Abstract
Introduction
The relationship between high volume and improved outcomes has been described for a host of elective high-impact, low-frequency procedures, but there are little data to support such a relationship in high-impact low-frequency procedures in trauma. Using emergency department thoracotomy (EDT) as a model, we hypothesized that patients presenting to centers with higher institutional volumes of EDT would have improved survival referent to those presenting to lower volume institutions.
Materials and Methods
We queried the Pennsylvania Trauma Outcomes Study (PTOS) registry from 2007-2015 for all EDTs performed at level I and II centers identified by ICD-9 procedure codes and a location stamp indicating the emergency department. We examined patient-level risk factors for survival in univariate regression and multivariable regression models. Centers were divided into tertiles of mean annual EDT volume and the association between mean annual EDT volume and patient survival was examined using logistic regression after controlling for patient factors.
Results
1,399 emergency department thoracotomies were performed at 28 centers. Overall survival was 6.8%. After controlling for patient age, mechanism of injury, signs of life, and injury severity, patients presenting to centers in the highest tertile of volume had significantly higher odds of survival compared to patients presenting to centers in the lowest tertile of volume (OR 4.56, 95% CI 1.43-14.50).
Conclusions
Patients presenting to centers with higher mean annual volume of EDTs have improved survival compared to those presenting to institutions with lower mean annual EDT volume. Efforts to understand the etiology of this finding may lead to interventions to improve outcomes at lower volume centers.
Keywords: Emergency department thoracotomy, epidemiology, volume, blunt trauma
Introduction
The relationship between institutional procedural volume and patient outcomes has been investigated across a wide variety of surgical procedures over the past three decades. These studies typically focus on high-impact low-frequency (HILF) procedures such as aortic reconstruction, pneumonectomy and oncologic resections in elective settings. In settings where HILF procedures may be emergent, simulation-based training has been used as a means to support provider and team readiness (1). As a general principle, higher institutional volume is associated with improved patient outcomes for HILF procedures such as major abdominal, thoracic (2-4), and vascular surgical interventions (5, 6). While the relationship between volume and patient outcomes for elective HILF procedures is well-established, studies investigating the relationship between emergent HILF procedural volume and patient outcomes are lacking.
Emergent HILF procedures for trauma are performed by physicians at designated centers where procedural volume may be low. As an extreme example, emergency department thoracotomy (EDT) represents one of the most invasive and technically demanding procedures performed on injured patients in extremis. Although promising less-invasive techniques such as Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) have been used in a subset of injured patients (7, 8), EDT remains a critically important procedure for injured victims of penetrating trauma presenting with hemodynamic collapse. Despite its widespread utilization however, survival after EDT remains low, ranging from 5-25% depending on presenting patient characteristics such as signs of life, mechanism of injury, and prehospital transport time (9-12).
Because of the time-critical nature of EDT, attempting to limit this procedure to high-volume centers is challenging. However, if a volume-outcomes relationship does exist for emergent HILF procedures in trauma, then investigations into the mediators of this association could lead to the development of interventions targeted at improving outcomes at lower-volume centers. Using EDT as our model, we sought to examine the relationship between center volume of EDT and patient outcomes, with the hypothesis that patients undergoing EDT at higher-volume centers have improved outcomes.
Materials and Methods
After approval from the University of Pennsylvania Institutional Review Board, we performed a retrospective analysis of the Pennsylvania Trauma Outcomes Study (PTOS) database from 2007 to 2015. The Pennsylvania Trauma Systems Foundation is the governing body of the state that accredits all trauma centers in the Commonwealth of Pennsylvania. To maintain accreditation, Pennsylvania trauma centers must abstract, collect, and submit data on all trauma patients to the PTOS registry. The database contains over 500,000 patient records from more than thirty years of admissions at state-accredited trauma centers and contains over 1200 data points for each patient. Importantly for the purpose of this study, the PTOS registry contains not only ICD-9 procedure codes for the first 82 procedures performed but also time, date, and location associated with each of these procedures.
The population of interest in this study was all patients undergoing EDT during the study period at level I and level II trauma centers in the state of Pennsylvania. Patients were included in the study if they were coded as having had a thoracotomy (defined by ICD-9 procedure code 34.02, exploratory thoracotomy) or procedure requiring thoracotomy (37.12, pericardiotomy; 37.4, heart & pericardial repair; 37.49, heart & pericardial repair nec; 37.91, open chest cardiac massage; 38.84 occlusion of the aorta; or 38.85, occlusion of other thoracic vessel) which occurred in the emergency department (defined by PTOS procedure location code 1, indicating emergency department). Patients under the age of 18 were excluded from the study. Data regarding demographic information (age, race, sex), mechanism of injury (blunt vs. penetrating), injury severity (as measured by injury severity score (ISS)), and physiology (heart rate, respiratory rate, and Glasgow Coma Scale (GCS)) on admission were collected. Additionally, based on patient physiology on arrival, patients were grouped as presenting with or without signs of life (SOL) to the trauma center, which for the purpose of this study was defined as a GCS >3, heart rate >0, or a respiratory rate >0. All candidate variables analyses were assessed for missingness and found to be missing in <10% of cases (age, <1%; mechanism, 0%; race, 8.3%; ISS, <1%, sex, 0%; heart rate 4.6%; GCS 5.7%) with the exception of respiratory rate, which was missing in 16.2% of cases. However, because this respiratory rate was used as part of a combined physiologic parameter “signs of life” (scored as present if any of HR, SBP, or RR were non-missing and greater than 0), the overall missingness of the signs of life variable was 8.7%. Examination of rates of casewise deletion secondary to complete case analysis in the final model confirmed < 10% missing data, and so we did not impute missing data secondary the low risk introduced bias with this approach (13, 14).
