Abstract
BACKGROUND AND OBJECTIVES
Attention deficit hyperactivity disorder (ADHD) is the most commonly seen developmental disorder, with significant impacts on the child’s social, psychological, and scholastic functioning. The aim of this study was to determine the prevalence and sociodemographic correlates of ADHD in female primary schoolchildren.
DESIGN AND SETTING
A cross-sectional study conducted in Al-Khobar Town, Eastern Saudi Arabia.
METHODS
A random sample of six primary schools for girls was chosen, from which samples of 1009 students were selected by systematic random sampling, with ages ranging between 6 and 15 years (mean and standard deviation, 9.2 [1.9]). All subjects were screened for different types of ADHD using the Attention Deficit Disorders Evaluation Scale.
RESULTS
The overall prevalence of ADHD was 3.5%. The prevalence of children with ADHD/inattentive type was 2.1% and the prevalence of children with ADHD/hyperactive-impulsive type was 5.6%. This rate decreased significantly with increase in age. The prevalence was higher in government school students, among Saudi citizens, later born siblings, higher number of siblings, and lower parental education.
CONCLUSIONS
It was concluded that the prevalence of ADHD in female primary schoolchildren is comparable with what has been reported in other studies. Some demographic factors should be taken into consideration when interpreting this result. Implications and recommendations to the concerned authorities are outlined to improve the health and educational care services to help these children.
Attention deficit hyperactivity disorder (ADHD) is one of the most common neurobehavioral disorders in children and adolescents. Characterized by a pattern of extreme pervasive, persistent, and debilitating inattention, overactivity, and impulsivity (American Psychiatric Association, Diagnostic Statistical Manual of Mental Disorders, 4th edition [DSM-IV]),1 ADHD is described as having a substantial lifelong impact on social, emotional, vocational, and academic performance as well as the health system in general.2 This disorder represents a growing public health concern because of its long-term adverse effects, long-term treatment with behavior-modifying drugs, and the significant financial impact on family schools and community.
Studies on the etiology of ADHD have included neurobehavioral, biological/gestational, and genetic origins. Evidence for the role of noradrenalin in the etiology of ADHD comes from animal studies that have shown that decreased levels of noradrenalin within the brain results in hyperactivity and impulsivity.3 Genetic studies on the segregation analysis of the twins and adoption studies suggest that there is a heritable component in some children and adults and that the familial nature of ADHD has consistently been supported.4–7 Recent neuropsychological studies have also found deficits in executive functions, suggesting the involvement of the prefrontal lobe in the etiology of ADHD.8–10
ADHD is also associated with considerable impacts on social and academic success, as well as self-esteem, and is often associated with learning disabilities and comorbid behavioral disorders, which further impede the successful development of these persons.11 Issues of comorbidity, socioeconomic and educational costs, and impact of ADHD have been examined in many studies.11–13 Likewise, research has been carried out in relation to issues of management and assessments of ADHD.2,14,15
Although one of the most prevalent neurodevelopmental disorders, the prevalence of ADHD has received relatively less attention in international studies. However, the accumulating data vary between studies depending on methodological and other factors, such as the representing sample, the assessment, and the diagnostic tools and criteria.16 This variability in reported data is represented in studies carried out in America and in European, Asian, and Arab countries. However, the prevalence rate reported in children ranges from 3% to 5%, and 4% to 7%1,17 with a ratio of male to female of 3:1. Some studies reported a prevalence rate of up to 15%,18 and reports on the persistence of ADHD into adulthood are estimated to be 30% to 50% of the childhood cases.19
Some of these studies represent surveys of large representative samples. Examples of the large surveys in this area are the US National Health Interview Survey,20 which included 10 367 children aged 4 to 17 years with a response rate of 79.4%, and a lifetime prevalence of ADHD was reported by parents to be 7.8%. The second example is the survey of Mental Health of Children and Young People in Great Britain (British Survey),21 which included 10 438 children aged 4 to 16 years, with a response rate of 76%, and an overall prevalence rate for ADHD of 2.2%, with a strong gender effect (boys 3.6% vs girls 0.9%). The third large survey is represented by the German health and examination survey conducted by Huss et al.22 This survey covered a total of 17 461 children and adolescents (7569 boys and 7267 girls); with an overall lifetime prevalence of ADHD diagnosis being 4.8%.
