Abstract
Objective:US health care institutions are implementing secure websites (patient portals) to achieve federal Meaningful Use (MU) certification. We sought to understand efforts to implement portals in “safety net” health care systems that provide services for low-income populations.
Materials and Methods:Our rapid ethnography involved visits at 4 California safety net health systems and in-depth interviews at a fifth. Visits included interviews with clinicians and executives (n = 12), informal focus groups with front-line staff (n = 35), observations of patient portal sign-up procedures and clinic work, review of marketing materials and portal use data, and a brief survey (n = 45).
Results:Our findings demonstrate that the health systems devoted considerable effort to enlisting staff support for portal adoption and integrating portal-related work into clinic routines. Although all health systems had achieved, or were close to achieving, MU benchmarks, patients faced numerous barriers to portal use and our participants were uncertain how to achieve and sustain “meaningful use” as defined by and for their patients.
Discussion:Health systems’ efforts to achieve MU certification united clinic staff under a shared ethos of improved quality of care. However, MU’s assumptions about patients’ demand for electronic access to health information and ability to make use of it directed clinics’ attention to enrollment and message routing rather than to the relevance and usability of a tool that is minimally adaptable to the safety net context.
Conclusion:We found a mismatch between MU-based metrics of patient engagement and the priorities and needs of safety net patient populations.
Keywords: meaningful use, electronic health records, safety net providers, health disparities, patient access to records
INTRODUCTION
In order to meet federal Meaningful Use (MU) certification criteria, US health care institutions are rapidly implementing secure websites (“patient portals”) linked to patients’ electronic health records (EHRs). Patient portals provide patients with access to personal health information and enable electronic communication with health care providers. Portals have been shown to contribute to improvements in chronic disease management, patient satisfaction, and patient-clinician interactions.1 Starting in 2014, MU financial incentives required that at least 50% of patients be offered online access to their health information and at least 5% of patients view, download, or transmit their electronic health data. (Recognizing that health systems were having difficulty achieving the 5% target, the Office of the National Coordinator for Health Information Technology subsequently changed this target metric to one patient per qualifying provider for each MU reporting period.)2
Safety net institutions provide services for a high proportion of low-income patients and face large obstacles to widespread portal adoption. These obstacles include English-only EHRs and sizable patient populations with limited health literacy and/or English literacy, limited proficiency with digital technologies, disabilities that impede portal use, and mental health and/or substance use conditions.3,4
This is the first study to our knowledge to explore patient portal implementation within safety net health care systems striving to meet MU criteria. Drawing on ethnographic fieldwork and sociotechnical theories that conceive of technology adoption as a process of organizational change, we examined how MU policies shaped portal implementation and patient engagement strategies at 5 California community health centers.
METHODS
Rapid ethnography
Ethnography has important strengths for the study of health information technology (IT) adoption and use. An ethnographic approach enables in-depth insight into the interactions between technologies and intended users and can explain unintended uses, “workarounds,” or non-use.5 Focusing on the collaborative and contingent nature of health care work, ethnographic inquiry counters longstanding assumptions in health IT design that technology use can be defined as discrete tasks engaged in by individuals or through pre-fixed workflows.6,7
Although ethnography typically involves lengthy fieldwork, here we draw on a “rapid ethnography” approach that includes brief observations at multiple field sites, in-depth interviews with key informants, engagement with social theory, and analysis of archival materials and quantitative data.8 This approach is informed by “sociotechnical” theories of technology use, which assert that organizations are complex systems that are simultaneously social and technical.9 These 2 dimensions of health care organizations are deeply interrelated, such that implementing new technologies requires attending to the dynamic and mutable interactions of people, objects, and work routines.10 It also means that introducing a new system or tool can have unanticipated effects on how the organization functions, particularly if implementation is assumed to be merely a matter of “inserting” a system or artifact into existing practices.
