Abstract
Rationale:
Myasthenia gravis (MG) is the most common cause of acquired neuromuscular junction disorder. Thymectomy has been established as an effective therapy for MG, as it attenuates the natural course of the disease and may result in complete remission.
Patient concerns:
We report the case of a 22-year-old female with a 6-year history of MG presented with bilateral ptosis, diplopia, and intermittent dysphagia. She denied shortness of breath, dysarthria, and fatigue.
Diagnoses:
She had been diagnosed with MG 6 years previously at the Neurology Department of our hospital. A computed tomography (CT) scan revealed thymic hyperplasia
Interventions:
She was treated with modified unilateral VATET that minimized incision size.
Outcomes:
Unilateral VATET was performed using two 5-mm incisions to minimize pressure on intercostal soft tissues/nerves and reduce postoperative pain.
Lessons:
The lesson learnt from this case report is that this modified VATET method could be a useful approach to the management of non-thymomatous MG. The ability to achieve complete dissection with good cosmetic results may lead to wider acceptance of this technique by patients with MG and their neurologists for earlier thymectomy and improved outcomes. Additional studies are needed to determine the superiority of this approach to established methods.
Keywords: myasthenia gravis, thymic hyperplasia, unilateral video-assisted thoracoscopic extended thymectomy
1. Introduction
Myasthenia gravis (MG) is the most common cause of acquired neuromuscular junction disorder. Thymectomy has been established as an effective therapy for MG, as it attenuates the natural course of the disease and may result in complete remission.[1] Bilateral video-assisted thoracoscopic extended thymectomy (VATET) has been widely used to treat MG and has several advantages over trans-sternal thymectomy, including less tissue injury, shorter hospital stay, and superior cosmetic result.[2] Unilateral VATET is an alternative approach to bilateral VATET that has comparable long-term outcomes but reduces operating time.[3] Some surgeons prefer a right-sided approach to a left-sided approach for unilateral VATET to reduce the risk of innominate vein injury.[3] However, right-sided and left-sided approaches have similar outcomes with regard to complications, hospital stay, and disease remission.[4] Here, we report a modified technique for unilateral right-sided VATET that uses two 5-mm operating ports to minimize the pressure on intercostal nerves and soft tissues during surgery. During the procedure, the resected thymus was placed into a specimen bag (introduced via the camera port) and cut into smaller pieces with a pair of scissors, allowing it to be extracted without the need for a large incision.
2. Case report
The patient described here provided informed consent for publication of this case report, and this study was approved by the ethics committee of The First Affiliated Hospital of Hainan Medical University. A 22-year-old Chinese female with a 6-year history of MG presented with bilateral ptosis, diplopia, and intermittent dysphagia at the Affiliated Hospital of Hainan Medical University. She had been diagnosed with MG 6 years previously at the Neurology Department of our hospital. She denied shortness of breath, dysarthria, and fatigue. A computed tomography (CT) scan revealed thymic hyperplasia (Fig. 1 A). She was prescribed pyridostigmine bromide 60 mg qid, and acceptable control of the disease was achieved with medication. Nevertheless, she was unable to tolerate long-term use of pyridostigmine bromide and decided to undergo surgery. There were no abnormalities in pulmonary function tests and other laboratory evaluations. She underwent surgery in August 2015.
Figure 1.
