Abstract
Background:
To compare the clinical values of bronchoscopic sputum suction and general sputum suction in respiratory failure patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) combined with sequential invasive–noninvasive mechanical ventilation at the pulmonary infection control (PIC) window (period of lower sputum production, with thinner viscosity and lighter color, and alleviated clinical signs of infection).
Methods:
Patients with AECOPD-induced respiratory failure received orotracheal intubation mechanical ventilation and were randomly divided into bronchoscopic sputum suction group or general sputum suction group, and who were then treated with sequential invasive–noninvasive mechanical ventilation at PIC window (both groups). Baseline data, postoperative blood gas conditions, and postoperative clinical parameters of the patients such as appearance of PIC window, time of invasive ventilation, total time of ventilation, hospital stay, weaning success rate, reintubation rate, ventilator-associated pneumonia (VAP) incidence, and fatality rate were measured to compare the effect of 2 different ways of sputum suction.
Results:
There was no significant difference in baseline characteristics, postoperative blood gas conditions, between 2 groups (all P > .05). Nevertheless, the bronchoscopic sputum suction group showed earlier appearance of PIC window, shorter time of invasive ventilation, total time of ventilation and hospital stay, lower reintubation rate, VAP incidence and fatality rate, and higher weaning success rate than the general sputum suction group (all P < .05).
Conclusion:
Bronchoscopic sputum suction combined with sequential invasive–noninvasive mechanical ventilation at PIC window showed clinical effects in treating respiratory failure patients with AECOPD.
Keywords: bronchoscopy, sputum, ventilation
1. Introduction
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD), characterized by changes of sputum production, dyspnea, and cough, is the major cause of death in elderly patients worldwide.[1] Moderate to severe AECOPD can lead to acute respiratory failure,[2] and ventilator support (noninvasive or invasive) is required to assist spontaneous breathing.[3] Invasive positive pressure ventilation (IPPV) is the first choice to relieve the airway obstruction and remove the airway secretions. Nevertheless, although the strategy is effective, the risk of complications (such as sinusitis, respiratory muscle weakness, and ventilator-associated pneumonia [VAP]) remains significant. VAP incidence has been reported in 32% to 46% of patients receiving ventilation for more than 14 days, and results in recurrent disease, postponed weaning time, and ventilator dependency.[4,5]
In recent years, noninvasive positive pressure ventilation (NIPPV) and the sequential invasive–noninvasive mechanical ventilation strategy have been shown to reduce the complications, shortening the retention time of the invasive artificial airway and lowering mortality.[6] Nevertheless, the optimal timing for this invasive to noninvasive switch still needs to be elucidated. In patients receiving invasive mechanical ventilation, the pulmonary infection control (PIC) window refers to a period of time during which the bronchial-pulmonary infection is under control, as shown by reduced amount of sputum production and with thinner viscosity and lighter color, decreased body temperature and white blood cells (WBCs), and diminished lung radiographic infiltrates.[7] It is advocated that the PIC window may be considered as the optimal timing for switching from invasive to noninvasive mechanical ventilation in patients with AECOPD.[8] In patients with AECOPD, sputum accumulates in the lower airways and will inevitably cause severe respiratory obstruction, atelectasis, pulmonary infection, and ventilator fatigue, leading to weaning failure and offline difficulty.[9] Therefore, removing the sputum is important for patient management, but blind negative pressure aspiration can damage the airway mucosa and leave sputum in place, worsening the patient's condition. Removing sputum under bronchoscopy could allow the precise removal of all sputum while minimizing mucosa damage.
Therefore, the aim of the present study was to assess the major clinical indicators (such as the appearance of the PIC window, time of invasive ventilation, and length of hospital stay) to compare the effect of 2 different ways for sputum suction (bronchoscopy-assisted vs negative pressure aspiration).
2. Materials and methods
2.1. Study design and subjects
This study is strictly designed as a randomized controlled study. A total of 107 respiratory failure patients with AECOPD admitted to the intensive care unit (ICU) of The Coal Group General Hospital between January 2014 and December 2016 were selected and randomly allocated to the bronchoscopic sputum suction group or general sputum suction group. Patients received orotracheal or nasotracheal intubation mechanical ventilation based on the standard of invasive mechanical ventilation.[10,11] Diagnosis of AECOPD was made according to The global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary diseases: GOLD executive summary.[12]
The inclusion criteria were: diagnosis of AECOPD; <85 years of age; diagnosed with acute respiratory failure based on arterial partial pressure of oxygen (PaO2) <60 mm Hg (1 mm Hg = 0.133 kPa) with or without arterial partial pressure of carbon dioxide (PaCO2) > 50 mm Hg; and treated with invasive mechanical ventilation by tracheal intubation.