Szatmari23 reviewed the findings of six large epidemiologic studies of ADHD and reported that the prevalence ranged from a low of 2% to a high of 6.3% with most falling within the range of 4.2% to 6.3%. In another systematic review Polanczyk et al reported that the worldwide pooled prevalence rate for ADHD was 5.29%.24 In their review they indicated that methodologic differences (including diagnostic criteria, source of information, and the requirement of impairment for diagnosis) explained more variance than the geographic origin of the study. A similar review, with similar conclusion, of worldwide prevalence studies has also been provided by Faraone et al.16 In a recent review of study on the prevalence of ADHD worldwide, Skounti et al noted that the prevalence of ADHD has been reported from 2.2% to 17.8%.25 These variations in the reported prevalence have been attributed to methodologic differences among the epidemiologic studies, such as using different assessment tools and diagnostic criteria, and variations in the representative samples.22,25,26
Prevalence studies on ADHD among Arab communities, especially the Gulf countries, are said to be scarce and have limited information.27 Examples of studies that have been carried out in the Arab Gulf communities include Bu-Haroon and her colleagues who studied the prevalence of symptoms of ADHD in the United Arab Emirates, with a sample of 1110 primary school students, and an overall prevalence reached 29.7%.28 In Qatar, the prevalence rate of ADHD was reported to be 11.1%.29
In Saudi Arabia, three studies exploring the prevalence of ADHD have been reported. Al-Haidar30 studied comorbidity and treatment characteristics of ADHD. Case records of 416 patients were reviewed; 25.5% were diagnosed to have ADHD, either as the only diagnosis (12.7%) or in combination with other psychiatric disorders. The most commonly associated disorder was expressive language disorder (28.3%), nocturnal enuresis (10.4%), mild mental retardation (38.7%), moderate mental retardation (12.3%), and severe mental retardation (1.9%). Al-Hamed et al31 studied the prevalence and some psychosocial factors of ADHD among male primary schoolchildren in Dammam City of Saudi Arabia. This was a school-based cross-sectional study, with a large sample size that included 1287 students with an age range between 6 and 13 years. The result of the study revealed an ADHD prevalence of 16.4%, an ADHD inattentive (IA) type of 16.3%, and a hyperactive-impulsive (HI) type of 12.4%. This could have been generalized to cover the population. Unfortunately, they studied only male children.
A recently published study by AlQahtani32 explored the prevalence of ADHD in primary schools in Saudi Arabia. Using a DSM-IV-based rating scale, the authors surveyed both teachers and parents to study the prevalence of ADHD for 708 primary school pupils. An overall rate of ADHD prevalence was 2.7%. The authors emphasized that applying a combination of reports from teachers and parents, the screening of ADHD is likely to be more accurate than reports by teachers or parents alone. However, it is clear that there is a paucity of scientific studies on the magnitude and the consequences of ADHD among schoolchildren in Saudi Arabia. ADHD is an important health problem among schoolchildren, and information on prevalence and patterns of the problem is needed so that there could be better planning of educational programs as part of multimodal treatment of ADHD. The present study explores the prevalence of ADHD among female primary schoolchildren and was conducted in the same area where the previous study was conducted.31
SUBJECTS AND METHODS
Ethical approval was obtained from the relevant health and education authorities to conduct the study, together with the permission of the Department of Family and Community Medicine. The various school administrators and the teachers were met so that the purpose of the study could be explained to them. A note was sent to all the parents of the children in the sample to explain the purpose of the study, and to assure them that all information would be strictly confidential and used only for research purposes.
The study population was composed of female governmental and nongovernmental primary schoolchildren between 6 and 15 years of age in Al-Khobar town, Eastern province of Saudi Arabia. After obtaining permission from the Research Department, Al-Dammam Branch of Ministry of Education, a random sample of six schools were chosen: five governmental schools and one private school. A total of six classes were randomly chosen, one from each grade in each school, by use of systematic random sampling. The children included in the study were chosen by a proportional allocation of the sample.
The Attention Deficit Disorders Evaluation Scale, school version,33 which has been translated and validated in Arabic by Al-Hamed et al31 was used as a data collection tool. The scale was requested by the researcher from Hawthorne Educational Service Inc., Colombia, MO, United States. The questionnaire consisted of two parts: Part I was concerned with measuring inattention and consisted of 29 questions. Part II was concerned with measuring hyperactivity-impulsivity and consisted of 31 questions. All the 60 questions were used to diagnose combined ADHD. The present authors used the same scoring procedure outline in the original manual; Al-Hamed and colleagues also used this procedure in their studies.31,33 In addition, we used a questionnaire of 12 questions eliciting demographic data on the student and related health information about the child.
