Abstract
Background
Tube thoracostomy (TT) complications and their reported rates are highly variable (1–40%) and inconsistently classified. Consistent TT complication classification must be applied to compare reported literature to standardize TT placement. We aim to determine the overall TT related complication rates in patients receiving TT for traumatic indications utilizing uniform definitions.
Method
Systematic review and meta-analysis was performed assessing TT related complications. Comprehensive search of several databases (1975–2015) was conducted. We included studies that reported on bedside TT insertion (≥ 22 F) in trauma patients. Data were abstracted from eligible articles by independent reviewers with discrepancies reconciled by a third. Analyses were based on complication category subtypes: insertional, positional, removal, infection/immunologic/education and malfunction.
Results
Database search resulted in 478 studies; after applying criteria 29 studies were analyzed representing 4981 TTs. Injury mechanisms included blunt 60% [49–71], stab 27% [17–34], and gunshot 13% [7.8–10]. Overall median complication rate was 19% (95% CI, 14 – 24.3). Complication subtypes included insertional (15.3%), positional (53.1%), removal (16.2%), infection/immunologic (14.8%), malfunction (0.6%). Complication rates did not change significantly over time for insertional, immunologic, or removal p=0.8. Over time, there was a decrease in infectious related TT complications as well as an increase in positional TT complications.
Conclusions
Generation of evidence based approaches to improve TT insertion outcomes is difficult as a variety of complication classifications have been utilized. This meta-analysis of complications after TT insertion in trauma patients suggests that complications have not changed over time remaining stable at 19% over the past three decades.
Level of Evidence
III
Study type
Systematic review and meta-analysis
Keywords: complications, tube thoracostomy, complication classification, meta-analysis, insertional
Introduction
Tube thoracostomy (TT) is commonly utilized in trauma for the removal of pleural fluids and air which may interfere with cardiopulmonary function. Complications related to TT insertion are underestimated, yet remain a source of significant morbidity, mortality, and cost (1–3). The current reported complication rates are increasing to 20–40% whereas earlier cohorts reported lesser rates of 5–20% (3–32). A lack of uniform complication reporting obfuscates any meaningful differences in outcomes over time. Furthermore, any generalizability and applicability of TT related research is limited due to the lack of meaningful comparability. To address this lack of comparability for TT related complication reporting, Aho et al utilized systematic review to generate a method for consistent reporting of complication types into five clearly defined categories: insertional, positional, infective/immunologic, removal, and malfunction (33)
In order to obtain higher quality data and in an effort to ultimately reduce the complications related to TT insertion, a uniform methodology to assign and define complication types has been created and validated. This system has been previously applied and demonstrates the ability to discern TT related complications (1,2,33). Therefore, we aimed to apply this uniform methodology to previously published reports by performing a systematic review and meta-analysis to determine complication rates related to TT insertion in the trauma setting and the rates of complication subtypes. We hypothesized that after uniform classification of complications, the complication rates would demonstrate a consistent rate throughout time and that the majority of complications would be related to positional complications.
Methods
Data sources and search strategies
This study was exempt from IRB review consistent with the Deceleration of Helsinki. A comprehensive search was conducted of several databases from inception to December 22, 2015, in the English language, and including any population. The databases included Ovid Medline In-Process & Other Non-Indexed Citations, Ovid MEDLINE, Ovid EMBASE, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, and Scopus. The search strategy was designed and conducted by an experienced librarian (L.P.), with input from the study’s principal investigators (M.C.H and J.M.A). Controlled vocabulary supplemented with keywords was used to search for studies involving tube thoracostomy insertion in the trauma setting. This review adhered to the standards of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (34). The abstracts from the literature search results were screened through PRISMA guidelines; with inclusion and exclusion criteria generated a priori. The study must have involved the reporting of complications after the insertion of TT for urgent/emergent trauma associated indications. Studies using ultrasound guided TT or pig-tail catheter insertion or TT insertion for non-traumatic indications were excluded. With respect to the size of the TT, studies that evaluated ≥22 French TT were included. TT that was placed in either the pre-hospital or in-patient setting by paramedics, physicians, resident physicians, or nurses was included given the broad spectrum of individuals that perform this procedure. Abstracts were reviewed by two investigators (M.C.H and M.E.K) independently in duplicate and a third investigator (J.M.A.) settled any disagreements. Studies passing abstract screenings were reviewed in full similarly.
