Abstract
Background
Substance use disorders are understood as a chronically relapsing condition that is difficult to treat. However, in recent years there have been promising developments in the treatment of substance use disorders, specifically with interventions based on mindfulness and Acceptance and Commitment Therapy. Little research has examined whether these types of interventions may positively impact residential substance use treatment outcomes.
Objectives
Thus, in the current study we developed and examined, in a randomized controlled trial (RCT), a 4-week, 8-session, adjunctive Mindfulness and Acceptance group therapy for patients in residential substance use treatment. Our primary outcomes were substance use cravings, psychological flexibility, and dispositional mindfulness at treatment discharge.
Methods
Patients (N = 117) from a private residential substance use facility were randomized to receive the adjunctive Mindfulness and Acceptance group or treatment-as-usual (TAU). Patients were assessed at treatment intake and at discharge from the 28-30 day residential program.
Results
Although treatment groups did not statistically differ at discharge on any primary outcome, small effect sizes favored the Mindfulness and Acceptance group on cravings and psychological flexibility.
Conclusions/Importance
Continued research is needed to determine whether the addition of mindfulness and acceptance-based interventions improve outcomes long-term following residential substance use treatment.
Keywords: Mindfulness, substance use, acceptance, randomized controlled trial
Substance use is an endemic problem throughout the United States and the world (Grant et al., 2015; Lundin, Hallgren, Forsman, & Forsell, 2015), and substance use disorders (SUD) are understood as chronically relapsing conditions that are difficult to treat (McLellan, Lewis, O’Brien, & Kleber, 2000; Walitzer & Dearing, 2006). Recently, however, there have been promising developments in the treatment of SUDs utilizing approaches that focus on enhancing acceptance and mindfulness. Specifically, treatments based on Acceptance and Commitment Therapy (ACT; Hayes, Strosahl, & Wilson, 2012) and Mindfulness-Based Relapse Prevention (MBRP; Bowen, Chawla, & Marlatt, 2011) have demonstrated effectiveness in reducing substance use and preventing relapse among individuals seeking outpatient substance use treatment (Bowen et al., 2014; Hayes et al., 2004).
Yet, there is a dearth of research on whether these approaches can be effectively implemented in residential substance use treatment programs. Thus, in the current study we conducted a randomized controlled trial (RCT) of a newly developed, adjunctive, 4-week group intervention that combined aspects of ACT and MBRP and examined whether this intervention reduced substance use cravings, increased psychological flexibility, and increased dispositional mindfulness at discharge from treatment to a greater degree than treatment-as-usual (TAU) among patients in residential substance use treatment.
Mindfulness-Based Treatments for Substance Use
There has been a growing body of research in recent years on the potential usefulness of mindfulness-based interventions in reducing substance use. Mindfulness has been defined as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally” (Kabat-Zinn, 1994, p. 4). This involves bringing attention to present moment experiences, including emotions, thoughts, and physical sensations, in a way that fosters curiosity and nonjudgment of experiences, allowing whatever arises to be exactly as it is (Segal, Williams, & Teasdale, 2012). With mindfulness, unpleasant emotions, thoughts, and sensations are not avoided, and pleasant emotions, thoughts, and sensations are not clung to or held with attachment. In essence, all experiences are viewed as ephemeral and, thus, reactive, automatic behavior when faced with unpleasant (or pleasant) experiences is reduced. The most well-known mindfulness-based program, Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990), is an 8-week group program designed to enhance mindfulness with ample empirical support (Baer, 2003).
Mindfulness-based protocols have been developed for substance use, most notably Mindfulness-Based Relapse Prevention (MBRP; Bowen et al., 2011). MBRP is an 8-week, outpatient group intervention for individuals with substance use disorders who have stopped using substances. MBRP draws on components from MBSR and traditional cognitive-behavioral relapse prevention (RP; Marlatt & Gordon, 1985). Two randomized controlled trials have demonstrated the effectiveness of MBRP in reducing substance use following treatment (Bowen et al., 2009; 2014), with individuals in MBRP having better treatment outcomes than individuals in traditional 12-step outpatient programming (Bowen et al., 2009) and individuals in traditional RP groups (Bowen et al., 2014). Additional mindfulness-based treatments for substance use, which are largely modeled after, or are similar to, MBRP, have demonstrated promising outcomes (Chiessa & Serretti, 2014, Garland et al., 2014; Zgierska et al., 2009).
Although there are many proposed mechanisms of change in mindfulness-based interventions (see Baer, 2003), it has been proposed that decreases in drug use cravings may be partially responsible for the beneficial outcomes of mindfulness-based interventions (Witwiewitz, Lustyk, & Bowen, 2012). Substance use cravings can be defined as “the subjective experience of an urge or desire to use substances” (Witkiewitz, Bowen, Douglas, & Hsu, 2013, p. 1564). Indeed, not only do mindfulness-based treatments for substance use decrease cravings (Bowen et al., 2009; 2014), but reduced cravings predict outcomes among individuals in mindfulness-based treatment (Witkiewitz & Bowen, 2010).