RESULTS
A total of 948 female primary school girls were studied. Their ages ranged from 6 to 15 years of age with a mean (SD) age of 9.2 (1.9) years. The response rate for the two questionnaires was 948, representing 94% of the 1009 students. Most of the fathers (80%) and mothers (63%) were educated beyond the preparatory level. Only 5.6% of the schoolchildren had a positive history of chronic disease, including various types of diseases, such as bronchial asthma, heart disease, and anemia. Table 1 shows selected sociodemographic characteristics of the sample. For the purpose of further statistical analysis, the age factor was categorized into three subcategories (6–8, 9–11, and >12 years). Most of the students (64.7%) were Saudis and 35.2% were non-Saudis. Of those, 85.2% were in government schools and 14.8% were in nongovernment (private) schools. The mean number of siblings was 3.6 (2.3) with median of 5. Those who had <3 siblings represented 28.3%, those who had between 4 and 6 siblings were 44.2%, and those who had >6 siblings were 24.5%.
Table 1.
Selected sociodemographic characteristics.
| Demographic feature | Number (%) n = 948 |
|---|---|
|
| |
| Age (years) | |
| 6–8 | 363 (38.3) |
| 9–11 | 451 (47.6) |
| ≥12 | 134 (14.1) |
|
| |
| Nationality | |
| Saudi | 614 (64.8) |
| Non-Saudi | 334 (35.2) |
|
| |
| School type | |
| Governmental | 808 (85.2) |
| Nongovernmental | 140 (14.8) |
|
| |
| Number of siblings | |
| 1–3 | 268 (28.3) |
| 4–6 | 419 (44.2) |
| >6 | 261 (24.5) |
|
| |
| Birth order | |
| 1–3 | 535 (56.4) |
| 4–6 | 288 (30.4) |
| >6 | 125 (13.2) |
|
| |
| Father’s education | |
| Illiterate | 41 (4.3) |
| Read and write | 67 (7.1) |
| Primary | 121 (12.8) |
| Preparatory | 163 (17.2) |
| Secondary | 231 (24.4) |
| University | 325 (34.3) |
|
| |