TT Complication reporting
The classification system employed in this study assigned complications into five separate categories based on a validated classification methodology (33): insertional, positional, removal, infectious/immunologic, and device malfunction, Table 1. Insertional related complications were considered intra/extra thoracic injuries to a structure after placement within 24 hours of placement. Positional related complications were due to malposition of the TT after placement after 24 hours of TT dwell time. Removal related complications included recurrence of pneumothorax, hemorrhage, or retained foreign body. Infectious or immunologic complications included development of an empyema or an infected retained hemothorax. Finally complications related to instruction/education/equipment failure were recorded as well. These complications consist of a lack of knowledge or education for equipment utilized for TT insertion or those related to nursing or patients clinical knowledge or education. An example includes improper connection of the tube to a water seal device or connecting a Heimlich valve backwards. This complication system, demonstrates research applicability, is simple, reproducible, and consistently reports complications (33,35). Moreover, it has already been utilized in research settings to define optimal angle of insertion and costs incurred due to tube thoracostomy related complications (1,2). The descriptions in Table 1 are not exhaustive of the potential complications that can occur, detailed complication reporting definitions may be found in prior work (33).
Table 1.
Standardized TT complication reporting tool [21]
| Complication Category | Examples of Complication | Specific Injuries Documented | |
|---|---|---|---|
| Insertional | |||
| Intrathoracic | Injury to structure upon placement within 24 hours | ||
| Extrathoracic | Injury to structure upon placement within 24 hours | ||
|
| |||
| Positional | |||
| Intrathoracic | Kinked/obstructed | ||
| Erosion into structures >24 hours after placement | |||
| Compression of structures >24 hours after placement | |||
| Extrathoracic | Subcutaneous injury | ||
| Abdominal injury without organ injury | |||
| Abdominal organ erosion into structures >24 hours after placement | |||
|
| |||
| Removal | Postremoval pneumothorax requiring procedural intervention | ||
| Postremoval bleeding | |||
| Spontaneous dislodgement | |||
| Retained foreign object | |||
|
| |||
| Infective/Immunologic | Infective | ||
| Minor | Site infection | ||
| Major | Empyema | ||
| Necrotizing fasciitis | |||
| Scalded skin syndrome | |||
| Immunologic | Pyoderma gangrenosum | ||
|
| |||
| Instructional/Educational/Equipment | Malfunction of equipment | ||
| Patient care education | |||
| Improper equipment setup | |||
| Improper securement not resulting in dislodgement, requiring intervention | |||
Statistical methods
Baseline patient demographics, injury pattern and mechanism, and tube thoracostomy complications were abstracted from each included article. Tube thoracostomy complications as originally reported in the analyzed data were reassigned based the previously validated complication classification system (33). Each of the complications was assigned a complication subtype. Outcomes (overall tube thoracostomy complication rate and complication subtypes) were evaluated by frequency.
All continuous variables were described using means with standard deviations (SD) if normally distributed and medians with inter-quartile ranges [IQR] if gross skewness was present. Categorical variables were summarized as proportions. Rates of complication subtype were calculated. Univariate analyses to assess the relationship of complication subtype and time using non-parametric, and ANOVA tests were used when appropriate. All analyses were performed using JMP (SAS Institute, Inc. Cary NC). GraphPad Prism (GraphPad Software, Inc. La Jolla CA) was utilized for visual graphics.
Results
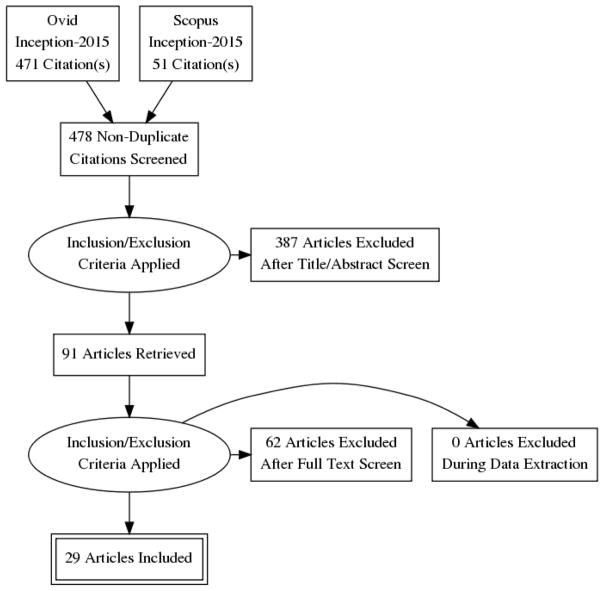
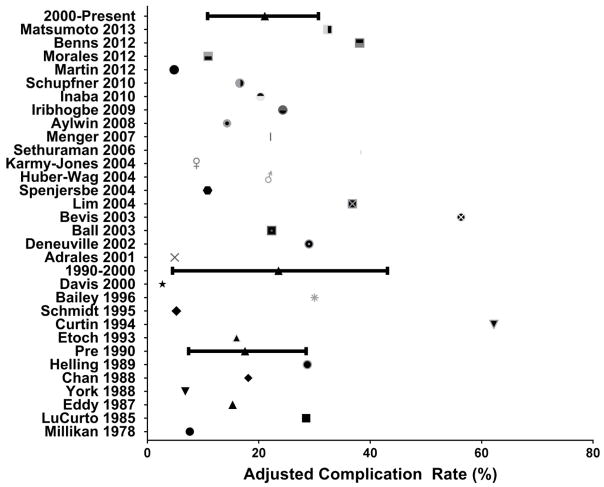
