Abstract
Purpose of the Study:
Older American Indians disproportionately suffer from poorer physical and mental health and have greater disability compared to their racial and ethnic counterparts. The purpose of this study was to examine the disablement process among older American Indians.
Design and Methods:
Data analyzed were from the Native Elder Care Study, which included in-person interviews with 505 community-dwelling American Indians aged ≥55 years. We used structural equation modeling to examine the contributive direct and indirect effects of health, demographic, and psychosocial risk factors on disability.
Results:
Pathology had direct and indirect effects through social support and depressive symptoms on chronic pain intensity. Pathology also had direct and indirect effects on disability. Chronic pain intensity was a significant mediator between pathology and functional limitations. With contributive effects of older age and female sex, greater functional limitations were associated with increased disability.
Implications:
Our results support the theorized main pathway of the Disablement Process Model with our sample of older American Indians. Our findings support the importance of taking into account intra and extraindividual factors in assessing the prevalence and incidence of disability for older American Indians.
Keywords: Disablement process, American Indians, Structural equation modeling
Over half of U.S. community-dwelling adults aged ≥65 years have at least one basic activity limitation ( National Center for Health Statistics, 2012 ). The number and proportion of older adults aged 60–69 years with disabilities is dramatically increasing ( Seeman, Merkin, Crimmins, & Karlamangla, 2010 ). Specifically, when comparing data from the 1988–1994 and 1999–2004 National Health and Nutrition Examination Survey, in contrast to adults aged ≥70 years, this cohort had a 40–70% increase of all types of disability over the course of a decade ( Seeman et al., 2010 ). Disability trends in the youngest older adult cohort may reflect a growing prevalence and associated burden of chronic conditions at earlier ages of life.
There is substantial evidence indicating that intraindividual factors, such as depression, and extraindividual factors, such as social support, affect physical health and functioning among older adults. Longitudinal studies have demonstrated that late life depression increases the risk for disability onset ( Barry, Allore, Bruce, & Gill, 2009 ; Braungart, 2005 ; Reynolds, Haley, & Kozlenko, 2008 ). Similarly, higher levels of social support has been found to be associated with better levels of physical functioning and quality of life among older adults ( Everard, Lach, Fisher, & Baum, 2000 ; García, Banegas, Pérez-Regadera, Cabrera, & Rodríguez-Artalejo, 2005).
Compared with their same-aged counterparts of other race and ethnicities, older American Indians have some of the highest levels of disability ( Denny, Holtzman, Goins, & Croft, 2005 ; Goins, Moss, Buchwald, & Guralnik, 2007 ; Moss, Schell, & Goins, 2006 ; National Center for Health Statistics, 2012 ). Current evidence suggests older American Indians suffer from poorer health status and greater depressive symptoms compared to their same age racial peers ( Barnes, Powell-Griner, & Adams, 2005 ; Curyto et al., 1998 ; Denny et al, 2005 ; John, Kerby, & Hennessy, 2003 ). Similarly, factors such as social support and chronic pain have been documented to vary by racial groups ( Ajrouch, Antonucci, & Janevic, 2001 ; Green, Baker, Smith, & Sato, 2003 ). These factors may impact the acceleration or mitigation of the disablement process. Therefore, more research is warranted to understand this process with American Indians. This information can help in identifying where interventions may be most impactful in preventing or delaying disability among older American Indians. The purpose of our study was to examine the disablement process with a sample of community-dwelling older American Indians, which has not yet been done with this population.
Methods
Conceptual Framework
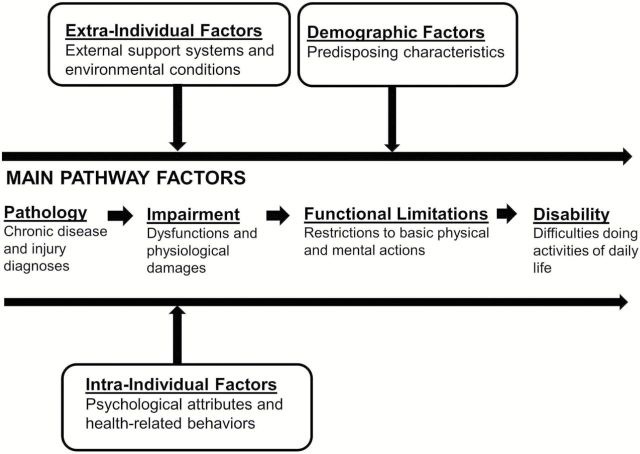
The Disablement Process Model ( Verbrugge & Jette, 1994 ) offers a structural framework for conceptualizing how physiological, intraindividual, and extraindividual factors may hasten or delay the onset of disability. Figure 1 shows the main pathway by which pathology, as measured by chronic disease burden and/or injuries, is theorized to increase the risk for impairment, functional limitations, and disability. Specifically, impairment is defined as structural or physiological abnormalities that causes damage and may manifest in such states as chronic pain. Functional limitations result in restrictions for basic physical functions while disability results in difficulties in performing usual activities of daily living. Certain predisposing characteristics, such as age and sex, may also contribute to the development of any of the main pathway variables. Similarly intraindividuals factors, such as depressive symptomatology, and extraindividual factors, such as social support, may act as mediators, moderators, or both of this process.