In the later years of the study, it seemed possible that resuscitative endovascular balloon occlusion (REBOA) might compete with EDT, reducing our sample size and overall biasing our study towards the null. As no ICD-9 procedure code specific to REBOA exists, as a proxy we assessed the stability of proportions of patients undergoing EDT by mechanism over the study period using Cochran-Armitage test of trend.
To investigate the relationship between patient-level factors and survival, we first built univariate regression models between candidate variables and survival. Those patient variables associated with survival with p<0.2 were then used in multivariable regression models on survival using forced entry. Because a robust body of evidence suggests that race may be associated with mortality after injury (15), race was included in our analyses as a potential confounder. Race was defined according to the PTOS data dictionary definitions (http://www.ptsf.org/upload/DRAFT_2017_PTOS_Manual_5-1-2017.pdf). To adhere to the principle of parsimony and avoid overfitting, we removed variables from the final multivariable model which did not contribute to model discrimination. Model discrimination was examined by examining the Area Under the Curve (AUC) of Receiver Operator Characteristic Curves (ROC). We tested calibration using the Hosmer-Lemeshow test and visual inspection of plots of observed to predicted survival derived from our model.
To assess the association between the primary exposure of mean annual EDT volume and patient survival, several models using different forms of the exposure variable were assessed (linear, fractional polynomial, logistic regression using quintiles of volume, and logistic regression using tertiles of volume). Based on prior literature assessing volume-outcomes relationships (16-18) and for the sake of ease of interpretation and, we ultimately selected tertiles of mean annual EDT volume to represent volume as an exposure variable.
We then constructed a logistic regression model on survival using tertiles of mean annual EDT volume while controlling for patient-level factors associated with survival from our previously developed multivariable model. For all models, we used robust variance estimation to account for clustering by center. As the primary purpose of this work was to investigate the relationship between volume of EDT and outcomes, other center-level variables such as bed number and teaching status were not assessed for inclusion in our multivariable survival models. After generation of the final model, we calculated the marginal predicted probability of survival for each tertile of mean annual EDT volume after adjusting for patient factors significantly associated with survival. Patient survival was defined as survival to discharge from the hospital.
To understand the characteristics of the trauma centers in each tertile of mean annual EDT volume, we merged data from the American Hospital Association’s national Annual Survey of Hospitals with the PTOS trauma registry. In addition to trauma center level, mean annual trauma volume, and proportions of trauma by mechanism, we examined the differences in annual hospital admissions, the number of medical/surgical ICU beds, total hospital beds, the teaching status by tertile of mean annual EDT volume. We explored teaching status using both the presence of a residency training approval by the Accreditation Council for Graduate Medical Education and by membership in the Council of Teaching Hospitals of the Association of American Medical Colleges.
Functional disability at discharge was measured using the modified Functional Independence Measure (FIM) score. The FIM score has been well studied and validated in the literature (19, 20). The modified FIM assigns a score ranging from 1 (total assistance) to 4 (independent function) for each of 3 categories (expression, movement and feeding) and has been used in the trauma literature to assess neurologic outcomes (21). We defined neurologically intact survival a modified Functional Independence Measure (FIM) score of 4 in at least one of the three categories or as a patient discharged to home. We used Kruskal-Wallis test to compare for non-normally distributed continuous variables and two-sample t-test to compare normally distributed continuous variables. Chi-squared test was used to compare categorical variables. Stata v14.0 (College Station, TX) was used for all statistical analysis.
Results
During the study period from 2007-2015, 1,399 emergency department thoracotomies were performed at 28 level I and level II trauma centers across the state of Pennsylvania (see Figure 1 for flow diagram of patients included in the study). Two centers that did not perform any emergency department thoracotomies during the study period were excluded. In total, 95/1399 (6.8%) of patients survived. The annual survival rate ranged between 5.3 and 8.3%, and there was no statistically significant difference in the trend of survival rates over the study period (Cochrane-Armitage test of trend p = 0.51). Although there is no specific ICD-9 procedural code which uniquely indicates REBOA, we considered that in the later years of the study REBOA may have competed with EDT and thus diminished the proportion of patients undergoing EDT. Stratified by injury mechanism, the proportion of patients who may have been candidates for REBOA (systolic blood pressure <90mmHg, no chest injury by AIS) undergoing EDT did not change over the study period (Cochrane-Armitage test of trend p = 0.44 for blunt mechanism, 0.71 for penetrating mechanism), providing indirect evidence that REBOA did not appear to be occurring at rates in our study population that might introduce bias. Characteristics of patients included in the study can be seen in Table 1. In univariate logistic regression on survival, patients who survived EDT were younger and more likely to be white. Compared to GSW, both blunt injury (OR 2.27, 95% CI 1.13-4.58) and stab wounds (OR 7.39, 95% CI 4.60-11.86) were associated with increased odds of survival. The patient factor that was most strongly associated with survival was the presence of signs of life (SOL) on arrival (OR 13.32, 95% CI 9.27-19.15). In patients arriving without SOL, 8/726 (1.1%) survived; in patients presenting with SOL, 87/673 (12.9%) survived. In multivariable logistic regression modelling on survival, we found that the association between signs of life and survival was strengthened (OR 13.99, 95% CI 8.66-22.62) by the inclusion of age, mechanism and ISS in the model, all of which maintained statistical significance. After adjusting for these patient factors, race was no longer associated with survival. Omission of this variable had no impact on discrimination or calibration of the model, and so this variable was removed from the final multivariable logistic regression model of the association between patient factors and survival in accordance with the principle of parsimony.