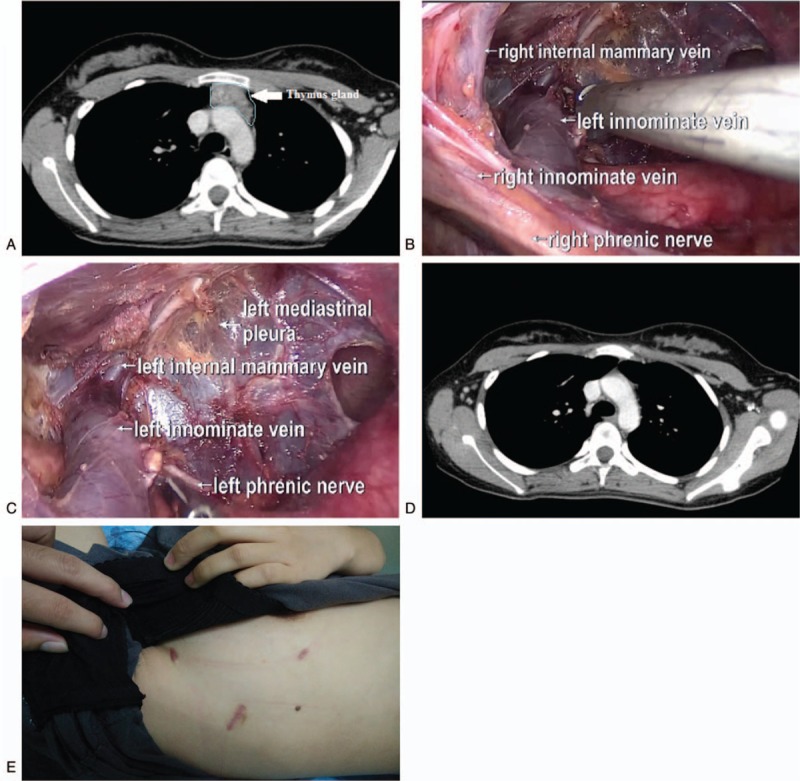
(A) Preoperative CT scan. (B) Thymic bed after thymectomy. (C) Another view of the thymic bed after thymectomy. (D) CT scan obtained 3 months postoperatively. (E) Incision site at 3 months postoperatively.
As muscle relaxants are contraindicated in patients with MG, the patient took pyridostigmine bromide 60 mg on the morning of the operation. A single-lumen endotracheal tube was used instead of a double-lumen tube to minimize tracheobronchial injury. The patient was placed in the supine position with the right side slightly bumped at 30°, the right upper limb elevated, and the right forearm fixed to the side of the head.
A notable feature of our modified VATET technique was that our surgical incisions were smaller (5-mm ports) than those used in traditional video-assisted thoracoscopic surgery (VATS). Two 5-mm operating ports were placed at the third and sixth interspace, respectively, along the right anterior axillary line. The camera port (1.2 cm) was placed at the fifth interspace along the right midaxillary line.
After entry into the right chest, an artificial pneumothorax was created using CO2 insufflation to expand the surgical field of vision and better expose the left phrenic nerve. CO2 insufflation was implemented using a pressure limit of 6 to 8 mm Hg to expand the mediastinal space but avoid tamponade. An electric hook was used to open tissue along the sternum to the mediastinal pleura from the lower right corner of the pericardial fat to the right internal mammary vein. The dissection plane along the right phrenic nerve was used to open the mediastinal pleura to the end of the right internal mammary vein.
Blunt and sharp dissection with a Harmonic scalpel was used to separate the thymus gland. After dissection of the right inferior horn from the pericardium, resection was continued superiorly along the right phrenic nerve and superior vena cava. The right upper pole was circumferentially freed from above the innominate vein until the thyrothymic ligaments were identified. The thymus was separated from the left innominate and left internal mammary veins. The left phrenic nerve, which can be difficult to find during traditional right-sided VATS, was easily identified under the left internal mammary vein. Ligation of blood vessels was not necessary, as the resection was performed with a Harmonic scalpel.
After the intact thymus gland and surrounding fatty tissue had been dissected free (Fig. 1 B, C), they were placed into a specimen bag that had been inserted via the camera port. A pair of scissors was used to cut the thymus and surrounding fatty tissue into multiple small pieces within the specimen bag. The specimen bag containing the shredded tissue was then retrieved through the camera port using curved forceps.
Meticulous hemostasis was achieved with the assistance of hemostatic fabrics. Chest drainage tubes were not needed, helping to minimize postoperative pain and facilitating rapid recovery after surgery. Soft tissue closure was accomplished with a multilayer absorbable suture, and this was followed by subcutaneous closure of the skin.
The entire operation was performed without complications. There was very little bleeding. Immediate extubation was performed because respiratory effort and blood gas values were acceptable. The patient was encouraged to ambulate as soon as possible after surgery and was taught to cough effectively to reduce the risk of pulmonary infection. The patient underwent chest X-ray 1 day after surgery to confirm the absence of pneumothorax or bleeding.