Sociotechnical theories also posit that technologies are not neutral tools, but rather are embedded with the implicit assumptions of their creators. An EHR, for example, contains assumptions about the people who will use the system, how they will use it, and its likely impact on clinical work.11,12 Health IT systems can fail because of mismatches between hidden assumptions in the tool and the real-life practices and priorities of intended users.13,14 Sociotechnical evaluations examine what counts as successful technology adoption for different groups and how these negotiated conceptions diverge from predetermined measures of success and failure.15–18
Participants
We aimed to recruit a range of health systems that had secured funding to support patient portal implementation, anticipating that they would be actively working to achieve MU certification. We contacted 5 health systems that had recently received small grants from the Center for Care Innovation through its California Healthcare Foundation Patient Portal Initiative (a total of 9 grants were awarded). Our choice aimed to maximize the diversity of geographic location, patient demographics, organization size, and moderate to high success in reaching MU benchmarks (see Table 1). All sites had been working with an EHR for at least 2 years, had achieved MU Stage 1 attestation, and were planning for Stage 2 attestation. All 5 agreed to participate.
Table 1.
Site characteristics
| Characteristic | Site 1 | Site 2 | Site 3 | Site 4 | Site 5 |
|---|---|---|---|---|---|
| Location | Southern California | Southern California | Northern California | Northern California | Northern California |
| Enrollment and usea | Over 70% given access per month; over 25% used portal per month | 73% issued token; 12% enrolled and sent a secure message | 1500 enrolled per month; ∼20 secure messages received per month | 62% given access per month; 60–70% of enrolled have sent ≥1 secure message |
|
| Patient portal features | Medical history; test results; secure messaging; viewing appointments; appointment scheduling; health education | Medical history; test results; appointment scheduling; prescription refills; health education | Medical history; test results; secure messaging; viewing appointments; appointment requests | Medical history; test results; secure messaging; billing statements; non-urgent appointment requests; viewing appointments; health history forms | Medical history; test results; secure messaging; appointment requests |
| EHR vendor | NextGen | NextGen | NextGen | eClinicalWorks | NextGen |
| Roles of participants |
|
|
|
|
Program development coordinator |
| Health systemb |
|
|
|
|
|
| Patient populationb | 83% at or below 100% federal poverty level (FPL); 35% of patient population has limited English proficiency |
|
|
|
|
a“Given access” is defined as having a formal record of offering a patient the opportunity to enroll in the patient portal, regardless of whether the offer was accepted or declined; “issued token” is defined as having sent a patient an e-mail with information about how to set up a portal account; percentages represent the proportion of unique patients seen in clinic.
bParticipating health systems were asked to provide detailed information about their clinical operations and patient populations. Variations in their responses are reflected in the information reported here.
Data collection and analysis
From September to November 2015, 3 of the authors (SA, CL, LT) conducted in-person site visits and phone interviews. At 4 sites, we conducted one- to one-and-a-half-day visits that included in-depth interviews with executives and clinicians (n = 12), informal focus groups with clinical and IT support staff (n = 35), observations of patient portal sign-up procedures and clinic work, and reviews of marketing materials and EHR use data. Unable to arrange a visit at Site 5, we conducted a phone interview with a program coordinator responsible for overseeing portal implementation. Interviews and focus groups were arranged by health system leaders and aimed at including a broad range of perspectives (see Supplementary Appendix for interview/focus group questions). Observations took place while accompanying a staff member on an extended tour of clinic facilities. Observed activities included call center work, patient check-in procedures, clinic team meetings, and patient-clinician encounters. Informal interviews with staff during clinic tours enabled us to ask questions about site-specific enrollment activities and patient outreach materials. Interviews and focus groups were audio-recorded and transcribed, and detailed field notes documented all site visit activities. We obtained informed consent from patients present at observations. The study was exempted from review by the University of California, San Francisco, Institutional Review Board.