Figure 1.
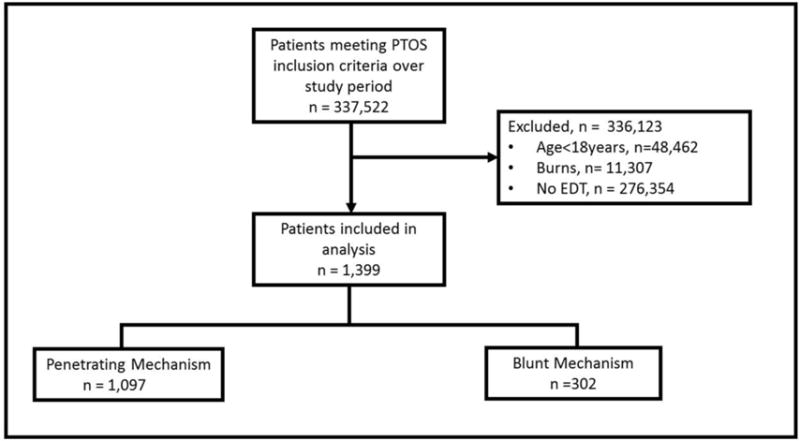
Flow diagram of patients included in the study. Abbreviations: PTOS = Pennsylvania Trauma Outcomes Study; EDT = Emergency Department Thoracotomy
Table 1.
Characteristics of patients undergoing EDT and associations with survival.
| Variable | Died (n=1,304) | Lived (n=95) | OR | 95% CI | p |
|---|---|---|---|---|---|
| Age, per year | 40 (IQR 22-46) | 33 (IQR 25-44) | 0.99 | (0.99-1.00) | 0.13 |
| Race | |||||
| Black | 810 (62.1%) | 47 (49.5%) | Ref | ||
| White | 363 (27.8%) | 37 (40.0%) | 1.76 | (1.12-2.75) | 0.01 |
| Other | 25 (1.9%) | 37 (1.1%) | 0.69 | (0.09-5.20) | 0.72 |
| Missing | 106 (8.1%) | 10 (10.5%) | - | - | |
| Sex | |||||
| Male | 1154 (88.5%) | 81 (85.3%) | Ref | ||
| Female | 150 (11.5%) | 14 (14.7%) | 1.33 | (0.84-2.10) | 0.22 |
| Mechanism | |||||
| Gunshot wound | 934 (70.9%) | 38 (40%) | Ref | ||
| Blunt injury | 278 (21.3%) | 26 (27.4%) | 2.27 | (1.13-4.58) | 0.02 |
| Stab wound | 102 (7.8%) | 31 (32.6%) | 7.39 | (4.60-11.86) | <0.001 |
| ISS, per point | 26 (IQR 17-59) | 25 (IQR 14-35) | 0.99 | (0.98-0.99) | <0.001 |
| Signs of life | |||||
| Absent | 718 (55.1%) | 8 (8.4%) | Ref | ||
| Present | 586 (44.9%) | 87 (91.6%) | 13.32 | (9.27-19.15) | <0.001 |
Data for nonparametric continuous variables expressed as median (Interquartile Range); categorical values expressed as n (%). P values are for univariate logistic regression analyses. Abbreviations: ISS = Injury Severity Score; OR = Odds Ratio; CI = Confidence interval
Emergency department thoracotomies were performed at 28/30 (93%) of Level I and Level II trauma centers over the study period. The mean annual volume of EDTs in the PA trauma system was 157 (SD 21.3), while a mean annual volume per center was 3.1(SD 11). Only 3 centers had a mean annual EDT volume of > 10. The maximum number of EDTs performed at a single center in a single year was 57. Most of the EDTs in the state of Pennsylvania were performed by two high-volume centers that combined performed >70 EDTs annually. The mean annual number of EDTs performed by center and mean annual number of EDT survivors can be seen in Figure 2. In general, centers with lower annual EDT volumes had fewer survivors and centers with higher annual EDT volumes had more survivors. However, there did not appear to be a linear relationship between rates of survival and overall annual center volume.
Figure 2.
