Abstract
Increased attention has focused on methods to increase empathy, compassion, and pro-social behavior. Meditation practices have traditionally been used to cultivate pro-social outcomes, and recently investigations have sought to evaluate their efficacy for these outcomes. We conducted a systematic review and meta-analysis of meditation for pro-social emotions and behavior. A literature search was conducted in PubMed, MEDLINE, PsycINFO, CINAHL, Embase, and Cochrane databases (inception-April 2016) using the search terms: mindfulness, meditation, mind-body therapies, tai chi, yoga, MBSR, MBCT, empathy, compassion, love, altruism, sympathy, or kindness. Randomized controlled trials in any population were included (26 studies with 1,714 subjects). Most were conducted among healthy adults (n=11) using compassion or loving kindness meditation (n=18) over 8–12weeks (n=12) in a group format (n=17). Most control groups were wait-list or no-treatment (n=15). Outcome measures included self-reported emotions (e.g., composite scores, validated measures) and observed behavioral outcomes (e.g., helping behavior in real-world and simulated settings). Many studies showed a low risk of bias. Results demonstrated small to medium effects of meditation on self-reported (SMD = .40, p < .001) and observable outcomes (SMD = .45, p < .001) and suggest psychosocial and neurophysiological mechanisms of action. Subgroup analyses also supported small to medium effects of meditation even when compared to active control groups. Clinicians and meditation teachers should be aware that meditation can improve positive pro-social emotions and behaviors.
Keywords: meditation, mindfulness, empathy, compassion, pro-social
Introduction
There has been a recent increase in research focused on empathy, compassion, and pro-social behaviors (Kirby, 2016; Strauss et al., 2016). Although there are varying definitions of empathy and compassion, they are often considered related but distinct pro-social emotions that consist of cognitive and affective components and can be learned with practice (Bibeau, Dionne, & Leblanc, 2016; Goetz, Keltner, & Simon-Thomas, 2010). Empathy involves vicariously experiencing another’s emotions by recognizing, understanding, and resonating with their emotional state (“putting yourself in someone else’s shoes;” Hogan, 1969; Lazarus, 1991; Strauss et al., 2016). Compassion takes empathy a step further and involves not only emotional recognition, understanding, and resonation, but also the ability to tolerate one’s own emotional reaction and the motivation to act to relieve the others’ suffering (“suffering with;” Gilbert, 2010; Strauss et al., 2016). Actions taken with altruistic intentions to help or benefit another person are broadly considered pro-social behaviors (e.g., volunteerism, charitable donation, care-taking; Penner, Dovidio, Pilavin, & Schroeder, 2005). Research supports the idea that greater empathy leads to greater compassion, and greater compassion leads to greater pro-social behavior (Lim & DeSteno, 2016).
Pro-social emotions and behaviors are important for both individual and societal well-being. Empathy and compassion are emphasized across diverse social institutions, including healthcare, education, and justice systems, as well as most world religions (Faulkner & McCurdy, 2000; Goetz et al., 2010). They are thought to confer adaptive evolutionary value by guiding individuals to protect and care for their offspring, family, as well as other community members, thereby maximizing the likelihood of survival and genetic propagation (Goetz et al., 2010). Pro-social outcomes have a positive public health impact because they not only benefit the individual receiving help, but they also benefit the helper. Indeed, a large body of research demonstrates that engaging in pro-social behavior is associated with greater happiness and psychological well-being, indices of physiological health (e.g., increased heart rate variability, immune function, telomere length, genetic expression), better physical functioning, better interpersonal relationships, and decreased morbidity in medical populations (Dunn, Aknin, & Norton, 2008; Hoge et al., 2013; Ironson, 2007; Nelson, Layous, Cole, & Lyubomirsky, 2016; Pace et al., 2009; Weinstein & Ryan, 2010). These benefits are greater for pro-social behavior as compared to self-focused helping behavior (e.g., Nelson et al., 2016). Given the wide range of social problems currently harming individuals and societies worldwide, the need for greater empathy, compassion, and pro-social behavior is clear (Hurst, Gibbon, & Nurse, 2016; Pascoe & Richman, 2009).
Meditation is one way to increase an individual’s empathy, compassion, and pro-social behavior. Meditation encompasses a collection of mental training practices that involve self-regulating one’s attention toward a chosen object of awareness from one moment to the next; it can take various different forms depending on how and where attention is focused (Kabat-Zinn, 1982; Walsh & Shapiro, 2006). Meditation practices have been used for centuries across a range of contemplative communities and historically emphasized as methods to reduce suffering for the self and others within a moral or religious context of benevolence and non-harming (Goldstein & Kornfield, 2001; Nydahl, 2008; Sears, Tirch, & Denton, 2011). Over the past twenty years, meditation practices have been increasingly secularized and integrated into psychological interventions to improve both negative and positive emotional outcomes (Kirby, 2016).
Two meditation practices that have received particular attention are mindfulness meditation and loving kindness meditation (LKM) practices derived from Buddhist contemplative traditions. Mindfulness meditation involves self-regulating one’s attention to intentionally notice present moment experiences openly and non-judgmentally as they occur (Sears et al., 2011). It incorporates the related practice of concentration meditation in that it involves focused concentration on an object of experience in the present moment. LKM is a more directly pro-social meditative practice aimed at increasing four specific other-oriented positive attitudes: loving kindness, compassion, empathic joy, and equanimity. LKM practices involve intentionally cultivating awareness of feelings of warmth, kindness, and compassion for others through mental visualizations, mantras, and/or other aspirational phrases (Wallace, 1999). There are also compassion meditation practices, which can be similar to LKM practices but have a unique focus on imagining another’s suffering and relieving that person’s suffering (e.g., by extending a heartfelt wish or imagining a golden beam of light toward them). Movement-based meditation practices derived from disciplines such as yoga and tai chi, which combine mindfulness meditation with physical postures or exercises, have also received increased research attention (Luberto, White, Sears, & Cotton, 2013).
There is a strong evidence base to support the efficacy of meditation-based interventions for improving emotional outcomes. This research work had initially been focused on decreasing negative emotions (i.e., rather than increasing positive emotions) using mindfulness-based interventions such as Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1982) and Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2012). The results of several systematic reviews and meta-analyses of mindfulness-based interventions suggest that these treatments significantly improve stress, anxiety, depression, quality of life, and emotion regulation across a range of psychiatric and medical populations (Bohlmeijer, Prenger, Taal, & Cuijpers, 2010; Eberth & Sedlmeier, 2012; Gotink et al., 2015; Hofmann, Sawyer, Witt, & Oh, 2010; Khoury et al., 2013; Piet, Wurtzen, & Zachariae, 2012). Reviews of movement-based mindfulness practices also show promising results for improving emotional problems (e.g., anxiety, depression), though these results are more preliminary given the limited methodological quality of these studies to date (Kirkwood, Rampes, Tuffrey, Richardson, & Pilkington, 2005; Luberto et al., 2013; Uebelacker et al., 2010).
More recently, research has begun to focus on LKM practices to decrease negative and promote positive emotions. Hofmann et al. (2010) suggested that LKM practices may be integrated into cognitive-behavioral therapies to improve emotions and behaviors related to interpersonal relationships, and a recent meta-analysis found that LKM indeed improves depression, mindfulness, compassion, self-compassion, and positive affect (Galante, Galante, Bekkers, & Gallacher, 2014). Other meta-analyses of LKM for improving self-oriented positive emotions (Zeng, Chiu, Wang, Oei, & Leung, 2015) and general psychosocial outcomes (Shonin, Van Gordon, Compare, Zangeneh, & Griffiths, 2015) have shown significant benefits. A narrative review also suggested that compassion meditation promotes pro-social outcomes in psychotherapists (Bibeau et al., 2016).
Despite the multiple reports of meditation and emotional well-being, no research has systematically reviewed the results of meditation interventions for pro-social outcomes. Previous systematic reviews and meta-analyses have tended to focus on one specific type of meditation practice (e.g., mindfulness or LKM; Galante et al., 2014; Zeng et al., 2015;), negative emotions (Hofmann et al., 2010), or self-focused positive emotions (e.g., Zeng et al., 2015). Those that did incorporate empathy and compassion outcomes either did not specifically include pro-social search terms (Galante et al., 2014; Shonin et al., 2015), or were not systematic and only examined outcomes in one specific population (i.e., psychotherapists; Bibeau et al., 2016). Thus, a comprehensive and systematic review of meditation for pro-social outcomes is lacking.
The purpose of the current study is therefore to conduct a systematic review and meta-analysis of randomized controlled trials of meditation-based clinical interventions for improving pro-social emotions and behaviors. Specifically, the aims are to synthesize existing results regarding effects and potential mechanisms of meditation for pro-social outcomes, estimate the effect size of meditation on pro-social outcomes, assess the quality of trials conducted, identify directions for future research, and draw evidence-based conclusions to guide future research and clinical practice.