Pathological examination showed that the lesion was thymus hyperplasia involving the pericardial fat. The patient was discharged 3 days after surgery. She was prescribed pyridostigmine bromide 30 mg qid within 3 months after surgery. At 3 months after surgery, the patient's symptoms were well controlled and her muscle tension was normal. A CT scan showed no residual thymus tissue in the anterior mediastinum (Fig. 1 D). Six months after surgery, pyridostigmine bromide treatment was discontinued. In May 2017, the patient was still without any manifestations of MG.
3. Discussion
Minimally invasive thymectomy has been used for non-thymomatous MG. We advocate surgery for some of our young patients even though their symptoms are purely ocular. Although some patients with purely ocular symptoms improve after thymectomy, the rationale for surgery is not based on symptomatic improvement but rather on the expectation of halting disease progression.[5,6] Compared with the conventional trans-sternal technique, VATET has equivalent efficacy and the advantages of shorter operation time, better preservation of pulmonary function, less bleeding, less postoperative pain, shorter length of stay, lower costs, fewer complications, and better cosmetic results.[7–9]
Thoracoscopic thymectomy can be performed from either the right or left side, and which approach is best remains controversial.[10,11] Indeed, Landreneau et al[10] advocate the use of the left-sided approach to thymus resection, as it achieves good surgical outcomes. On the contrary, Zielinski et al[11] recommend the right-sided approach because of an increased risk of innominate vein injury when the left-sided approach is used. The right-sided approach was selected for the case reported here because of the risk of innominate vein injury.
We have developed a minimally invasive technique that permits the removal of all thymic tissue and adjacent mediastinal fatty tissue using 5-mm ports. Our center initially used 2 ports measuring 3 cm for VATET, but progressive refinement of the technique over time now enables us to use 5-mm operating ports, as in the present case. Although a thymus/thymoma less than 4 cm in diameter can be removed through the observation port intact, this is not possible for larger specimens. To overcome the requirement of a larger incision for a bigger specimen and thus improve cosmetic results, we utilized the innovative approach of using a pair of scissors to shred the tissue within a specimen bag before its removal from the chest cavity. The cosmetic results were important for this 22-year-old female, and the use of 5-mm ports achieved minimal scarring (Fig. 1 E). In addition, the use of smaller ports during surgery may exert less pressure on the intercostal nerves and thus potentially lessen postoperative pain, including chronic pain.[12,13] A chest tube was not implanted in the present case because the surgical process was smooth and complete hemostasis was achieved with only 10 mL of blood loss. This may also have helped to reduce postoperative pain and improve cosmetic results.
For the past 2 years, we have been using single-lumen tubes instead of double-lumen tubes for ventilation, because single-lumen tubes reduce endotracheal friction and result in less tracheal injury.[14] The creation of an artificial pneumothorax with CO2 insufflation compressed the ipsilateral lung and mediastinum, thereby widening the surgical field of vision and making it easier to free the left innominate and thymic veins and identify the left phrenic nerve. A final advantage of the operation described here was that it was performed using minimal equipment (a Harmonic scalpel, hook cautery, and curved hemostatic forceps).
In conclusion, this modified VATET method could be a useful approach to the management of non-thymomatous MG. The ability to achieve complete dissection with good cosmetic results may lead to wider acceptance of this technique by patients with MG and their neurologists for earlier thymectomy and improved outcomes. Additional studies are needed to determine the superiority of this approach to established methods.
Acknowledgment
We thank Edwin Lin, MD, PhD, from the University of Utah and Dr. Thomas K. Varghese and Dr. Zach DeBoard, from the University of Utah Huntsman Cancer Hospital, for reviewing this article.
Author contributions
FPM and CGP participated in the literature search, study design and surgery, and wrote the manuscript. JCN, LPF, LJT, and ZWP participated in the design and coordination of the study and provided critical revision. All authors read and approved the final manuscript.
Conceptualization: Ping-Ming Fan, Guo-Ping Chen, Wu-Ping Zheng.