Our database search resulted in 478 studies which were reviewed using inclusion and exclusion criteria according to PRISMA criteria (Figure 1). After application of inclusion/exclusion criteria, 29 papers were reviewed. Overall, 4981 TT insertions were analyzed. The reported complication rate during the study period was 19% (n=949). Table 2 outlines the complication nomenclature utilized in each study. Over time there has been significant variation in the way complications are reported. Not all reports have the same definitions, even for similar complication types like intraparenchymal placement. Moreover, the definitions utilized were broad. For example, Millikan et al utilized diaphragmatic perforation, empyema, and iatrogenic injury to a viscus as definitions for TT related complications. These were reclassified as insertional and infectious. Conversely, complications due to removal were more inclusive of recurrent/unresolved pneumothorax which was defined in (n=7, 24%) of studies. Some studies defined complications utilizing cross-sectional imaging confirmation (n=3, 10%). These underscore the variety of definitions incorporated within the literature for traumatically injured patients requiring TT large bore TT insertion. Figure 2 outlines the individual study complication rates and demonstrates that the overall complication rate has not significantly changed despite the variation in complication definition reporting.
Figure 1.
PRISMA Flow diagram
Table 2.
Description of complication types within each report
| Author | Complication Type (s) Reported | Complication Category Utilized |
|---|---|---|
| Millikan et al | Diaphragmatic perforation, empyema and viscus iatrogenic injury | Insertional, Infectious |
| LoCurto et al | Empyema | Infectious |
| Eddy et al | Empyema and incomplete pleural drainage | Infectious |
| Helling et al | Empyema, retained hemothorax, air leak | Infectious, Removal |
| York et al | TT related hemorrhage, misplacement or empyema | Insertional, Infectious |
| Curtin et al | Fissural or non fissural TT, intra-parenchymal | Positional, Insertional |
| Etoch et al | Undrained pneumothorax or effusion, pneumothorax following TT removal, inadequate placement requiring another TT, empyema, and other | Removal, Insertional, Infectious |
| Chan et al | Empyema, unresolved pneumothorax, persistent effusion, incorrect placement | Infectious, Removal, Insertional |
| Schmidt et al | TT malfunction or malpositioning | Positional |
| Bailey et al | Insertional (organ laceration or perforation, hemorrhage), positional or infective | Insertional, Positional, Infectious |
| Adrales et al | Empyema or recurrent pneumothorax | Infectious, Removal |
| Deneuville et al | Improper placement with our without iatrogenic injury, undrained hemo/pneumothorax, recurrent pneumothorax after TT removal, recurrent intrathoracic fluid collections after TT removal, and other | Insertional, Removal, Positional |
| Davis et al | Visceral injury, tube dislodgement, superficial skin infection, extrapleural tube placement, intraabdominal placement | Insertional, Positional |
| Lim et al | Tube malposition (fissure, extrapleural or intraparenchymal) | Positional, Insertional |
| Spanjersberg et al | Empyema, extrapleural placement | Infectious, Insertional |
| Ball et al | Insertional, Positional, Infective | Insertional, Positional, Infectious |
| Huber-Wagner et al | TT malposition | Positional |
| Aylwin et al | Life threatening conditions after TT insertion and non-life threatening conditions | Insertional, Positional |
| Bevis et al | TT kink, extrapleural placement, mediastinum abutment, intrafissure placement, intra-abdominal or transdiaphragmatic placement | Positional, Insertional |
| Karmy-Jones et al | Empyema | Infectious |
| Menger et al | Recurrent/residual hemo/pneumothorax, empyema | Removal, Infectious |
| Iribhogbe et al | Insertional (organ laceration or perforation, hemorrhage), positional or infective | Insertional, Positional, Infectious |
| Sethuraman et al | Immediate/delayed, major/minor | Insertional, Positional |
| Inaba et al | Pneumonia, empyema, retained or unresolved hemo/pneumothorax | Infectious, Removal |
| Martin et al | Air leak, persistent pneumothorax, infection, clotted/positional/kink causing non functional TT | Removal, Insertional, Positional |
| Schupfner et al | Interlobar, interparenchymal, and extrathoracic position | Positional |
| Morales et al | Air leak, clotted TT, empyema, recurrent pneumothorax | Removal, Positional, Infectious |
| Benns et al | Intraparenchymal, extrahoracic, fissural | Insertional, Positional |
| Matsumoto et al | Radiologic malposition(extrathoracic, abdominal, parenchymal or interlobal) or residual pneumothorax (functional versus nonfunctional) | Insertional, Positional |
Figure 2.