Another proposed mechanism of change in response to mindfulness-based interventions is increased dispositional mindfulness. Dispositional mindfulness is considered a naturally occurring characteristic, and can be assessed by asking individuals to report on their tendencies to have sustained awareness and attention to what occurs in the present moment of their everyday life (Bowen & Enkema, 2014; Brown & Ryan, 2003). In essence, high dispositional mindfulness is consistent with the “way of being” that is sought through mindfulness meditation practice. Indeed, prior studies on mindfulness-based interventions show increases in dispositional mindfulness following treatment (Baer, Carmody, & Hunsinger, 2012), including research on MBRP (Bowen et al., 2009). Importantly, higher levels of dispositional mindfulness is associated with lower levels of substance use (Bowen & Enkema, 2014). Thus, it will be important for studies on mindfulness-based treatments for substance use to continue to investigate their impact on substance use cravings and dispositional mindfulness.
Acceptance-Based Treatments for Substance Use
Recent research has begun to investigate the impact of acceptance-based approaches on substance use. Specifically, treatments based on Acceptance and Commitment Therapy (ACT) have been developed for substance use. ACT, considered a “third wave” behavioral therapy, attempts to increase psychological flexibility through targeting acceptance, values, cognitive fusion, committed action, self-as-context, and present moment processes (Hayes et al., 2012). Psychological flexibility can be defined as “the ability to contact the present moment more fully as a conscious human being, and to change or persist in behavior when doing so serves valued ends” (Hayes, Luoma, Bond, Masuda, & Lillis, 2006, p. 6). Higher psychological flexibility is theoretically and empirically associated with better mental health outcomes, including reduced substance use, and is one mechanism of action responsible for positive outcomes produced by ACT (Hayes et al., 2012).
As related to substance use, Hayes and colleagues (2004), demonstrated that patients who were receiving methadone maintenance had better outcomes (i.e., reduced substance use) following treatment when they received 16-weeks of individual and group-based ACT, relative to when patients received 12-step facilitation therapy. Luoma, Kohlenberg, Hayes, and Fletcher (2012) demonstrated that three 2-hour group sessions that were based on ACT and targeted shame resulted in fewer substance use days and increased treatment utilization 4-months following residential treatment relative to patients who did not receive the adjunctive ACT group intervention. A recent meta-analysis of 10 RCTs of ACT for substance use demonstrated small to medium effects favoring ACT over other treatments for substance use (Lee, An, Levin, & Twohig, 2015).
Integrating Mindfulness and Acceptance for Residential Treatment
Based on prior literature demonstrating positive outcomes with mindfulness-based interventions for substance use with outpatient samples, and initial research with ACT-based interventions for substance use with residential samples, we developed an integrated, group-based, adjunctive intervention targeting mindfulness and psychological flexibility for individuals in residential substance use treatment. Because mindfulness-based and ACT interventions share many similarities (McCracken & Vowles, 2014), the integration of these two approaches is warranted. Indeed, a small pilot study for substance use has previously integrated these approaches. Vieten, Astin, Buscemi, and Galloway (2010), in a sample of individuals with alcohol dependence who had quit drinking, demonstrated that an 8-week, outpatient, integrated acceptance and mindfulness group resulted in improvements in psychological well-being and reduced craving severity from pre-to-post intervention.
There are many important differences between outpatient and residential substance use treatment programs that may make implementing MBRP, or other mindfulness and acceptance-based protocols, within residential programs difficult without modifications. For instance, MBRP was developed as a closed group protocol, as each session is believed to build upon the previous session. Closed groups would be difficult to implement in residential substance abuse programs where admission is rolling and continuous. Thus, open-enrollment protocols would likely need to be developed for residential settings. Open-enrollment protocols could enhance mindfulness training, as new patients will have the opportunity to learn from more experienced patients (Bowen et al., 2010). However, we are unaware of any research that has examined open-enrollment mindfulness and acceptance groups for residential substance use patients.
Current Study
In the current study, we developed a 4-week, 8-session, open and rolling Mindfulness and Acceptance group intervention for substance use that drew heavily from MBRP and ACT. We then conducted a randomized controlled trial with men and women in residential substance use treatment by randomly assigning patients to receive treatment-as-usual or treatment-as-usual plus adjunctive Mindfulness and Acceptance group. We hypothesized that individuals in the Mindfulness and Acceptance group would report reduced substance use cravings, increased psychological flexibility related to substance use, and increased dispositional mindfulness relative to individuals who received treatment-as-usual (TAU) at discharge from residential treatment.
Method
Trial Design
We conducted a RCT in which individuals in residential substance use treatment were randomly assigned to standard substance use treatment (i.e., TAU) or TAU plus a Mindfulness and Acceptance group. Participants were assessed at baseline (i.e., after medical detoxification and prior to the start of treatment) and at treatment discharge. The primary outcomes were substance use cravings, dispositional mindfulness, and psychological flexibility. We expected the Mindfulness and Acceptance group to evidence superior outcomes relative to TAU at treatment discharge.