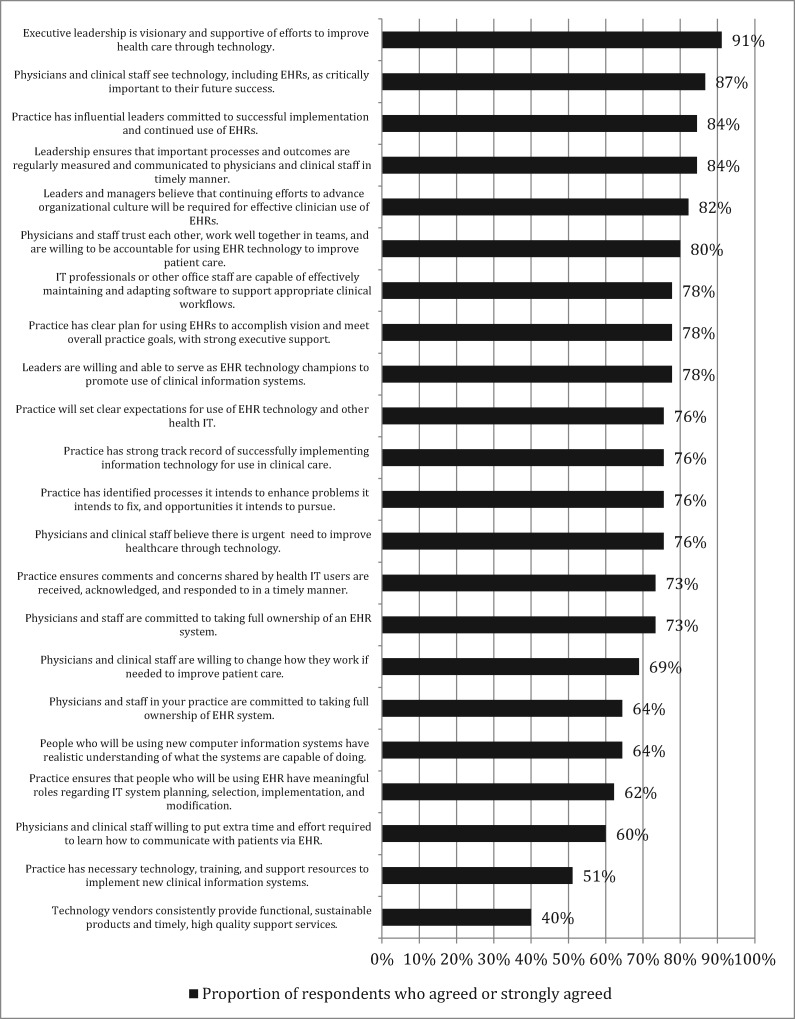
We administered a modified version of the American Medical Association’s Health IT Readiness Survey to providers and staff (n = 45), with questions about facilitators of and barriers to health IT adoption19 (See Figure 1 ).
Figure 1.
Health IT readiness assessment survey results (n = 45; all sites combined). We modified the American Medical Association’s Health Information Technology Readiness Survey by removing 3 questions focused on provider-facing EHR functions (documentation of patient care, retrieval of patient information, and ePrescribing) and adding a question focused on provider willingness to communicate with patients through the EHR.
Five of the authors (SA, CL, LT, MH, KH) participated in data analysis, in which health systems were treated as units of analysis. We used the constant comparative method, in which interpretations are made and adjusted in light of each new account20 (see also21). After repeatedly reading interview transcripts, field notes, and survey responses, the group met regularly to develop a coding framework that was applied to all data in the online qualitative data analysis program Dedoose (version 7.1.3). All transcripts and notes were coded independently by at least 2 coders, and differences were resolved in group discussions. Further discussions identified key themes related to commonalities and differences across sites, with a particular focus on how MU policy and the safety net context influenced portal implementation.
RESULTS
We found that clinics engaged in significant efforts to implement the portal and that these activities fell into 2 broad domains: (1) enlisting staff support by framing the portal as beneficial for patients and health systems and (2) transforming clinic routines in order to accommodate portal-related work. Although all health systems had achieved, or were close to achieving, MU benchmarks, few patients actually used portal services. Participating health systems were uncertain how to achieve and sustain “meaningful use” as defined by and for their patients. We elaborate on these themes below (see Table 2 for additional quotes by theme).