The exclusion criteria were: any neurologic diseases other than pulmonary encephalopathy; severe arrhythmia and myocardial infarction, with or without pulmonary infarction; upper gastrointestinal perforation infarction and hemorrhage, with or without recent gastrointestinal surgery; or patients who were unable to wear nasal/facial mask due to facial injury or deformity.
The PIC window was defined as: consciousness, powerful sputum, and stable hemodynamics; significantly diminished bronchial-pulmonary infection shadow in X-ray chest film, with absence of fusion patches; accompanied by 2 or more of the following indicators: body temperature <38.0°C; peripheral WBC count <10.0 × 109/L, or percentage of neutrophils <78.0%; and sputum significantly reduced, turned white or lighter, viscosity decreased to below II degree.[13]
This study has been approved by the Institutional Review Board of the Coal Group General Hospital. All patients assigned the informed consent form before being enrolled in the study.
2.2. Grouping and intervention
Patients were divided into 2 groups using a random number table. The bronchoscopy group consisted of 42 patients who received orotracheal intubation by means of sputum suction and bronchial alveolar lavage (BAL) under bronchoscopy. Forty cases in the general group received the same intubation by direct laryngoscopy and sputum was routinely aspirated by negative pressure suction (Fig. 1). All patients were routinely intubated using a laryngoscope.
Figure 1.
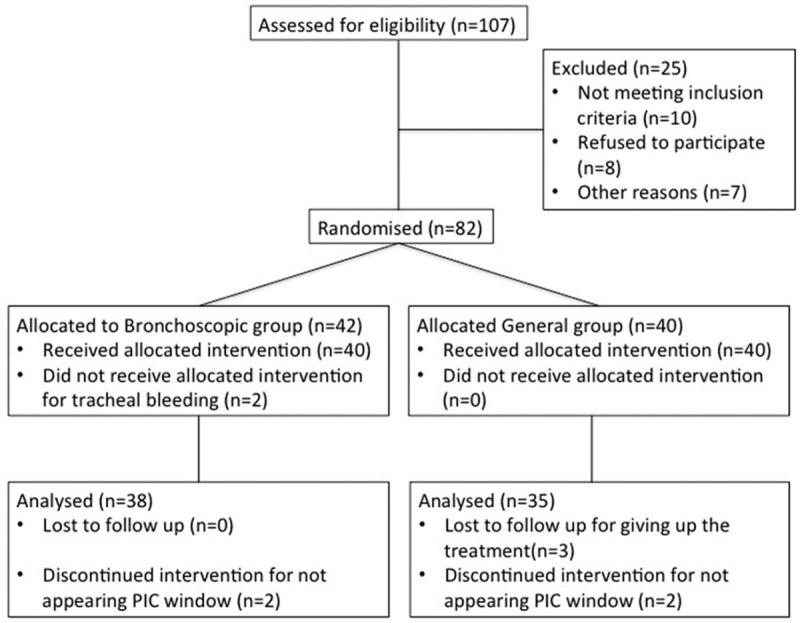
Grouping chart flow. PIC = pulmonary infection control.
In the bronchoscopy group, daily routine sputum suction was performed using a PENTAX FB-15BS portable fiber bronchoscopy (PENTAX Medical Shanghai Co, Ltd, Shanghai, China) through tracheal intubation at least once. Patients were in the supine position and under sedation. The ventilator settings were: volume control ventilation (VCV), tidal volume (VT) 7–10 mL/kg, respiratory rate 16 times/min, positive end-expiration pressure (PEEP) 0 mm Hg, and FiO2 100%. Under continuous mechanical ventilation, the bronchoscope was inserted in the endotracheal tube. The disposable sputum cups were connected with the bronchoscope and the negative pressure. Sputum was aspirated under direct vision. In addition, conventional negative pressure suction was performed according to patients’ situation. When patients showed the PIC window, the tracheal tube was removed and switched to noninvasive ventilation using the Vision ventilator.
In the general group, the intubation was completed in the same way as in the bronchoscopic group and then followed by connection to a ventilator (Vision, Wellkang, Melbourne, FL) for invasive ventilation. When the PIC window appeared, the tracheal tube was removed and the patient changed to noninvasive ventilation with the Vision ventilator. Daily routine sputum suction was performed by conventional negative pressure suction.