Participants
Participants were 117 men and women, aged 18 years and older, who were in a 28-30 day residential substance use treatment program in the Southeastern United States. In order to be included in the study, participants had to be 18 years of age or older and cleared from withdrawal by medical staff. Participants were excluded if they screened positive for psychotic symptoms on the Psychiatric Diagnostic Screening Questionnaire (Zimmerman, 2002), which is administered by the treatment facility to all patients, or if they were deemed cognitively impaired (e.g., dementia, Alzheimer’s) by a physician during their initial medical assessment upon admission to the treatment facility. Table 1 displays diagnostic and demographic information for the sample.
Table 1.
Demographic and Diagnostic Information for Study Sample.
| Total (N = 117) | Mindfulness & Acceptance Group (n = 64) | TAU (n = 53) | ||
|---|---|---|---|---|
| Gender | χ2 =5.65* | |||
| Male | n = 87 | n = 42 | n = 45 | |
| Female | n = 30 | n = 22 | n = 8 | |
| Age, M | 41.27 (SD = 10.68) |
42.47 (SD = 10.54) |
39.83 (SD = 10.73) |
t = 1.33 |
| Annual Income, M | 67645.08 (SD = 49718.61) |
59950.81 (SD = 42584.20) |
76848.03 (SD = 56151.56) |
t = .21 |
| Years of Education, M | 14.19 (SD = 2.42) | 14.23 (SD = 2.20) | 14.14 (SD = 2.68) | t = 1.81 |
| Race | χ2 =5.04 | |||
| Caucasian | 92.2% | 87.6% | 96.2% | |
| African American | 3.4% | 4.7% | 3.8% | |
| Hispanic | 1.7% | 3.1% | 0% | |
| Asian American | 1.7% | 1.5% | 0% | |
| Indian | .9% | 3.1% | 0% | |
| Prior Substance Use Treatment | 41% | 35.9% | 47.1% | χ2 = 1.51 |
| Diagnosis | χ2 = 12.82 | |||
| Alcohol Dependence |
58.1% | 54.7% | 62.3% | |
| Opioid Dependence |
17.1% | 20.3% | 13.2% | |
| Polysubstance Dependence |
14.5% | 18.8% | 9.4% | |
| Alcohol Abuse | 3.4% | 4.7% | 1.9% | |
| Sedative/Hypnotic/Anxiolytic Dependence |
.9% | 0% | 1.9% | |
| Cocaine Dependence | .9% | 1.6% | 0% | |
| Cannabis Dependence | .9% | 0% | 1.9% | |
| Amphetamine Dependence | .9% | 0% | 1.9% | |
| Cannabis Abuse | .9% | 0% | 1.9% | |
| Hallucinogen Abuse | .9% | 0% | 1.9% | |
| Cocaine Abuse | .9% | 0% | 1.9% | |
| Amphetamine Abuse | .9% | 0% | 1.9% |
p < .05
Procedure
Participants were recruited from a residential treatment program offered through a private substance use treatment facility that provides residential and outpatient services. The majority of patients at this treatment facility are mandated to treatment from their employer (e.g., 50%) and a small minority are mandated to treatment for legal reasons (e.g., 2-3%). Upon admission to the treatment facility, all patients are screened for substance use withdrawal by a general physician and, if necessary, receive medical detoxification. Patients who were not at risk for substance use withdrawal, and patients who successfully completed medical detoxification, were approached individually by trained undergraduate and graduate student research assistants to request participation in the current study. All patients were informed that their participation was voluntary, that all information they provided would be kept confidential from the substance use treatment facility (with the exception of their group attendance in the Mindfulness and Acceptance condition), and that they could withdraw from the study at any time without negatively impacting their treatment at the facility. After a description of the study, interested patients completed an informed consent approved by the Institutional Review Board of the University of Tennessee. Next, they completed a baseline packet of self-report measures, and were then randomized into a treatment condition. Aside from the newly developed Mindfulness and Acceptance group (discussed below), patients in both treatment conditions received identical treatment services, although there was some individual variability across treatment (i.e., some participants may have received couples therapy; participants without a spouse/significant other may have received family therapy with a brother/sister). Participants received no compensation for study participation. Recruitment occurred from August, 2012 to January, 2013. Of the 139 men and women screened for participation, 2 failed to meet inclusion criteria and 20 declined participation. Thus, 117 men and women constituted the intent-to-treat sample (see Figure 1).
Figure 1.
