al., 2017). Methodological factors, such as MRI acquisition parameters or subcortical volume quantification procedures, may contribute to inconsistencies in the literature. Previous studies have noted possible inaccuracies of the FreeSurfer automated segmentation methods for measuring subcortical volumes (Wenger et al., 2014), and have highlighted differences between automated segmentation and manual tracing procedures (Hanson et al., 2015). However, this approach is consistent with the many previous large-scale studies that have used FreeSurfer methods, and rigorous quality control procedures were used in the PING study (Jernigan et al., 2016).
In summary, we investigated shared and unique gray matter morphometry associated with continuous variability in anxiety symptoms, depressive symptoms, and impulsivity among children and adolescents. Higher levels of depressive symptoms were uniquely associated with reduced CT in vmPFC/medial OFC. Higher levels of impulsivity, but not anxiety or depression, were significantly associated with reduced CT in lateral PFC regions (rostral middle frontal gyrus, pars orbitalis) and the frontal pole. Higher levels of depressive symptoms, but not impulsivity, were significantly associated with smaller hippocampal volume and larger pallidal volume. These findings shed light on the similarities and differences in underlying neuroanatomy of internalizing symptoms and impulsivity during childhood and adolescence.
Acknowledgements
Data collection and sharing for this project was funded by the Pediatric Imaging, Neurocognition, and Genetics Study (PING) (National Institutes of Health Grant RC2DA029475). PING is funded by the National Institute on Drug Abuse and the Eunice Kennedy Shriver National Institute of Child Health & Human Development. PING data are disseminated by the PING Coordinating Center at the Center for Human Development, University of California, San Diego. This work was also made possible by funding from the Annie E. Casey Foundation; Teachers College, Columbia University; and a National Institute of Mental Health (NIMH) training grant (T32MH13043).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nicl.2018.07.020.
Contributor Information
Emily C. Merz, Email: emilymerz@gmail.com.
Xiaofu He, Email: xh2170@cumc.columbia.edu.
Kimberly G. Noble, Email: kgn2106@tc.columbia.edu.
Appendix A. Supplementary data
Supplementary material
References
- Aldao A., Gee D.G., De Los Reyes A., Seager I. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: current and future directions. Dev. Psychopathol. 2016;28(4pt1):927–946. doi: 10.1017/S0954579416000638. [DOI] [PubMed] [Google Scholar]
- Beauchaine T.P., Zisner A.R., Sauder C.L. Trait impulsivity and the externalizing Spectrum. Annu. Rev. Clin. Psychol. 2017;13:343–368. doi: 10.1146/annurev-clinpsy-021815-093253. [DOI] [PubMed] [Google Scholar]
- Bernhardt B.C., Smallwood J., Tusche A., Ruby F.J.M., Engen H.G., Steinbeis N., Singer T. Medial prefrontal and anterior cingulate cortical thickness predicts shared individual differences in self-generated thought and temporal discounting. NeuroImage. 2014;90:290–297. doi: 10.1016/j.neuroimage.2013.12.040. [DOI] [PubMed] [Google Scholar]
- Blom E.H., Han L.K.M., Connolly C.G., Ho T.C., Lin J., Lewinn K.Z.…Yang T.T. Peripheral telomere length and hippocampal volume in adolescents with major depressive disorder. Transl. Psychiatry. 2015;5(11) doi: 10.1038/tp.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodden D.H.M., Bögels S.M., Muris P. The diagnostic utility of the Screen for Child Anxiety Related Emotional Disorders-71 (SCARED-71) Behav. Res. Ther. 2009;47(5):418–425. doi: 10.1016/j.brat.2009.01.015. [DOI] [PubMed] [Google Scholar]