Figure 1.
The disablement process model (modified from Verbrugge and Jette, 1994 ).
Study Design and Data Collection
Data for this study are from the Native Elder Care Study, a cross-sectional study of community-dwelling older adult members of a federally recognized American Indian tribe located in the Southeast region of the United States ( Goins, Garroutte, Fox, Geiger, & Manson, 2011 ). Data were collected from 2006 to 2008 using in-person interviewer–administered surveys and included participant information on demographic characteristics, disability, mental and physical health, personal assistance needs, health care use, and psychosocial factors. The study was a collaborative community-based study that was requested by tribal leaders to generate needs assessment data on their older tribal members to inform service delivery efforts. The tribe’s institutional review board, tribe’s health board, tribal council, tribal elder council, and (West Virginia University) institutional review board approved the project. All participants provided informed consent and received a $20 gift card for completing the interview. The (Oregon State University) institutional review board approved the secondary data analyses for this study.
Sample
Inclusion criteria for the Native Elder Care Study included being an enrolled tribal member, aged ≥55 years, a resident of the tribal service area, non-institutionalized, and having passed a cognitive screen. The lower older age threshold of 55 years was used at the request of the tribal partners based on their observations that tribal members experienced health declines at younger ages compared to the general population. The study’s sampling frame was the current listing of enrolled members where we were able to identify 1,430 potential participants based on age and residential location. We then randomly selected names from this list for study recruitment and stratified by age using the following age groups: 55–64, 65–74, and ≥75 years. Trained interviewers approached individuals for participation through telephone calls and/or inperson home visits. Forty-seven persons from our list could not be located and 50 were determined to be ineligible for participation. Among the remaining individuals, 78 declined to participate yielding a final sample size of 505 with an 86.6% response rate. Comparisons between those who declined and participants showed that men were significantly more likely than women to decline (54% vs. 46%, p < .001) and older adults were more likely to decline than younger adults, although not significantly.
Measures
Main Pathway Variables
Pathology
We included self-reported doctor diagnosed health conditions that at least moderately correlated ( p < .001) with our disability measure to assess pathology. We summed the total of six conditions (congestive heart failure, arthritis, osteoarthritis, broken bone, joint fusion, and stroke) to which respondents indicated that had been diagnosed with since the age of 50. The resulting range was 0–6. This combined measure is a robust measure of pathology as it consists of a combination of chronic conditions and injury-related conditions, each of which can affect the burden of functioning in older adults.
Impairment
We used chronic pain intensity as our impairment measure. We use chronic pain because it is a commonly used measure and can be directly used to assess the severity of pathology. Chronic pain intensity was measured with an adapted self-report scale rating the intensity of chronic pain ( Von Korff, Ormel, Katon, & Lin, 1992 ). Three items had a response scale from 0 to 10, with higher scores indicative of higher chronic pain intensity. These items were combined into a mean scale.
Functional Limitations
We used the Short Performance Physical Battery tool to assess lower body functional limitations ( Guralnik et al., 1994 ). This tool consists of a series of balance tests, chair stands, and gait speed assessments to gauge the level of physical functioning and it’s opposite, functional limitations. The total score for the three tests ranges from 0 to 12, with lower scores indicating greater functional limitations. For the analyses and for ease of interpretation, we reverse coded the scale so that the measure represents the level of lower body functional limitations.
Disability
We defined disability as having difficulty with any of eight activities of daily living (ADLs) and eight instrumental activities of daily living (IADLs) ( Fillenbaum, 1985 ; Lawton & Brody, 1969 ). The ADLs included bathing/showering, dressing, eating, transferring, walking, toileting, grooming, and getting outside. The IADLs included using the telephone, light housework, heavy housework, preparing meals, shopping, managing money, managing medications, and transportation. For each of the 16 activities, if participants indicated that they had difficulty doing then they were coded as one. These activities were then summed to create a scale from 0 to 16, with greater scores indicating greater disability.
Other Pathway Variables
Intraindividual Factor—Depressive Symptomatology
We used the 20-item Centers for Epidemiologic Studies—Depression (CES-D) Scale to measure depressive symptomatology ( Radloff, 1977 ). This scale has been widely used among a number of population-based studies. The scale’s validity and reliability has been confirmed among older adults and across different racial groups ( Mui, Burnette, & Chen, 2002 ) and has been validated with older American Indians ( Chapleski, Lichtenberg, Dwyer, Youngblade, & Tsai, 1997 ). The Scale has a response scale of 0–3 (0 = rarely or none of the time, 1 = some or a little of the time, 2 = occasionally or a moderate amount of time, 3 = most or all of the time) for all items. Positive affect items were reverse coded. Therefore, the total sum score ranged from 0 to 60 comprising both the count and frequency of experiencing each of the CES-D items. This tool has been used to screen for depression with a commonly accepted cut-off score of ≥16 indicating clinically significant depressive symptomatology ( Radloff, 1977 ; Weissman, Sholomskas, Pottenger, Prusoff, & Locke, 1977 ).