| Total | 948 (100) |
|
| |
| Mother’s education | |
| Illiterate | 126 (13.3) |
| Read and write | 89 (9.4) |
| Primary | 135 (14.2) |
| Preparatory | 132 (13.9) |
| Secondary | 245 (25.8) |
| University | 221 (23.3) |
|
| |
| Total | 948 (100) |
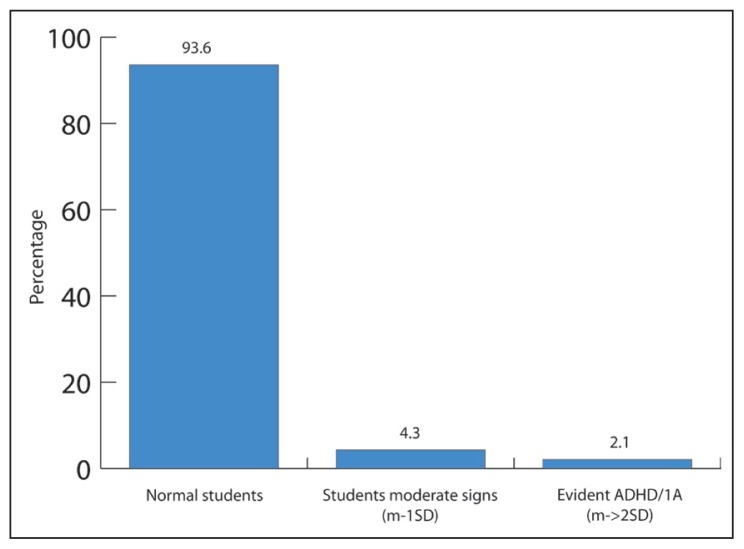
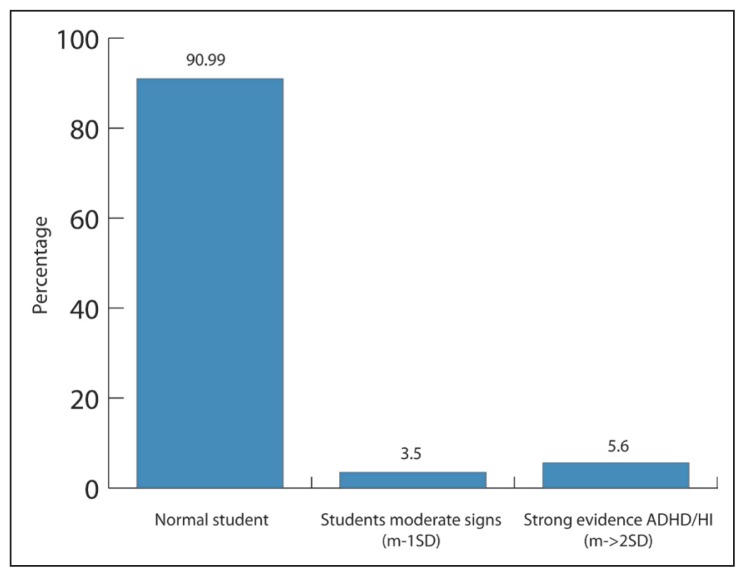
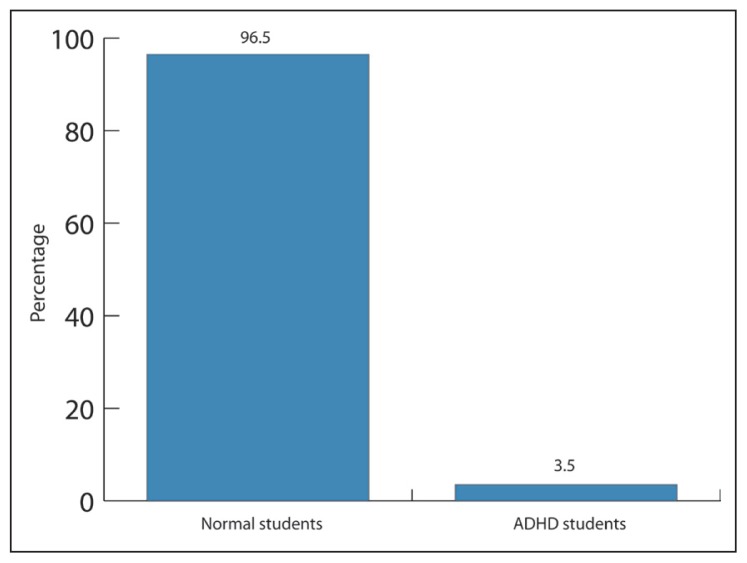
The overall prevalence of ADHD was 3.5%. The prevalence of children with ADHD/IA type was 2.1%, the prevalence of children with ADHD/HI type was 5.6%, and the prevalence of children with possible ADHD/CT was 3.5%. Figures 1–3 present the prevalence of different types of ADHD. Table 2 shows the relationship between different age groups and the prevalence of ADHD. The finding indicates that, although the prevalence rate decreases with increase in age, the only statistical difference appeared in the prevalence rate of ADHD/combined type (CT) (overall ADHD), which decreases with age (1.4% at age 6–8 years, 1.2% at age 9–11 years, and 1.1% at age >12 years), with χ2 of 7.8 and P=.02. Table 3 shows the relationship between the number of the siblings and the prevalence of ADHD. The overall ADHD rate was 4 times (1.6%) more in the larger family than in the smaller families (0.4%) (χ2=7.2, P value=.028). Table 4 shows the relationship between the birth order of the children and the prevalence of ADHD. The finding reveals that there are statistically significant relationships between birth order and the prevalence of ADHD. The rate of ADHD increases with the later birth order, (0.6%–1.6%, P value=.021). The percentile of positive ADHD reflects the same trends (an increase in the rate from 0.5%–1.6%).
Figure 1.
Prevalence of ADHD/IA type
Figure 2.
Prevalence of ADHD/HI type
Figure 3.
Prevalence of ADHD/CT (overall)
Table 2.