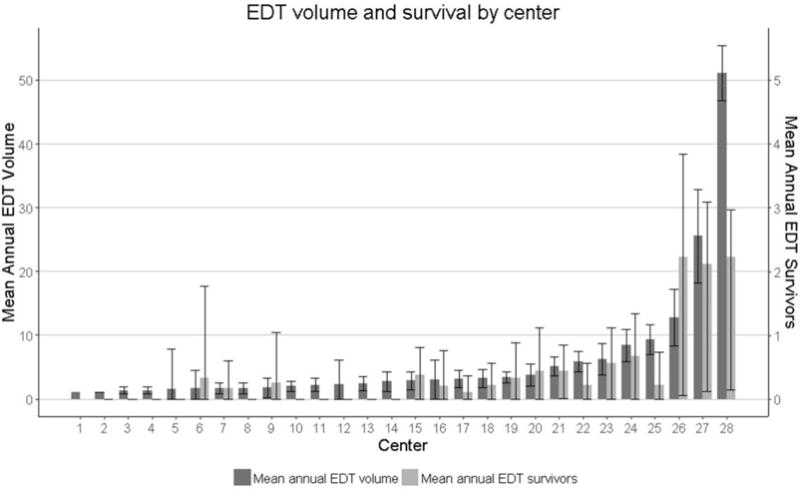
Mean annual volume of EDT and mean annual number of EDT survivors at the 28 Level I and Level II trauma centers in the study. Abbreviations: EDT = Emergency Department Thoracotomy
To begin to consider the effect of EDT volume on patient survival, we calculated the mean annual volume of EDT for each center over the study period and then divided centers into three tertiles of mean annual EDT volume (low, 1-2; middle, 2.2-3.4; and high, 3.7-51.1). In terms of observed survival, 3/71 (4.2%) of patients presenting to lowest tertile hospitals, 10/174 (5.6%) of patients presenting to middle tertile centers, and 95/1,072 (6.8%) of patients presenting to highest tertile centers survived to discharge. After adjusting for patient factors associated with survival, patients at centers in the highest tertile of volume had significantly higher odds of survival (OR 4.56, 95% CI 1.43-14.50) compared to those at centers in the lowest tertile of mean annual EDT volume. Patient factors that remained significantly associated with survival can be seen in Table 2 and included age, mechanism of injury, injury severity score, and signs of life. The area under the curve for the receiver operator characteristic curve for our final model was 0.83 (95% CI 0.79-0.87), indicating good discrimination. The Hosmer-Lemeshow chi-squared statistic for the final model was 7.30 (p = 0.70), indicating acceptable calibration. To assess for the potential impact of REBOA on our findings, we performed a sensitivity analysis by removing data from 2014 and 2015, when it was at least plausible that REBOA might compete. Repetition of these analyses after removal of all cases from 2014-2015 did not substantially alter the direction or magnitude of the point estimates of the associations between any variable in the model and survival. The probability of survival by tertile of mean annual EDT volume after adjusting for patient factors can be seen in Figure 3. At high-volume centers, the adjusted probability of survival was 7.6% whereas at low-volume centers the probability was 2.1%.
Table 2.
Multivariate logistic regression analyses of the association between mean annual EDT volume survival, adjusted for patient factors.
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Mean Annual EDT volume | |||
| Low (1-2) | Ref | ||
| Middle (2.2-3.4) | 3.22 | (0.92-11.22) | 0.07 |
| High (3.7-51.1) | 4.56 | (1.43-14.50) | 0.01 |
| Age, per year | 0.99 | (0.98-0.99) | <0.001 |
| Mechanism | |||
| Gunshot wound | Ref | ||
| Blunt injury | 2.26 | (1.24-4.13) | 0.01 |
| Stab wound | 10.35 | (6.81-15.73) | <0.001 |
| Iss, per point | 0.99 | (0.98-1.00) | 0.01 |
| Signs of life | 13.99 | (8.66-22.62) | <0.001 |
Abbreviations: EDT = Emergency Department Thoracotomy; ISS = Injury Severity Score; OR = Odds Ratio; CI = Confidence interval
Figure 3.
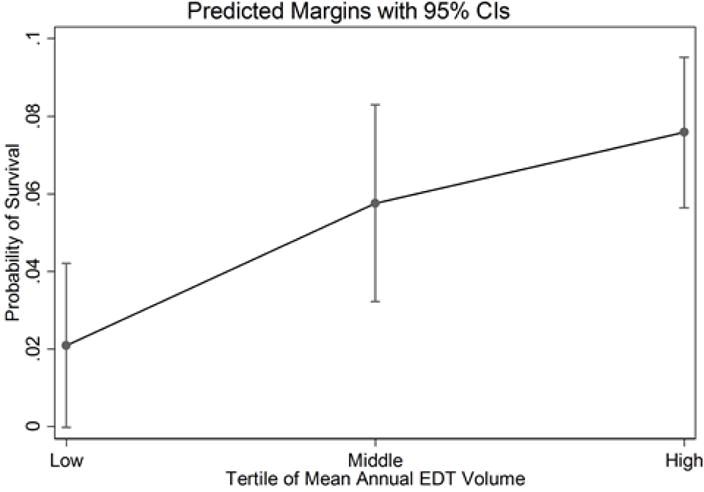
Predicted probability patient survival by tertile of mean annual emergency department thoracotomy volume, adjusted for patient age, mechanism of injury, injury severity score, and the presence of signs of life
Characteristics of centers in each tertile of volume can be seen in Table 3. Trauma centers in the highest tertile of volume were more likely to be Level I trauma centers than those in the low and middle tertiles (p<0.001). There was a trend towards increased overall trauma volume over low, middle, and high tertile centers such that centers with higher mean annual volumes of EDT tended to have higher overall volumes of trauma, but this did not reach statistical significance (p= 0.09). Centers in the highest tertile of mean annual EDT volume had higher volumes of penetrating trauma than those in lower tertiles. There was no difference in annual hospital admissions, the number of Medical/Surgical intensive care unit beds, or total hospital beds between tertiles of care. In addition, we found no difference in teaching status as defined by presence of residency programs or membership in the Council of Teaching Hospitals of the Association of American Medical Colleges between tertiles of volume.