Extraindividual Factor—Social Support
We used the Medical Outcomes Study-Social Support Scale, a 19-item scale to assess perceived social support ( Sherbourne & Stewart, 1991 ). Each item on the scale has a five-point response selection related to the frequency of which one has available types of support (0 = none of the time, 1 = a little of the time, 2 = some of the time, 3 = most of the time, 4 = all of the time) with a sum score range from 0 to 95.
Risk Factors
We included age and sex as non-modifiable risk factors for increased disability. Age was treated as categorical with three groups: 55–64, 65–74, and ≥75 years.
Statistical Analyses
First, we examined differential disability scores across sample characteristics by calculating age-stratified weighted means and standard errors. Unadjusted Poisson regression models were estimated to obtain p values for each variable category against the reference category. Next, we used ordinary least squared regression models to identify theorized endogenous variables (those affected by one or more variables in the model). Individual regression models were run to test for mediation and moderation. Last, structural equation modeling (SEM) was used to test a pathway model for examining the structural relationship of the independent variables on disability ( Acock, 2013 ). The maximum likelihood estimator method option was used in the pathway analysis, which uses all information available including missing values. Missing values occurred among 1% of cases for the pathology measure, 3% for pain intensity, 3% for functional limitations, <3% for depressive symptomatology, and <2% for social support. Continuous variables were standardized for the pathway analysis. Model fit was assessed with Goodness of Fit criteria: chi-square ( X2 ), comparative fit index, Tucker–Lewis index, and root mean squared error of approximation values. Sensitivity SEM analyses were run with ADL- and IADL-only disability scales. All analyses were completed using StataCorp’s statistical software package version 11.0 ( StataCorp, 2009 ).
Results
Table 1 presents sample characteristics and the weighted means, standard deviations, and bivariate associations of disability by sample characteristics. Unadjusted analyses indicated that those aged ≥75 years, female sex, with any of the six health conditions, with greater chronic pain intensity, with more functional limitations (SPPB score of 0 to 6), with clinically significant depressive symptomatology, and with lower levels of social support had significantly greater mean scores of disability.
Table 1.
Disability by Sample Characteristics ( n = 505)
| Sample characteristic | Total sample | Disability (range 0–16) | ||
|---|---|---|---|---|
| % | Mean | SE | p value | |
| Total | 100.0 | 2.07 | 0.15 | — |
| Age (years) | ||||
| 55–64 | 53.3 | 2.04 | 0.24 | REF |
| 65–74 | 30.0 | 1.48 | 0.17 | .050 |
| ≥75 | 16.7 | 3.27 | 0.29 | .001 |
| Sex | ||||
| Male | 37.2 | 1.60 | 0.22 | REF |
| Female | 62.8 | 2.35 | 0.19 | .017 |
| Chronic health conditions | ||||
| Congestive heart failure | ||||
| No | 92.2 | 1.78 | 0.14 | REF |
| Yes | 7.8 | 5.59 | 0.65 | <.001 |
| Arthritis | ||||
| No | 55.5 | 1.09 | 0.15 | REF |
| Yes | 44.5 | 3.29 | 0.24 | <.001 |
| Osteoarthritis | ||||
| No | 88.3 | 1.79 | 0.15 | REF |
| Yes | 11.7 | 4.17 | 0.41 | <.001 |
| Broken bone | ||||
| No | 76.4 | 1.62 | 0.15 | REF |
| Yes | 23.6 | 3.55 | 0.34 | <.001 |
| Joint fusion | ||||
| No | 95.2 | 1.90 | 0.14 | REF |
| Yes | 4.8 | 5.52 | 0.82 | <.001 |
| Stroke | ||||
| No | 92.8 | 1.85 | 0.14 | REF |
| Yes | 7.2 | 5.03 | 3.40 | <.001 |
| Chronic pain intensity | ||||
| Low | 42.1 | 0.65 | 0.10 | REF |
| Moderate | 36.4 | 2.07 | 0.22 | <.001 |
| High | 21.6 | 4.86 | 0.40 | <.001 |
| SPPB score | ||||
| 0–6 | 23.4 | 4.78 | 0.34 | REF |
| 7–12 | 76.6 | 1.25 | 0.13 | <.001 |
| CES-D score | ||||
| <16 | 84.7 | 1.69 | 0.14 | REF |
| ≥16 | 15.3 | 4.19 | 0.50 | <.001 |
| Social support | ||||
| Low | 33.4 | 2.85 | 0.22 | REF |
| Moderate | 33.5 | 2.10 | 0.25 | .052 |
| High | 33.1 | 1.28 | 0.28 | <.001 |
Note: All estimates are based on age stratum-weighted and imputed data. CES-D, Center for Epidemiologic Studies Depression scale; SPPB, Short Performance Physical Battery (Functional Limitations); SE , standard error; REF, reference category. p significance values obtained from unadjusted Poisson regression models.