Relationship between different age groups and the prevalence of ADHD.
| ADHD type | Age (years) | χ2 | P | ||
|---|---|---|---|---|---|
| 6–8 | 9–11 | ≥12 | |||
|
| |||||
| n=363 (38.3%) | n=451 (47.6%) | n=134 (14.1%) | |||
| ADHD/IA | |||||
| Normal | 344 (36.3) | 423 (44.6) | 120 (12.7) | 4.6 | .331 |
| Possible | 13 (1.4) | 19 (2) | 9 (0.9) | ||
| Serious signs | 6 (0.6) | 9 (0.9 | 5 (0.5) | ||
|
| |||||
| ADHD/HI | |||||
| Normal | 330 (34.8) | 417 (44) | 115 (12.1) | 7.4 | .118 |
| Possible | 10 (1.1) | 16 (1.7) | 7 (0.7) | ||
| Serious signs | 23 (2.4) | 18 (1.9) | 12 (1.3) | ||
|
| |||||
| ADHD/CT | |||||
| Normal | 351 (37) | 440 (46.4) | 124 (13.1) | 7.8 | .020 |
| Positive ADHD | 13 (1.4) | 11 (1.2) | 10 (1.1) | ||
|
| |||||
| Percentile | |||||
| Normal | 352 (37.1) | 440 (46.4) | 124 (13.1) | 8.2 | .17 |
| Positive ADHD | 11 (1.2) | 11 (1.2) | 10 (1.1 | ||
Values are n (%).
Table 3.
Relationship between number of the students’ siblings and the prevalence of ADHD.
| ADHD type | Number of siblings | χ2 | P | ||
|---|---|---|---|---|---|
| 1–3 n=268 (28.3%) |
4–6 n=419 (44.2%) |
>6 n=261 (27.5%) |
|||
|
| |||||
| ADHD/I | |||||
| Normal | 259 (27.3) | 393 (41.5) | 235 (24.8) | 11.1 | .026 |
| Moderate signs | 8 (0.8) | 16 (1.7) | 17 (1.8) | ||
| Serious signs | 1 (0.1 | 10 (1.1) | 9 (0.9) | ||
|
| |||||
| ADHD/HI | |||||
| Normal | 257 (27.1) | 384 (40.5) | 221 (23.3) | 22.3 | .001 |
| Moderate signs | 2 (0.2) | 16 (1.7) | 15 (1.6) | ||
| Serious signs | 9 (0.9) | 19 (2) | 25 (2.6) | ||
|
| |||||
| ADHD/C | |||||
| Normal | 264 (27.8) | 405 (42.7) | 246 (25.9) | 7.2 | .028 |
| Positive ADHD | 4 (0.4) | 14 (1.5) | 15 (1.6) | ||
|
| |||||
| Percentile | |||||
| Normal | 265 (28) | 405 (42.7) | 246 (25.9) | 8.7 | .013 |
| Positive ADHD | 3 (0.3) | 14 (1.5) | 15 (1.6) | ||
Values are n (%).
Table 4.
Relationship between student birth order and the prevalence of ADHD.
| ADHD type | Age (years) | χ2 | P | ||
|---|---|---|---|---|---|
| 1–2 n=379 (40%) |
3–4 n=298 (31.4%) |
>5 n=271 (28.6%) |
|||
|
| |||||
| ADHD/IA | |||||
| Normal | 362 (38.2) | 281 (29.6) | 244 (25.7) | 9.99 | .04 |
| Moderate signs | 13 (1.4) | 12 (1.3) | 16 (1.7) | ||
| Serious signs | 4 (0.4) | 5 (0.5) | 11 (1.2) | ||
|
| |||||
| ADHD/HI | |||||
| Normal | 355 (37.4) | 272 (28.7) | 235 (24.8) | 11.0 | .027 |
| Moderate signs | 12 (1.3) | 8 (0.8) | 13 (1.4) | ||
| Serious signs | 12 (1.3) | 18 (1.9) | 23 (2.4) | ||
|
| |||||
| ADHD/CT | |||||
| Normal | 373 (39.3) | 286 (30.2) | 256 (27) | 7.73 | .021 |
| Positive ADHD | 6 (0.6) | (1.3) | 15 (1.6) | ||
|
| |||||
| Percentile | |||||
| Normal | 374 (39.5) | 386 (30.2) | 256 (27) | 9.17 | .01 |
| Positive ADHD | 5 (0.5) | 12 (1.3) | 15 (1.6) | ||
Values are n (%)
DISCUSSION
The aim of this study was to explore the prevalence of ADHD among female primary schoolchildren in Al-Khobar town, Eastern province of Saudi Arabia, and to examine some sociodemographic correlates of this prevalence. The finding of this study was that the overall prevalence of ADHD in female students aged between 6 and 15 years was 3.5%. This rate is comparable to that reported in local studies.32 The students with moderate signs of ADHD/IA (1 SD below the mean) were 4.3% and those with strong evidence of serious signs of ADHD/IA were 2.1%. With regard to ADHD/HI, 3.5% of students had moderate signs and 5.6% of them had serious signs and evidence of ADHD/HI (>2 SD below the mean). It is unrealistic to compare the present findings with other studies that focused on both boys and girls unlike this study that focused only on girls. However, this prevalence rate is not surprising because it gave a ratio of 1:5 when compared with the reported rate of ADHD in boys (16.7%) in Dammam.31 This ratio is also comparable with other international studies in which the ratio between boys and girls ranged from 1:3 to 1:10, depending on whether the study was clinically based or community based. The variation of the prevalence of ADHD also characterized the reported international and regional studies.22,25,26,34