Individual complication rates for included studies adjusted using standardized classifications
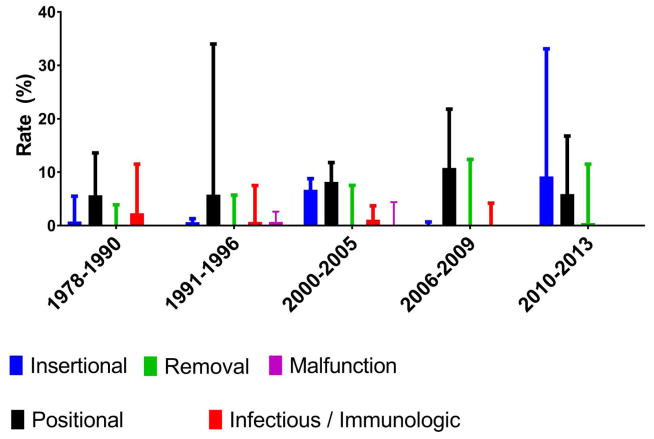
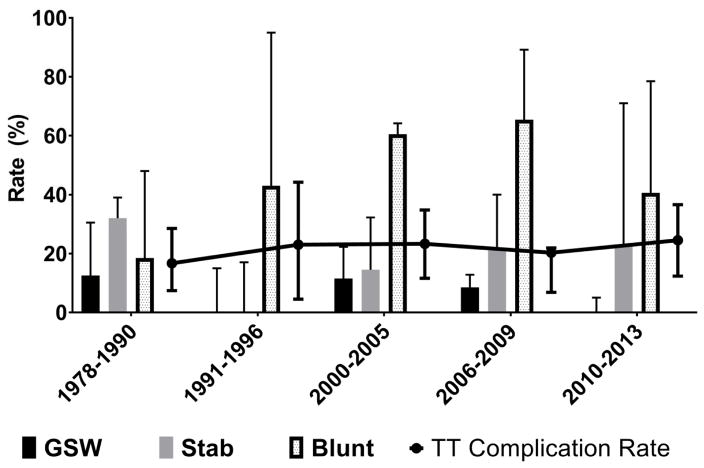
Figure 3 categorizes the TT related complication rates by subtype. Over time several trends may be recognized. First the rates of positional related complications steadily increase with time but rapidly diminish in most recent reports. Moreover, the rates of insertional complications increase with time and the greatest burden of insertional related complications is in more recent cohorts. Removal related complications do not have a significant trend over time. Finally, infectious related complications (empyema) diminish with time and are absent in the most recent reports. The rate of infectious related complications decreased from the pre-2000 studies to the current post-2000 cohorts (10% versus 1%, p=0.03). There were no immunologic (allergic reaction to tube) complications. Figure 4 demonstrates the rates of traumatic mechanisms and complication subtype after TT insertion respectively. While the rates of TT related complications relatively remained the same in the analyzed data, the characteristics of traumatic injury changed. Gunshot wound related injuries diminished with time whereas the rates of blunt injury increased without concomitant changes in TT complication rates. Stab related wounds did not demonstrate an association with TT related complications. Similarly, the blunt trauma mechanism rate increased (pre year 2000 of 19% versus post year 2000 61%, p=0.04) but did not appear to have an influence on the TT related complications.
Figure 3.
Median [IQR] Rate of complication subtypes during thirty years
Figure 4.
Traumatic mechanism during the past thirty years requiring tube thoracostomy
Excluding studies that evaluated non-physician providers inserting TT (n=3), there was a similar rate of complications between resident surgeons and board certified surgeons (20.3% versus 22.1%, p=0.66). The vast majority of included manuscripts reviewed outcomes after TT insertion solely by resident surgeons (n=21 manuscripts) or solely by board certified surgeons (n=5 manuscripts). Likely the similarity of complications between residents and surgeons is due to complication underreporting.