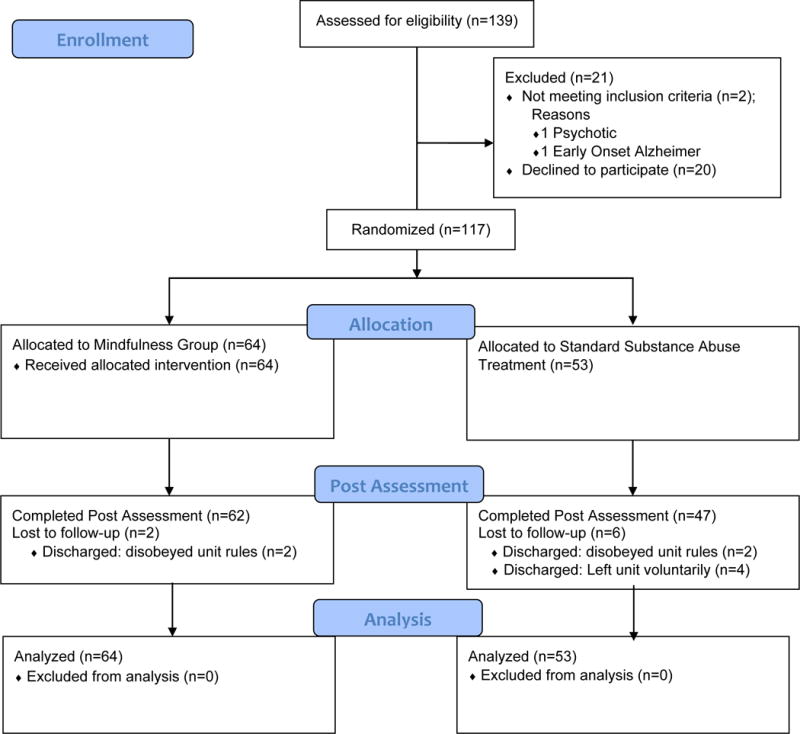
CONSORT Flow Diagram
Substance use diagnoses for patients were based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision (DSM-IV-TR) criteria (American Psychiatric Association, 2000) and determined through consultation and the consensus of treatment facility team members (e.g., psychologist, psychiatrist, general physician, and substance abuse counselors). Diagnoses were based on DSM-IV-TR criteria as the study was conducted prior to the publication of DSM-V. Patients provided consent for this information to be obtained from their medical records for use in the current study.
Randomization
Assignment to treatment conditions was based on a computerized random number generator. Of the 117 participants, 64 were assigned to the Mindfulness and Acceptance condition and 53 were assigned to TAU. After completing informed consent and a baseline questionnaire packet, research assistants randomly assigned participants to treatment conditions. Because research assistants were often involved in the scheduling and randomization of participants, they were not blind to treatment condition.
Interventions
Standard Substance Use Treatment (Treatment-As-Usual; TAU)
The TAU condition consisted of a 28-30 day residential substance use treatment program that is largely guided by the traditional 12-step model (i.e., abstinence-based treatment guided by Alcoholics Anonymous and Narcotics Anonymous [AA/NA]). TAU consisted of varied therapeutic activities each day, including process-oriented groups, AA/NA meetings, coping skills groups, family therapy, exercise groups, acupuncture (optional), and individual meetings with counselors. There was no structured protocol or planned activities for TAU groups, as therapists were allowed to discuss topics based on the needs of each group/patient. A single therapist conducted TAU activities, and the number of patients in each TAU group could vary from 1 (i.e., in individual meetings) to approximately 10 (i.e., in coping skills groups). TAU did not contain any group or individual therapy focused on mindfulness, although the concept of acceptance was discussed in various contexts in TAU (e.g., AA/NA meetings, process-oriented groups).
Mindfulness and Acceptance Group
This group was delivered in 8 twice weekly, 1.5 hour, group sessions, which were based on MBRP (Bowen et al., 2009; 2014), MBSR (Kabat-Zinn, 1990), and Acceptance and Commitment Therapy (Hayes et al., 2012). That is, these established interventions informed our selection of topics, activities, discussion points, and interactions with participants in the newly developed group protocol. Each session had a central theme (e.g., “Mindfulness in Daily Life”), consisting of experiential exercises, and included group discussions on how the material covered related to substance use and relapse prevention. Table 2 displays an outline of each session. Each session began with a 20 to 30 minute guided meditation and was followed by a number of additional, briefer, experiential exercises and group discussions about the roles of mindfulness and acceptance in relapse prevention. Participants were assigned daily exercises to practice between group sessions and were provided with a CD player that contained the guided meditations covered in groups for continued personal practice. Due to the nature of the treatment facility where the study was conducted, the Mindfulness and Acceptance group was open and rolling; thus patients began the group at various sessions. Importantly, no participant completed the same group twice, and all participants had the opportunity to attend all 8 groups.
Table 2.
Mindfulness and Acceptance Group Session Outline.