Main Pathway Factors
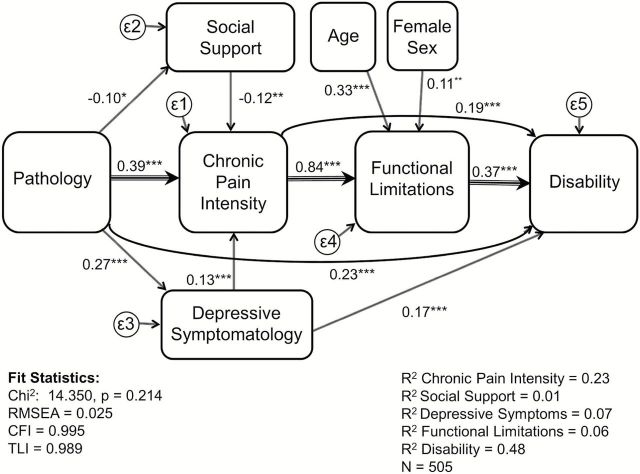
We present a theorized recursive pathway model by which variables are significantly associated with disability ( Figure 2 ). Table 2 provides the direct, indirect, and total effects for each of the model variables. Pathology had a positive significant direct (β = 0.23, p < .001) and indirect effect (β = 0.27, p < .001) on disability specifically through chronic pain intensity, functional limitations, social support and depressive symptomatology comprising a total effect β = 0.49 ( p < .001). Chronic pain intensity and functional impairment were significant mediators of the main disablement process pathway. We found chronic pain intensity’s direct effect (β = 0.19, p < .001) and indirect effect (β = 0.31, p < .001) through functional limitations had a total effect (β = 0.51, p < .001) on disability, suggesting that chronic pain severity accounts for 23% of the variance ( R2 = 0.23) in the model. Functional limitation had a significant direct effect (β = 0.37, p < .001) on disability, accounting for 6% of the variance ( R2 = 0.06). We found no significant interactions between the independent variables.
Figure 2.
Pathway analysis of disability.
Table 2.
Standardized Direct, Indirect, and Total Effects of Disablement Path ( n = 505)
| Direct effect | |||
|---|---|---|---|
| β (standardized) | Indirect effect | Total effect | |
| Chronic pain intensity | |||
| Pathology | 0.39*** | 0.05*** | 0.44*** |
| Depressive symptomatology | 0.13*** | — | 0.13*** |
| Social support | −0.12** | — | −0.12** |
| Social support | |||
| Pathology | −0.10* | — | −0.10* |
| Depressive symptoms | |||
| Pathology | 0.27*** | — | 0.27*** |
| Functional limitations | |||
| Chronic pain intensity | 0.84*** | — | 0.84*** |
| Pathology | — | 0.37*** | 0.37*** |
| Age | 0.33*** | — | 0.33*** |
| Female sex | 0.11** | — | 0.11** |
| Depressive symptomatology | — | 0.11*** | 0.11*** |
| Social support | — | −0.10*** | −0.10** |
| Disability | |||
| Chronic pain intensity | 0.19*** | 0.31*** | 0.51*** |
| Functional limitations | 0.37*** | — | 0.37*** |
| Pathology | 0.23*** | 0.27*** | 0.49** |
| Age | — | 0.12*** | 0.12*** |
| Female sex | — | 0.04** | 0.04** |
| Depressive symptomatology | 0.17*** | 0.07*** | 0.24*** |
| Social support | — | −0.06*** | −0.06*** |
Note : The significance levels shown are for the standardized solution. Comparative fit index = 0.995; Tucker–Lewis i = 0.989; root mean squared error of approximation = 0.025.* p < .05. ** p < .01. *** p < .001. X2 = 14.350, p = .214.
Intraindividual and Extraindividual Factors, Predisposing Characteristics
Depressive symptomatology had significant direct and indirect effects on disability. Greater depressive symptomatology was directly (β = 0.17, p < .001) and indirectly (β = 0.07, p < .001), through chronic pain intensity and functional limitations with a total effect (β = 0.24, p < .001) on disability. Social support had an inverse direct effect (β = −0.10, p < .01) on chronic pain intensity and no direct effect on disability. Both older age and female sex had indirect effects through functional limitations on disability (β = 0.12, p < .001 and β = 0.04, p < .01, respectively).