Table 2 shows the relationship between different age groups and the prevalence of ADHD. It is clear that the rate of ADHD decreases with age. The results on the CT and the percentile index show that the symptoms of ADHD are mostly obvious in the age group 6 to 11 years when diagnosis is recommended.35 In addition, this result is comparable to other studies that indicated that ADHD is more prominent in this age group and that its symptoms start regressing at or after the age of 12 years.33,34,36,37 This finding is also comparable to that of the Dammam study in which most of the ADHD children were aged 9 to 11 years. This finding highlights the importance of the role of educational personnel, especially teachers in noticing children with ADHD as early as possible.
Our findings revealed a statistically significant relationship between the number of siblings and the prevalence of ADHD/IA, ADHD/HI, and ADHD/CT, in which children in small families had a lower rate of ADHD than children in larger families. This means that the possibility of having ADHD children might be lessened as the family size decreases. As shown in Table 3, the overall ADHD rate was 4 times (1.6%) more in larger families than in the smaller families (0.4%) (χ2 = 7.2, P value=.028). It is possible that the care needed by children is more likely to be afforded when the size of the family is smaller. The larger the family size, the lesser care the child receives and the greater the behavioral problems observed, ADHD being one of those problems.38
The results suggest that the risk of showing serious signs of behavioral problems related to ADHD increased with the order of the birth. These results could be explained in relation to the findings of other studies, which maintained that as the family size increases, the chances of a child having good care decreases resulting in the physical, psychological, and social health of the child.37,39
The associations in this study should not be considered as cause-effect relationships, as they are based on correlation analysis. However, these findings might highlight the relationships between social factors and certain “problem behaviors” that are seen in children with ADHD and other disorders, such as oppositional defiant and conduct disorders. The findings of the present study highlight the importance of increasing efforts of health and education authorities to provide necessary tools and means for early identification and management of ADHD. It is essential for health practitioners, primary care pediatricians, child psychiatrists, and psychologists, as well as special educationists, to have enhanced training in the identification and management of ADHD. Clinicians are also encouraged to develop culturally suitable assessments and screening tools for ADHD. Linguistic and psychometric adaptation of ADHD scales to Arabic language would be a valuable addition toward better understanding and management of ADHD in Arab communities.
One of the major limitations of this study is that it is based on a screening tool used to interview only parents and/or teachers. Although it is essential to involve teachers and parents in the evaluation process of ADHD, it is equally important to confirm the diagnoses by professionally trained mental health clinicians. In our study, this was not feasible because of the large size of the sample and for other practical reasons. This might be a serious limitation, and we recommend that future studies should include mental health clinicians in the assessment procedure. However, although several community-based surveys have used screening tests to have estimates of ADHD prevalence,16,22,24 it is agreed that these studies faced some methodological limitations in revealing accurate prevalence estimates. Another limitation of this study is being limited to female subjects; future research should include more representative sample of both male and female subjects. It is possible that improved operationalization of symptoms could lead to increased measurement precision and a better assessment of the cross-national validity of diagnostic categories.
Finally, a methodologic point is related to the accuracy of rating scales that were originally developed in another language and translated into Arabic. Despite attempts to examine certain aspects of the psychometric properties of such scales (eg, as in Al-Hamed et al31), limitations of these scales have been rightly highlighted by other authors.40 Future research should consider detailed evaluations of the more psychometric and linguistic validation of such scales.