| Session Theme | Topics Covered | Experiential Exercises |
|---|---|---|
| 1. Automatic Pilot and Control is the Problem | Discussion of “automatic pilot” mode of being and attempts to “control” cravings and risk for relapse. Mindfulness and acceptance as a method to counter automatic pilot and control. | Body scan; polygraph metaphor; jelly donut metaphor |
| 2. Acceptance | How acceptance of “things we cannot change”, with compassion and kindness, can aid in the process of recovery | Mindful movement; Chinese handcuffs; tug-of-war with a monster; body scan |
| 3. Awareness of Triggers and Craving | How mindfulness can help us to become more aware of triggers/cravings; mindfulness as a way to reduce reactive behavior | Mindful movement; walking down the street; SOBER space; urge surfing; mountain mediation |
| 4. Defusion | How thoughts are related to substance use and how we can “defuse” from them | Sitting meditation; “milk” exercise; leaves on a stream |
| 5. High Risk Situations | High-risk situations for substance use are discussed and mindful awareness as an alternative to reactive behaviors | Sitting meditation; SOBER space; quicksand metaphor; walking meditation |
| 6. Values | Defining and identifying values and elucidating how mindfulness and acceptance can help us to live our lives consistent with our values | Compassion meditation; passengers on the bus; funeral metaphor; mountain meditation |
| 7. Kindness and Compassion | Introduction to kindness and compassion toward ourselves and others; how compassion can reduce risk for relapse | Body scan; kindness and compassion meditation; daily activities worksheet |
| 8. Mindfulness and Acceptance in Daily Life | Eliciting ways in which mindfulness and acceptance can be integrated into daily life | Sitting meditation; raisin exercise; SOBER space |
Participants in the Mindfulness and Acceptance group attended these group sessions in place of regularly scheduled process-oriented groups (which TAU participants attended) to ensure that both treatment conditions were matched for treatment contact time. Participants were informed of when their Mindfulness and Acceptance groups would occur on their daily schedules, which were posted by the treatment facility at the beginning of each day of treatment. Consistent with the treatment facility policies, participants were allowed to miss groups if they had a previously scheduled doctor’s appointment outside of the treatment facility or family/couples therapy during the time of the group. This policy also applied to participants in TAU. Participants in the Mindfulness and Acceptance condition were not allowed to miss a group to attend a TAU group. All Mindfulness and Acceptance groups were audio recorded.
Therapists
Each Mindfulness and Acceptance group was facilitated by one Master’s level graduate student therapist in Clinical Psychology. This therapist had extensive training in mindfulness-based, acceptance and commitment, and substance use treatments, as well as a personal daily meditation practice, including attendance of intensive mindfulness meditation retreats. The therapist received weekly supervision throughout the study from a licensed psychologist with extensive experience treating substance use. Therapists facilitating TAU were primarily licensed Chemical Dependency Counselors with varying levels of education, training, and experience.
Treatment Adherence
Therapist adherence to the Mindfulness and Acceptance group protocol was assessed with a Treatment Components Checklist (TCC) created specifically for the current study. A TCC was created for each specific group and two trained research assistants independently coded a subsample of sessions for therapist adherence on the delivery of treatment activities for each session. One research assistant coded 20% of all Mindfulness and Acceptance sessions randomly selected across all sessions, and the two research assistants independently coded 3 common audio-recorded sessions to determine inter-rater reliability. The percentage of therapist adherence to the treatment activities recommended per session, as detailed in the study protocol, was 97.8%. Study raters agreed on 100% of the tapes they both rated for therapist adherence.
Measures
Alcohol and Drug Cravings
The Penn Alcohol Craving Scale (PACS; Flannery, Volpicelli, & Pettinati, 1999) was utilized to assess alcohol cravings and was adapted to also assess drug cravings, consistent with prior research (e.g., Bowen et al., 2009). The PACS includes 5 items that asks about the intensity, frequency, and duration of craving, and overall intensity of alcohol cravings during the previous week. All items are rated on a 6-point scale, with higher scores reflecting higher self-reported cravings. This measure was administered twice at each assessment: once for alcohol and once for drugs. In the current sample the internal consistencies were .95 and .91 for alcohol cravings and .96 and .92 for drug cravings at baseline and discharge, respectively.
Dispositional Mindfulness
The 39-item Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006) was used to assess dispositional mindfulness at baseline and discharge. The FFMQ examines five different aspects of dispositional mindfulness: Observation of Experience (“I pay attention to how my emotions affect my thoughts and behavior”), Describing with Words (“My natural tendency is to put my experiences into words”), Acting with Awareness (“I rush through activities without being really attentive to them” [reverse scored]), Nonjudging of Experience (“I disapprove of myself when I have irrational ideas” [reverse scored]), and Nonreactivity to Experience (“When I have distressing thoughts or images, I just notice them and let them go”). Patients were asked to indicate their opinion of how true each item was of themselves on a 5-point scale (1 = never or very rarely true; 5 = very often or always true) and a total score was obtained by summing all items. Higher scores on the FFMQ reflect higher dispositional mindfulness. The FFMQ was developed based on a factor analysis of mindfulness questionnaires and has demonstrated good psychometric properties (Christopher, Neuser, Michael, & Baitmangalkar, 2012). The internal consistencies for the FFMQ total scores in the current study, for baseline and discharge, were .92 and .93.
Psychological Flexibility – Substance Abuse
The 18-item Acceptance and Action Questionnaire, Substance Abuse version (Luoma et al., 2011) was used to measure psychological flexibility in relation to substance abuse. The AAQ-SA, based largely on the well validated Acceptance and Action Questionnaire (AAQ; Hayes et al., 2004), was developed to assess psychological flexibility as it related to substance misuse. All items were rated on a 7-point scale (1 = never true; 7 = always true) and higher scores reflect greater psychological flexibility specific to substance use urges, cravings, and thoughts. Example items include “My urges and cravings to use substances get in the way of my success [reverse scored]” and “Having some worries about substance use will not prevent me from living a fulfilling life.” The psychometric properties of the AAQ-SA have been established in substance use treatment samples (Luoma et al., 2011). The internal consistency of the AAQ-SA in the current sample was .85 and .83 at baseline and discharge, respectively.