- Boes A.D., Bechara A., Tranel D., Anderson S.W., Richman L., Nopoulos P. Right ventromedial prefrontal cortex: a neuroanatomical correlate of impulse control in boys. Soc. Cogn. Affect. Neurosci. 2009;4(1):1–9. doi: 10.1093/scan/nsn035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos M.G.N., Peters S., van de Kamp F.C., Crone E.A., Tamnes C.K. Emerging depression in adolescence coincides with accelerated frontal cortical thinning. J. Child Psychol. Psychiatry. 2018 doi: 10.1111/jcpp.12895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.T., Kuperman J.M., Chung Y., Erhart M., McCabe C., Hagler D.J.…Dale A.M. Neuroanatomical assessment of biological maturity. Curr. Biol. 2012;22(18):1693–1698. doi: 10.1016/j.cub.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano S.C., Fonseca M., Hatch J.P., Olvera R.L., Nicoletti M., Hunter K.…Soares J.C. Medial temporal lobe abnormalities in pediatric unipolar depression. Neurosci. Lett. 2007;427(3):142–147. doi: 10.1016/j.neulet.2007.06.014. [DOI] [PubMed] [Google Scholar]
- Cummings C.M., Caporino N.E., Kendall P.C. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol. Bull. 2014;140(3):816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Avanzato C., Joormann J., Siemer M., Gotlib I.H. Emotion regulation in depression and anxiety: examining diagnostic specificity and stability of strategy use. Cogn. Ther. Res. 2013;37(5):968–980. [Google Scholar]
- De Bellis M.D., Casey B.J., Dahl R.E., Birmaher B., Williamson D.E., Thomas K.M.…Ryan N.D. A pilot study of amygdala volumes in pediatric generalized anxiety disorder. Biol. Psychiatry. 2000;48(1):51–57. doi: 10.1016/s0006-3223(00)00835-0. [DOI] [PubMed] [Google Scholar]
- Dennison M.J., Sheridan M.A., Busso D.S., Jenness J.L., Peverill M., Rosen M.L., McLaughlin K.A. Neurobehavioral markers of resilience to depression amongst adolescents exposed to child abuse. J. Abnorm. Psychol. 2016;125(8):1201–1212. doi: 10.1037/abn0000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desikan R.S., Ségonne F., Fischl B., Quinn B.T., Dickerson B.C., Blacker D.…Killiany R.J. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage. 2006;31(3):968–980. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Ducharme S., Albaugh M.D., Hudziak J.J., Botteron K.N., Nguyen T.-V., Truong C.…O'Neill J. Anxious/depressed symptoms are linked to right ventromedial prefrontal cortical thickness maturation in healthy children and young adults. Cereb. Cortex. 2014;24(11):2941–2950. doi: 10.1093/cercor/bht151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eijndhoven P., van Wingen G., Katzenbauer M., Groen W., Tepest R., Fernández G.…Tendolkar I. Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. Am. J. Psychiatry. 2013;170(12):1477–1486. doi: 10.1176/appi.ajp.2013.12121504. [DOI] [PubMed] [Google Scholar]
- Fendrich M., Weissman M.M., Warner V. Screening for depressive disorder in children and adolescents: validating the center for epidemiologic studies depression scale for children. Am. J. Epidemiol. 1990;131(3):538–551. doi: 10.1093/oxfordjournals.aje.a115529. [DOI] [PubMed] [Google Scholar]
- Fischl B., van der Kouwe A., Destrieux C., Halgren E., Ségonne F., Salat D.H.…Dale A.M. Automatically parcellating the human cerebral cortex. Cereb. Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- Forbes E., Brown S., Kimak M., Ferrell R., Manuck S., Hariri A. Genetic variation in components of dopamine neurotransmission impacts ventral striatal reactivity associated with impulsivity. Mol. Psychiatry. 2009;14(1):60–70. doi: 10.1038/sj.mp.4002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frodl T., Meisenzahl E.M., Zetzsche T., Born C., Jäger M., Groll C.…Möller H.-J. Larger amygdala volumes in first depressive episode as compared to recurrent major depression and healthy control subjects. Biol. Psychiatry. 2003;53(4):338–344. doi: 10.1016/s0006-3223(02)01474-9. [DOI] [PubMed] [Google Scholar]