Method
Literature Search
A literature search was performed by a medical librarian (LP) in the Ovid Medline, PubMed, Ovid PsycINFO, CINAHL, Embase, Cochrane Library, and ClinicalTrials.gov databases from inception through April 2016. Similar to previous reviews of meditation (Gotink et al., 2015), search terms were intended to capture studies of meditation interventions that have been secularized for delivery in standard clinical practice settings. We only included secular practices because these are more likely to be offered in standard clinical practice settings (e.g., MBCT, MBSR), they can promote a wider outreach for individuals who may not subscribe or feel comfortable with non-secular practices, and much of the literature to date has tended to focus on secularized interventions. Non-secular practices are also often religion-specific and may not be generalizable. Prayer was excluded as it is inherently non-secular. Also similar to previous reviews, cognitive-behavioral therapies (CBT) that do not use formal meditation practice consistently as the foundation of treatment were excluded (e.g., traditional CBT, Dialectical Behavior Therapy, Acceptance and Commitment Therapy; Hofmann et al., 2010). Thus, search terms included: meditation, mindfulness, MBSR, MBCT, mind-body therapies, tai chi, yoga, empathy, compassion, sympathy, love, altruism, and kindness. Each search query was combined with a filter based on Royle and Waugh’s search strategy for identifying randomized controlled trials for systematic reviews (Royle & Waugh, 2005). An additional filter was used to limit to English language studies. No publication date limits were used. See Appendix A for the full search strategy in Ovid Medline.
Eligibility Criteria
Randomized controlled trials of a meditation-based intervention that assessed at least one quantitative outcome related to pro-social emotions or behaviors were eligible for inclusion. Meditation-based interventions were considered those whose theoretical foundation incorporated philosophies from meditative traditions and provided direct and consistent training in meditation practices as the primary foundation of the intervention (i.e., across at least half of the sessions). Studies that only assessed self-focused compassion were excluded. Unpublished manuscripts, conference presentations, and dissertations were excluded. Non-English studies were excluded due to insufficient funds for translation. We did not exclude studies based on patient demographics such as age or clinical status (i.e., studies of children and adults of any population were included).
Data Extraction and Synthesis
Two independent reviewers (CML and NS) extracted data from each study and discussed results to ensure agreement. Any discrepancies were resolved through discussion with the senior author (GY). The following data were extracted: study sample, intervention type and format, control group type and format, intervention dose and adherence, prosocial outcome variables and time-points, and results for effects on prosocial outcomes. We also extracted any reported data on potential mechanisms of meditation effects (e.g., mediation or correlation analyses examining relationships between changes in pro-social outcomes and other biopsychosocial variables).
Risk of Bias Assessment
Two independent reviewers (CML and NS) assessed risk of bias for each included study according to Cochrane Collaboration guidelines (Higgins & Green, 2008). Risk of bias was assessed as high, low, or unclear for each of eight domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete data, selective reporting, baseline imbalance, and differential attrition (Jüni, Altman, & Egger, 2001; Liberati et al., 2009). In our synthesis, particular attention was paid to low-risk studies, defined as studies with low risk on most (5 out of 8) of the domains assessed. Studies that were not deemed low-risk and showed a high risk of bias on only 1 domain or had an unclear risk of bias on at least half of the domains (4 out of 8) were considered medium risk. Studies with high risk of bias on more than one domain were considered high risk.
Meta-analysis
Using the program Comprehensive Meta-Analysis (Version 3.0; Borenstein, Hedges, Higgins, & Rothstein, 2014), we conducted a meta-analysis on subjective and objective outcomes among studies that provided sufficient data for meta-analysis. One reviewer (CML) extracted data for meta-analysis and a second independent reviewer (RS) verified the results, with no discrepancies noted. Data were extracted for mean and standard deviation (SD) of the pretest and posttest values, mean and SD of change scores and sample size for each group, and t-score or p-value within groups. A pooled effect size was calculated for subjective and objective outcomes separately. Since the outcome variables were measured in different scales, the standardized mean difference (SMD) was used as an estimate of effect size. Subgroup analyses were also conducted to calculate effect sizes for meditation when compared to active controls versus inactive controls. For studies that included two control groups, we conducted two comparisons and divided the total N by 2 to avoid over-estimation of the study. Given that very few studies included follow-up data, we focused the meta-analysis on immediate pre-post effects. We examined heterogeneity of the included studies based on the i-squared statistic and Q test to determine a fixed or random effects meta-analysis model according to the results (i-squared < 40% for fixed effects; Higgins & Green, 2008). Publication bias was also assessed by funnel plot and the fail-safe N. We did not contact authors to obtain missing data in order to prevent bias introduced by selective responding of authors.
Results
Literature Search
See Figure 1 for details of our literature search and article selection process according to PRISMA guidelines (Moher, Liberati, Tezlaff, & Altman, 2009). Our search yielded 479 results. After excluding duplicates (n = 282), unpublished manuscripts (n = 18), non-RCTs (n = 52), non-meditation interventions (n = 18), and studies that did not quantitatively measure pro-social outcomes (n = 43) or only measured self-focused compassion (n = 40), there were 26 studies that met our eligibility criteria.
Figure 1.
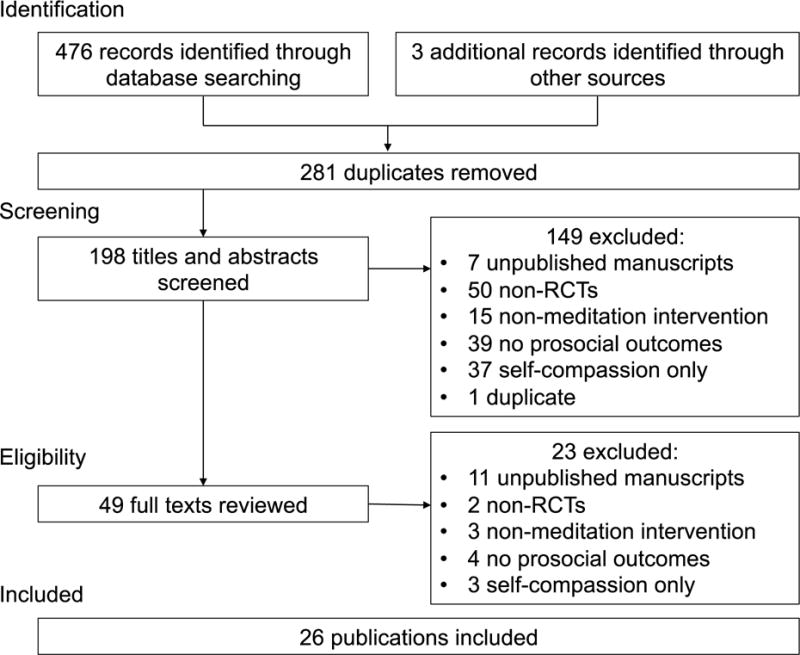
Flowchart of article selection process
Characteristics of Included Studies
Table 1 presents a summary of sample characteristics, meditation interventions, control interventions, and outcome measures across the 26 included studies (total N = 1,714). Most studies (n = 22) were conducted in non-clinical adult populations using a primarily LKM or CM intervention (n = 10) or both mindfulness and LKM combined (n = 8). Studies did not tend to use protocolized interventions but rather incorporated similar elements to develop original protocols. Outcomes included various subjective and objective measures of empathy, compassion, and pro-social behaviors. All studies measured outcomes shortly after the end of the intervention; only 4 studies incorporated a longer-term follow-up (range = 8 – 52 weeks post intervention).
Table 1.
Summary of Characteristics of Included Studies
|
Sample
| |
| Total N (Mean; Range) | 1,714 (66; 29 – 125) |
| Gender, mean percent | 69% |
| Race, mean percent | 68% |
| Adult studies | 22 |
| Age, M (SD), Range | 30.58 (10.33), 19 – 48 years |
| Non-clinical community samples, N | 11 |
| College students, N | 5 |
| Other, N | 6 |
| Child studies | 4 |
| Age, M (SD), Range | 6.28 (3.45), 4 – 10 years |
| Conducted in a school setting, N | 4 |
| Meditation experience, N | |
| None | 14 |
| Experienced meditators | 3 |
| Did not specify | 9 |
|
Meditation Intervention | |
| Meditation type, N | |
| LKM or CM | 10 |
| Combined mindfulness and LKM or CM | 8 (2 of these included yoga) |
| Mindfulness compared to LKM or CM | 2 |
| Primarily mindfulness | 2 |
| Other or did not specify | 4 |
| Intervention format, N | |
| Group format | 17 |
| Individual format (audio recordings) | 5 |
| Both or not specified | 4 |
| Intervention duration, N | |
| 8–12 weeks | 13 |
| 4–6 weeks | 5 |
| Other or not reported | 8 |
| Recommended at-home practice, N | 8 (typically 20 minutes/day) |
|
Control Group | |
| Wait-list or no-intervention, N | 15 |
| Active control groups, N | 5 |
| Both active and inactive, N | 6 |
| Type of active controls, N | |
| Education | 5 |
| Cognitive tasks (e.g., cognitive reappraisal) | 4 |
| Group discussion | 2 |
|
Outcome Measures | |
| Subjective/self-reported, N | 12 |
| Objective/observable, N | 7 |
| Both subjective and objective, N | 7 |
| Validated self-report measures, N | 15 |
| Type of objective measure, N | |
| Non-conscious or automatic responding | 6 |
| Computerized donation tasks | 3 |
| Real-time helping behavior | 3 |
| Peer-rated pro-sociality | 3 |
Note. 26 studies were included. Gender and race are based on n=13 studies because the other 13 did not report these demographics. Type of objective outcomes sum higher than 14 because one study used two types of objective outcomes.