Table 2.
Additional quotes by theme
| Thematic domains | Subthemes | Illustrative quotes |
|---|---|---|
| Enlisting staff support | Pursuing financial benefit and competitive advantage | “We had already budgeted to receive the meaningful use money, so we were committed.” (executive, Site 2) |
| Providing all patients with access to their electronic health information |
|
|
| Promising improved quality and efficiency |
|
|
| Fitting the portal into clinic routines | Enrolling patients |
|
| Moving patients from enrollment to use |
|
|
| Routing patients’ messages |
|
|
| Rethinking meaningful use | Limits to portal access and usability |
|
Enlisting staff support
Pursuing financial benefit and competitive advantage
MU financial incentives provided a powerful rationale for diverting staff time and effort to portal implementation:
“We were very driven by Meaningful Use. The dollars were significant and were already budgeted, meaning the dollars are already being used. We continue to do a lot of work to make sure that incentive money is coming to us. Engagement is coming from the top.” (Site 2)
As this quote highlights, meeting portal-related MU requirements was both financially beneficial and a means of preventing financial loss when incentive payments had already been absorbed into chronically overstretched clinic budgets. Some leaders also assumed that meeting MU requirements would give community health centers a competitive advantage in an increasingly market-based safety net landscape. Referring to a larger health system’s use of the portal in marketing campaigns designed to attract prospective patients, a physician assistant at Site 3 said, “What they’re advertising on TV as something special, we have it right here.”
Providing patients with electronic access to their health information
Although MU financial payouts offered a powerful organizational motive for portal adoption, appealing to staff and patients required a message aligned with the ethos of safety net health systems, which are dedicated to providing high-quality care to underserved patient populations. To promote the portal to staff, leaders drew on one of the key underlying assumptions of MU: that patients want, and should be given, electronic access to their health information. Thus, launching the portal was implicitly framed as a moral obligation: “We think it’s the right thing to do,” said a program director at Site 2.
Our participants recognized that not all of their patients had Internet access at home or would feel comfortable using a portal. However, staff and clinicians came to believe that a significant portion of their patients wanted electronic medical information and could benefit from it with simple instruction. In other words, even though the digital divide was a real concern, it was not considered sufficient to delay portal rollout:
“I think they’re interested. They just don’t know how to do it. They haven’t been shown how to do it. I think showing them and helping them is going to be the best thing.” (staff member, Site 3)
Promising improved quality and efficiency
The promise of gains in clinic efficiency and improved communication between clinicians and patients was also invoked to build staff and clinician support. For example, patients presumably would be able to bypass busy call centers with the portal’s offer of direct access to clinicians: “This is convenient. You can save a phone call. You can save time,” said a nurse midwife at Site 3. For clinicians, meanwhile, the portal was billed as an essential component of ambulatory medicine’s evolution toward “team-based care,” in which multiple clinicians and support staff work collaboratively to provide patient care.
The problems that clinics anticipated the portal would solve were therefore multiple: financial pressures, market-based competition, inefficient clinic operations, and patients wanting more timely access to clinic services. Commitment to the portal was also bolstered by a belief that providing high-quality medical care requires taking on an ever-expanding array of technological devices and services. The implicit faith in technological solutions also applied to the health of the organization overall, as seen in the results of our Health IT Readiness survey, in which 87% of respondents agreed that “technology like EHRs are critically important for future success” (see Figure 1 for complete survey results).
Fitting the portal into clinic routines
Technology adoption is often assumed to be simply a matter of inserting a new device or system into existing work routines, or replacing an existing system with one that is more efficient or effective. However, the adoption process is usually characterized more by organizational transformation than by simple integration or substitution. This was apparent in the wide-ranging efforts by participating health systems to increase awareness of the patient portal, enroll patients, and manage patient messages. Moreover, these transformations took place with a sense among clinic staff that they lacked the capacity to implement new IT systems. For example, in the Readiness Survey, only 51% of respondents agreed that their practice had “the necessary technology, training, and support resources needed to implement new clinical information systems.”