- Gold A.L., Brotman M.A., Adleman N.E., Lever S.N., Steuber E.R., Fromm S.J.…Leibenluft E. Comparing brain morphometry across multiple childhood psychiatric disorders. J. Am. Acad. Child Adolesc. Psychiatry. 2016;55(12):1027–1037.e3. doi: 10.1016/j.jaac.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold A.L., Steuber E.R., White L.K., Pacheco J., Sachs J.F., Pagliaccio D.…Pine D.S. Cortical thickness and subcortical gray matter volume in pediatric anxiety disorders. Neuropsychopharmacology. 2017 doi: 10.1038/npp.2017.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer A.E., Lau J.Y.F., McClure-Tone E.B., Parrish J., Shiffrin N.D., Reynolds R.C.…Nelson E.E. Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Arch. Gen. Psychiatry. 2008;65(11):1303–1312. doi: 10.1001/archpsyc.65.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson J.L., Nacewicz B.M., Sutterer M.J., Cayo A.A., Schaefer S.M., Rudolph K.D.…Davidson R.J. Behavior problems after early life stress: contributions of the Hippocampus and amygdala. Biol. Psychiatry. 2015;77(4):314–323. doi: 10.1016/j.biopsych.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes A.J., Hollinshead M.O., Roffman J.L., Smoller J.W., Buckner R.L. Individual differences in cognitive control circuit anatomy link sensation seeking, impulsivity, and substance use. J. Neurosci. 2016;36(14):4038–4049. doi: 10.1523/JNEUROSCI.3206-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T., Cuthbert B., Garvey M., Heinssen R., Pine D.S., Quinn K.…Wang P. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatr. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jaworska N., Yücel K., Courtright A., MacMaster F.P., Sembo M., MacQueen G. Subgenual anterior cingulate cortex and hippocampal volumes in depressed youth: the role of comorbidity and age. J. Affect. Disord. 2016;190:726–732. doi: 10.1016/j.jad.2015.10.064. [DOI] [PubMed] [Google Scholar]
- Jernigan T.L., Brown T.T., Hagler D.J., Jr., Akshoomoff N., Bartsch H., Newman E.…Dale A.M. The pediatric imaging, neurocognition, and genetics (PING) data repository. NeuroImage. 2016;124(Part B):1149–1154. doi: 10.1016/j.neuroimage.2015.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempton M.J., Salvador Z., Munafò M.R., Geddes J.R., Simmons A., Frangou S., Williams S.C.R. Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder. Arch. Gen. Psychiatry. 2011;68(7):675–690. doi: 10.1001/archgenpsychiatry.2011.60. [DOI] [PubMed] [Google Scholar]
- Koolschijn P.C.M.P., van IJzendoorn M.H., Bakermans-Kranenburg M.J., Crone E.A. Hippocampal volume and internalizing behavior problems in adolescence. Eur. Neuropsychopharmacol. 2013;23(7):622–628. doi: 10.1016/j.euroneuro.2012.07.001. [DOI] [PubMed] [Google Scholar]
- Kraemer H.C., Yesavage J.A., Taylor J.L., Kupfer D. How can we learn about developmental processes from cross-sectional studies, or can we? Am. J. Psychiatry. 2000;157(2):163–171. doi: 10.1176/appi.ajp.157.2.163. [DOI] [PubMed] [Google Scholar]
- Lener M.S., Kundu P., Wong E., Dewilde K.E., Tang C.Y., Balchandani P., Murrough J.W. Cortical abnormalities and association with symptom dimensions across the depressive spectrum. J. Affect. Disord. 2016;190:529–536. doi: 10.1016/j.jad.2015.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby J.L., Belden A.C., Jackson J.J., Lessov-Schlaggar C.N., Harms M.P., Tillman R.…Barch D.M. Early childhood depression and alterations in the trajectory of gray matter maturation in middle childhood and early adolescence. JAMA Psychiatry. 2016;73(1):31–38. doi: 10.1001/jamapsychiatry.2015.2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luking K.R., Pagliaccio D., Luby J.L., Barch D.M. Reward processing and risk for depression across development. Trends Cogn. Sci. 2016;20(6):456–468. doi: 10.1016/j.tics.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey S., Chaarani B., Kan K.-J., Spechler P.A., Orr C., Banaschewski T.…Garavan H. Brain regions related to impulsivity mediate the effects of early adversity on antisocial behavior. Biol. Psychiatry. 2017 doi: 10.1016/j.biopsych.2015.12.027. [DOI] [PubMed] [Google Scholar]