Discussion
The lack of a universally accepted TT complication classification system has prevented the rigorous interpretation of technique and outcomes related to TT insertion. Complications, as defined by the included studies, varied widely in classification and with time. The adequate comparison of outcomes, determination of complication root causes, improving TT insertion education, and estimating complication severity is not easily possible. Through systematic review and meta-analysis, we demonstrated that the complication rate after TT insertion in trauma setting is 19%. This rate remained steady during the period of analysis. We determined that nearly one in five patients with a TT suffer some form of complication. This is concerning and suggests a better understanding of TT related complication is required. Reclassification of previously heterogeneous complications types between studies demonstrated 1) no substantial change in the rate of insertional, or removal complications, 2) a notable decrease in the rate of infectious complications and 3) there was a considerable increase in the rate of positional complications. Despite a relatively unchanging complication rate, this work underscores a potential need to reevaluate TT insertion technique, improve complication recognition during critical time points, and improve efforts to standardize both education and performance of this common procedure.
During the past three decades, variability in the reporting, classification, and consideration of TT related complications existed. Millikan et al defined complications only as major – insertion into the abdominal cavity or lung parenchyma (4). In a more recent prospective trial, complications were reported with increasing granularity and included pneumonia, empyema, or hemothorax (27). Even further, complication rates have been reported as high as 60% in 2017 that used inclusive TT complications definitions (fissural placement, transdiaphragmatic placement, dislodgment, vascular injury, empyema, surgical site infection, iatrogenic injury and even drainage failure) (36). To reduce variability in TT related complication reporting, our prior work utilized systematic review (33) to generate a method for consistent reporting of complication types into several categories: insertional, positional, infective/immunologic, removal, and malfunction. This methodology provides a validated framework for complication reporting which is inclusive and standardized for all potential subtypes (33).
Positional complications increased during the study period. This increase most likely represents utilization of improved complication definitions in more recent studies. Furthermore, advancements in cross sectional imaging have permitted in depth inspection of the thoracic cavity post TT insertion. This also may have influenced the increase in recognized positional complication rates and the impact that a poorly positioned TT has on functionality. Historically, TT insertion location are performed based on indication such as hemothorax or pneumothorax (37). A recent analysis by Kugler et al demonstrated using multivariate analysis that non-ideal TT trajectory of the intra-thoracic TT was associated with secondary interventions (38). This work highlights that TT function, rather than position, dictates additional TT placement or repositioning. Taken together, positional TT related complications and their subsequent management may be difficult. Early recognition as well as attention to proper technique may assist surgeons to prevent and reduce this complication subtype.
Our analysis also demonstrated there was a reduction in TT related infectious complications during the study period. This reduction is likely multifactorial. A simple explanation involves an improved focus on sterile technique during TT insertion. Moreover, attention to early TT removal may also coincide with decreases in infectious related TT complications (empyema foremost). A variety of changes in clinical practice such as antibiotic administration for concurrent injuries or even prophylactic antibiotics for isolated penetrating chest trauma who required a TT may have additional impact on reducing infectious related complication rates. Determining the major cause of this effect is difficult, but substantiates vigilance for sterile technique during insertion. Dubose et al demonstrated an increased risk for empyema in patients with rib fractures, elevated Injury Severity Scores (ISS), and need for additional procedures to intra-thoracic blood (39). Efforts to minimize infectious complications have also been evaluated. Kugler et al utilized irrigation and suction of the thorax in a pilot study and demonstrated improvements on chest radiograph (40). This was further assessed by Savage et al wherein the authors compared patients receiving suction evacuation compared to historical controls (41). While no demonstrable improvements were made in the rates of empyema or development of retained hemothorax, these efforts highlight the use of minimally invasive techniques that with time may clarify our understanding in preventing empyema and infectious related complications in severely injured patients.
Traumatic mechanisms requiring TT insertion demonstrated variability. While the injury patterns changes with time, notably increasing rates of blunt injury, the complications related to TT insertion did not change. This coincides with evidence previously reported by Cothren et al (42) which demonstrates diminishing rates of intentionally related injuries and increasing rates of blunt related trauma.
There are several limitations to the conclusions generated in this study. Significantly, the majority of studies did not identify all complications. The lack of uniform complication reporting makes it possible that our analysis to determine specific complication subtype rates difficult. As this is a meta-analysis of complication reporting related to TT insertion, our analysis did not include measures of injury type, patient specific factors, location and timing of injury, or operative interventions. These limit our findings; however, we submit that complication recognition utilizing more uniform definitions will be beneficial to improve complication recognition and efforts to minimize complication development. The sizes and method of placement of the TT were not uniform in each study and therefore different complications could potentially ensue for different TT sizes (22 F versus 36 F). Finally, there is no prospective study that assesses the ability of this complication reporting system to accurately describe and account for all TT related complications; however, it does provide an initial method for equitable comparisons. Since there is significant bias and heterogeneity of complications in the current literature, we analyzed and re-classified the available complication data from each manuscript. We undertook the effort to reduce the bias and heterogeneity by focusing purely on patient that incurred trauma and received at the minimum a 22 F TT. Our analysis is thus focused on a select population albeit a population that TT is commonly utilized. A publication bias may present as included studies may not want to report complications outside the reported range compared to the current literature. We were only able to analyze (6%, n=29) of the 478 studies based on our inclusion criteria. Several of the studies were single institutional retrospective reviews, which limits our conclusions. Our findings are derived from a very small subset of patients that received a larger bore TT. This impacts interpretation of our results, highlighting that our focused precision on improving complication reporting may not necessarily be generalizable when smaller TT catheters are utilized, or in patients receiving TT for non-traumatic indications. Further, negative findings that demonstrated no differences based upon operator type, tube size, angle of insertion, location of insertion etc. may never have been published.