The patients in both groups were switched to noninvasive mechanical ventilation after the PIC window appeared. For weaning, the A/C mechanical ventilation mode was adopted for 4 to 12 hours, and then changed to the synchronized intermittent mandatory ventilation (SIMV)+ pressure support ventilation (PSV) mode. The SIMV frequency and PSV level were gradually reduced according to the patient's condition and improvement of ventilation function, until the SIMV frequency dropped to 10 to 12 times/min, and the PSV level was no longer down after 10 to 12 cmH2O. After reaching these above conditions and with the appearance of the PIC window, the tracheal cannula was removed and replaced by noninvasive bi-level positive pressure ventilation.
2.3. Follow-up and outcome indicators
The patients were followed for 20 days. The primary endpoint was the appearance of the PIC window. The secondary endpoint was the time of invasive ventilation, total time of ventilation, hospital stay, weaning success rate, VAP incidence, and fatality rate. VAP was defined as pneumonia occurring >48 hours after endotracheal intubation. To assess the safety of the operation between the 2 groups, we chose 11 main complications and incidents which were most possibly related: reflexive respiratory/cardiac arrest, upper respiratory tract injury (pain, hemorrhage infection, etc), bleeding in airway, asphyxia, arrhythmia, blood pressure fluctuation, cerebrovascular accident, shock, pneumothorax or blood pneumothorax, mediastinal or subcutaneous emphysema, and vomiting.
2.4. Statistical analysis
Statistical analyses were performed using GraphPad Prism 6.0 (GraphPad Software, Inc, www.graghpad.com/prism). Categorical data were presented as n (%) and analyzed using the Chi-squared test. Continuous data were submitted to a normal distribution test. Those in line with normal distribution were presented as mean ± standard deviation and analyzed using the Student t test, while those not meeting the normal distribution were expressed as median and range, and analyzed with nonparametric test. A difference with P < .05 was considered statistically significance.
3. Results
3.1. Baseline characteristics
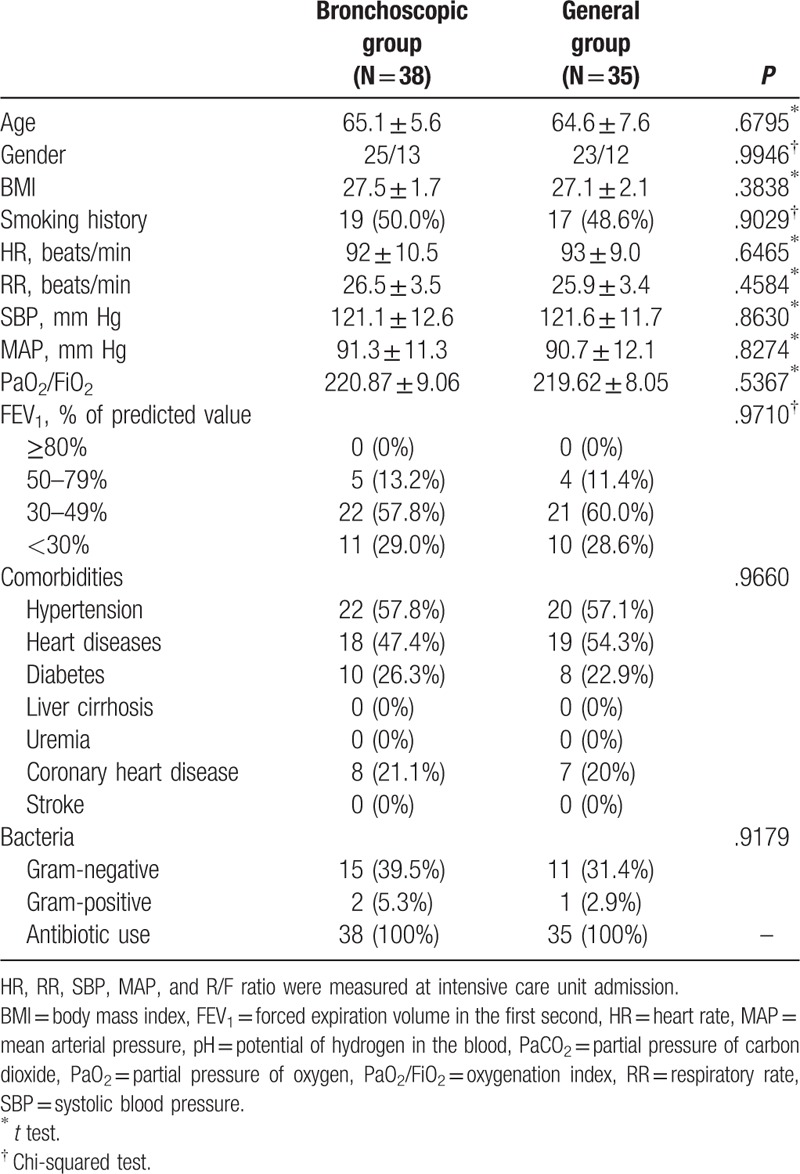
There were 38 and 35 patients in the bronchoscopic and general groups, respectively, with complete data that could be analyzed (Fig. 1). There were no significant differences in general characteristics including age, gender, body mass index (BMI), smoking history, lung function, and comorbidities between the 2 groups (all P > .05) (Table 1). No significant differences were observed between the 2 groups regarding blood gas, heart rate, and respiration-related indicators such as systolic blood pressure, mean arterial pressure, and oxygenation index (all P > .05).