- MacMaster F.P., Carrey N., Langevin L.M., Jaworska N., Crawford S. Disorder-specific volumetric brain difference in adolescent major depressive disorder and bipolar depression. Brain Imaging and Behav. 2014;8(1):119–127. doi: 10.1007/s11682-013-9264-x. [DOI] [PubMed] [Google Scholar]
- Marrus N., Belden A., Nishino T., Handler T., Ratnanather J.T., Miller M.…Botteron K. Ventromedial prefrontal cortex thinning in preschool-onset depression. J. Affect. Disord. 2015;180:79–86. doi: 10.1016/j.jad.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo K., Rosenberg D.R., Easter P.C., MacMaster F.P., Chen H.-H., Nicoletti M.…Soares J.C. Striatal volume abnormalities in treatment-naïve patients diagnosed with pediatric major depressive disorder. J. Child Adolesc. Psychopharmacol. 2008;18(2):121–131. doi: 10.1089/cap.2007.0026. [DOI] [PubMed] [Google Scholar]
- Milham M.P., Nugent A.C., Drevets W.C., Dickstein D.S., Leibenluft E., Ernst M.…Pine D.S. Selective reduction in amygdala volume in pediatric anxiety disorders: a voxel-based morphometry investigation. Biol. Psychiatry. 2005;57(9):961–966. doi: 10.1016/j.biopsych.2005.01.038. [DOI] [PubMed] [Google Scholar]
- Mueller S.C., Aouidad A., Gorodetsky E., Goldman D., Pine D.S., Ernst M. Grey matter volume in adolescent anxiety: an impact of the brain-derived neurotropic factor Val66Met polymorphism? J. Am. Acad. Child Adolesc. Psychiatry. 2013;52(2):184–195. doi: 10.1016/j.jaac.2012.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutlu A.K., Schneider M., Debbané M., Badoud D., Eliez S., Schaer M. Sex differences in thickness, and folding developments throughout the cortex. NeuroImage. 2013;82:200–207. doi: 10.1016/j.neuroimage.2013.05.076. [DOI] [PubMed] [Google Scholar]
- Nakao T., Radua J., Rubia K., Mataix-Cols D. Gray matter volume abnormalities in ADHD: voxel-based meta-analysis exploring the effects of age and stimulant medication. Am. J. Psychiatry. 2011;168(11):1154–1163. doi: 10.1176/appi.ajp.2011.11020281. [DOI] [PubMed] [Google Scholar]
- Newman E., Thompson W.K., Bartsch H., Hagler D.J., Chen C.-H., Brown T.T.…Jernigan T.L. Anxiety is related to indices of cortical maturation in typically developing children and adolescents. Brain Struct. Funct. 2015;221(6):3013–3025. doi: 10.1007/s00429-015-1085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble K.G., Houston S.M., Brito N.H., Bartsch H., Kan E., Kuperman J.M.…Sowell E.R. Family income, parental education and brain structure in children and adolescents. Nat. Neurosci. 2015;18(5):773–778. doi: 10.1038/nn.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyewuenyi I.C., Muldoon M.F., Christie I.C., Erickson K.I., Gianaros P.J. Basal ganglia morphology links the metabolic syndrome and depressive symptoms. Physiol. Behav. 2014;123:214–222. doi: 10.1016/j.physbeh.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostby Y., Tamnes C.K., Fjell A.M., Westlye L.T., Due-Tønnessen P., Walhovd K.B. Heterogeneity in subcortical brain development: a structural magnetic resonance imaging study of brain maturation from 8 to 30 years. J. Neurosci. 2009;29(38):11772–11782. doi: 10.1523/JNEUROSCI.1242-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson B.S., Warner V., Bansal R., Zhu H., Hao X., Liu J.