Table 3.
Characteristics of the 28 trauma centers in the study by tertile of mean annual EDT volume.
| Low (1-2) n = 10 |
Tertile of mean annual EDT volume Middle (2.2-3.4) n = 9 |
High (3.7-51.1) n = 9 |
p | |
|---|---|---|---|---|
| Trauma Center Level | 0.03 | |||
| I | 3 (30%) | 4 (44%) | 8 (89%) | |
| II | 7 (70%) | 5 (56%) | 1 (11%) | |
| Annual Trauma Volume | 756 (IQR 559-960) | 1096 (IQR 907-1159) | 1278 (IQR 1075-1328) | 0.09 |
| Mechanism of Injury | ||||
| Gunshot wound | 4.2% (IQR 3.2%-5.5%) | 5.3% (IQR 5.1%-6.0%) | 9.6% (IQR 7.2%-16.7%) | 0.01 |
| Blunt mechanism | 94.0% (IQR 93.1%-94.6%) | 92.3% (IQR 91.0%-92.8%) | 87.6% (IQR 79.4%-89.9%) | 0.01 |
| Stab wound | 1.9% (IQR 1.5%-2.4%) | 2.3% (IQR 2.0%-2.8%) | 2.9% (IQR 2.7%-4.8%) | 0.02 |
| Annual Hospital Admissions | 20,100 (IQR 12,755-28,156) | 27,230 (IQR 21,707-29,129) | 22,678 (IQR 20,571-26,732) | 0.34 |
| Medical/Surgical ICU Beds | 33 (IQR 18-54) | 18 (IQR 16-41) | 30 (IQR 27-65) | 0.50 |
| Total hospital beds | 202 (IQR 177-372) | 336 (IQR 225-377) | 218 (IQR 188-295) | 0.35 |
| Residency Program | 10 (100%) | 8 (89%) | 8 (89%) | 0.52 |
| Teaching Hospital | 3 (30%) | 3 (30%) | 6 (67%) | 0.30 |
Data for nonparametric continuous variables expressed as median (Interquartile Range); categorical values expressed as n (%). P values are Fisher’s exact test for categorical variables and Kruskal-Wallis test for nonparametric continuous variables. EDT = Emergency Department Thoracotomy
Of patients who survived to discharge and had available data, 67 (71%) were neurologically intact as defined by a FIM score of 4 in at least one category or discharge to home.
Discussion
In this retrospective cohort study, we report evidence of a positive relationship between institutional volume of an emergent high-impact low-frequency procedure and patient survival. Risk-adjusted survival increased from about 2% at low-volume centers to over 7% at high-volume centers. Although much has been written about the relationship between overall trauma center volume and outcomes (22-26), ours is the first study of which we are aware to report a relationship between volume of a specific procedure and patient survival in a trauma cohort.
While we have demonstrated that risk-adjusted survival is highest at centers that perform higher volumes of EDT, defining a specific numeric threshold above which improved outcomes are expected is difficult. An understanding the relationship between EDT procedural volume and outcomes is made complex by consideration of the selection criteria for the procedure. Conceptually, restricting EDT to patients who are likeliest to survive would be expected to result in higher survival rates even as it decreases overall volume of EDT and decreases the number of total survivors (since some patients undergoing EDT who do not meet commonly accepted selection criteria for EDT will be unexpected survivors (27)). Conversely, relaxing EDT selection criteria to include patients unlikely to survive in any event would be expected to decrease the survival rate while at the same time increasing the overall volume of EDT and the total number of survivors. For this reason, simply relaxing selection to increase EDT volume would not be expected to result in increased survival rates. For instance, the center with the highest institutional volume in this study did nearly twice the number of EDTs as the center with the second-highest institutional volume but had essentially the same number of survivors, resulting in a lower overall survival rate.