Risk of Bias Assessment
Eleven studies showed a low risk of bias, 12 showed a medium risk, and 3 showed high risk (Tables 1 and 2). Four studies were classified as medium risk because risk was unclear on most domains, rather than because there were any high-risk domains. In general, studies showed lower risk of bias in terms of selective reporting of outcome measures (24 low risk), but higher risk of bias in terms of baseline imbalance (4 high risk), participant blinding, incomplete outcome data, and differential attrition (3 high risk each; see Figure 2).
Table 2.
Risk of Bias for Each Study
| Reference | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting | Baseline imbalance | Differential attrition |
|---|---|---|---|---|---|---|---|---|
| Ashar et al., 2016 | Low | Unclear | Low | Unclear | Low | Low | Unclear | High |
| Asuero et al., 2014 | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Low | Low |
| Condon et al., 2013 | Unclear | Unclear | Low | Low | Unclear | Low | Unclear | Unclear |
| Flook et al., 2015 | Unclear | Unclear | Unclear | High | Unclear | Low | Low | Low |
| He et al., 2015 | Low | Unclear | Unclear | Unclear | High | Low | Low | Unclear |
| Hutcherson et al., 2008 | Unclear | Unclear | Low | Unclear | Unclear | Low | Unclear | Low |
| Jazaierir et al., 2013 | Low | Unclear | High | Unclear | Low | Low | Low | Low |
| Kang et al., 2014 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
| Kang et al., 2015 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
| Keefe 1979 | Low | Unclear | Low | Unclear | Low | Low | Low | Low |
| Kemeny et al., 2012 | Low | Unclear | Low | Low | Low | Low | Low | Low |
| Kok et al., 2013 | Unclear | Unclear | High | Unclear | Low | Low | Low | High |
| Logie et al., 2015 | Unclear | Unclear | Low | Unclear | Low | Low | High | Low |
| Mascaro et al., 2013 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
| Oman et al., 2010 | Unclear | Unclear | High | Unclear | Low | Low | Low | Low |
| Pearl et al., 1994 | Unclear | Unclear | Unclear | Unclear | High | Low | Unclear | Unclear |
| Poehlmann-Tynan et al., 2016 | Unclear | Unclear | Low | Low | High | Low | Low | Unclear |
| Rosenberg et al., 2015 | Unclear | Unclear | High | Low | Low | Low | Low | Low |
| Schonert-Reichl et al., 2015 | Low | Low | Low | Low | Low | Low | High | Low |
| Shapiro et al., 1998 | Unclear | Unclear | Low | Low | Unclear | Low | Low | Unclear |
| Shapiro et al., 2010 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
| Taylor et al., 2015 | Unclear | Unclear | Unclear | Unclear | Unclear | Low | High | Unclear |
| Velasquez et al, 2015 | Unclear | Unclear | Low | Unclear | Unclear | High | Low | High |
| Wallmark et al., 2013 | Low | Unclear | High | Unclear | Low | High | High | Low |
| Weng et al., 2013 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
| Weng et al., 2015 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Low |
Note. Performance bias (blinding of participants and personnel) was considered low if (1) there was an active control group and participants were not likely to know which was the true intervention; (2) there was an inactive control group (e.g., wait-list control) but participants were not aware that the intent of the intervention was to increase prosocial outcomes (e.g., the intervention was framed as stress reduction); or (3) there was an inactive control group and participants were aware of the purpose of the intervention, but outcomes were measured in terms of implicit attitudes or behaviors based on deception. Performance bias was considered high when there was an inactive control group, participants were aware of the intent of the intervention, and outcomes were self-reported. Performance bias was considered unclear when it was unclear whether participants knew the intent of the intervention (e.g., when the authors did not report how the study was advertised or presented to participants).
Figure 2.
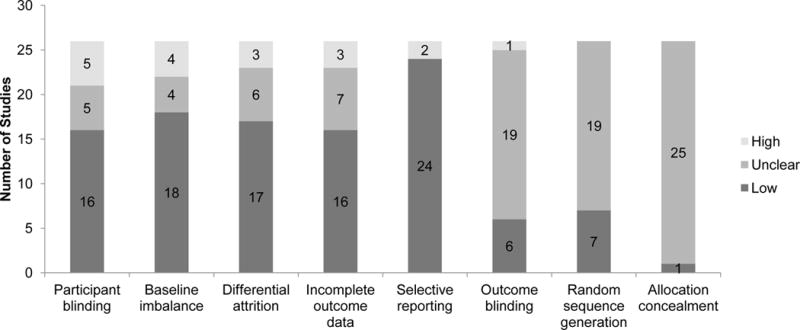
Risk of bias across all studies
Synthesis of Results for Observable Outcomes
Table 3 presents the summary and results of each study. Most studies (11 out of 14; 79%) found support for improvements in observable outcomes following meditation as compared to the control intervention, with no clear difference in results by study quality. There were 7 low-risk studies that measured observable pro-social outcomes and all of them reported improvements following meditation (Kang, Gray, & Dovidio, 2014; Kemeny et al., 2012; Mascaro, Riling, Negi, & Raison, 2013; Rosenberg et al., 2015; Schonert-Reichl et al., 2015; Weng et al., 2013; Weng, Fox, Hessenthaler, Stodola, & Davidson, 2015). The majority of these studies used active control groups (n = 5; Kang et al., 2014; Mascaro et al., 2013; Schonert-Reichl et al., 2015; Weng et al., 2013; Weng et al., 2015). The remaining 7 studies were medium-risk, and 4 of these found support for improvements in observable pro-social outcomes as compared to active (Hutcherson, Seppala, & Gross, 2008; Logie & Frewen, 2015) and wait-list controls (Condon, Desbordes, Miller, & DeSteno, 2013; Flook, Goldberg, Pinger, & Davidson, 2015). Two of the 3 studies that did not find significant effects were conducted in children (Poehlmann-Tynan et al., 2016; Velásquez, López, Quiñonez, & Paba, 2015). Two studies that reported observable improvements were the same studies that did not find support for subjective improvements (Kang et al., 2014; Rosenberg et al., 2015). Both of the studies that directly compared mindfulness and compassion meditation found no significant differences between them for improving pro-social outcomes (Condon et al., 2013; Logie & Ferwen, 2015). In studies with follow-up assessments, one found maintained gains at 5-months post-intervention (Kemeny et al., 2012) and the other found no significant improvements post-intervention or at follow-up (Poehlmann-Tynan et al., 2016).
Table 3.
Summary of Included Studies
| Reference (Bias Risk) | Sample | Meditation Intervention | Control Group | Intervention dose | Intervention Adherence | Outcome Variables | Results |
|---|---|---|---|---|---|---|---|
|
Ashar et al., 2016 (medium) |
N = 58 non-clinical adults; non-meditators; 63% F, 81% W, Mage = 28.59 | CM; individual, audio recording | Oxytocin
placebo Strangers’ photos and brief stories |
20 minutes daily × 4 weeks; no home practice | Sessions completed: 74% | (S) Compassion composite score | + |
| (O) Charitable donations | − | ||||||
|
Asuero et
al., 2014 (medium) |
N = 68 PCPs in Spain; 92% F, Mage = 47.00 | MM; group, in person | Wait-list | 2.5 hours once/week × 8 weeks; one 8-hour retreat; “regular” home practice | Retention: 100% Session attendance:
92% Home practice adherence: 85% |
(S) Jefferson empathy questionnaire | + |
|
Condon et
al., 2013 (medium) |
N = 39 non-clinical adults; non-mediators; 74% F, Mage = 25.23 | MM; group, in person CM; group, in person |
Wait-list | 2 hours once/week × 8 weeks; 20 minutes daily home practice | Session attendance: M = 6.60 sessions Home practice: M = 3.74 practices/week | (O) Giving up a seat for an injured person | + no meditation group differences |
|
Flook et al., 2015 (medium) |
N = 68 children; 50% F, 59% W, Mage = 4.67 | Kindness Curriculum group, in person | Wait-list | 20-30 minutes 2×/week × 12 weeks | Not reported | (O) Teacher-rated social competence | + |
| (O) Sharing task | + | ||||||
|
He et al.,
2015 (medium) |
N = 55 Chinese college students; non-meditators; 84% F, Mage = 18.5 | LKM; group, video | No intervention | 30 minutes 3×/week × 4 weeks | Not reported | (S) Inclusion of Other in Self Scale | + |
|
Hutcherson et al., 2008 (medium) |