…Weissman M.M. Cortical thinning in persons at increased familial risk for major depression. Proc. Natl. Acad. Sci. U. S. A. 2009;106(15):6273–6278. doi: 10.1073/pnas.0805311106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin S., Young C.B., Duan X., Chen T., Supekar K., Menon V. Amygdala subregional structure and intrinsic functional connectivity predicts individual differences in anxiety during early childhood. Biol. Psychiatry. 2014;75(11):892–900. doi: 10.1016/j.biopsych.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raznahan A., Shaw P., Lalonde F., Stockman M., Wallace G.L., Greenstein D.…Giedd J.N. How does your cortex grow? J. Neurosci. 2011;31(19):7174–7177. doi: 10.1523/JNEUROSCI.0054-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds S., Carrey N., Jaworska N., Langevin L.M., Yang X.-R., MacMaster F.P. Cortical thickness in youth with major depressive disorder. BMC Psychiatry. 2014;14:83. doi: 10.1186/1471-244X-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosso I.M., Cintron C.M., Steingard R.J., Renshaw P.F., Young A.D., Yurgelun-Todd D.A. Amygdala and hippocampus volumes in pediatric major depression. Biol. Psychiatry. 2005;57(1):21–26. doi: 10.1016/j.biopsych.2004.10.027. [DOI] [PubMed] [Google Scholar]
- Schilling C., Kühn S., Romanowski A., Schubert F., Kathmann N., Gallinat J. Cortical thickness correlates with impulsiveness in healthy adults. NeuroImage. 2012;59(1):824–830. doi: 10.1016/j.neuroimage.2011.07.058. [DOI] [PubMed] [Google Scholar]
- Schilling C., Kühn S., Paus T., Romanowski A., Banaschewski T., Barbot A.…IMAGEN consortium (www.imagen-europe.com) Cortical thickness of superior frontal cortex predicts impulsiveness and perceptual reasoning in adolescence. Mol. Psychiatry. 2013;18(5):624–630. doi: 10.1038/mp.2012.56. [DOI] [PubMed] [Google Scholar]
- Schmaal L., Hibar D.P., Sämann P.G., Hall G.B., Baune B.T., Jahanshad N.…Veltman D.J. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA major depressive disorder working group. Mol. Psychiatry. 2016 doi: 10.1038/mp.2016.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnack H.G., van Haren N.E.M., Brouwer R.M., Evans A., Durston S., Boomsma D.I.…Hulshoff Pol H.E. Changes in thickness and surface area of the human cortex and their relationship with intelligence. Cereb. Cortex. 2015;25(6):1608–1617. doi: 10.1093/cercor/bht357. [DOI] [PubMed] [Google Scholar]
- Shad M.U., Muddasani S., Rao U. Gray matter differences between healthy and depressed adolescents: a voxel-based morphometry study. J. Child Adolesc. Psychopharmacol. 2012;22(3):190–197. doi: 10.1089/cap.2011.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P., Kabani N.J., Lerch J.P., Eckstrand K., Lenroot R., Gogtay N.…Wise S.P. Neurodevelopmental trajectories of the human cerebral cortex. J. Neurosci. 2008;28(14):3586–3594. doi: 10.1523/JNEUROSCI.5309-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P., Gilliam M., Liverpool M., Weddle C., Malek M., Sharp W.…Giedd J. Cortical development in typically developing children with symptoms of hyperactivity and impulsivity: support for a dimensional view of attention deficit hyperactivity disorder. Am. J. Psychiatry. 2011;168(2):143–151. doi: 10.1176/appi.ajp.2010.10030385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K.S., Tindell A.J., Aldridge J.W., Berridge K.C. Ventral pallidum roles in reward and motivation. Behav. Brain Res. 2009;196(2):155–167. doi: 10.1016/j.bbr.2008.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strawn J.R., John Wegman C., Dominick K.C., Swartz M.S., Wehry A.M., Patino L.R.…Delbello M.P. Cortical surface anatomy in pediatric patients with generalized anxiety disorder. J. Anxiety Disord. 2014;28(7):717–723. doi: 10.1016/j.janxdis.2014.07.012. [DOI] [PubMed] [Google Scholar]