The patient and center level factors which underlie this phenomenon are yet to be discovered, but if subject to modification could serve as the basis for interventions designed to help low-volume centers achieve outcomes comparable to high-volume centers. The association between survival and volume is likely multifactorial and may be influenced by factors at both the level of the provider and the system. In our study, higher volume centers were more likely to be level I trauma centers. Designated trauma centers with well-developed protocols, surgical expertise, nursing expertise, quick access to necessary equipment and adjuncts such as blood products and around the clock intensive care have been shown in the literature to be associated with improved outcomes (28, 29). Additionally, the training and experience of the individual surgeon performing the procedure likely contributes to outcomes. To that end, even a modest amount of simulation training has been demonstrated to significantly improve times to achieve defined emergent thoracotomy procedure milestones (1) in simulation studies with cardiac surgery trainees. The role of simulation in training for complex procedures is well studied in the medical literature (30-33) and has been shown to improve provider speed during other resuscitative procedures (34). As procedural simulation training devices become more widely available, we hope the results of investigations like ours may lead centers to consider simulation training as a potential means to improve outcomes.
Even when undertaken by an experienced trauma team and a seasoned operator, survival after emergency department thoracotomy is low. From 2007-2015 the survival after EDT in the state of Pennsylvania was 6.8%, consistent with findings from published case series which have a combined survival rate of 7.8% (35, 36). One unexpected finding in our study that stands in contrast to most of the available literature (9, 11, 35-37) was that referent to gunshot wounds, blunt trauma was associated with improved survival. There are several possible explanations for this finding. First, most of the published literature on EDT consists of cases series, which tend to be published by high-volume, single-institution centers that practice in large urban settings with relatively high volumes of penetrating trauma. In our study, we were able to include data from all level I and level II centers in a statewide trauma system, including less academic centers with high volumes of blunt trauma that might be less likely to publish their experience. Publication bias by studies from centers that do not represent the trauma system as a whole may therefore be one possible explanation for our discordant finding. Second, there may be unmeasured confounding with respect to time in circulatory arrest. Because EDT for blunt mechanism of injury may be restricted to those patients with witnessed arrest, it is possible that patients with GSWs who arrive in arrest may have been without perfusion for longer than is appreciated. If some subset of these patients is beyond salvage, this would tend to reduce the survival rate in this group which might explain our results. Future work with better prehospital data may help address this issue. Additionally, injury patterns by mechanism vary widely and relatively crude measures such as the ISS may not capture all data relevant to outcomes. For example, gunshot wounds with great vessel injury have been shown in the literature to have very poor outcomes after EDT regardless of SOL on presentation (38), but this might not be adequately captured in AIS scores. Data on source of exsanguination is unfortunately not captured in the PTOS registry. Finally, it is possible that changes in weaponry and the acuity with which penetrating trauma victims are presenting may have changed mortality for patients with GSWs referent to historical data. Over the past two decades, there has been a trend towards larger caliber more destructive weapons, and an increase in semi-automatic weapons (39). A recent retrospective analysis from Denver Health Medical Center underscores this concept with the finding that victims of gunshot wounds are presenting with higher ISS scores and an increase in the number of severe gunshot wounds. Additionally, mortality from firearms increased over the study period, whereas mortality from every other injury mechanisms remained the same or improved (40). As retrospective analyses can determine association but not causality, the most correct explanation for our finding of improved survival with blunt trauma compared to gunshot wounds will require further investigation.
Our study has limitations and suffers from the inherent weaknesses of a retrospective investigation. Because the PTOS registry contains only data from trauma centers in a single state, we are unable to say whether or not our findings are generalizable to the national scale. However, attempts to use large national datasets such as the National Trauma Data Bank (NTDB) to determine the relationship between center EDT volume and outcomes are limited because the NTDB does not contain location data for procedures. We therefore do not believe it is possible to reliably differentiate between thoracotomies performed in the emergency department on arrival and thoracotomies that may have been performed in the operating room using the NTDB. Because patients who will tolerate transport to the operating room for thoracotomy are likely to be systematically different than those requiring thoracotomy on arrival, any large registry study combining these two groups would be expected to demonstrate unexpectedly high rates of survival secondary to misclassification bias. Although there is no gold standard in the volume-outcomes literature, we used percentiles of volume to analyze our data as it is a common approach used in the medical outcomes literature. We tested other more complex statistical methods, such as multivariable fractional polynomial models, and ultimately found our results using tertiles to be similar. For the sake of simplicity and clarity, we elected to use percentiles. Finally, were not able to define the presence of signs of life with as much granularity as has been reported in case series of EDT. The PTOS registry does not capture patient movement, pupillary response or other common definitions of SOL, and thus our definition differs from other broader definitions found in the literature. However, the definition we used of SOL had an extremely strong association with survival and did an outstanding job classifying survivors vs. non-survivors.
Conclusions
This study is the first to demonstrate a relationship between institutional emergency department thoracotomy volume and improved patient survival rates. We found that signs of life on arrival to the trauma bay is by far the most important predictor of survival in patients undergoing EDT for both penetrating and blunt trauma. When considering EDT as applied throughout a statewide trauma system procedure and not in specialized, high-volume trauma centers, blunt injury may be associated with higher survival than has been previously reported. Because regionalization of emergent HILF procedures is unlikely to be a realistic goal, further investigation into mediators of improved outcomes associated with higher emergent HILF procedural volumes is warranted. Increased understanding of the provider and system level factors that mediate improved survival at higher volume centers may inform future interventions designed to improve outcomes at lower volume centers.