Conclusions
Standardization of complications continues to remain a difficult task given the breadth of anatomy that potentially can be injured during tube thoracostomy insertion. In the setting of trauma, the overall TT insertion complication rate demonstrated minimal fluctuation and has been approximately 19% during the past three decades. Further, the data demonstrate an increase in positionally related complications and an incremental decrease in infectious related complications. TT is a potentially lifesaving procedure that is common and performed in multiple disciplines.
Footnotes
This work was not previously published or presented.
Author Contribution:
Study design was developed by Matthew Hernandez, Johnathon Aho, and Martin Zielinski. Data generation was performed by Matthew Hernandez, Moustafah El Khatib, Muhammad Zeb, Larry Prokop Data analysis and interpretation was performed by Matthew Hernandez, Johnathon Aho, Moustafah El Khatib, Muhammad Zeb, and Larry Prokop Manuscript writing was performed by Matthew Hernandez, Johnathon Aho, Larry Prokop and Moustafah El Khatib.
Disclosures and Funding: The authors do not have any relevant disclosures or conflicts of interest for this work and no funding was utilized for this work
References
- 1.Hernandez MC, Zeb MH, Heller SF, Zielinski MD, Aho JM. Tube Thoracostomy Complications Increase Cost. World J Surg. 2017;41(6):1482–1487. doi: 10.1007/s00268-017-3897-7. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez MC, Laan DV, Zimmerman SL, Naik ND, Schiller HJ, Aho JM. Tube thoracostomy: Increased angle of insertion is associated with complications. J Trauma Acute Care Surg. 2016;81(2):366–70. doi: 10.1097/TA.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan L, Reilly KM, Henderson C, Kahn F, Salluzzo RF. Complication rates of tube thoracostomy. Am J Emerg Med. 1997;15(4):368–70.7. doi: 10.1016/s0735-6757(97)90127-3. [DOI] [PubMed] [Google Scholar]
- 4.Millikan JS, Moore EE, Steiner E, Aragon GE, Van Way CW., 3rd Complications of tube thoracostomy for acute trauma. Am J Surg. 1980;140(6):738–41. doi: 10.1016/0002-9610(80)90107-5. [DOI] [PubMed] [Google Scholar]
- 5.LoCurto JJ, Jr, Tischler CD, Swan KG, Rocko JM, Blackwood JM, Griffin CC, Lazaro EJ, Reiner DS. Tube thoracostomy and trauma--antibiotics or not? J Trauma. 1986;26(12):1067–72. doi: 10.1097/00005373-198612000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bevis LC, Berg-Copas GM, Thomas BW, Vasquez DG, Wetta-Hall R, Brake D, Lucas E, Toumeh K, Harrison P. Outcomes of tube thoracostomies performed by advanced practice providers vs trauma surgeons. Am J Crit Care. 2008;17(4):357–63. [PubMed] [Google Scholar]
- 7.Helling TS, Gyles NR, 3rd, Eisenstein CL, Soracco CA. Complications following blunt and penetrating injuries in 216 victims of chest trauma requiring tube thoracostomy. J Trauma. 1989;29(10):1367–70. doi: 10.1097/00005373-198910000-00013. [DOI] [PubMed] [Google Scholar]
- 8.York D, Dudek L, Larson R, Marshall W, Dries D. A comparison study of chest tube thoracostomy: air medical crew and in-hospital trauma service. Air Med J. 1993;12(7):227–9. doi: 10.1016/S1067-991X(05)80187-7. [DOI] [PubMed] [Google Scholar]
- 9.Curtin JJ, Goodman LR, Quebbeman EJ, Haasler GB. Thoracostomy tubes after acute chest injury: relationship between location in a pleural fissure and function. AJR Am J Roentgenol. 1994;163(6):1339–42. doi: 10.2214/ajr.163.6.7992724. [DOI] [PubMed] [Google Scholar]