- Strawn J.R., Hamm L., Fitzgerald D.A., Fitzgerald K.D., Monk C.S., Phan K.L. Neurostructural abnormalities in pediatric anxiety disorders. J. Anxiety Disord. 2015;32:81–88. doi: 10.1016/j.janxdis.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschernegg M., Pletzer B., Schwartenbeck P., Ludersdorfer P., Hoffmann U., Kronbichler M. Impulsivity relates to striatal gray matter volumes in humans: evidence from a delay discounting paradigm. Front. Hum. Neurosci. 2015;9 doi: 10.3389/fnhum.2015.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu P.C., Chen L.-F., Hsieh J.-C., Bai Y.-M., Li C.-T., Su T.-P. Regional cortical thinning in patients with major depressive disorder: a surface-based morphometry study. Psychiatry Res. 2012;202(3):206–213. doi: 10.1016/j.pscychresns.2011.07.011. [DOI] [PubMed] [Google Scholar]
- Tu P.C., Kuan Y.H., Li C.T., Su T.P. Structural correlates of trait impulsivity in patients with bipolar disorder and healthy controls: a surface-based morphometry study. Psychol. Med. 2017;47(7):1292–1299. doi: 10.1017/S0033291716003299. [DOI] [PubMed] [Google Scholar]
- Valera E.M., Faraone S.V., Murray K.E., Seidman L.J. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol. Psychiatry. 2007;61(12):1361–1369. doi: 10.1016/j.biopsych.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Vulser H., Lemaitre H., Artiges E., Miranda R., Penttilä J., Struve M.…Stephens D. Subthreshold depression and regional brain volumes in young community adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54(10):832–840. doi: 10.1016/j.jaac.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Deng Y., Fung G., Liu W., Wei X., Jiang X.…Chan R.C.K. Distinct structural neural patterns of trait physical and social anhedonia: evidence from cortical thickness, subcortical volumes and inter-regional correlations. Psychiatry Res. 2014;224(3):184–191. doi: 10.1016/j.pscychresns.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Wenger E., Mårtensson J., Noack H., Bodammer N.C., Kühn S., Schaefer S.…Lövdén M. Comparing manual and automatic segmentation of hippocampal volumes: reliability and validity issues in younger and older brains. Hum. Brain Mapp. 2014;35(8):4236–4248. doi: 10.1002/hbm.22473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside S.P., Lynam D.R. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personal. Individ. Differ. 2001;30(4):669–689. [Google Scholar]
- Whittle S., Lichter R., Dennison M., Vijayakumar N., Schwartz O., Byrne M.L.…Allen N.B. Structural brain development and depression onset during adolescence: a prospective longitudinal study. Am. J. Psychiatr. 2014;171(5):564–571. doi: 10.1176/appi.ajp.2013.13070920. [DOI] [PubMed] [Google Scholar]
- Wierenga L.M., Langen M., Oranje B., Durston S. Unique developmental trajectories of cortical thickness and surface area. NeuroImage. 2014;87:120–126. doi: 10.1016/j.neuroimage.2013.11.010. [DOI] [PubMed] [Google Scholar]
- Winkler A.M., Kochunov P., Blangero J., Almasy L., Zilles K., Fox P.T.…Glahn D.C. Cortical thickness or Grey matter volume? The importance of selecting the phenotype for imaging genetics studies. NeuroImage. 2010;53(3):1135–1146. doi: 10.1016/j.neuroimage.2009.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou D., Lebel C., Treit S., Evans A., Beaulieu C. Accelerated longitudinal cortical thinning in adolescence. NeuroImage. 2015;104:138–145. doi: 10.1016/j.neuroimage.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Zisner A., Beauchaine T.P. Neural substrates of trait impulsivity, anhedonia, and irritability: mechanisms of heterotypic comorbidity between externalizing disorders and unipolar depression. Dev. Psychopathol. 2016;28(4pt1):1177–1208. doi: 10.1017/S0954579416000754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material