Discussion
This study is the first to examine the disablement process among older American Indians. These results support the theorized disablement pathway by which pathology and other factors may lead to increased disability ( Verbrugge & Jette, 1994 ). Our findings share similarity with other disablement studies in showing that functional limitations, particularly in lower body functioning, is more proximal to disability and mediate the relationship between pathology and disability ( Lawrence & Jette, 1996 ; Peek, Ottenbacher, Markides, & Ostir, 2003 ). However, our study differs from these studies with the inclusion of chronic pain intensity as a measure of impairment, a theorized link between pathology and functional limitations ( Verbrugge & Jette, 1994 ). In fact, results suggest that chronic pain accounts for the greatest variance by far of all of the endogenous variables in the model. Results from a longitudinal study also found a mediating effect of chronic pain on physical functioning and disability ( Young Casey, Greenberg, Nicassio, Harpin, & Hubbard, 2008 ).
We found that social support and depressive symptomatology contribute to the disablement process with the former acting as a buffer and the latter as a catalyst for further likelihood of disability. Our findings indicate these two psychosocial factors along with chronic pain mediate the relationship between pathology and functional limitations. These findings support results of other studies. One long-term prospective study supports the role of social support as a predictor of functional disability and pain in persons with early rheumatoid arthritis ( Evers, Kraaimaat, Geenen, Jacobs, & Bijlsma, 2003 ). Also, prospective studies have found depressed mood to be predictive of greater pain and disability ( Boersma & Linton, 2006 ; Ericsson, Poston, Linder, Taylor, Haddock, & Foreyt, 2002 ; Pincus, Burton, Kim, Vogel, & Field, 2002 ).
Our study differs from the two studies findings indicating that demographic factors impact occur at earlier stages of the disablement process ( Lawrence & Jette, 1996 ; Peek, Ottenbacher, Markides, & Ostir, 2003 ). Our results suggest that age and female sex have a more significant impact on functional limitations, with no significant direct effect on disability in our pathway model. The significant direct effect of older age on functional limitations parallels evidence of the association of older age with loss of strength ( Goodpaster et al., 2006 ) and other markers of frailty ( Bandeen-Roche et al., 2006 ), thereby increasing the risk of disability ( Ensrud et al., 2008 ). Although our study found a significant relationship between female sex and lower body functioning, the evidence remains inconclusive as to the robustness of this relationship in older adults ( Freedman, Martin, & Schoeni, 2002 ) and those that have controlled for chronic health conditions have seen this relationship greatly diminished ( Dunlop, Manheim, Sohn, Liu, & Chang, 2002 ). It is worth highlighting that in our sample, the those aged 50–64 years had significantly more disability compared to the those aged 65–74 years. We believe that this represents a cohort effect similarly observed in national data, whereby a greater proportion of the newest generation of older adults appears to be experiencing a greater burden of disease-related disabilities ( Seeman et al., 2010 ).
Our findings have implications for health and aging professionals and rehabilitation practitioners. Using social, behavioral, and cognitive approaches, psychosocial interventions may offer positive benefits for older adults experiencing and adjusting to chronic health conditions, subsequent chronic pain, and limitations to everyday activities ( Ciechanowski et al., 2004 ; Martire, Lustig, Schulz, Miller, & Helgeson, 2004 ). As current evidence suggests ( McAuley, Jerome, Marquez, Elavsky, & Blissmer, 2003 ; McCracken & Turk, 2002 ; Raji, Ostir, Markides, & Goodwin, 2002 ; Seeman, Berkman, Lusignolo, & Albert, 2001 ; Sullivan, Adams, Rhodenizer, & Stanish, 2006 ), psychosocial interventions hold the promise to improve mood, manage and reduce chronic pain, and improve physical functioning. In fact, a meta-analysis concludes that psychological interventions have short-term and long-term positive effects on chronic pain as well as physical and psychological functioning ( Hoffman, Papas, Chatkoff, & Kerns, 2007 ). Due to a dearth of reporting on race and ethnicity among prior studies, future studies are warranted to test the comparative effects of such interventions among different racial and ethnic groups. Similarly, we argue that, due to exacerbation of difficulties faced by those with restricted access to resources and programs, work is urgently needed to determine whether these interventions have differential impacts across socioeconomic status indicators.
Our findings should be regarded in the context of several limitations. Causality cannot be assumed because our data were cross-sectional. Even when constructing pathway analysis, the theorized direction of relationships can only be confirmed with longitudinal data. Future studies would benefit by using a longitudinal approach to assessing these relationships and to better understand the direction of causality of these risk factors. In regards to our mediation analysis of the disablement process, it should be noted that we used the count of six chronic and injury-related conditions that were moderately correlated with disability in our sample. It is plausible that if pathology is operationalized in alternative ways, different results might be found. Further research on the disablement process would be worth exploring by individual types of pathologies or specific well-known clusters of chronic conditions. Our data were all self-reported and therefore subject to recall bias. Finally, the results from this study are limited in its generalizability to older American Indian adults of a single tribe and are not representative of other older adult populations or other American Indian tribes.
In sum, our research supports the theorized pathway of the Disablement Process Model with our sample of older American Indians. Moreover, our model introduces the importance of measuring chronic pain and psychosocial factors when assessing older adults’ rehabilitative needs. More work is needed demonstrating the comparative effectiveness of interventions aimed at improving functioning and well-being among older adults of various racial/ethnic identity and socioeconomic status.