- 10.Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg. 1995;130(5):521–6. doi: 10.1001/archsurg.1995.01430050071012. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt U, Stalp M, Gerich T, Blauth M, Maull KI, Tscherne H. Chest tube decompression of blunt chest injuries by physicians in the field: effectiveness and complications. J Trauma. 1998;44(1):98–101. doi: 10.1097/00005373-199801000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Bailey RC. Complications of tube thoracostomy in trauma. J Accid Emerg Med. 2000;17(2):111–4. doi: 10.1136/emj.17.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adrales G, Huynh T, Broering B, Sing RF, Miles W, Thomason MH, Jacobs DG. A thoracostomy tube guideline improves management efficiency in trauma patients. J Trauma. 2002;52(2):210–6. doi: 10.1097/00005373-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Deneuville M. Morbidity of percutaneous tube thoracostomy in trauma patients. Eur J Cardiothorac Surg. 2002;22(5):673–8. doi: 10.1016/s1010-7940(02)00478-5. [DOI] [PubMed] [Google Scholar]
- 15.Davis DP, Pettit K, Rom CD, Poste JC, Sise MJ, Hoyt DB, Vilke GM. The safety and efficacy of prehospital needle and tube thoracostomy by aeromedical personnel. Prehosp Emerg Care. 2005;9(2):191–7. doi: 10.1080/10903120590924500. [DOI] [PubMed] [Google Scholar]
- 16.Lim KE, Tai SC, Chan CY, Hsu YY, Hsu WC, Lin BC, Lee KT. Diagnosis of malpositioned chest tubes after emergency tube thoracostomy: is computed tomography more accurate than chest radiograph? Clin Imaging. 2005;29(6):401–5. doi: 10.1016/j.clinimag.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 17.Elsayed H, Roberts R, Emadi M, Whittle I, Shackcloth M. Chest drain insertion is not a harmless procedure--are we doing it safely? Interact Cardiovasc Thorac Surg. 2010;11(6):745–8. doi: 10.1510/icvts.2010.243196. [DOI] [PubMed] [Google Scholar]
- 18.Spanjersberg WR, Ringburg AN, Bergs EA, Krijen P, Schipper IB. Prehospital chest tube thoracostomy: effective treatment or additional trauma? J Trauma. 2005;59(1):96–101. doi: 10.1097/01.ta.0000171448.71301.13. [DOI] [PubMed] [Google Scholar]
- 19.Wells BJ, Roberts DJ, Grondin S, Navsaria PH, Kirkpatrick AW, Dunham MB, Ball CG. To drain or not to drain? Predictors of tube thoracostomy insertion and outcomes associated with drainage of traumatic hemothoraces. Injury. 2015;46(9):1743–8. doi: 10.1016/j.injury.2015.04.032. [DOI] [PubMed] [Google Scholar]
- 20.Ball CG, Lord J, Laupland KB, Gmora S, Mulloy RH, Ng AK, Schieman C, Kirkpatrick AW. Chest tube complications: how well are we training our residents? Can J Surg. 2007;50(6):450–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Huber-Wagner S, Korner M, Ehrt A, Kay MV, Pfeifer KJ, Mutschler W, Kanz KG. Emergency chest tube placement in trauma care - which approach is preferable? Resuscitation. 2007;72(2):226–33. doi: 10.1016/j.resuscitation.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 22.Aylwin CJ, Brohi K, Davies GD, Walsh MS. Pre-hospital and in-hospital thoracostomy: indications and complications. Ann R Coll Surg Engl. 2008;90(1):54–7. doi: 10.1308/003588408X242286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karmy-Jones R, Holevar M, Sullivan RJ, Fleisig A, Jurkovich GJ. Residual hemothorax after chest tube placement correlates with increased risk of empyema following traumatic injury. Can Respir J. 2008;15(5):255–8. doi: 10.1155/2008/918951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menger R, Telford G, Kim P, Bergey MR, Foreman J, Sarani B, Pascual J, Reilly P, Schwab CW, Sims CA. Complications following thoracic trauma managed with tube thoracostomy. Injury. 2012;43(1):46–50. doi: 10.1016/j.injury.2011.06.420. [DOI] [PubMed] [Google Scholar]
- 25.Iribhogbe PE, Uwuigbe O. Complications of Tube Thoracostomy using Advanced Trauma Life Support Technique in Chest Trauma. West Afr J Med. 2011;30(5):369–72. [PubMed] [Google Scholar]
- 26.Sethuraman KN, Duong D, Mehta S, Director T, Crawford D, St George J, Rathley NK. Complications of tube thoracostomy placement in the emergency department. J Emerg Med. 2011;40(1):14–20. doi: 10.1016/j.jemermed.2008.06.033. [DOI] [PubMed] [Google Scholar]