N = 93 non-clinical adults; non-meditators; 57% F, 46% W, Mage = 23.6 | LKM; individual, audio recording | Imagining others’ physical appearance | one 7-minute practice | N/A | (S) explicit attitudes toward others | + |
| (O) Implicit attitudes task | + | ||||||
|
Jazaieri et
al., 2013 (low) |
N = 100 non-clinical adults; 72% F, 71% W, Mage = 43.33 | CM; group, in person | Wait-list | 2 hours once/week × 8 weeks; 15 minutes daily home practice | Session attendance: 98% ≥7 sessions Retention: 85% Home practice: M = 101.11 minutes/week | (S) Fear of compassion scale | + |
|
Kang et al., 2014 (low) |
N = 101 non-clinical adults; non-meditators; 64% F, 61% W, Mage = 25.20 | LKM; group, in person | Discussion about loving
kindness Wait-list |
1 hour once/week × 6 weeks; 20 minutes home practice × 5days/week | Session attendance: M = 4.86 sessions Home practice: M = 553.84 minutes | (S) explicit bias | − |
| (O) Implicit attitudes task | + | ||||||
|
Kang et al.,
2015 (low) |
N = 54 non-clinical adults; non-meditators; 67% F, 59% W, Mage = 24.94 | LKM; group, in person | Discussion about loving
kindness Wait-list |
1 hour once/week × 6 weeks; 20 minutes home practice 5 days/week | Session attendance: M = 4.30 sessions | (S) Self-Other Four Immeasurables scale | + |
|
Keefe,
1979 (low) |
N = 56 social work students | Meditation, not specified | Empathy education No intervention |
30 minutes daily × 3 weeks | Not reported | (S) Kagan affective sensitivity scale | − |
|
Kemeny et
al., 2012 (low) |
N = 76 female school teachers; non-meditators; Mage = 41.05 | MM, LKM, yoga; group, in person | Wait-list | 42 hours over 8 weeks; 25 minutes daily home practice | Session attendance: M = 6.67 sessions | (O) Emotional recognition task; implicit compassion task; marital interaction task; 5 month f/u | + follow-up: + |
|
Kok et al.,
2013 (high) |
N = 65 university faculty; non-meditators; 66% F, 83% W, Mage = 37.5 | LKM; group, in person | Wait-list | 1 hour once/week × 6 weeks; daily home practice | Not reported | (S) daily social connectedness; 1-week post intervention | + |
|
Logie et al., 2015 (medium) |
N = 105 undergraduate students; mostly non-meditators; 67% F, 63% W, Mage = 18.63 | LKM; individual, audio recording MM, individual, audio recording | Read about mindfulness | one 15-minute practice | NA | (S) Self-Other Four Immeasurables scale | + no meditation group differences |
| (O) Self/other referential processing task | + no meditation group differences |
||||||
|
Mascaro et
al., 2013 (low) |
N = 29 non-clinical adults; 45% F, Mage = 31.0 | CM | Health education | 2 hours once/week × 8 weeks; 20 minutes daily home practice | Session attendance: M attendance = 7.38 sessions Home practice: M = 315.9 minutes | (O) Empathic accuracy task | + |
|
Oman et al.,
2010 (medium) |
N = 58 healthcare providers; 40% meditators; 86% F | Passage meditation; group, in person | Wait-list | 2 hours once/week × 8 weeks | Not reported | (S) IRI; MMRS; compassionate love scale; altruism scale; post, and 8- and 19-week f/u | + follow-up: + |
|
Pearl et
al., 1994 (medium) |
N = 50 non-clinical adults; non-meditators; Mage = 23.9 | Meditation, not specified | No intervention | Approximately eight weeks | Not reported | (S) Affective sensitivity scale | − |
|
Poehlmann-Tynan et al., 2016 (medium) |
N = 29 children; 49% girls, Mage = 3.92 | Kindness Curriculum; group, in person | Reading group | 20–30 minutes 2×/week × 12 weeks | Session attendance: M = 21 sessions | (O) Response to someone getting ‘hurt’; compassionate stories; 3-month f/u | − follow-up: − |
|
Rosenberg et al., 2015 (low) |
N = 60 experienced meditators; 54% F, Mage = 48 | MM and CM retreat; group and individual | Wait-list | 3-month retreat | Retention: 100% Total practice: M = 41 hours | (S) Emotions composite | − |
| (O) facial coding during film clips of suffering | + | ||||||
|
Schonert-Reichl et al., 2015 (low) |
N = 100 children; 46% F, 66% English first language, Mage = 10.24 | MM and prosocial; group, in person | Social responsibility education | 40–50 minutes once/week × 12 weeks | 100% of lessons administered | (S) IRI; Social Goals questionnaire | + |
| (O) Peer-reported prosociality | + | ||||||
|
Shapiro et
al., 1998 (medium) |
N = 78 medical students; 64% F, 79% W | MM, LKM; group, in person | Wait-list | 2.5 hours once/week × 7 weeks; weekly home practice | Retention: 97% | (S) Empathy rating scale | + |
|
Shapiro et
al., 2010 (low) |
N = 30 undergraduate students; 87% F, 83% W, Mage = 18.73 | MBSR; group, in person | Wait-list | 90 minutes once/week × 8 weeks | Retention: 100% | (S) IRI, Heartland forgiveness scale; 2- and 12-month f/u | + follow-up: + |
|
Taylor et
al., 2015 (medium) |
N = 59 teachers; 90% F, 67% W, Mage = 47.00 | MM and compassion; group, in person | Wait-list | 11 sessions over 9 weeks (36 hours total); daily practice | Session attendance: Mode = 9 sessions Home practice: M = 12.8 hours | (S) Santa Clara compassion scale; Tendency to Forgive scale; specific person forgiveness | + |
|
Velasquez et al, 2015 (high) |
N = 125 children in Colombia | Yoga; group, in person | Wait-list | 2 hours twice/week × 12 weeks | Session attendance: M = 17 sessions | (S) Empathy questionnaire | − |
| (O) Peer prosociality | − | ||||||
|
Wallmark et
al., 2013 (high) |
N = 46 non-clinical adults; non-meditators; 86% F, Mage = 33.8 | MM and FI; group, in person | Wait-list | 75 minutes once/week × 8 weeks; 30 minutes daily home practice | Not reported | (S) IRI | + |
|
Weng et al.,
2013 (low) |
N= 56 non-clinical adults; non-meditators; 61% F, Mage = 22.5 | CM; individual, audio recording | Cognitive reappraisal No intervention |
30 minutes daily × 2 weeks | Home practice: M = 11.8 days of practice, M = 351.7 minutes total | (O) Redistribution of money game | + |
|
Weng et al.,
2015 (low) |
N= 56 non-clinical adults; non-meditators; 61% F, Mage = 22.5 | CM; individual, audio recording | Cognitive reappraisal No intervention |
30 minute daily × 2 weeks | Home practice: M = 11.8 days of practice, M = 351.7 minutes total | (O) Redistribution of money game | + |
Note. Results are in reference to the significance of the group * time interaction, such that positive findings (+) indicate significantly greater improvements in the meditation group compared to the control group, and negative findings (−) indicate no greater benefits of meditation compared to the control group. F = female, W = white. CM = compassion meditation, MM = mindfulness meditation, LKM = loving kindness meditation. S = subjective (self-reported) outcomes, O = objective (observable) outcomes. All outcomes were assessed immediately post-intervention and outcomes that were also measured at longer-term follow-ups are noted. IRI = Interpersonal Reactivity Index (Davis, 1994); MMRS = Multidimensional Measure of Religion and Spirituality (Fetzer, 1999).
A total of 11 studies provided sufficient data on observable outcomes for meta-analysis with 12 comparisons available (see Figure 3). There was sufficient homogeneity among studies to conduct a fixed effects analysis (i-squared = .00; Q-value = 1.82, p = .96). The effect size across these studies was .45 (p < .001; 95% CI = .28 – .61). Results were similar for studies with active (SMD = .48, p < .001; 95% CI = .25 – .72) and inactive control groups (SMD = .41, p < .001; 95% CI = .19 – .63). Publication bias was not suspected based on the funnel plot (see Figure 4) and the number of negative studies needed to make the results non-significant (N = 76, p = .92).
Figure 3. Effects of meditation on objective and subjective outcomes.
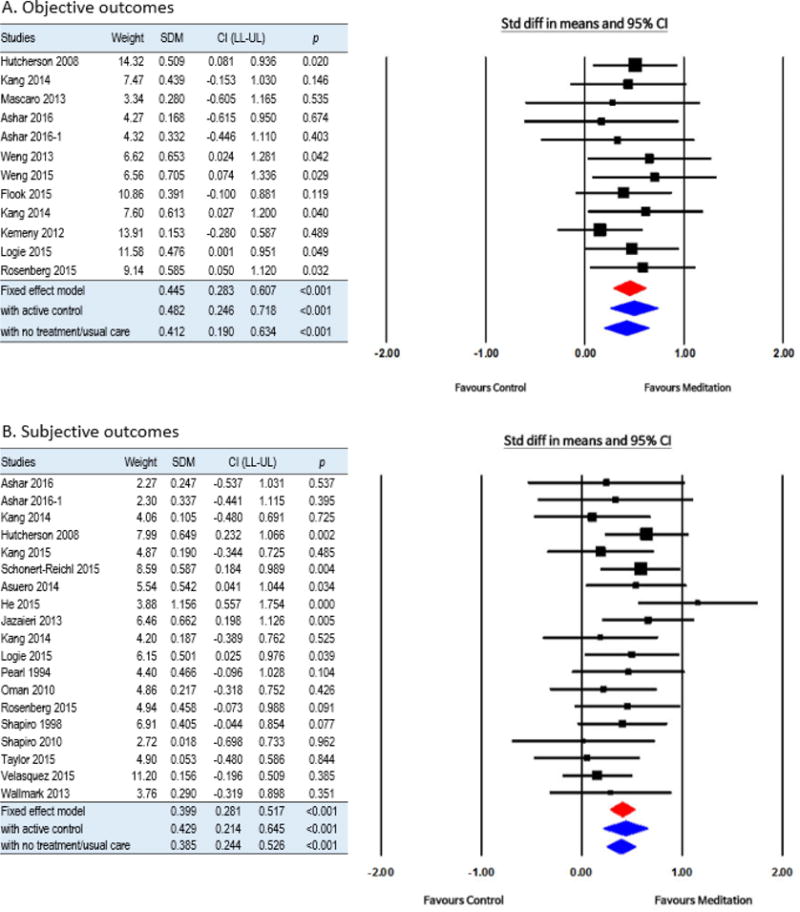
Note. SDM, standardized difference in means; CI, confidence interval; LL, lower limit; UL, upper limit.