Funding
This study was funded in part from the National Institute of Aging (AG022336).
Acknowledgements
We would like to thank the tribe and its study participants for their role in making this study possible.
References
- Acock A . ( 2013. ). Discovering structural equation modeling using stata . College Station: , TX: : StataCorp LP; . [Google Scholar]
- Ajrouch K. J. Antonucci T. C. , & Janevic M. R . ( 2001. ). Social networks among Blacks and Whites: The interaction between race and age . Journal of Gerontology B: Psychological Sciences and Social Sciences , 56 , S112 – S118 . doi: 10.1093/geronb/56.2.S112 [DOI] [PubMed] [Google Scholar]
- Bandeen-Roche K. Xue Q. Ferrucci L. Walston J. Guralnik J. M. Chaves P. … Fried L. P . ( 2006. ). Phenotype of frailty: Characterization in the Women’s Health and Aging Studies . The Journals of Gerontology Series A: Biological Sciences and Medical Sciences , 61 , 262 – 266 . doi: 10.1136/jech.2008.078428 [DOI] [PubMed] [Google Scholar]
- Barnes, P. M., Powell-Griner, E., & Adams, P. F. (2005). Health characteristics of the American Indian and Alaska Native adult population, United States, 1999–2003. (Advance Data No. 356), Vital and Health Statistics. Center for Disease Control and Prevention: Atlanta, GA. [Google Scholar]
- Barry L. C., Allore H. G., Bruce M. L., Gill T. M . ( 2009. ). Longitudinal association between depressive symptoms and disability burden among older persons . The Journals of Gerontology Series A: Biological Sciences and Medical Sciences , 64 , 1325 – 1332 . doi: 10.1093/gerona/glp135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boersma K., Linton S. J . ( 2006. ). Expectancy, fear and pain in the prediction of chronic pain and disability: A prospective analysis . European Journal of Pain , 10 , 551 – 557 . doi: 10.1016/j.ejpain.2005.08.004 [DOI] [PubMed] [Google Scholar]
- Braungart E. R . ( 2005. ). Three studies of the Disablement Process in the oldest old: Predicting disability level, onset, and differential patterns of change over time . (Doctor of Philosophy), Pennsylvania State University; , Pittsburgh, PA: . [Google Scholar]
- Chapleski E. E. Lichtenberg P. A. Dwyer J. W. Youngblad`e L. M. , & Tsai P. F . ( 1997. ). Morbidity and comorbidity among Great Lakes American Indians: Predictors of functional ability . The Gerontologist , 37 , 588 – 597 . doi: 10.1093/geront/37.5.588 [DOI] [PubMed] [Google Scholar]
- Ciechanowski P. Wagner E. Schmaling K. Schwartz S. Williams B. Diehr P. ,… LoGerfo J . ( 2004. ). Community-integrated home-based depression treatment in older adults: A randomized controlled trial . Journal of the American Medical Association , 291 , 1569 – 1577 . doi: 10.1001/jama.291.13.1569 [DOI] [PubMed] [Google Scholar]
- Curyto K. J. Chapleski E. E. Lichtenberg P. A. Hodges E. Kaczynski R. , & Sobeck J . ( 1998. ) Prevalence and prediction of depression in American Indian elderly . Clinical Gerontologist , 18 , 19 – 37 . doi: 10.1300/J018v18n03_04 [Google Scholar]
- Denny C. H., Holtzman D., Goins R. T., Croft J. B . ( 2005. ). Disparities in chronic disease risk factors and health status between American Indian/Alaska Native and White elders: Findings from a telephone survey, 2001 and 2002 . American Journal of Public Health , 95 , 825 – 827 . doi: 10.2105/AJPH.2004.043489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop D. D. Manheim L. M. Sohn M.-W. Liu X. , & Chang R. W . ( 2002. ). Incidence of functional limitation in older adults: The impact of gender, race, and chronic conditions . Archives of Physical Medicine and Rehabilitation , 83 , 964 – 971 . doi: 10.1053/apmr.2 002.32817 [DOI] [PubMed] [Google Scholar]
- Ensrud K. E. Ewing S. K. Taylor B. C. Fink H. A. Cawthon P. M. Stone K. L. ,… Rodondi N . ( 2008. ). Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women . Archives of Internal Medicine , 168 , 382 – 389 . doi: 10.1001/archinternmed.2007.113 [DOI] [PubMed] [Google Scholar]
- Ericsson M. Poston W. S. C. Linder J. Taylor J. E. Haddock C. K. , & Foreyt J. P . ( 2002. ). Depression predicts disability in long-term chronic pain patients . Disability and Rehabilitation , 24 , 334 – 340 . doi: 10.1080/09638280110096241 [DOI] [PubMed] [Google Scholar]