Enrolling patients
Across sites, implementation strategies were largely focused on ensuring that staff helped patients with enrollment, which involves verifying personal information like date of birth, choosing a username and password, and setting up security questions (see Table 3 for additional implementation activities by site). The emphasis on enrollment helped clinics to reach Stage 2 MU target metrics, which prioritized offering patients “timely online access to their health information.”2 The assumption built into the MU metric is that providing patients with instructions is sufficient to convert them into active portal users. Therefore, outreach strategies often emphasized enrolling as many patients as possible.
Table 3.
Portal implementation activities by site
| Site | Promote portal to patients | Assist patients with enrollment and use | Route patient messages | Build support among clinicians and staff |
|---|---|---|---|---|
| Site 1 |
|
|
|
|
| Site 2 |
|
|
Response team for each clinician performed “triage” and responded to secure messages when appropriate |
|
| Site 3 |
|
|
|
|
| Site 4 |
|
|
|
|
| Site 5 | Flyers for the patient portal in English and Chinese posted in clinic |
|
|
|
To accomplish this goal, participating health systems took an “all-hands-on-deck” approach. “There needs to be an organization-wide engagement with the portal,” said a program coordinator at Site 2. Portal “champions” (a term used by implementation teams to describe people responsible for building awareness and support for the portal) were tasked with reminding clinicians and staff to encourage patients to sign up for a portal account, while “implementation teams” developed promotional materials and other strategies to ensure that portal enrollment remained a day-to-day priority. Most clinics enlisted volunteers to distribute promotional materials and provide enrollment assistance to patients, including handing out unique codes for online portal registration, called “tokens,” and walking patients through the registration process on a clinic computer. One clinic installed self-service computer kiosks devoted exclusively to portal enrollment in the waiting room.
However, kiosks and volunteers were less effective than hoped, in part because the purpose of the portal was not clear to many patients. “[We had to] explain what the portal was,” said a coordinator at Site 2. Such explanations tended to be more persuasive when coming from trusted staff members or clinicians, so most clinics eventually shifted patient outreach responsibilities from volunteers to clinic staff, particularly front desk clerks and medical assistants. At times, the push to achieve MU’s 50% enrollment target became all-consuming and led to staff being reassigned to new positions or asked to defer other work: “When a site wasn’t meeting the goal, we moved around the staff, like Tetris,” said an executive at Site 2. During our visits to the clinics, portal registration fatigue was evident in descriptions of flagging interest in promoting the portal among busy clinic staff and prompted additional strategies to bolster enthusiasm, such as contests between affiliated clinics with prizes for the highest rate of enrollment.
Moving patients from enrollment to use
MU also tasks health systems with demonstrating that at least 5% of patients actually use the portal, ie, view, download, or transmit their health information or send an electronic message to a clinician. This goal proved to be a significant challenge for all health centers, because patients who were given tokens rarely went on to register for an account, and even patients who had received enrollment assistance were unlikely to log on to the portal later. Understanding that many patients lacked computer proficiency, front desk clerks and medical assistants often used clinic computers to show patients how to use portal services. A coordinator at Site 2 explained:
Some of them didn’t even use technology at all.… If there was time, we would teach them how to navigate their inbox. That was a new experience for them.
Assisting with the navigation of complex EHR websites was no small task for busy safety net clinics, which lack the capacity to provide one-on-one computer training and technical support for a large number of patients. Therefore, moving patients from enrollment to use often remained an elusive goal.
Routing patient messages
Portal-enabled messaging promised to bring efficiencies to patients’ interactions with the clinic by reducing call volume and enabling direct communication with clinicians. In reality, however, messaging created new forms of sociotechnical work for health systems, much of it directed at preventing patients from communicating directly with clinicians. Specifically, at all sites we learned about procedures that monitor, sort, and forward messages to nonclinicians when possible. Often, the goal of this “triage” process appeared to be to allay clinicians’ concerns that the portal would create additional unpaid work and might increase “frivolous” (ie, nonclinical) messages from patients (see Table 3 for triage procedures by site). The chief medical officer at Site 2 explained his site’s efforts to limit clinician involvement: “Each provider has a response team surrounding them.” Several clinicians confirmed that triage reduced the burden of patient messaging: “By the time I even see it, it’s usually been responded to already,” said a clinician at Site 3.