Figure 4.
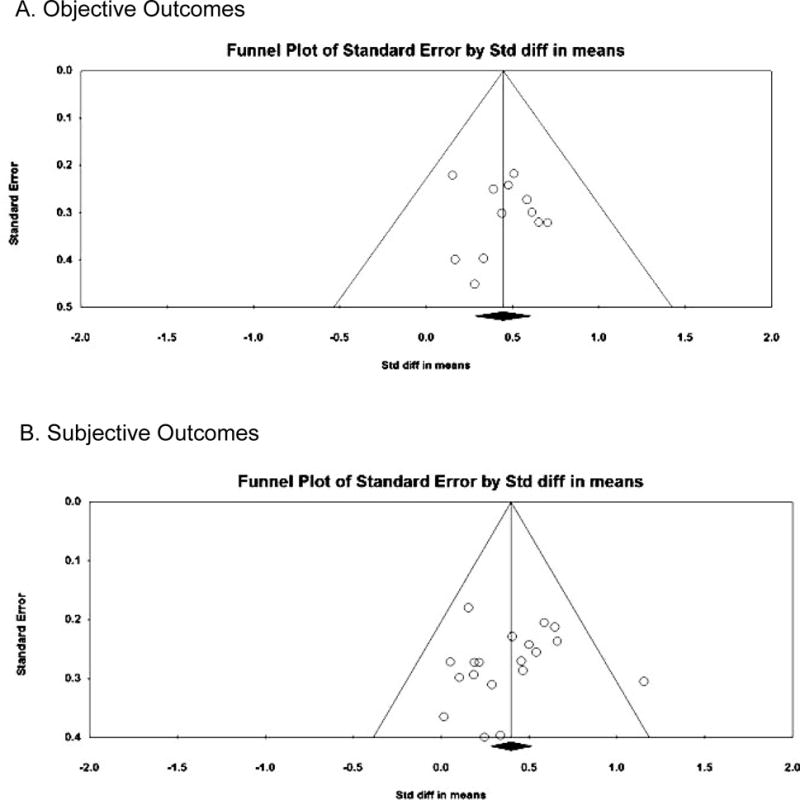
Funnel plots for objective and subjective outcomes
Synthesis of Results for Self-reported Outcomes
The majority of studies (14 out of 19; 74%) found significant improvements in self-reported outcomes following meditation compared to the control intervention for at least one pro-social outcome (e.g., empathy, compassion, or pro-social behavior). These results did not appear to appreciably vary depending on the study’s level of risk of bias. There were 7 low-risk studies and 4 found support for improvements in self-reported empathy or compassion as compared to wait-list (Jazaieri et al., 2013; Shapiro, Brown, Thoresen, & Plante, 2010) and active control groups (Kang, Gray, & Dovidio, 2015; Schonert-Reichl et al., 2015). Three low-risk studies did not find support for subjective improvements (Kang et al., 2014; Keefe, 1979; Rosenberg et al., 2015). There were 9 medium-risk studies and 8 found support for subjective improvements (Ashar et al., 2016; Asuero et al., 2014; He et al., 2015; Hutcherson et al., 2008; Logie & Ferwen, 2015; Oman, Thoresen, & Hedberg, 2010; Shapiro, Schwartz, & Bonner, 1998; Taylor et al., 2015). Three studies were classified as high-risk and two of these found improvements (Kok et al., 2013; Wallmark, Safarzadeh, Daukantaite, & Maddux, 2013). Both studies that included a long-term follow-up found that improvements were maintained over time (Oman et al., 2010; Shapiro et al., 2010).
A total of 18 studies provided sufficient data on self-reported outcomes for meta-analysis. These studies allowed for 19 comparisons because one study used two control groups. Results indicated sufficient homogeneity to conduct a fixed effects meta-analysis (i-squared = .00; Q-value = 3.94, p = .49). The effect size for subjective outcomes across these studies was .40 (95% CI = .28 – .52, p < .001). The results were similar across studies that used active (SMD = .43, p < .001; 95% CI = .21 – .65) and inactive control groups (SMD = .39, p < .001; 95% CI = .24 – .53). Publication bias was not suspected based on the funnel plot and because the number of studies needed to make the results non-significant was 165 (p = .55).
Synthesis of Results for Potential Mechanisms
Fourteen studies reported results for potential mediators of effects of meditation on pro-social outcomes. Six of these studies conducted formal mediation analyses (Ashar et al., 2016; Hutcherson et al., 2008; Kang et al., 2014; Oman et al., 2010; Kok et al., 2013; Shapiro et al., 1998). Formal mediation results revealed that increased social and emotional connectedness mediated the effects of compassion meditation and charitable donations (Ashar et al., 2016); increased positive affect mediated the effect of LKM on explicit bias toward marginalized groups (Hutcherson et al., 2008); decreased stress mediated the effect of LKM on bias (Kang et al., 2014); and greater home practice and decreased stress mediated the effect of meditation on compassion (Oman et al., 2010). Kok et al. (2013) tested more complex structural models and found that loving kindness meditation led to improvements in positive emotions, which led to improvements in social connectedness, which led to improvements in vagal tone. Shapiro et al. (1998) found that greater meditation compliance led to decreased anxiety, which led to greater empathy.
Eight studies did not conduct formal mediation analyses but explored correlations between changes in pro-social outcomes and changes in other variables that suggest potential mechanisms of action (Jazaieri et al., 2013; Keefe, 1979; Kemeny et al., 2012; Mascaro et al., 2013; Rosenberg et al., 2015; Velásquez et al., 2015; Wallmark et al., 2013; Weng et al., 2013). Almost all (7 out of 8) examined the relationship between amount of home practice/meditation adherence and pro-social outcomes: 5 found that greater meditation practice was correlated with greater pro-social outcomes (Jazaieri et al., 2013; Keefe, 1979; Rosenberg et al., 2015; Velásquez et al., 2015; Wallmark et al., 2013) and 2 found no significant correlation (Kemeny et la., 2012; Mascaro et al., 2013). One study also found that increases in mindfulness and self-compassion, and decreases in stress, were significantly correlated with increases in empathy (Wallmark et al., 2013). Two studies used fMRI to explore correlations between pro-social outcomes and changes in neural function (Mascaro et al., 2013; Weng et al., 2013). Mascaro et al. (2013) found that improvements in empathy were correlated with increased activity in the inferior frontal gyrus (IFG) and dorsomedial prefrontal cortex (dmPFC). Weng et al. (2015) found that greater pro-social behavior (charitable donations) were correlated with changes in the inferior parietal cortex and dorsolateral prefrontal cortex.
Discussion
The results of the current systematic review support the efficacy of meditation-based interventions for increasing empathy, compassion, and pro-social behaviors. Meditation interventions showed significantly greater improvements in at least one pro-social outcome as compared to control groups in 22 out of the 26 included RCTs (85%). Meta-analysis results indicated that meditation training had a small-medium and significant effect on both subjective and objective pro-social outcomes, which was similar across studies with active and inactive control groups if not slightly higher among those with active controls. Many studies were low-risk, with only 3 studies showing a high risk of bias and there were no clear differences in outcomes based on risk of bias. Effects for observable outcomes (e.g., real-world helping behavior, facial expressions) were somewhat stronger and more consistent than results for self-reported outcomes, though both showed significant improvements in the meta-analysis.
Results of several studies suggest potential mechanisms by which meditation can improve pro-social outcomes. Potential emotional mechanisms include an increased sense of social-emotional connectedness with others (Ashar et al., 2016; Kok et al., 2013), increased positive affect (Hutcherson et al., 2008; Kok et al., 2013), decreased stress and negative affect (Kang et al., 2014; Oman et al., 2010; Shapiro et al., 1998), and greater trait mindfulness and self-compassion (Wallmark et al., 2013). Some studies directly tested self-focused emotional mechanisms as mediators of meditation training on pro-social outcomes and found significant indirect effects, suggesting that meditation leads to improvements in individuals own socio-emotional functioning and, thereby, improvements in pro-social outcomes (Ashar et al., 2016; Hutcherson et al., 2008; Kang et al., 2014; Kok et al., 2013; Shapiro et al., 1998). Consistent with the larger literature demonstrating that meditation interventions improve self-focused emotions (Hofmann et al. al., 2010; Kirby et al., 2016), these results suggest that one way meditation practice can lead to improvements in pro-social emotions is by improving individuals’ own socio-emotional well-being. These mechanisms are also consistent with research demonstrating that mindfulness-based interventions increase trait mindfulness (Quaglia, Braun, Freeman, McDaniel, & Brown, 2016), as trait mindfulness is likely to promote real-time awareness of others’ suffering and thus greater opportunities for pro-social action (Bibeau et al., 2016). Amount of meditation practice may play a role in a dose-response relationship, with reports of greater practice associated with greater improvements (Jazaieri et al., 2013; Keefe, 1979; Oman et al., 2010; Rosenberg et al., 2015; Shapiro et al., 1998; Velásquez et al., 2015; Wallmark et al., 2013). However, it is possible that some studies did not find a relationship between home practice and outcomes and did not report these non-significant findings.