- 27.Inaba K, Lustenberger T, Recinos G, Georgiou C, Velmahos GC, Brown C, Salim A, Demetriades D, Rhee P. Does size matter? A prospective analysis of 28–32 versus 36–40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72(2):422–7. doi: 10.1097/TA.0b013e3182452444. [DOI] [PubMed] [Google Scholar]
- 28.Martin M, Schall CT, Anderson C, Kopari N, Davis AT, Stevens P, Haan P, Kepros JP, Mosher BD. Results of a clinical practice algorithm for the management of thoracostomy tubes placed for traumatic mechanism. Springerplus. 2013;2:642. doi: 10.1186/2193-1801-2-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schupfner R, Wagner W, Schneller A. Results of thoracic drainages placed in air rescue. Interv Med Appl Sci. 2013;5(4):168–74. doi: 10.1556/IMAS.5.2013.4.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morales CH, Mejia C, Roldan LA, Saldarriaga MF, Duque AF. Negative pleural suction in thoracic trauma patients: A randomized controlled trial. J Trauma Acute Care Surg. 2014;77(2):251–5. doi: 10.1097/TA.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 31.Benns MV, Egger ME, Harbrecht BG, Franklin GA, Smith JW, Miller KR, Miller KR, Nash NA, Richardson JD. Does chest tube location matter? An analysis of chest tube position and the need for secondary interventions. J Trauma Acute Care Surg. 2015;78(2):386–90. doi: 10.1097/TA.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 32.Matsumoto S, Sekine K, Funabiki T, Yamazaki M, Orita T, Shimizu M, Hayashida K, Kishikawa M, Kitano M. Chest tube insertion direction: is it always necessary to insert a chest tube posteriorly in primary trauma care? Am J Emerg Med. 2015;33(1):88–91. doi: 10.1016/j.ajem.2014.10.042. [DOI] [PubMed] [Google Scholar]
- 33.Aho JM, Ruparel RK, Rowse PG, Brahmbhatt RD, Jenkins D, Rivera M. Tube Thoracostomy: A Structured Review of Case Reports and a Standardized Format for Reporting Complications. World J Surg. 2015;39(11):2691–706. doi: 10.1007/s00268-015-3158-6. [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339(1):b2535–b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sritharen Y, Hernandez MC, Haddad NN, Kong V, Clarke D, Zielinski MD, Aho JM. External Validation of a Tube Thoracostomy Complication Classification System. World J Surg. 2017 Sep 20; doi: 10.1007/s00268-017-4260-8. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Kashani P, Harati S, Shirafkan A, Amirbeigi A, Hatamabadi HR. Comparing the Quality and Complications of Tube Thoracostomy by Emergency Medicine and Surgery Residents; a Cohort Study. Emerg (Tehran) 2017;5(1):e33. Epub ahead of print. [PMC free article] [PubMed] [Google Scholar]
- 37.Batchelder TL, Morris KA. Critical factors in determining adequate pleural drainage in both the operated and nonoperated chest. Am Surg. 1962;28:296–302. [PubMed] [Google Scholar]
- 38.Kugler NW, Carver TW, Knechtges P, Milia D, Goodman L, Paul JS. Thoracostomy tube function not trajectory dictates reintervention. J Surg Res. 2016;206(2):380–5. doi: 10.1016/j.jss.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 39.DuBose J, Inaba K, Okoye O, Demetriades D, Scalea T, O’Connor J, Menaker J, Morales C, Schiflett T, Brown C, et al. Development of posttraumatic empyema in patients with retained hemothorax. J Trauma Acute Care Surg. 2012;73(3):752–7. doi: 10.1097/TA.0b013e31825c1616. [DOI] [PubMed] [Google Scholar]
- 40.Kugler NW, Carver TW, Paul JS. Thoracic irrigation prevents retained hemothorax: A pilot study. J Surg Res. 2016;202(2):443–8. doi: 10.1016/j.jss.2016.02.046. [DOI] [PubMed] [Google Scholar]
- 41.Savage SA, Cibulas GA, Ward TA, Davis CA, Croce MA, Zarzaur BL. Suction evacuation of hemothorax. J Trauma Acute Care Surg. 2016;81(1):58–62. doi: 10.1097/TA.0000000000001099. [DOI] [PubMed] [Google Scholar]
- 42.Cothren CC, Moore EE, Hedegaard HB, Meng K. Epidemiology of urban trauma deaths: A comprehensive reassessment 10 years later. World J Surg. 2007;31(7):1507–11. doi: 10.1007/s00268-007-9087-2. [DOI] [PubMed] [Google Scholar]