- Everard K. M. Lach H. W. Fisher E. B. , & Baum M. C . ( 2000. ). Relationship of activity and social support to the functional health of older adults . The Journals of Gerontology Series B: Psychological Sciences and Social Sciences , 55 , S208 – S212 . doi: 10.10 93/geronb/55.4.S208 [DOI] [PubMed] [Google Scholar]
- Evers A. W. M. Kraaimaat F. W. Geenen R. Jacobs J. W. G. , & Bijlsma J. W. J . ( 2003. ). Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis . Behaviour Research and Therapy , 41, 1295 – 1310 , doi: 10.1016/S0005-7967(03)00036-6 [DOI] [PubMed] [Google Scholar]
- Fillenbaum G. G . ( 1985. ). Screening the elderly. A brief instrumental activities of daily living measure . Journal of the American Geriatrics Society , 33 , 698 – 706 . [DOI] [PubMed] [Google Scholar]
- Freedman V. A. Martin L. G. , & Schoeni R. F . ( 2002. ). Recent trends in disability and functioning among older adults in the United States . Journal of the American Medical Association , 288 , 3137 – 3146 . doi: 10.1001/jama.288.24.3137 [DOI] [PubMed] [Google Scholar]
- García E. L. Banegas J. Pérez-Regadera A. G. Cabrera R. H. , & Rodríguez-Artalejo , F. ( 2005. ). Social network and health-related quality of life in older adults: A population-based study in Spain . Quality of Life Research , 14 , 511 – 520 . doi: 10.1007/s11136-004-5329-z [DOI] [PubMed] [Google Scholar]
- Goins R. T., Garroutte E. M., Fox S. L., Dee Geiger S., Manson S. M . ( 2011. ). Theory and practice in participatory research: Lessons from the Native Elder Care Study . The Gerontologist , 51 , 285 – 294 . doi: 10.1093/geront/gnq130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goins R. T. Moss M. Buchwald D. , & Guralnik J. M . ( 2007. ). Disability among older American Indians and Alaska Natives: An analysis of the 2000 Census public use microdata sample . The Gerontologist , 47 , 690 – 696 . doi: 10.1002/gps.282510.1002/gps.2825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodpaster B. H. Park S. W. Harris T. B. Kritchevsky S. B. Nevitt M. Schwartz A. V. … Newman A. B . ( 2006. ). The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study . The Journals of Gerontology Series A: Biological Sciences and Medical Sciences , 61 , 1059 – 1064 . [DOI] [PubMed] [Google Scholar]
- Green C. G. Baker T. A. Smith E. M. , & Sato Y . ( 2003. ). The effect of race in older adults presenting for chronic pain management: A comparative study of black and white Americans . The Journal of Pain , 4 , 82 – 90 . doi :http://dx.doi.org/10.1054/jpai.2003.8 [DOI] [PubMed] [Google Scholar]
- Guralnik J. M. Simonsick E. M. Ferrucci L. Glynn R. J. Berkman L. F. Blazer D. G. ,… Wallace R. B . ( 1994. ). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission . Journals of Gerontology , 49 , M85 – M85 . doi: 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Hoffman B. M. Papas R. K. Chatkoff D. K. , & Kerns R. D . ( 2007. ). Meta-analysis of psychological interventions for chronic low back pain . Health Psychology , 26 , 1 – 9 . doi: 10.1037/0278-6133.26.1.1 [DOI] [PubMed] [Google Scholar]
- John R. Kerby D. S. , & Hennessy C. H . ( 2003. ). Patterns and impact of comorbidity and multimorbidity among community-resident American Indian elders . The Gerontologist , 43 , 649 – 660 . doi: 10.1093/geront/43.5.649 [DOI] [PubMed] [Google Scholar]
- Lawrence R. H. , & Jette A. M . ( 1996. ). Disentangling the disablement process . Journal of Gerontology B: Psychological Sciences and Social Sciences , 51B , S173 – S182 . doi: 10.1093/geronb/51B.4.S173 [DOI] [PubMed] [Google Scholar]
- Lawton M. P. , & Brody E. M . ( 1969. ). Assessment of older people: Self-maintaining and instrumental activities of daily living . The Gerontologist , 9 , 179 – 186 . doi: 10.1093 /geront/9.3_Part_1.179 [PubMed] [Google Scholar]
- Martire L. M. Lustig A. P. Schulz R. Miller G. E. , & Helgeson V. S . ( 2004. ). Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness . Health Psychology , 23 , 599 . doi: 10.1037/0278-6133.23.6.599 [DOI] [PubMed] [Google Scholar]
- McAuley E. Jerome G. J. Marquez D. X. Elavsky S. , & Blissmer , B. ( 2003. ). Exercise self-efficacy in older adults: Social, affective, and behavioral influences . Annals of Behavioral Medicine , 25 , 1 – 7 . doi: 10.1207/S15324796ABM2501_01 [DOI] [PubMed] [Google Scholar]
- McCracken L. M., Turk D. C . ( 2002. ). Behavioral and cognitive-behavioral treatment for chronic pain: Outcome, predictors of outcome, and treatment process . Spine , 27 , 2564 – 2573 . doi :10.1097/01.BRS.0000032130.45175.66 [DOI] [PubMed] [Google Scholar]