This synthesis has also identified potential physiological and neural mechanisms underlying these effects. Many meditation practices elicit physiological processes associated with the relaxation response (i.e., parasympathetic dominance), which is the physiological counter to the stress response (i.e., sympathetic dominance; Benson, 1997). Regular elicitation of the relaxation response is associated with reduced stress and negative emotions (Esch et al., 2003) and is thought to play a role in improving pro-social emotions (Kirby, 2016). In the current review, meditation was indeed associated with improvements in vagal tone (Kok et al., 2013). Meditation was also associated with altered activation in areas of the prefrontal cortex (Mascaro, Darcher, Negi, & Raison, 2015; Weng et al., 2013). These findings are similar to previous studies of meditation for general health outcomes (Pace et al., 2009; Marchand, 2014) and non-RCTs of meditation for pro-social outcomes (Klimecki, Leiberg, Lamm, & Singer, 2012; Klimecki, Leiberg, Ricard, & Singer, 2014; Leiberg, Klimecki, & Singer, 2011) and further support a neural and physiological basis for meditation’s effects on pro-social outcomes specifically.
Although not emphasized in most of the studies included in the current review, meditation-relaxation physiology may be associated with improved pro-social outcomes through oxytocin-mediated improvements in attachment style. The same physiological processes that characterize the relaxation response have been shown to occur in the context of secure attachment and mother-child dyads, which provide a foundation for compassion (Fricchione, 2011; Hill-Soderlund et al, 2008; Mikulincer, Shaver, Gillath, & Nitzberg, 2005; Oosterman, De Schipper, Fisher, Dozier, & Schuengel, 2010). Oxytocin plays a role in both relaxation and secure attachment physiology and is also associated with greater pro-social behaviors (e.g., improved face expression recognition, enhanced encoding of positive social memories; Isgett, Algoe, Boulton, Way, & Fredrickson, 2016; Mascaro et al, 2015; Strathearn, Fonagy, Amico, & Montague, 2009). If meditation stimulates oxytocin receptors and mimics the physiology of secure attachment, then it is reasonable and researchable to hypothesize that meditative approaches will enhance pro-social behaviors (Kim, Fonagy, Koos, Forsett, & Strathearn, 2014; Rilling, 2009; Strathearn et al, 2009). Only one study included in the current review directly addressed the potential role of oxytocin, by using a placebo oxytocin control group; results indicated greater improvement in subjective but not objective pro-social outcomes among CM participants than oxytocin placebo participants. Recent theories highlight that the role of oxytocin in social behavior is complex and not necessarily pro-social, depending on individual difference characteristics (e.g., gender, psychopathology; Shamay-Tsoory & Abu-Akel, 2016). Future research should explore whether oxytocin is another physiological mechanism by which meditation leads to enhanced pro-social benefits.
Another potential mechanism of action that was not emphasized in the current systematic review and has not been explored in any of the studies included here involves emotional tolerance and regulation. Beyond reductions in level of emotional problems, improvements in the way individuals withstand or respond to negative affect might also play a role (Mascaro et al., 2015). Theoretical conceptualizations of compassion emphasize that individuals must be able to tolerate the distress they feel in response to another’s suffering in order to effectively enact helping behaviors (Strauss et al., 2016). Distress tolerance, an individual difference variable defined as the ability to withstand negative affective states (Simons & Gaher, 2005), is a well-established risk factor for emotional disorders that influences emotion regulation strategies (i.e., low levels of distress tolerance motivate maladaptive avoidance). Meditation interventions, particularly mindfulness meditation, have been shown to significantly increase distress tolerance and improve emotion regulation (Lotan, Tanay, & Bernstein, 2013; Chambers, Gullone, & Allen, 2009), and emotion regulation is thought to play a role in the effects of LKM on pro-social outcomes (Mascaro et al., 2015). Thus, meditation might also improve compassion and other pro-social outcomes by improving the way individuals tolerate and respond to distress, in addition to decreasing the amount of distress an individual experiences. Future research should directly test these potential mechanisms.
The current findings are supported by the relatively strong design and low risk of bias across many RCTs, the homogeneity of studies included in the meta-analysis, and evidence for lack of publication bias. Many studies used active control groups and objective behavioral outcomes, and meta-analysis results were similar across type of control group and outcome measure. However, samples were all non-clinical and primarily female and White, and half did not report the racial composition of the sample. Greater sample diversity is needed and future studies should describe the full demographic characteristics of the sample. Describing the details of the randomization procedure and concealment and maintaining participant blinding (e.g., concealing the true intent of the study, using active matched control groups) could also further improve the methodological rigor of future studies.
Nonetheless, this review highlights several directions for future research. First, research on more clinically and demographically diverse samples is needed to enhance generalizability. Second, although the meta-analysis indicated homogeneity among studies, there was variability among the meditation interventions. Future studies may consider using manualized protocols or conduct dismantling studies to establish optimal intervention dose and content. In addition, research should examine a wider range of meditation types and formats, such as movement-based meditations and individual (rather than group) in-person interventions. This research should also include comparative efficacy trials that directly compare different types of meditation and other evidence-based interventions that improve emotional problems (i.e., traditional cognitive-behavioral therapy). In the current review, most studies incorporated LKM, which is a relatively newer research area as compared to mindfulness meditation, and found significant pro-social benefits. Moreover, both of the studies that compared LKM to mindfulness did not find significant differences in pro-sociality, though Logie & Frewen (2015) found a greater effect of LKM on reducing self-positivity bias as compared to mindfulness meditation, and other previous studies have found some differences in emotional outcomes across meditation types (Zeng et al., 2015). Future studies should also incorporate longer-term follow-ups. These findings provide further support for continued research on LKM and the need for comparative efficacy work.
It is also worth noting that some research suggests empathy and compassion may have different utility for the person giving versus receiving help, particularly when empathizing with another’s suffering. Empathy (affect-sharing) may increase personal distress and reduce pro-social behavior, while compassion (affect-sharing with motivation to help) may strengthen personal resources and promote positive outcomes (e.g., Klimecki et al., 2014; Singer & Klimecki, 2014). It is possible that these differential effects could vary depending on the individual’s own general ability to tolerate emotional distress. We included empathy to be comprehensive in our review of pro-social outcomes but further research on the differential effects of empathy and compassion is warranted.
The current findings also have implications for clinical practice and meditation teachers in non-clinical settings. Clinicians and meditation teachers should be aware that meditation interventions (e.g., MBSR, MBCT) could provide additional benefits beyond reduced emotional distress. Clinicians might select meditation-based protocols for patients who are specifically interested in increasing empathy and compassion (e.g., parents, healthcare providers), or consider incorporating meditation training into other evidence-based interventions to maximize improvements for individuals experiencing interpersonal problems. Results suggest that integrating meditation training into other evidence-based interventions may be feasible, as even two weeks of 20 minutes daily practice via mobile phone applications have shown significant pro-social benefits. Meditation teachers in non-clinical settings should be aware that there is a scientific evidence base to support the broader pro-social benefits of individual meditation training, teach meditation with these benefits in mind, and consider discussing these potential benefits with students.
Limitations
In the current systematic review, limitations include heterogeneity in the interventions and an inability to non-English studies, which may have biased the results and limits generalizability. Nonetheless, these results advance the scientific understanding of meditation for health outcomes and suggest that meditation training is a promising way to increase individual-level pro-social outcomes. Improving these pro-social outcomes has the potential to promote important societal changes needed today. Further research using more diverse samples and meditation practices is warranted.
Acknowledgments
Funding: This study was supported by funding from the National Center for Complementary and Integrative Health (NCCIH 2T32AT000051-6; Luberto) and National Cancer Institute (NCI 1K24CA197382; Park)
Appendix A: Ovid MEDLINE Search Strategy
| Query # | Search Strategy |
|---|---|
| 1 | Mind-Body Therapies/ or Mindfulness/ or meditation/ or tai ji/ or yoga/ |
| 2 | (“mind body” or MBSR or MBCT or mindfulness or meditat* or yoga or “tai chi” or “tai ji” or taiji).ti,ab. |
| 3 | 1 or 2 |
| 4 | Empathy/ or love/ or altruism/ |
| 5 | (empath* or compassion* or sympathy or love or kindness or altruis*).ti,ab. |
| 6 | 4 or 5 |
| 7 | 3 and 6 |
| 8 | limit 7 to english language |
| 9 | random*.tw,hw |
| 10 | 8 and 9 |
Footnotes
Conflict of Interest: The authors have declared that they have no conflict of interest.