Table 1.
General data of bronchoscopic group and general group.
3.2. Postoperative clinical indicators
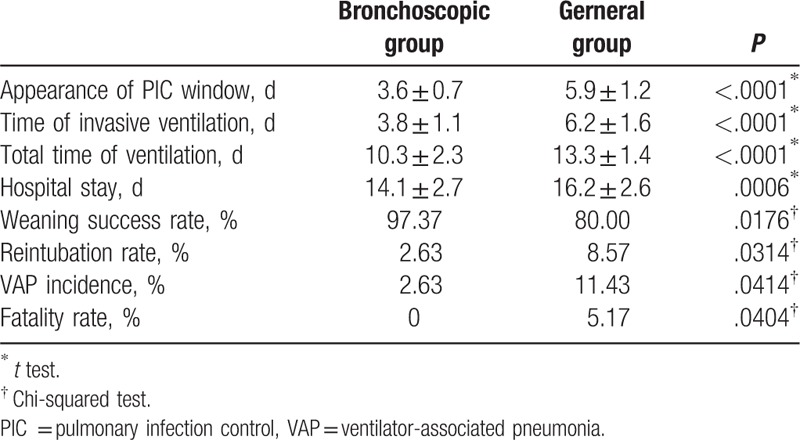
Compared with patients in the general sputum suction group, the appearance of PIC window was earlier by almost 2 days after sputum aspiration in the bronchoscopy group (3.6 ± 0.7 vs 5.9 ± 1.2, P < .05). Time of invasive ventilation and total time of ventilation were shorter (3.8 ± 1.1 vs 6.2 ± 1.6 and 10.3 ± 2.3 vs 13.3 ± 1.4, respectively; both P < .05). The general sputum suction group showed prolonged length of hospital stay (14.1 ± 2.7 vs 16.2 ± 2.6) and increased VAP incidence (2.63% vs 11.43%) (P < .05), following lower weaning success rate (80% vs 97.37%, P < .05) and higher fatality rate (5.17% vs 0, P < .05) (Table 2).
Table 2.
Postoperative clinical indicators between bronchoscopic group and general group.
3.3. Preoperative and postoperative blood gas analyses
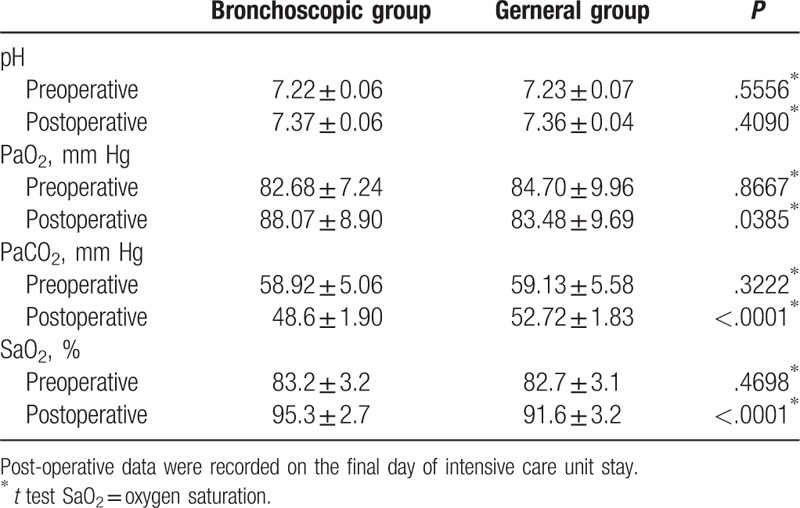
The arterial blood gas and oxygen saturation were examined before and after sputum aspiration. Sputum aspiration by bronchoscopy was more effective for sputum removal according to PaCO2 (48.6 ± 1.90 vs 52.72 ± 1.83, P < .05). Although patients improved after operation, there were no differences between the 2 groups (P > .05) (Table 3).