Ambivalence about the value of portal-based interactions with patients also emerged in our survey, with 60% of respondents agreeing that “physicians and staff are willing to put in extra time and effort to learn to communicate with patients through the EHR.”
Moreover, the additional work generated by a relatively small volume of patient messages created a disincentive for clinics to achieve a higher rate of patient use of the portal than is mandated by MU. A clinic manager at Site 1 said, “If the volume went up, the monitoring of the inboxes would have to shift over to a clinical person or we would have to hire someone.” Some clinics even discouraged their staff from promoting the portal once the MU threshold was reached: “Our managers maintain… ‘don’t market [the portal] too much. We really don’t want all our patients signed up. We just need to reach the five percent requirement,’” said a staff member at Site 5.
Portal-based messaging also added complexity to the clinic’s procedures for conveying information to patients. For example, clinicians were often reluctant to communicate electronically about test results or urgent clinical matters out of concern that the message would not be received fast enough, since patients without e-mail accounts have to proactively search for messages on portal websites. These concerns often prompted clinicians and staff to call patients rather than initiate or continue an electronic exchange, highlighting the contrast between the portal’s promise of efficiency and the additional complex modes of communication that it actually generated:
“… We’ve been talking about the portal like it’s going to make things so much easier, but what actually happened is now you have two different ways of doing things, because you have patients who are on portal and patients who aren’t.… You have an extra workflow to figure out.” (staff member, Site 1)
Finally, the message routing process could be confusing to patients, who were often under the impression that an electronic message would be delivered directly, and exclusively, to their clinician. Clinic staff regularly fielded questions from patients concerned about breaches of privacy and were unaware that their messages could be viewed by numerous clinic staff and would be archived in the EHR. Some health systems attempted to mitigate these concerns by including standardized scripts about messaging policies in all secure messages sent to patients.
Rethinking meaningful use
At the time of our study, all participating health systems had already reached, or were approaching, MU metrics for patient engagement. By MU standards, therefore, portal implementation was a success. However, there was little sustained patient use of the portal, and most sites reported a low volume of patient messages. Moreover, despite substantial efforts to promote enrollment, many of our informants doubted that most patients enrolled on-site would log on independently. In other words, the “letter” of MU was achieved in terms of signing up many patients for portal access, without the “spirit” of MU (patients viewing and acting on their personal medical information) being realized. As a staff member at Site 3 said, “… We’re all doing a dance, but there’s nothing underneath the shells.” The “dance” was achieving MU certification, which was often described as a distraction from focusing on meaningful engagement as defined by patients themselves:
“… The driver becomes meeting certain meaningful use standards sometimes taking priority over meaningful use for our patients.” (executive, Site 2)
Limits to portal access and usability
For both patients who signed up for portal access and those who did not, a number of usability and accessibility challenges emerged that undermined their ability to “meaningfully” engage with the tool. First, health systems reported difficulties making adjustments and improvements to portal websites to accommodate patient needs. “You’re really at the mercy of whatever EHR that you decided to use,” a Site 1 staff member explained. Citing repeated technical problems, an IT manager at Site 3 similarly concluded that “the vendors are focusing on Meaningful Use instead of usability and functions.” The sense that health systems were adopting the portal despite EHR vendors was echoed by our survey findings: only 40% of respondents agreed that “technology vendors consistently provide functional, sustainable products and timely, high-quality support services.” While we were unable to directly assess usability among patients, our informants’ comments echo the growing literature documenting EHR usability barriers within safety net patient populations.22,23
Additional reasons that patients could not or would not use the portal included language. Although portal navigation was available in English and Spanish at participating clinics, it was not available in other languages, and nearly all medical records and test results were written exclusively in English. “… The [EHR vendor] website isn’t available in their Chinese language.… How were they going to get their patients to be able to utilize this?” asked a program coordinator at Site 5. “Patients want to act in their own language,” an executive at Site 2 concurred. Language barriers were compounded by limited digital and linguistic literacy among safety net patients. “The majority of patients either can’t read or don’t have e-mail,” said a clinical staff member at Site 3.