Author Contributions
CML: conducted the systematic review, wrote the paper
NS: served as the second reviewer for data extraction
RS: conducted the meta-analysis, edited the paper
LLP: conducted the literature search, edited the paper
ERP: contributed to writing and editing the paper
GLF: contributed to writing and editing the paper
GYY: assisted with data extraction and meta-analysis, contributed to writing and editing the paper
References
- Ashar YK, Andrews-Hanna JR, Yarkoni T, Sills J, Halifax J, Dimidjian S, Wager TD. Effects of compassion meditation on a psychological model of charitable donation. Emotion. 2016;16(5):691–705. doi: 10.1037/emo0000119. [DOI] [PubMed] [Google Scholar]
- Asuero AM, Queraltó JM, Pujol-Ribera E, Berenguera A, Rodriguez-Blanco T, Epstein RM. Effectiveness of a mindfulness education program in primary health care professionals: A pragmatic controlled trial. Journal of Continuing Education in the Health Professions. 2014;34(1):4–12. doi: 10.1002/chp.21211. [DOI] [PubMed] [Google Scholar]
- Benson H. The relaxation response: therapeutic effect. Science. 1997;278(5344):1693–1697. doi: 10.1126/science.278.5344.1693b. Retrieved from http://www.jstor.org/stable2894939. [DOI] [PubMed] [Google Scholar]
- Bibeau M, Dionne F, Leblanc J. Can compassion meditation contribute to the development of psychotherapists’ empathy? A review. Mindfulness. 2016;7(1):255–263. doi: 10.1007/s12671-015-0439-y. [DOI] [Google Scholar]
- Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. Journal of Psychosomatic Research. 2010;68(6):539–544. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis Version 3.0 [Computer software] Englewood, NJ: Biostat; 2014. [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Condon P, Desbordes G, Miller WB, DeSteno D. Meditation increases compassionate responses to suffering. Psychological Science. 2013;24(10):2125–2127. doi: 10.1177/095679761348603. [DOI] [PubMed] [Google Scholar]
- Dunn EW, Aknin LB, Norton MI. Spending money on others promotes happiness. Science. 2008;319(5870):1687–1688. doi: 10.1126/science.1150952. [DOI] [PubMed] [Google Scholar]
- Eberth J, Sedlmeier P. The effects of mindfulness meditation: A meta-analysis. Mindfulness. 2012;3(3):174–189. doi: 10.1007/s12671-012-0101-x. [DOI] [Google Scholar]
- Esch T, Fricchione GL, Stefano GB. The therapeutic use of the relaxation response in stress-related diseases. Medical Science Monitor. 2003;9(2):RA23–RA34. [PubMed] [Google Scholar]
- Faulkner LR, McCurdy RL. Teaching medical students social responsibility: The right thing to do. Academic Medicine. 2000;75(4):346–350. doi: 10.1097/00001888-200004000-00010. [DOI] [PubMed] [Google Scholar]
- Flook L, Goldberg SB, Pinger L, Davidson RJ. Promoting prosocial behavior and self-regulatory skills in preschool children through a mindfulness-based Kindness Curriculum. Developmental Psychology. 2015;51(1):44. doi: 10.1037/a0038356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fricchione GL. Compassion and healing in medicine and society: On the nature and use of attachment solutions to separation challenges. Baltimore, MD: Johns Hopkins University Press; 2011. [Google Scholar]
- Galante J, Galante I, Bekkers MJ, Gallacher J. Effect of kindness-based meditation on health and well-being: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2014;82(6):1101–1114. doi: 10.1037/a0037249. [DOI] [PubMed] [Google Scholar]
- Gilbert P. An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy. 2010;3(2):97–112. doi: 10.1521/ijct.2010.3.2.97. [DOI] [Google Scholar]
- Goetz JL, Keltner D, Simon-Thomas E. Compassion: An evolutionary analysis and empirical review. Psychological Bulletin. 2010;136(3):351–374. doi: 10.1037/a0018807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein J, Kornfield J. Seeking the heart of wisdom: The path of insight meditation. Boston: Shambala; 2001. [Google Scholar]
- Gotink RA, Chu P, Busschbach JJ, Benson H, Fricchione GL, Hunink MG. Standardised mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLOS One. 2015;10(4):e0124344. doi: 10.1371/journal.pone.0124344. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- He X, Shi W, Han X, Wang N, Zhang N, Wang X. The interventional effects of loving-kindness meditation on positive emotions and interpersonal interactions. Neuropsychiatric Disease and Treatment. 2015;11:1273–1277. doi: 10.2147/NDY.S79607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions (Version 5.0.0) Chichester, England: Wiley-Blackwell; 2008. [Google Scholar]
- Hill-Soderlund AL, Mills-Koonce WR, Propper C, Calkins SD, Granger DA, Moore GA, Cox MJ. Parasympathetic and sympathetic responses to the strange situation in infants and mothers from avoidant and securely attached dyads. Developmental Psychobiology. 2008;50(4):361–376. doi: 10.1002/dev.20302. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan R. Development of an empathy scale. Journal of Consulting and Clinical Psychology. 1969;33(3):307–316. doi: 10.1037/h0027580. [DOI] [PubMed] [Google Scholar]
- Hoge EA, Chen MM, Orr E, Metcalf CA, Fischer LE, Pollack MH, Simon NM. Loving-Kindness Meditation practice associated with longer telomeres in women. Brain, Behavior, and Immunity. 2013;32:159–163. doi: 10.1016/j.bbi.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Hurst CE, Gibbon HMF, Nurse AM. Social inequality: Forms, causes, and consequences. New York: Routledge; 2016. [Google Scholar]
- Hutcherson CA, Seppala EM, Gross JJ. Loving-kindness meditation increases social connectedness. Emotion. 2008;8(5):720–724. doi: 10.1037/a0013237. [DOI] [PubMed] [Google Scholar]
- Ironson G. Altruism and health in HIV. In: Post SG, editor. Altruism and health: Perspectives from empirical research. New York: Oxford University Press; 2007. pp. 70–81. [Google Scholar]
- Isgett SF, Algoe SB, Boulton AJ, Way BM, Fredrickson BL. Common variant in OXTR predicts growth in positive emotions from loving-kindness training. Psychoneuroendocrinology. 2016;73:244–251. doi: 10.1016/j.psyneun.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jazaieri H, Jinpa GT, McGonigal K, Rosenberg EL, Finkelstein J, Simon-Thomas E, Goldin PR. Enhancing compassion: A randomized controlled trial of a compassion cultivation training program. Journal of Happiness Studies. 2013;14(4):1113–1126. doi: 10.1007/s10902-012-9373-z. [DOI] [Google Scholar]
- Jüni P, Altman DG, Egger M. Assessing the quality of randomised controlled trials. British Medical Journal. 2001;323(7303):42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-834(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kang Y, Gray JR, Dovidio JF. The nondiscriminating heart: Loving kindness meditation training decreases implicit intergroup bias. Journal of Experimental Psychology: General. 2014;143(3):1306–13013. doi: 10.1037/a0034150. [DOI] [PubMed] [Google Scholar]
- Kang Y, Gray JR, Dovidio JF. The head and the heart: Effects of understanding and experiencing loving kindness on attitudes toward the self and others. Mindfulness. 2015;6(5):1063–1070. doi: 10.1007/s12671-014-0355-6. [DOI] [Google Scholar]
- Keefe T. The development of empathic skill: A study. Journal of Education For Social Work. 1979;15(2):30–37. Retrieved from http://www.jstor.org/stable/23038875. [Google Scholar]
- Kemeny ME, Foltz C, Cavanagh JF, Cullen M, Giese-Davis J, Jennings P, Ekman P. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion. 2012;12(2):338–350. doi: 10.1037/a0026118. [DOI] [PubMed] [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Hofmann SG. Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review. 2013;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Kim S, Fonagy P, Koos O, Dorsett K, Strathearn L. Maternal oxytocin response predicts mother-to-infant gaze. Brain Research. 2014;1580:133–142. doi: 10.1016/j.brainres.2013.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby JN. Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychology and Psychotherapy: Theory, Research and Practice. 2016;90(3):432–455. doi: 10.1111/papt.12104. [DOI] [PubMed] [Google Scholar]
- Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: A systematic review of the research evidence. British Journal of Sports Medicine. 2005;39(12):884–891. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimecki OM, Leiberg S, Lamm C, Singer T. Functional neural plasticity and associated changes in positive affect after compassion training. Cerebral Cortex (New York, NY:1991) 2012;23(7):1552–1561. doi: 10.1093/cercor/bhs142. [DOI] [PubMed] [Google Scholar]
- Klimecki OM, Leiberg S, Ricard M, Singer T. Differential pattern of functional brain plasticity after compassion and empathy training. Social Cognitive and Affective Neuroscience. 2014;9(6):873–879. doi: 10.1093/scan/nst060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, Fredrickson BL. How positive emotions build physical health: Perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychological Science. 2013;24(7):1123–1132. doi: 10.1177/0956797612470827. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Emotion and adaptation. Oxford: Oxford University Press; 1991. [Google Scholar]
- Leiberg S, Klimecki O, Singer T. Short-term compassion training increases prosocial behavior in a newly developed prosocial game. PloS One. 2011;6(3):e17798. doi: 10.1371/journal.prone.0017798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Annals of Internal Medicine. 2009;151(4):W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- Lim D, DeSteno D. Suffering and compassion: The links among adverse life experiences, empathy, compassion, and prosocial behavior. Emotion. 2016;16(2):175–182. doi: 10.1037/emo0000144. [DOI] [PubMed] [Google Scholar]