Table 3.
Preoperative and postoperative blood gas analyses.
3.4. Safety assessments
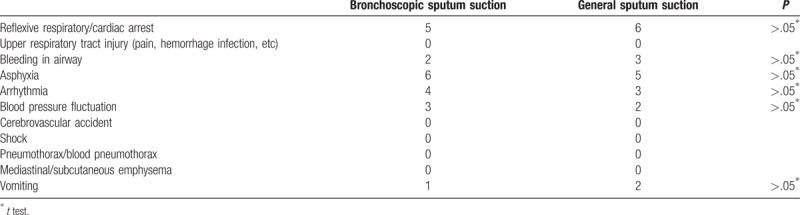
Patients in both groups showed reflexive respiratory/cardiac arrest (5 in the bronchoscopy group and 6 in the general group), bleeding in airway (2 vs 3), asphyxia (6 vs 5), arrhythmia (4 vs 3), blood pressure fluctuation (3 vs 2), and vomiting (1 vs 2), but there were no differences between the 2 groups (all P > .05) (Table 4). No patient showed upper respiratory tract injury (pain, hemorrhage infection, etc), cerebrovascular accident, shock, pneumothorax/blood pneumothorax, and mediastinal/subcutaneous emphysema.
Table 4.
Analyses of safety assessments.
4. Discussion
In this study, we found that using bronchoscopy to remove sputum is an effective way during invasive ventilation in respiratory failure patients with AECOPD and plays important roles in reaching an early PIC window for switching to noninvasive mechanical ventilation. Bronchoscopic sputum suction showed encouraging results and great advantage in various indicators, such as shortening the time of invasive ventilation and the length of hospital stay, and improving the weaning success rate.
The IPPV is associated with a high risk of VAP and increased mortality rate despite of effectively relieving respiratory obstruction or failure in patients with AECOPD.[14] Prolonged invasive ventilation may be a consequence of respiratory muscle fatigue and cause weaning failure and offline difficulty. Thus, to avoid this dilemma situation, it is imperative to find out an optimal timing for early extubation to NIPPV ventilation. Noninvasive mechanical ventilation is more compatible under physiologic situation by relieving the respiratory work consumption for patients with AECOPD.[15,16] The PIC window concept was put forward for this purpose.[7,17] This idea was first proposed by Wang et al, and is a period of time during which bronchial-pulmonary infection is under control, as shown by reduced amount of sputum production, decreased body temperature, WBC counts, and diminished lung radiographic infiltrates in patients with consciousness, powerful sputum and stable hemodynamics.[18] Wang et al favorably regarded the PIC window as a significant timing to decrease the invasive and total durations of ventilatory support, the risk of VAP, and the duration of ICU stay. The PIC window is used more and more increasingly for those who cannot reach the extubation criteria. Several studies confirmed that the PIC window was more feasible to adapt in the treatment of the patient with obvious bronchial pulmonary infection, and for those who are not affected significantly by pulmonary infection still can be applied by 2 hours spontaneous breathing trial (SBT-2).[19]
In the present study, we found an earlier PIC window and more positive secondary endpoints such as shorter time of invasive ventilation, total time of ventilation and hospital stay, lower reintubation rate, VAP incidence and fatality rate, and higher weaning success rate in bronchoscopic group than which in the general group. We attribute these positive results to the reasons that sputum suction under bronchoscopy would have a direct view of the sputum position and readily to smooth the respiratory tract. BAL can be used to dilute the sputum and make it easy for aspiration. In addition, BAL fluid can stimulate cough with some anti-inflammatory effect and improve the function of the lung such as correcting hypoxemia and exert its diagnostic function.[20] Moreover, through bronchoscopy, forceps can be applied to clamp the thick and viscous sputum due to weak cough and gathering in the lungs and small bronchial phlegm.[21] Combined with systemic application of antibiotics, the anti-inflammatory drugs could reached the distal area of the lung, attenuating the mucosa edema, and shortening the course of the disease. Compared with general sputum suction, the operation under bronchoscopy could avoid damage to the mucosa due to the blind use of negative pressure.[22]
Nevertheless, there was no advantage in the safety assessments. The 2 groups presented the similar complications and incidents such as reflexive respiratory/cardiac arrest, airway bleeding, asphyxia, arrhythmia, blood pressure fluctuation, and vomiting. No patient showed upper respiratory tract injury (pain, hemorrhage infection, etc), cerebrovascular accident, shock, pneumothorax/blood pneumothorax, and mediastinal/subcutaneous emphysema.