Footnotes
Study type: Level 3: Retrospective cohort study
Meetings at which this was presented: 47th World Surgical Congress, August 13-17, 2017, Basel Switzerland. Article Type: Clinical Science
Conflicts of Interest and Source of Funding: No authors have conflicts to declare. DNH is currently supported by a training grant through the National Heart, Lung, and Blood Institute. (K08HL131995)
References
- 1.Hamilton AJ, Prescher H, Biffar DE, Poston RS. Simulation trainer for practicing emergent open thoracotomy procedures. J Surg Res. 2015;197(1):78–84. doi: 10.1016/j.jss.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 2.Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. New England Journal of Medicine. 2002;346(15):1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 3.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon Volume and Operative Mortality in the United States. New England Journal of Medicine. 2003;349(22):2117–27. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 4.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. New England Journal of Medicine. 1979;301(25):1364–9. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- 5.Pearce WH, Parker MA, Feinglass J, Ujiki M, Manheim LM, Sawyer W, Schneider J, McCarthy W, III, Blebea J, Hertzer N. The importance of surgeon volume and training in outcomes for vascular surgical procedures. Journal of Vascular Surgery. 1999;29(5):768–78. doi: 10.1016/s0741-5214(99)70202-8. [DOI] [PubMed] [Google Scholar]
- 6.Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. Journal of the American Medical Association. 1999;281(14):1310–7. doi: 10.1001/jama.281.14.1310. [DOI] [PubMed] [Google Scholar]
- 7.Brenner ML, Moore LJ, DuBose JJ, Tyson GH, McNutt MK, Albarado RP, Holcomb JB, Scalea TM, Rasmussen TE. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. The journal of trauma and acute care surgery. 2013;75(3):506–11. doi: 10.1097/TA.0b013e31829e5416. [DOI] [PubMed] [Google Scholar]
- 8.Du Bose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, Moore L, Holcomb J, Turay D, Arbabi CN, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA) Journal of Trauma and Acute Care Surgery. 2016;81(3):409–19. doi: 10.1097/TA.0000000000001079. [DOI] [PubMed] [Google Scholar]
- 9.Burlew CC, Moore EE, Moore FA, Coimbra R, McIntyre RC, Jr, Davis JW, Sperry J, Biffl WL. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012;73(6):1359–63. doi: 10.1097/TA.0b013e318270d2df. [DOI] [PubMed] [Google Scholar]
- 10.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190(3):288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 11.Seamon MJ, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, Fox N, Jawa RS, Khwaja K, Lee JK, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma. Journal of Trauma and Acute Care Surgery. 2015;79(1):159–73. doi: 10.1097/TA.0000000000000648. [DOI] [PubMed] [Google Scholar]
- 12.Søreide K, Petrone P, Asensio JA. Emergency thoracotomy in trauma: Rationale, risks, and realities. Scandinavian Journal of Surgery. 2007;96(1):4–10. doi: 10.1177/145749690709600102. [DOI] [PubMed] [Google Scholar]
- 13.Bennett DA. How can I deal with missing data in my study? Australian & New Zealand Journal of Public Health. 2001;25(5):464–9. [PubMed] [Google Scholar]
- 14.Barzi F, Woodward M. Imputations of missing values in practice: results from imputations of serum cholesterol in 28 cohort studies. Am J Epidemiol. 2004;160(1):34–45. doi: 10.1093/aje/kwh175. [DOI] [PubMed] [Google Scholar]
- 15.Haider AH, Weygandt PL, Bentley JM, Monn MF, Rehman KA, Zarzaur BL, Crandall ML, Cornwell EE, Cooper LA. Disparities in trauma care and outcomes in the United States: A systematic review and meta-analysis. The journal of trauma and acute care surgery. 2013;74(5):1195–205. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006;355(1):41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- 17.Shahul S, Hacker MR, Novack V, Mueller A, Shaefi S, Mahmood B, Ali SH, Talmor D. The effect of hospital volume on mortality in patients admitted with severe sepsis. PLoS One. 2014;9(9):e108754. doi: 10.1371/journal.pone.0108754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waits SA, Sheetz KH, Campbell DA, Ghaferi AA, Englesbe MJ, Eliason JL, Henke PK. Failure to rescue and mortality following repair of abdominal aortic aneurysm. J Vasc Surg. 2014;59(4):909–14. doi: 10.1016/j.jvs.2013.10.078. e1. [DOI] [PubMed] [Google Scholar]
- 19.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74(5):531–6. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 20.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–32. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 21.Martin MJ, Mullenix PS, Steele SR, Asensio JA, Andersen CA, Demetriades D, Salim A. Functional outcome after blunt and penetrating carotid artery injuries: analysis of the National Trauma Data Bank. J Trauma. 2005;59(4):860–4. doi: 10.1097/01.ta.0000187964.47703.e9. [DOI] [PubMed] [Google Scholar]