- Moss M. P., Schell M. C., Goins R. T . ( 2006. ). Using GIS in a first national mapping of functional disability among older American Indians and Alaska Natives from the 2000 census . International journal of health geographics , 5 , 37 . doi: 10.1186/1476-072X-5-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mui A. Burnette D. , & Chen L . ( 2002. ). Cross-cultural assessment of geriatric depression: A review of the CES-D and GDS . In Skinner J. H. , Teresi J. A. Holmes D. Stahl S. M & Stewart A. L. (Eds.), Multicultural measurement in older populations (pp. 147 – 178 ). New York: : Springer Publishing Co; . [Google Scholar]
- National Center for Health Statistics . ( 2012. ). National Health Interview Survey 2012 . Atlanta, GA: : Centers for Disease Control and Prevention; . [Google Scholar]
- Peek M. K. Ottenbacher K. J. Markides K. S. , & Ostir G. V . ( 2003. ). Examining the disablement process among older Mexican American adults . Social Science and Medicine , 57 , 413 – 425 . doi: 10.1016/S0277-9536(02)00367-2 [DOI] [PubMed] [Google Scholar]
- Pincus T., Burton A. K., Vogel S., Field A. P . ( 2002. ). A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain . Spine , 27 , E109 – E120 . doi :10.1097/00007632-200203010-00017 [DOI] [PubMed] [Google Scholar]
- Radloff L. S . ( 1977. ). The CES-D scale a self-report depression scale for research in the general population . Applied Psychological Measurement , 1 , 385 – 401 . doi: 10.1177/0 14662167700100306 [Google Scholar]
- Raji M. A. Ostir G. V. Markides K. S. , & Goodwin J. S . ( 2002. ). The interaction of cognitive and emotional status on subsequent physical functioning in older Mexican Americans . The Journals of Gerontology Series A: Biological Sciences and Medical Sciences , 57 , M678 – M682 . doi :10.1093/gerona/57.10.M678 [DOI] [PubMed] [Google Scholar]
- Reynolds S. L. Haley W. E. , & Kozlenko N . ( 2008. ). The impact of depressive symptoms and chronic diseases on active life expectancy in older Americans: Findings from the Hispanic established population for the epidemiologic study of the elderly . American Journal of Geriatric Psychiatry , 16 , 425 – 432 . doi: 10.1097/JGP.0b013e31816ff32e [DOI] [PubMed] [Google Scholar]
- Seeman T. E. Berkman L. Lusignolo T. M. , & Albert M . ( 2001. ). Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging . Health Psychology , 20 , 243 – 255 . doi: 10.10 37/0278-6133.20.4.243 [DOI] [PubMed] [Google Scholar]
- Seeman T. E. Merkin S. S. Crimmins E. M. , & Karlamangla A. S . ( 2010. ). Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988-1994 and 1999-2004 . American Journal of Public Health , 100 , 100 – 107 . doi: 10.2105/AJPH.2008.157388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne C. D. , & Stewart A. L . ( 1991. ). The MOS social support survey . Social Science & Medicine , 32 , 705 – 714 . doi: 10.1016/02779536(91)90150-B [DOI] [PubMed] [Google Scholar]
- StataCorp . ( 2009. ). Stata Statistical Software: Release 11 . College Station, TX: : StataCorp; . [Google Scholar]
- Sullivan M. J., Adams H., Rhodenizer T., Stanish W. D . ( 2006. ). A psychosocial risk factor–targeted intervention for the prevention of chronic pain and disability following whiplash injury . Physical Therapy , 86 , 8 – 18 . [DOI] [PubMed] [Google Scholar]
- Verbrugge L. M. , & Jette A. M . ( 1994. ). The disablement process . Social Science & Medicine , 38 , 1 – 14 . doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Von Korff M. Ormel J. Katon W. , & Lin E. H. B . ( 1992. ). Disability and depression among high utilizers of health care: A longitudinal analysis . Archives of General Psychiatry , 49 , 91 – 100 . doi: 10.1001/archpsyc.1992.01820020011002 [DOI] [PubMed] [Google Scholar]
- Weissman M. M. Sholomskas D. Pottenger M. Prusoff B. A. , & Locke B. Z . ( 1977. ). Assessing depressive symptoms in five psychiatric populations: A validation study . American Journal of Epidemiology , 106 , 203 – 214 . [DOI] [PubMed] [Google Scholar]
- Young Casey C. Greenberg M. A. Nicassio P. M. Harpin R. E. , & Hubbard D . ( 2008. ). Transition from acute to chronic pain and disability: A model including cognitive, affective, and trauma factors . Pain , 134 , 69 – 79 . doi: 10.1016/j.pain.2007.03.032 [DOI] [PubMed] [Google Scholar]