The population selected in our study was in a bad health condition; most of them had a long course of chronic injury of the airway, low immunity, and recurrent lung infection. In addition, we have not seen any other studies in the comparison between bronchoscopic sputum suction and general suction with the PIC window as the switching point. Nevertheless, it is still controversial whether the PIC window is appropriate as a weaning point of invasive ventilation.[23] Yan et al reported in a clinical analysis that SBT-2 was a better timing than PIC for patients with AECOPD to implement invasive to noninvasive ventilation switch.[17] The authors compared the incidence rates of successful treatment with NIPPV and tracheal reintubation, and the results showed 88.2% and 60.8%, and 11.8% and 39.2% in SBT-2 and PIC, respectively. Despite of the longer time of invasive ventilation in SBT-2 and similar morbidity rate in both groups, SBT-2 was considered as an optimal timing based on a higher success rate and a lower risk of tracheal reintubation. In the present study, given that these patients were in a severe condition and their pulmonary infection would be worsening, the PIC window was regarded as a better option according to the studies by Wang et al and Song et al.[18,19] Further data must be collected.
In conclusion, our study showed the bronchoscopic sputum suction presents more encouraging results that negative pressure suction, especially by the early appearance of the PIC window, high weaning success, and low mortality rate. This approach could be worthy of application in patients with AECOPD.
Acknowledgment
The authors acknowledge the General Hospital of Datong Minal Group Company for providing the data for this study.
Author contributions
Conceptualization: Zhihao Qiao, Jianghong Yu.
Data curation: Zhihao Qiao, Kai Yu, Mengya Zhang.
Formal analysis: Zhihao Qiao, Jianghong Yu, Kai Yu, Mengya Zhang.
Investigation: Zhihao Qiao, Kai Yu, Mengya Zhang.
Methodology: Zhihao Qiao, Jianghong Yu.
Project administration: Kai Yu.
Resources: Jianghong Yu, Kai Yu.
Software: Jianghong Yu, Mengya Zhang.
Validation: Zhihao Qiao.
Visualization: Jianghong Yu.
Writing – original draft: Zhihao Qiao.
Writing – review & editing: Zhihao Qiao, Jianghong Yu, Kai Yu, Mengya Zhang.
Footnotes
Abbreviations: AECOPD = acute exacerbation of chronic obstructive pulmonary disease, BAL = bronchial alveolar lavage, BMI = body mass index, IPPV = Invasive positive pressure ventilation, NIPPV = non-invasive positive pressure ventilation, PIC = pulmonary infection control, SBT-2 = spontaneous breathing trial, VAP = ventilator-associated pneumonia, WBC = white blood cell.
This work was funded by the ShanXi Science and Technology Department (Grant no: 20140313013-1).
The authors have no conflicts of interest to disclose.