Importance of Mindfulness and Acceptance Group
At treatment discharge, patients who participated in the Mindfulness and Acceptance group were asked to rate, on a 5-point scale (1 = not at all important; 5 = very important), how important they thought the group was in supporting their treatment.
Data Analytic Strategy
Differences between treatment groups on substance use cravings and dispositional mindfulness at treatment discharge were examined in several ways. First, a multivariate analysis of variance (MANOVA) was used to compare groups at discharge (and baseline) on the variables of interest. In addition, because our sample size was relatively small, we calculated effect size differences between groups at discharge on cravings and dispositional mindfulness. Effect sizes (d) were calculated by comparing the mean scores of treatment groups at discharge, divided by their pooled standard deviations (Cohen, 1988). As detailed by Cohen (1988), a small effect size is equal to a d of .20, a medium effect size is equal to a d of .50, and a large effect size is equal to a d of .80. Lastly, bivariate correlations between the single item assessing patients’ perception of the importance of the Mindfulness and Acceptance group and outcome variables were examined.
Results
All analyses were conducted in SPSS version 18.0. As displayed in Table 1, treatment groups did not differ on substance use diagnoses and demographic characteristics, with one exception. The Mindfulness and Acceptance group had significantly more women than TAU. The mean number of sessions attended by participants in the Mindfulness and Acceptance condition was 5.40 (SD = 1.52) and the average number of participants in each group was 6.46 (SD = 2.32).
Differences between treatment conditions on substance use cravings and dispositional mindfulness are presented in Table 3. Results from the MANOVA demonstrated no significant differences between treatment groups on any variable at discharge from the treatment facility (F = .37, p > .05; Wilk’s Lambda = .97)1. Effect size differences between groups were small, with the Mindfulness and Acceptance group reporting lower drug cravings (d = .23) and higher psychological flexibility related to substance use (d = .20) relative to TAU.
Table 3.
Differences between groups on study variables.
| Mindfulness and Acceptance Group | Treatment as usual | F | d | |||
|---|---|---|---|---|---|---|
| Variable, M (SD) | Baseline (n = 64) |
Discharge (n = 62) |
Baseline (n = 53) |
Discharge (n = 47) |
||
| Alcohol Craving | 7.52 (8.71) | 4.16 (4.49) | 8.52 (9.00) | 3.85 (4.22) | .09 | .07 |
| Drug Craving | 8.08 (9.61) | 2.42 (4.52) | 8.66 (8.86) | 3.47 (4.44) | .14 | .23 |
| FFMQ Total | 117.01 (26.13) | 126.13 (24.75) | 118.67 (15.69) | 127.94 (18.37) | .01 | .08 |
| AAQ-SA | 81.74 (18.95) | 100.14 (15.62) | 82.47 (14.75) | 97.17 (13.38) | .91 | .20 |
Note: F values and effect sizes reflect differences between groups at discharge. Groups did not significantly differ on variables at baseline. FFMQ = Five facet mindfulness questionnaire; AAQ-SA = Acceptance and action questionnaire – substance abuse version.
Finally, bivariate correlations, for the patients assigned to the Mindfulness and Acceptance group only, demonstrated an inverse relationship between drug cravings at discharge and the perceived importance of this group (r = -.50, p < .001) and a positive association with psychological flexibility (r = .34, p < .05). That is, as the perceived importance of the group increased, drug cravings decreased and psychological flexibility related to substance use increased. Perceived importance was not significantly associated with the number of Mindfulness and Acceptance groups attended. The number of treatment groups attended was not associated with any variables at discharge. No other correlations were significant.
Discussion
Mindfulness and Acceptance-based interventions have received increased research attention in recent years among substance use populations (Bowen et al., 2014; Luoma et al., 2012). However, the majority of this prior research has examined these treatments among individuals in outpatient settings (e.g., Bowen et al., 2014; Hayes et al., 2004), and thus it is unclear whether these approaches can be successfully used for individuals in residential substance use treatment. Therefore, we conducted a preliminary randomized controlled trial of an adjunctive Mindfulness and Acceptance group for individuals in residential substance use treatment.
Overall, findings did not demonstrate statistically significant differences between treatment groups at the conclusion of residential treatment. That is, both TAU and the Mindfulness and Acceptance group showed similar improvement in study variables across the course of treatment. There are a number of possible explanations for these non-significant findings. First, it is possible that the addition of the Mindfulness and Acceptance group was not powerful enough to improve upon an intensive, 28-30 day residential treatment program. That is, the effects of the Mindfulness and Acceptance group might have been watered down within a residential setting where patients receive intensive treatment. Additionally, we cannot rule out the possibility that individuals in the Mindfulness and Acceptance group shared their experiences in the adjunctive treatment with individuals in TAU, as they were in the same residential treatment program simultaneously. Because participants were actively using substances upon admission to treatment, the lack of significant differences between groups may have also reflected the beneficial effects of abstinence.