Data curation: Ping-Ming Fan, Guo-Ping Chen, Chao-Na Jiang, Peng-Fei Lv, Jing-Tai Li, Zhi-Lin Chen, Li-Ping Zheng, Jie-Zhi Su.
Formal analysis: Ping-Ming Fan, Guo-Ping Chen, Chao-Na Jiang, Peng-Fei Lv, Jing-Tai Li, Zhi-Lin Chen, Li-Ping Zheng, Jie-Zhi Su, Wu-Ping Zheng.
Project administration: Wu-Ping Zheng.
Writing – original draft: Ping-Ming Fan, Guo-Ping Chen.
Writing – review & editing: Chao-Na Jiang, Peng-Fei Lv, Jing-Tai Li, Zhi-Lin Chen, Li-Ping Zheng, Jie-Zhi Su, Wu-Ping Zheng.
Footnotes
Abbreviations: CT = computed tomography, MG = myasthenia gravis, VATET = video-assisted thoracoscopic extended thymectomy, VATS = video-assisted thoracoscopic surgery.
PMF and GPC contributed equally to this study.
Informed consent was obtained from the patient to publish this article.
The authors have no conflicts of interest.
References
- [1].Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized trial of thymectomy in Myasthenia gravis. N Engl J Med 2016;375:511–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lin MW, Chang YL, Huang PM, et al. Thymectomy for non-thymomatous myasthenia gravis: a comparison of surgical methods and analysis of prognostic factors. Eur J Cardiothorac Surg 2010;37:7–12. [DOI] [PubMed] [Google Scholar]
- [3].Liu Z, Yang J, Lin L, et al. Unilateral video-assisted thoracoscopic extended thymectomy offers long-term outcomes equivalent to that of the bilateral approach in the treatment of non-thymomatous myasthenia gravis. Interact Cardiovasc Thorac Surg 2015;21:610–5. [DOI] [PubMed] [Google Scholar]
- [4].Elsayed HH, Gamal M, Raslan S, et al. Video-assisted thoracoscopic thymectomy for non-thymomatous myasthenia gravis: a right-sided or left-sided approach? Interact Cardiovasc Thorac Surg 2017;25:651–3. [DOI] [PubMed] [Google Scholar]
- [5].Gronseth GS, Barohn RJ. Practice parameter: thymectomy for autoimmune myasthenia gravis (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:7–15. [DOI] [PubMed] [Google Scholar]
- [6].Zahid I, Sharif S, Routledge T, et al. Video-assisted thoracoscopic surgery or transsternal thymectomy in the treatment of myasthenia gravis? Interact Cardiovasc Thorac Surg 2011;12:40–6. [DOI] [PubMed] [Google Scholar]
- [7].Yuan ZY, Cheng GY, Sun KL, et al. Comparative study of video-assisted thoracic surgery versus open thymectomy for thymoma in one single center. J Thorac Dis 2014;6:726–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jurado J, Javidfar J, Newmark A, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg 2012;94:974–81. discussion 81-82. [DOI] [PubMed] [Google Scholar]
- [9].Petersen RH. Video-assisted thoracoscopic thymectomy using 5-mm ports and carbon dioxide insufflation. Ann Cardiothorac Surg 2016;5:51–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992;54:142–4. [DOI] [PubMed] [Google Scholar]
- [11].Zielinski M, Czajkowski W, Gwozdz P, et al. Resection of thymomas with use of the new minimally-invasive technique of extended thymectomy performed through the subxiphoid-right video-thoracoscopic approach with double elevation of the sternum. Eur J Cardiothorac Surg 2013;44:e113–9. discussion e9. [DOI] [PubMed] [Google Scholar]
- [12].Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ng CS, Wong RH, Lau RW, et al. Minimizing chest wall trauma in single-port video-assisted thoracic surgery. J Thorac Cardiovasc Surg 2014;147:1095–6. [DOI] [PubMed] [Google Scholar]
- [14].Kim HY, Baek SH, Je HG, et al. Comparison of the single-lumen endotracheal tube and double-lumen endobronchial tube used in minimally invasive cardiac surgery for the fast track protocol. J Thorac Dis 2016;8:778–83. [DOI] [PMC free article] [PubMed] [Google Scholar]