References
- [1].Zheng J, Shi Y, Xiong L, et al. The Expression of IL-6, TNF-alpha, and MCP-1 in respiratory viral infection in acute exacerbations of chronic obstructive pulmonary disease. J Immunol Res 2017;2017:8539294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Peng L, Ren PW, Liu XT, et al. Use of noninvasive ventilation at the pulmonary infection control window for acute respiratory failure in AECOPD patients: a systematic review and meta-analysis based on GRADE approach. Medicine (Baltimore) 2016;95:e3880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Dixit D, Bridgeman MB, Andrews LB, et al. Acute exacerbations of chronic obstructive pulmonary disease: diagnosis, management, and prevention in critically ill patients. Pharmacotherapy 2015;35:631–48. [DOI] [PubMed] [Google Scholar]
- [4].Combes A, Luyt CE, Fagon JY, et al. Early predictors for infection recurrence and death in patients with ventilator-associated pneumonia. Crit Care Med 2007;35:146–54. [DOI] [PubMed] [Google Scholar]
- [5].Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med 2002;165:867–903. [DOI] [PubMed] [Google Scholar]
- [6].Zou SH, Zhou R, Chen P, et al. Application of sequential noninvasive following invasive mechanical ventilation in COPD patients with severe respiratory failure by investigating the appearance of pulmonary-infection-control-window [in Chinese]. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2006;31:120–4. [PubMed] [Google Scholar]
- [7].Luo Z, Zhan Q, Wang C. Noninvasive positive pressure ventilation is required following extubation at the pulmonary infection control window: a prospective observational study. Clin Respir J 2014;8:338–49. [DOI] [PubMed] [Google Scholar]
- [8].Collaborating Research Group for Sequential Invasive to Noninvasive Ventilation. Application of pulmonary infection control window as switching point for sequential invasive to noninvasive ventilation in treatment of severe respiratory failure of chronic obstructive pulmonary disease: a randomized controlled study. Zhonghua Jie He He Hu Xi Za Zhi 2006;29:14–8. [PubMed] [Google Scholar]
- [9].Wang ZF, Chen Y, Zheng MF, et al. Study on needling depth and direction from different acupoints to sphenopalatine ganglion [in Chinese]. Zhongguo Zhen Jiu 2009;29:289–92. [PubMed] [Google Scholar]
- [10].Chen W, Qing-yuan Z. Guideline for mechanical ventilation in patients with acute exacerbation of chronic obstructive pulmonary disease (2007) [in Chinese]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007;19:513–8. [PubMed] [Google Scholar]
- [11].Chinese Society of Critical Care Medicine, Chinese Medical Association. Practical guidelines for mechanical ventilation (2006) [in Chinese]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007;19:65–72.17326905 [Google Scholar]
- [12].Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347–65. [DOI] [PubMed] [Google Scholar]
- [13].Collaborating Research Group for Noninvasive Mechanical Ventilation of Chinese Respiratory Society. Pulmonary infection control window in treatment of severe respiratory failure of chronic obstructive pulmonary diseases: a prospective, randomized controlled, multi-centred study. Chin Med J (Engl) 2005;118:1589–94. [PubMed] [Google Scholar]
- [14].Pawar M, Mehta Y, Khurana P, et al. Ventilator-associated pneumonia: Incidence, risk factors, outcome, and microbiology. J Cardiothorac Vasc Anesth 2003;17:22–8. [DOI] [PubMed] [Google Scholar]
- [15].Burns KE, Meade MO, Premji A, et al. Noninvasive positive-pressure ventilation as a weaning strategy for intubated adults with respiratory failure. Cochrane Database Syst Rev 2013;CD004127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hill NS. Noninvasive ventilation for chronic obstructive pulmonary disease. Respir Care 2004;49:72–87. [PubMed] [Google Scholar]
- [17].Yan HY, Yang Y, Wu YL. Clinical analysis of optimal timing for application of noninvasive positive pressure ventilation in treatment of AECOPD patients. Eur Rev Med Pharmacol Sci 2014;18:2176–81. [PubMed] [Google Scholar]
- [18].Wang C, Shang M, Huang K. Sequential non-invasive following short-term invasive mechanical ventilation in COPD induced hypercapnic respiratory failure [in Chinese]. Zhonghua Jie He He Hu Xi Za Zhi 2000;23:212–6. [PubMed] [Google Scholar]
- [19].Song Y, Chen R, Zhan Q, et al. The optimum timing to wean invasive ventilation for patients with AECOPD or COPD with pulmonary infection. Int J Chron Obstruct Pulmon Dis 2016;11:535–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Radha S, Afroz T, Prasad S, et al. Diagnostic utility of bronchoalveolar lavage. J Cytol 2014;31:136–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lee HY, Choi SM. Foreign body aspiration of a press-through package that lodged between the vocal cords. Am J Respir Crit Care Med 2015;192:1517. [DOI] [PubMed] [Google Scholar]
- [22].Suys E, Nieboer K, Stiers W, et al. Intermittent subglottic secretion drainage may cause tracheal damage in patients with few oropharyngeal secretions. Intensive Crit Care Nurs 2013;29:317–20. [DOI] [PubMed] [Google Scholar]
- [23].Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033–56. [DOI] [PubMed] [Google Scholar]