REFERENCES
- 1.American Psychiatric Association. Diagnostic And Statistical Manual Of Mental Disorders (DSM-IV) 4th ed. Washington, DC: APA; 1994. pp. 78–85. [Google Scholar]
- 2.Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. USA: The Guilford Press; 1998. [Google Scholar]
- 3.Castellanos FX. Toward a pathophysiology of attention deficit hyperactivity disorder. Clin Pediatr (Phila) 1997;36:381–93. doi: 10.1177/000992289703600702. [DOI] [PubMed] [Google Scholar]
- 4.Faraone SV, Doyle AE, Mick E, Biederman J. Meta-analysis of the association between the 7-repeat allele of the dopamine d(4) receptor gene and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1052–7. doi: 10.1176/appi.ajp.158.7.1052. [DOI] [PubMed] [Google Scholar]
- 5.Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57:1313–23. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 6.Larsson H, Lichtenstein P, Larsson JO. Genetic contributions to the development of ADHD subtypes from childhood to adolescence. J Am Acad Child Adolesc Psychiatry. 2006;45:973–81. doi: 10.1097/01.chi.0000222787.57100.d8. [DOI] [PubMed] [Google Scholar]
- 7.Thapar A, Langley K, O’donovan M, Owen M. Refining the attention deficit hyperactivity disorder phenotype for molecular genetic studies. Mol Psychiatry. 2006;11:714–20. doi: 10.1038/sj.mp.4001831. [DOI] [PubMed] [Google Scholar]
- 8.Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- 9.Durston S. A review of the biological bases of ADHD: What have we learned from imaging studies? Ment Retard Dev Disabil Res Rev. 2003;9:184–95. doi: 10.1002/mrdd.10079. [DOI] [PubMed] [Google Scholar]
- 10.Frazier TW, Youngstrom EA, Naugle RI. The latent structure of attention-deficit/hyperactivity disorder in a clinic-referred sample. Neuropsychology. 2007;21:45–64. doi: 10.1037/0894-4105.21.1.45. [DOI] [PubMed] [Google Scholar]
- 11.Spencer TJ. ADHD and comorbidity in childhood. J Clin Psychiatry. 2006;67(Suppl 8):27–31. [PubMed] [Google Scholar]
- 12.Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice, and DSM-IV. J Am Acad Child Adolesc Psychiatry. 1997;36:1065–79. doi: 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Leibson CL, Katusic SK, Barbaresi WJ, Ransom J, O’Brien PC. Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder. JAMA. 2001;285:60–6. doi: 10.1001/jama.285.1.60. [DOI] [PubMed] [Google Scholar]
- 14.Brown RT, Levers CE. Psychotherapy and pharmacotherapy treatment outcome research in pediatric populations. J Clin Psychol Med Settings. 1999;6:63–88. [Google Scholar]
- 15.DuPaul GJ, Stoner G. ADHD in the schools: Assessment and intervention strategies. 2nd Ed. New York, NY: Guilford; 2003. [Google Scholar]
- 16.Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2:104–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Nolan EE, Gadow KD, Sprafkin J. Teacher reports of DSM-IV ADHD, ODD and CD symptoms in schoolchildren. J Am Acad Child Adolesc Psychiatry. 2001;40:241–9. doi: 10.1097/00004583-200102000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Wolraich ML, Hannah JN, Baumgaertel A, Feuer ID. Examination of DSM-IV criteria for attention deficit/hyperactivity disorder in a county-wide sample. J Dev Behav Pediatr. 1998;19:162–8. doi: 10.1097/00004703-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Searight HR, Burke JM, Rottnek F. Adult ADHD: Evaluation and treatment in family medicine. Am Fam Physician. 2000;62:2077–86. [PubMed] [Google Scholar]
- 20.Cuffe SP, Moore CG, McKeown RE. Prevalence and correlates of ADHD symptoms in the national health interview survey. J Atten Disord. 2005;9:392–401. doi: 10.1177/1087054705280413. [DOI] [PubMed] [Google Scholar]
- 21.Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry. 2003;42:1203–11. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Huss M, Hölling H, Kurth BM, Schlack R. How often are German children and adolescents diagnosed with ADHD ? Prevalence based on the judgment of health care professionals: Results of the German health and examination survey (KiGGS) Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):52–8. doi: 10.1007/s00787-008-1006-z. [DOI] [PubMed] [Google Scholar]