It is also possible that treatment effects between groups would not emerge until after the conclusion of treatment. For instance, in their RCT of an ACT-based shame intervention, Louma and colleagues (2012) found that individuals in the ACT condition did not have better outcomes at discharge from treatment, but did have better outcomes 4-months following treatment relative to individuals who did not receive the shame-based intervention. This is certainly plausible in our case, as the impact of the Mindfulness and Acceptance group may be enhanced over time. For instance, it is possible that patients in the Mindfulness and Acceptance group may respond differently to cravings post-treatment (i.e., with acceptance and awareness) relative to TAU, which may reduce the likelihood that cravings will lead to substance use. Longitudinal research is needed to examine these questions.
It is also possible that one reason treatment groups did not significantly differ on dispositional mindfulness at discharge from treatment is due to the method in which mindfulness was assessed. There is a debate in the field on the best way to assess dispositional mindfulness (Sauer et al., 2013), with researchers raising several concerns in the use of self-report measures as the primary method to capture this complex construct (Grossman, 2008). A recent study demonstrated that individuals randomized to a mindfulness-intervention or a health intervention (which did not discuss mindfulness) both had increases in dispositional mindfulness at the conclusion of the study and did not differ from each other on dispositional mindfulness (Goldberg et al., in press). However, other mindfulness-based studies have demonstrated significant differences on dispositional mindfulness between control conditions and mindfulness-based conditions at the conclusion of treatment (e.g., Bowen et al., 2009). Thus, continued research is needed in this area.
It is worth noting that findings demonstrated a small effect size at discharge between treatment conditions on drug use cravings and psychological flexibility. Specifically, the Mindfulness and Acceptance group reported fewer drug cravings and higher psychological flexibility related to substance use than TAU. Prior mindfulness-based interventions for individuals in outpatient substance use treatment have demonstrated reduced cravings relative to TAU (Bowen et al., 2009). Because mindfulness-based interventions attempt to increase, in a non-judgmental and non-reactive way, awareness of emotions, sensations, and thoughts, it is possible that cravings for substances are allowed to naturally arise and fall among individuals who receive mindfulness training. Over time, this may lead to habituation to cravings, as they are no longer being avoided or attempt to be controlled (Bowen et al., 2009; 2014). Related to psychological flexibility, this is one of the primary mechanisms by which ACT-based interventions are hypothesized to produce beneficial outcomes (Hayes et al., 2012).
Limitations
There are several notable limitations of the current study. First, there were more women in the Mindfulness and Acceptance group than TAU, and the overall number of women in the study was small. Future research should therefore include a larger number of women. Moreover, our sample size in the study was small, which limited our statistical power to detect significant differences between groups. Second, we were unable to examine long-term follow-up data on our sample, and future research should attempt to gather objective indicators of substance use (i.e., drug screens) to identify group differences following treatment. Third, only one facilitator conducted the Mindfulness and Acceptance group. Traditionally, MBRP consists of two facilitators, and there is some research to suggest that two facilitators produce better treatment outcomes than one group therapy facilitator (e.g., Kivlighan, London, & Miles, 2012). Thus, future research should compare the outcomes of mindfulness- and acceptance-based groups for substance use with one or two facilitators. Fourth, patients in the Mindfulness and Acceptance group attended, on average, 5.4 of the 8 sessions. Patients were allowed to miss this group if they had a doctor’s appointment outside of the treatment facility or a family therapy session scheduled during the time of the group. Future research should attempt to increase the number of sessions attended, as this may impact outcomes. Fifth, we did not track how many TAU sessions participants attended, although the maximum number of TAU sessions one could attend was 8, consistent with the Mindfulness and Acceptance condition. Sixth, because TAU groups were unstructured and did not have a protocol, we did not assess therapist adherence in these groups. Seventh, we did not assess for drug use during treatment, although the treatment facility where the study was conducted does conduct random urine drug screens and no patients in our study were removed from the facility because of failed drug screens. However, we did not collect urine drug screens from participants as part of our study and future research should collect these.
Although the use of an open, rolling Mindfulness and Acceptance group in this study was necessary due to the open, rolling admissions procedure of the treatment facility where the study was conducted, the majority of mindfulness-based and acceptance-based group studies have occurred with closed groups (e.g., Bowen et al., 2014; Luoma et al., 2012). Thus, it is possible that there are differences between open and closed mindfulness-based groups, as closed groups are intended to build upon each other (Bowen et al., 2011), and future research should explore this possibility. Because patients in TAU and the Mindfulness and Acceptance group were in treatment at the same time, in the same residential program, it is possible that patients discussed their respective interventions with each other. Thus, it is possible that patients in TAU were exposed to material presented in the Mindfulness and Acceptance group, although we did not collect this information from TAU participants. Researchers should attempt to address this concern in future studies, such as by assigning cohorts of patients to receive TAU or the adjunctive intervention, as has been done in previous research (e.g., Luoma et al., 2012). Finally, as with any study that collects data on sensitive and personal information, social desirability may have impacted study findings and future research should consider this when assessing outcomes.