Health systems also reported that many patients were afraid portal use would elicit government surveillance. This fear was particularly acute among undocumented immigrants. As a clinic manager at Site 1 explained, “… A lot of our patients are undocumented. They have a vision that their name is going to be in a big computer and that they’re going to be deported.” By contrast, family members or caregivers who wanted to use the portal on behalf of a patient were often denied access due to privacy laws. Finally, clinic staff told us that many patients preferred in-person interactions with their clinicians. One clinic, for example, provided services for a high proportion of homeless people, whose frequent visits rendered the clinic a de facto social center. For many of these patients, the portal increased a sense of social isolation rather than promoting convenience.
DISCUSSSION
Our account of community clinics’ efforts to adopt a patient portal highlights the simultaneously productive and troubled confluence of a national policy mandate, health IT systems, and on-the-ground realities of medical service provision for low-income and ethnically diverse patients in California. We found that efforts to achieve MU certification translated into creative, sustained attempts to ensure that patients benefit from the EHR, and united clinic staff under a shared ethos of improved quality of care. However, MU’s assumptions about patients’ pent-up demand for electronic access to health information, and ability to make use of it, directed clinics’ attention to enrollment and message management rather than the relevance and usability of a tool that was minimally adaptable to safety net patient populations. Ultimately, despite health systems’ faith in the promise of the portal, embodied in the metaphor of an “open door” to information and communication, most of their patients could not obtain the promised benefits. Moreover, implementation generated considerable additional work for health systems and did not lead to anticipated gains in efficiency. An executive at Site 1 expressed ambivalence about this tradeoff:
“I’m not sure if, at the end of the day, the MU dollars offset the cost to the organizations implementing it. I don’t know if just because you achieved MU, you’re providing high-quality care.”
Limitations
Our study has a number of limitations. We conducted only one interview at Site 5. However, the interviewee was responsible for portal enrollment and MU attestation, and was able to offer detailed insight into the experiences and challenges of portal adoption at her site. We gained minimal insight into patients’ experiences with the portal, and we visited just 5 health systems. Participating health centers were likely at a more advanced stage of implementation than other community health centers, given that they were a part of a grant program supporting portal adoption. Future studies would benefit from in-depth engagement with patients and with health systems that lack additional resources to promote portal adoption.
CONCLUSION
MU policies contain an assumption that patients will follow a more or less straight path from information to enrollment to use. However, research has demonstrated that safety net patient populations face considerable barriers to using and benefitting from patient portals, including limited digital and health literacy,4,22,23 resulting in disparities in portal enrollment and use.24,25 Health systems that serve vulnerable populations may lack the capacity to overcome these barriers. Nonetheless, portals need to be made more broadly accessible if patients from all walks of life are to benefit from them. This will require involving patients in design and development efforts,26,27 tackling entrenched disparities in digital and health literacy, and increasing access to the Internet. If a national commitment to reducing the digital divide, and the socioeconomic inequities on which it is built, is not forthcoming, safety net health care providers will face an even steeper climb to Meaningful Use as defined by and for their patients.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank the clinicians, clinic staff, and patients who generously shared their time and perspectives with us.
COMPETING INTERESTS
The authors have no competing interests to declare.
Funding
This study was supported by a grant from the Agency for Healthcare Research and Quality (R24HS022047). DS was also supported by NIH grant R01LM012355.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
References
- 1. Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res. 2012;14:e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Medicare and Medicaid Services. Stage 2 Overview Tip Sheet. 2012. https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms/downloads/stage2overview_tipsheet.pdf. Accessed July 15, 2016.