- Logie K, Frewen P. Self/other referential processing following mindfulness and loving-kindness meditation. Mindfulness. 2015;6(4):778–787. doi: 10.1007/s12671-014-0317-z. [DOI] [Google Scholar]
- Lotan G, Tanay G, Bernstein A. Mindfulness and distress tolerance: Relations in a mindfulness preventive intervention. International Journal of Cognitive Therapy. 2013;6(4):371–385. doi: 10.1521/ijct.2013.6.4.371. [DOI] [Google Scholar]
- Luberto CM, White C, Sears RW, Cotton S. Integrative medicine for treating depression: An update on the latest evidence. Current Psychiatry Reports. 2013;15(9):1–9. doi: 10.1007/s11920-013-2. [DOI] [PubMed] [Google Scholar]
- Marchand WR. Neural mechanisms of mindfulness and meditation: Evidence from neuroimaging studies. World Journal of Radiology. 2014;6(7):471–479. doi: 10.4329/wjr.v6.i7.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascaro JS, Rilling JK, Negi LT, Raison CL. Compassion meditation enhances empathic accuracy and related neural activity. Social and Cognitive Affective Neuroscience. 2013;8(1):48–55. doi: 10.1093/scan/nss095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascaro JS, Darcher A, Negi LT, Raison CL. The neural mediators of kindness-based meditation: a theoretical model. Frontiers in Psychology. 2015;6:109. doi: 10.3389/fpsyg.2015.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR, Gillath O, Nitzberg RA. Attachment, caregiving, and altruism: Boosting attachment security increases compassion and helping. Journal of Personality and Social Psychology. 2005;89(5):817–839. doi: 10.1037/0022-3514.89.5.817. doi: [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.1037/0022-3514.89.5.817. [DOI] [PubMed] [Google Scholar]
- Nelson SK, Layous K, Cole SW, Lyubomirsky S. Do unto others or treat yourself? The effects of prosocial and self-focused behavior on psychological flourishing. Emotion (Washington, DC) 2016;16(6):850–861. doi: 10.1037/emo0000178. [DOI] [PubMed] [Google Scholar]
- Nydahl LO. The way things are: A living approach to Buddhism for today’s world. United Kingdom: John Hunt Publishing; 2008. [Google Scholar]
- Oman D, Thoresen CE, Hedberg J. Does passage meditation foster compassionate love among health professionals?: A randomised trial. Mental Health, Religion & Culture. 2010;13(2):129–154. doi: 10.1080/13674670903261954. [DOI] [Google Scholar]
- Oosterman M, De Schipper JC, Fisher P, Dozier M, Schuengel C. Autonomic reactivity in relation to attachment and early adversity among foster children. Development and Psychopathology. 2010;22(1):109–118. doi: 10.1017/S0954579409990290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009;34(1):87–98. doi: 10.1016/j.psyneun.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, Richman LS. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135(4):531–554. doi: 10.1037/a0016095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl JH, Carlozzi AF. Effect of meditation on empathy and anxiety. Perceptual and Motor Skills. 1994;78(1):297–298. doi: 10.2466/pms.1994.78.1.297. [DOI] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, Piliavin JA, Schroeder DA. Prosocial behavior: Multilevel perspectives. Annual Psychology Review. 2005;56:365–392. doi: 10.1146/annurev.psych.56.091103.070141. [DOI] [PubMed] [Google Scholar]
- Piet J, Würtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(6):1007–1020. doi: 10.37/a0028329. [DOI] [PubMed] [Google Scholar]
- Poehlmann-Tynan J, Vigna AB, Weymouth LA, Gerstein ED, Burnson C, Zabransky M, Zahn-Waxler C. A pilot study of contemplative practices with economically disadvantaged preschoolers: Children’s empathic and self-regulatory behaviors. Mindfulness. 2016;7(1):46–58. doi: 10.1007/s1261-015-0426-3. [DOI] [Google Scholar]
- Quaglia JT, Braun SE, Freeman SP, McDaniel MA, Brown KW. Meta-analytic evidence for effects of mindfulness training on dimensions of self-reported dispositional mindfulness. Psychological Assessment. 2016;28(7):803–818. doi: 10.1037/pas0000268. [DOI] [PubMed] [Google Scholar]
- Rilling JK. A potential role for oxytocin in the intergenerational transmission of secure attachment. Neuropsychopharmacology. 2009;34(13):2621–2622. doi: 10.1038/npp.2009.136. [DOI] [PubMed] [Google Scholar]
- Rosenberg EL, Zanesco AP, King BG, Aichele SR, Jacobs TL, Bridwell DA, Saron CD. Intensive meditation training influences emotional responses to suffering. Emotion (Washington, DC) 2015;15(6):775–790. doi: 10.1037/emo0000080. [DOI] [PubMed] [Google Scholar]
- Royle P, Waugh N. A simplified search strategy for identifying randomised controlled trials for systematic reviews of health care interventions: A comparison with more exhaustive strategies. BMC Medical Research Methodology. 2005;5:23. doi: 10.1186/141-288-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonert-Reichl KA, Oberle E, Lawlor MS, Abbott D, Thomson K, Oberlander TF, Diamond A. Enhancing cognitive and social–emotional development through a simple-to-administer mindfulness-based school program for elementary school children: A randomized controlled trial. Developmental Psychology. 2015;51(1):52–66. doi: 10.1037/a0038454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears RW, Tirch DD, Denton RB. Mindfulness in clinical practice. New York: Professional Resource Exchange; 2011. [Google Scholar]
- Segal Z, Williams J, Teasdale J. Mindfulness-based cognitive therapy for depression, second edition. New York: Guilford Press; 2012. [Google Scholar]
- Shamay-Tsoory SG, Abu-Akel A. The social salience hypothesis of oxytocin. Biological psychiatry. 2016;79(3):194–202. doi: 10.1016/j.biopsych.2015.07.020. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine. 1998;21(6):581–599. doi: 10.1023/A:1018700892. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of mindfulness-based stress reduction effects by trait mindfulness results from a randomized controlled trial. Journal of Clinical Psychology. 2010;67(3):267–277. doi: 10.1002/jclp.20761. [DOI] [PubMed] [Google Scholar]
- Shonin E, Van Gordon W, Compare A, Zangeneh M, Griffiths MD. Buddhist-derived loving-kindness and compassion meditation for the treatment of psychopathology: A systematic review. Mindfulness. 2015;6(5):1161–1180. doi: 10.1007/s12671-014-0368-1. [DOI] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- Singer T, Klimecki OM. Empathy and compassion. Current Biology. 2014;24(18):R875–R878. doi: 10.1016/j.cub.2014.05.054. [DOI] [PubMed] [Google Scholar]
- Strauss C, Taylor BL, Gu J, Kuyken W, Baer R, Jones F, Cavanagh K. What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review. 2016;47:15–27. doi: 10.1016/j.cpr.2016.05.004. [DOI] [PubMed] [Google Scholar]
- Strathearn L, Fonagy P, Amico J, Montague PR. Adult attachment predicts maternal brain and oxytocin response to infant cues. Neuropsychopharmacology. 2009;34(13):2655–2666. doi: 10.1038/npp.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C, Harrison J, Haimovitz K, Oberle E, Thomson K, Schonert-Reichl K, Roeser RW. Examining ways that a mindfulness-based intervention reduces stress in public school teachers: A mixed-methods study. Mindfulness. 2015;7(1):115–129. doi: 10.1007/s12671-015-0425-4. [DOI] [Google Scholar]
- Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. Journal of Psychiatric Practice. 2010;16(1):22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- Velásquez AM, López MA, Quiñonez N, Paba DP. Yoga for the prevention of depression, anxiety, and aggression and the promotion of socio-emotional competencies in school-aged children. Educational Research and Evaluation. 2015;21(5–6):407–421. doi: 10.1080/13803611.2015.1111804. [DOI] [Google Scholar]
- Wallace BA. Boundless heart: Cultivation of the four immeasurables. Boston: Snow Lion Publications; 1999. [Google Scholar]
- Wallmark E, Safarzadeh K, Daukantait D, Maddux RE. Promoting altruism through meditation: An 8-week randomized controlled pilot study. Mindfulness. 2013;4(3):223–234. doi: 10.1007/s12671-012-0115-4. [DOI] [Google Scholar]
- Walsh R, Shapiro SL. The meeting of meditative disciplines and Western psychology: A mutually enriching dialogue. American Psychologist. 2006;61(3):227–239. doi: 10.1037/0003-066X.61.3.227. [DOI] [PubMed] [Google Scholar]
- Weinstein N, Ryan RM. When helping helps: Autonomous motivation for prosocial behavior and its influence on well-being for the helper and recipient. Journal of Personality and Social Psychology. 2010;98(2):222–244. doi: 10.1037/a0016984. [DOI] [PubMed] [Google Scholar]
- Weng HY, Fox AS, Shackman AJ, Stodola DE, Caldwell JZ, Olson MC, Davidson RJ. Compassion training alters altruism and neural responses to suffering. Psychological Science. 2013;24(7):1171–1180. doi: 10.1177/0956797612469537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng HY, Fox AS, Hessenthaler HC, Stodola DE, Davidson RJ. The role of compassion in altruistic helping and punishment behavior. PloS One. 2015;10(12):e0143794. doi: 10.137/journal.pone.0143794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng X, Chiu CP, Wang R, Oei TP, Leung FY. The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology. 2015;6:1693. doi: 10.3389/fpsyq.2015.01693. [DOI] [PMC free article] [PubMed] [Google Scholar]