Conclusion
In summary, we conducted a randomized controlled trial of an adjunctive Mindfulness and Acceptance group for individuals in residential substance use treatment. Although treatment groups did not significantly differ on study outcomes at discharge from treatment, findings showed small effect size differences at discharge, in favor of the Mindfulness and Acceptance group, for reduced drug cravings and increased psychological flexibility. Moreover, among individuals who received the Mindfulness and Acceptance group, the perceived importance of the group was associated with lower drug cravings and greater psychological flexibility related to substance use at discharge. In all, our study provides the first evidence for the ability to effectively implement a comprehensive Mindfulness and Acceptance program in a residential substance use treatment setting. Continued research is needed to determine the best approach to implementing mindfulness and acceptance-based interventions for residential substance use patients.
Acknowledgments
This work was supported, in part, by grants F31AA020131 and K24AA019707 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) awarded to the first and last authors, respectively. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Footnotes
We also compared groups on all five subscales of the FFMQ, and groups did not differ significantly at baseline or discharge on any subscale.
Conflict of interest: The first and last authors receive consulting compensation from Cornerstone of Recovery.
References
- American Psychiatric Association. Diagnostic and statistical manual-text revision (DSM-IV-TR, 2000) Washington, DC: Author; 2000. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical psychology: Science and practice. 2003;10:125–143. [Google Scholar]
- Baer RA, Carmody J, Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness‐based stress reduction program. Journal of Clinical Psychology. 2012;68:755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-based relapse prevention for addictive behaviors: A clinician’s guide. New York, NY: Guilford Press; 2011. [Google Scholar]
- Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: Findings from a clinical sample. Addictive behaviors. 2014;39:532–537. doi: 10.1016/j.addbeh.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer ME, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry. 2014;71:547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse. 2014;49:492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Christopher MS, Neuser NJ, Michael PG, Baitmangalkar A. Exploring the psychometric properties of the five facet mindfulness questionnaire. Mindfulness. 2012;3(2):124–131. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn alcohol craving scale. Alcoholism: Clinical and Experimental Research. 1999;23:1289–1295. [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82(3):448–459. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Wielgosz J, Dahl C, Schuyler B, MacCoon DS, Rosenkranz M, Davidson RJ. Does the Five Facet Mindfulness Questionnaire Measure What We Think It Does? Construct Validity Evidence From an Active Controlled Randomized Clinical Trial. Psychological Assessment. doi: 10.1037/pas0000233. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Hasin DS. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P. On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research. 2008;64:405–408. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT. Measuring experiential avoidance: A preliminary test of a working model. The psychological record. 2004;54(4):553–578. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Bissett R, Piasecki M, Batten SV, Gregg J. A preliminary trial of twelve-step facilitation and acceptance and commitment therapy with polysubstance-abusing methadone-maintained opiate addicts. Behavior Therapy. 2004;35(4):667–688. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: The process and practice of mindful change. Guilford Press; 2012. [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of your Mind to Face Stress, Pain and Illness. New York: Dell Publishing; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are. New York: Hyperion; 1994. [Google Scholar]
- Kivlighan DM, Jr, London K, Miles JR. Are two heads better than one? The relationship between number of group leaders and group members, and group climate and group member benefit from therapy. Group Dynamics: Theory, Research, and Practice. 2012;16:1–13. [Google Scholar]
- Lee EB, An W, Levin ME, Twohig MP. An initial meta-analysis of acceptance and commitment therapy for treating substance use disorders. Drug and Alcohol Dependence. 2015;155:1–7. doi: 10.1016/j.drugalcdep.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. Journal of Studies on Alcohol and Drugs. 2015;76:773–780. doi: 10.15288/jsad.2015.76.773. [DOI] [PubMed] [Google Scholar]
- Luoma J, Drake CE, Kohlenberg BS, Hayes SC. Substance abuse and psychological flexibility: The development of a new measure. Addiction Research & Theory. 2011;19(1):3–13. [Google Scholar]
- Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and steady wins the race: A randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. Journal of Consulting and Clinical Psychology. 2012;80:43–53. doi: 10.1037/a0026070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention: Maintenance strategies in addictive behaviour change. New York, NY: Guilford; 1985. [Google Scholar]
- McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. American Psychologist. 2014;69:178–187. doi: 10.1037/a0035623. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O‘Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Sauer S, Walach H, Schmidt S, Hinterberger T, Lynch S, Büssing A, Kohls N. Assessment of mindfulness: Review on state of the art. Mindfulness. 2013;4:3–17. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. New York, NY: Guilford Press; 2012. [Google Scholar]
- Vieten C, Astin JA, Buscemi R, Galloway GP. Development of an acceptance-based coping intervention for alcohol dependence relapse prevention. Substance Abuse. 2010;31:108–116. doi: 10.1080/08897071003641594. [DOI] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clinical Psychology Review. 2006;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addictive Behaviors. 2013;38:1563–1571. doi: 10.1016/j.addbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Lustyk MKB, Bowen S. Retraining the addicted brain: A review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychology of Addictive Behaviors. 2013;27(2):351. doi: 10.1037/a0029258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt A. Mindfulness meditation for substance use disorders: A systematic review. Substance Abuse. 2009;30:266–294. doi: 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M. The Psychiatric Diagnostic Screening Questionnaire manual. Los Angeles: Western Psychological Services; 2002. [Google Scholar]