- 22.Caputo LM, Salottolo KM, Slone DS, Mains CW, Bar-Or D. The relationship between patient volume and mortality in American trauma centres: a systematic review of the evidence. Injury. 2014;45(3):478–86. doi: 10.1016/j.injury.2013.09.038. [DOI] [PubMed] [Google Scholar]
- 23.Matsushima K, Schaefer EW, Won EJ, Armen SB, Indeck MC, Soybel DI. Positive and negative volume-outcome relationships in the geriatric trauma population. JAMA Surg. 2014;149(4):319–26. doi: 10.1001/jamasurg.2013.4834. [DOI] [PubMed] [Google Scholar]
- 24.Minei JP, Fabian TC, Guffey DM, Newgard CD, Bulger EM, Brasel KJ, Sperry JL, MacDonald RD. Increased Trauma Center Volume Is Associated With Improved Survival After Severe Injury: Results of a Resuscitation Outcomes Consortium Study. Annals of surgery. 2014;260(3):456–65. doi: 10.1097/SLA.0000000000000873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, Rivara FP. Relationship between trauma center volume and outcomes. Jama. 2001;285(9):1164–71. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 26.Weinberg JA, Fabian TC. Does Volume Affect Outcome with Severe Trauma? Adv Surg. 2015;49:235–45. doi: 10.1016/j.yasu.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 27.Seamon MJ, Fisher CA, Gaughan JP, Kulp H, Dempsey DT, Goldberg AJ. Emergency department thoracotomy: Survival of the least expected. World Journal of Surgery. 2008;32(4):604–12. doi: 10.1007/s00268-007-9392-9. [DOI] [PubMed] [Google Scholar]
- 28.Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, Flint L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371–8. doi: 10.1097/01.ta.0000197916.99629.eb. discussion 8. [DOI] [PubMed] [Google Scholar]
- 29.Mullins RJ, Mann NC. Population-based research assessing the effectiveness of trauma systems. J Trauma. 1999;47(3 Suppl):S59–66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 30.Burton KS, Pendergrass TL, Byczkowski TL, Taylor RG, Moyer MR, Falcone RA, Geis GL. Impact of simulation-based extracorporeal membrane oxygenation training in the simulation laboratory and clinical environment. Simulation in Healthcare. 2011;6(5):284–91. doi: 10.1097/SIH.0b013e31821dfcea. [DOI] [PubMed] [Google Scholar]
- 31.Hunt EA, Shilkofski NA, Stavroudis TA, Nelson KL. Simulation: Translation to Improved Team Performance. Anesthesiology Clinics. 2007;25(2):301–19. doi: 10.1016/j.anclin.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Lighthall GK, Poon T, Harrison TK. Using in situ simulation to improve in-hospital cardiopulmonary resuscitation. Joint Commission Journal on Quality and Patient Safety. 2010;36(5):209–16. doi: 10.1016/s1553-7250(10)36034-x. [DOI] [PubMed] [Google Scholar]
- 33.Martin JT, Reda H, Dority JS, Zwischenberger JB, Hassan ZU. Surgical resident training using real-time simulation of cardiopulmonary bypass physiology with echocardiography. Journal of Surgical Education. 2011;68(6):542–6. doi: 10.1016/j.jsurg.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 34.Custalow CB, Kline JA, Marx JA, Baylor MR. Emergency department resuscitative procedures: animal laboratory training improves procedural competency and speed. Acad Emerg Med. 2002;9(6):575–86. doi: 10.1111/j.1553-2712.2002.tb02294.x. [DOI] [PubMed] [Google Scholar]
- 35.Asensio JA. Practice management guidelines for emergency department thoracotomy. Journal of the American College of Surgeons. 2001;193(3):303–9. doi: 10.1016/s1072-7515(01)00999-1. [DOI] [PubMed] [Google Scholar]
- 36.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: Review of published data from the past 25 years. Journal of the American College of Surgeons. 2000;190(3):288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell TA, Waldrep KB, Sams VG, Wallum TE, Blackbourne LH, White CE. An 8-year review of operation enduring freedom and operation iraqi freedom resuscitative thoracotomies. Military Medicine. 2015;180(3):33–6. doi: 10.7205/MILMED-D-14-00440. [DOI] [PubMed] [Google Scholar]
- 38.Seamon MJ, Shiroff AM, Franco M, Stawicki SP, Molina EJ, Gaughan JP, Reilly PM, Schwab CW, Pryor JP, Goldberg AJ. Emergency department thoracotomy for penetrating injuries of the heart and great vessels: An appraisal of 283 consecutive cases from two urban trauma centers. Journal of Trauma - Injury, Infection and Critical Care. 2009;67(6):1250–7. doi: 10.1097/TA.0b013e3181c3fef9. [DOI] [PubMed] [Google Scholar]
- 39.McGonigal MD, Cole J, Schwab CW, Kauder DR, Rotondo MF, Angood PB. Urban firearm deaths: a five-year perspective. J Trauma. 1993;35(4):532–6. discussion 6-7. [PubMed] [Google Scholar]
- 40.Sauaia A, Gonzalez E, Moore HB, Bol K, Moore EE. Fatality and Severity of Firearm Injuries in a Denver Trauma Center, 2000-2013. JAMA. 2016;315(22):2465–7. doi: 10.1001/jama.2016.5978. [DOI] [PubMed] [Google Scholar]