- 23.Szatmari P. The epidemiology of attention-deficit hyperactivity disorders. In: Weiss G, editor. Child and adolescent psychiatric clinics of North America: Attention-deficit hyperactivity disorder. Philadelphia: Saunders; 1992. pp. 361–72. [Google Scholar]
- 24.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 25.Skounti M, Philalithis A, Galanakis E. Variations in prevalence of attention deficit hyperactivity disorder worldwide. Eur J Pediatr. 2007;166:117–23. doi: 10.1007/s00431-006-0299-5. [DOI] [PubMed] [Google Scholar]
- 26.Scahill L, Schwab-Stone M. Epidemiology of ADHD in school-age children. Child Adolesc Psychiatr Clin N Am. 2000;9:541–55. [PubMed] [Google Scholar]
- 27.Sayal K, Hornsey H, Warren S, Macdiarmid F, Taylor E. Identification of children at risk of attention deficit/hyperactivity disorder, a school based intervention. Soc Psychiatry Epidemiol. 2006;41:806–13. doi: 10.1007/s00127-006-0100-0. [DOI] [PubMed] [Google Scholar]
- 28.Bu-Haroon A, Eapen V, Bener A. The prevalence of hyperactivity symptoms in the United Arab Emirates. Nordic J Psychiatry. 1999;53:439–42. [Google Scholar]
- 29.Bener A, Al Qahtani R, Teebi AS, Bessisso M. The Prevalence of Attention Deficit Hyperactivity Symptoms in Schoolchildren in a Highly Consanguineous Community. Med Princ Pract. 2008;17:440–6. doi: 10.1159/000151564. [DOI] [PubMed] [Google Scholar]
- 30.Al-Haidar FA. Co-morbidity and treatment of attention deficit hyperactivity disorder in Saudi Arabia. East Mediterr Health J. 2003;9:988–95. [PubMed] [Google Scholar]
- 31.Al-Hamed JH, Taha AZ, Sabra AA, Bella H. Attention Deficit Hyperactivity Disorder (ADHD): Is it a Health Problem among Male Primary School Children? Bahrain Med Bull. 2008;30:1–9. [PubMed] [Google Scholar]
- 32.AlQahtani MM. Attention-deficit hyperactive disorder in school-aged children in Saudi Arabia. Eur J Pediatr. 2010;169:1113–7. doi: 10.1007/s00431-010-1190-y. [DOI] [PubMed] [Google Scholar]
- 33.McCarney SB. School Version Technical Manual. 2nd edition. Published by Hawthorne Educational Services Inc; 1995. The Attention Deficit Disorders Evaluation Scale. [Google Scholar]
- 34.Döpfner M, Breuer D, Wille N, Erhart M, Ravens-Sieberer U The BELLA study group. How often do children meet ICD-10/DSM-IV criteria of attention deficit/hyperactivity disorder and hyperkinetic disorder? Parent-based prevalence rates in a national sample – results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):59–70. doi: 10.1007/s00787-008-1007-y. [DOI] [PubMed] [Google Scholar]
- 35.Cantwell DP. ADHD, A Review Of The Past 10 Years. J Am Acad Child Adolesc Psychiatry. 1996;35:978–87. doi: 10.1097/00004583-199608000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Buckley S, Hillery J, Guerin S, McEvoy J, Dodd P. The prevalence of features of attention deficit hyperactivity disorder in a special school in Ireland. J Intellect Disabil Res. 2008;52:156–62. doi: 10.1111/j.1365-2788.2007.01017.x. [DOI] [PubMed] [Google Scholar]
- 37.Faisal M, El Zarrad KH. Children. Sharjah, UAE: Sharjah City for Humanitarian Services; 2002. Hyperactivity, Attention Deficit, And Impulsive Control Disorder. [Google Scholar]
- 38.Hartung CM, Willcutt EG, Lahey BB, Pelham WE, Loney J, Stein MA, et al. Sex differences in young children who meet criteria for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2002;3:453–64. doi: 10.1207/S15374424JCCP3104_5. [DOI] [PubMed] [Google Scholar]
- 39.Teeter PA. Interventions for ADHD: Treatment In Developmental Context. New York NY: The Guilford Publication Inc; 1998. [Google Scholar]
- 40.Hassan AM, Al-Haidar F, Al-Alim F, Al-Hag O. A screening tool for attention deficit hyperactivity disorder in children in Saudi Arabia. Ann Saudi Med. 2009;29:294–8. doi: 10.4103/0256-4947.55321. [DOI] [PMC free article] [PubMed] [Google Scholar]