- 3. Patel V, Barker W, Siminerio E. Disparities in individuals’ access and use of health IT in 2013. Office of the National Coordinator for Health IT. Washington, DC; 2015. https://www.healthit.gov/sites/default/files/briefs/oncdatabrief26june2015consumerhealthit.pdf. Accessed September 12, 2016.
- 4. Tieu L, Sarkar U, Schillinger D et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res. 2015;17:e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med. 2011;9:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bunce AE, Gold R, Davis JV et al. Ethnographic process evaluation in primary care: explaining the complexity of implementation. BMC Health Services Res. 2014;14:607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Swinglehurst D, Greenhalgh T, Myall M et al. Ethnographic study of ICT-supported collaborative work routines in general practice. BMC Health Services Res. 2010;10:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ackerman S, Gleason N, Gonzales R. Using rapid ethnography to support the design and implementation of health information technologies. Stud Health Technol Inform. 2015;215:14–27. [PubMed] [Google Scholar]
- 9. Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform. 1999;55:87–101. [DOI] [PubMed] [Google Scholar]
- 10. Wears RL, Berg M. Computer technology and clinical work: still waiting for Godot. JAMA. 2005;293:1261–63. [DOI] [PubMed] [Google Scholar]
- 11. Forsythe D. New bottles, old wine: hidden cultural assumptions in a computerized explanation system for migraine sufferers. Med Anthropol Quart. 2007;10:551–74. [DOI] [PubMed] [Google Scholar]
- 12. Akrich M. The description of technical objects. In Bijker WE, Law J, eds. Shaping Technology/Building Society. Cambridge, MA: MIT Press; 1992:205–24. [Google Scholar]
- 13. Ackerman SL, Tebb K, Stein JC et al. Benefit or burden? A sociotechnical analysis of diagnostic computer kiosks in four California hospital emergency departments. Social Sci Med. 2012;75:2378–85. [DOI] [PubMed] [Google Scholar]
- 14. Murray E, Burns J, May C et al. Why is it difficult to implement e-health initiatives? A qualitative study. Implement Sci. 2011;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Greenhalgh T, Russell J. Why do evaluations of ehealth programs fail? an alternative set of guiding principles. PLoS Med. 2010;7:e1000360. doi:10.1371/journal.pmed.100036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform. 2001;64:143–56. [DOI] [PubMed] [Google Scholar]
- 17. Greenhalgh T, Potts HWW, Wong G et al. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Quart. 2009;87:729–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cresswell KM, Sheikh A. Undertaking sociotechnical evaluations of health information technologies. Inform Primary Care. 2014;21:78–83. [DOI] [PubMed] [Google Scholar]
- 19. American Medical Association. Health IT Readiness Survey. https://www.stepsforward.org/modules/ehr-software-vendor-selection. Accessed December 2, 2016.
- 20. Corbin J, Strauss A. Basics of Qualitative Research. Thousand Oaks, CA: SAGE Publications; 2007. [Google Scholar]
- 21. Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36:391–409. [Google Scholar]
- 22. Czaja SJ, Zarcadoolas C, Vaughon WL et al. The usability of electronic personal health record systems for an underserved adult population. Hum Factors. 2015;57:491–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tieu L, Schillinger D, Sarkar U et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc. 2016;0:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goel MS, Brown TL, Williams A et al. Disparities in enrollment and use of an electronic patient portal. JGIM. 2011;26:1112–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yamin CK, Emani S, Williams DH et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–74. [DOI] [PubMed] [Google Scholar]
- 26. Ahern DK, Woods SS, Lightowler MC et al. Promise of and potential for patient-facing technologies to enable meaningful use. Am J Prevent Med. 2011;40:S162–72. [DOI] [PubMed] [Google Scholar]
- 27. Otte-Trojel T, de Bont A, van de Klundert J et al. Characteristics of patient portals developed in the context of health information exchanges: early policy effects of incentives in the meaningful use program in the United States. J Med Internet Res. 2014;16:e258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.