Abstract
Background: A volar locking plate (VLP) is the most frequently used form of implant used for open reduction and internal fixation of distal radius fractures. They are known to have a complication rate of up to 27%. We hypothesized that plate design could influence complication rates. Methods: We performed a review of patients undergoing VLP fixation for distal radius fracture. A total of 228 patients underwent fixation with the Distal Volar Radial Anatomical (DVR) plate; 388 patients underwent fixation with the VariAx plate. Independent observers performed blinded case note and radiographic review, to assess for the quality of reduction, and complications for the inserted VLP. Results: Mean time to surgery was 6.0 days; mean follow-up was 17.5 weeks. Mean age was 56.5 years. The quality of reduction was classified as anatomical (46%), good (36.3%), moderate (13.0%), or poor (3.9%). Complications were identified in 109 patients (17%). Plate prominence was seen in 133 patients (21%). The DVR plate was less prominent (P < .001) and had better overall radiographic appearances (P = .025). Flexor tendon complications were related to plate prominence (P = .005). Inferior reduction was associated with increased time to surgery (P = .020). Conclusions: This study highlights the importance of prompt surgery, effective fracture reduction, and careful plate positioning to avoid volar prominence.
Keywords: distal radius fracture, volar plating, complications, tendon rupture
Introduction
Distal radius fractures, the most common fracture treated by orthopedic surgeons, are increasing in incidence.6 There is no clear-cut choice of fixation device for displaced fractures and the requirement for anatomical reduction. At the time of this study, volar locking plate (VLP) fixation was the most common method of internal fixation for these injuries,15 with some studies reporting a more rapid return to function compared with percutaneous pinning.20 However, the procedure carries reported complication rates as high as 22% to 27%,1 with specific complications including flexor and extensor tendon injury and intra-articular screw penetration.2
Numerous VLP designs exist. In vitro, biomechanical studies have compared different plates, looking at plate position and screw direction.2 Clinical evidence is lacking and there is no clear consensus on the best performing device. In addition to plate choice, other factors such as surgical experience, fracture type, plate positioning,22 and fracture reduction will influence patient outcomes.
We reviewed our large data set with the specific question: Does choice of plate and its design influence our complication rate?
Materials and Methods
We performed a retrospective review of all patients identified as having a VLP fixation for a distal radius fracture over a 4-year period, between January 2008 and December 2011. Patients who underwent distal radius fixation with a dorsal or nonlocking plate were excluded. Cases were identified from a prospectively maintained, trauma database provided by Bluespier (Bluespier International, Droitwich, Worcestershire, UK). Of the 717 patients initially identified, 623 were considered eligible for review with 94 excluded due to inadequate case notes or radiographs. From the case notes we recorded time of surgery (from injury), grade of operating surgeon, grade of supervisor (where applicable), tourniquet time, the specific VLP, length of stay, and any complications on a designated pro forma.
Fracture Classification
All radiographs were assessed by a senior orthopedic trainee (J.W.) to reduce interobserver variation. Images were viewed on a standard workstation, using the Centricity picture archiving and communication system (PACS; GE Healthcare, Little Chalfont, Buckinghamshire, UK). Fractures were classified by type and group according to the AO system.
Surgical Treatment
The VariAx VLP (Stryker, Kalamazoo, Michigan) was used in 388 patients and the Hand Innovations Distal Volar Radial Anatomical (DVR) VLP (DePuy, Inc, Warsaw, Indiana) in 228 patients. Plate choice was at the discretion of the operating surgeon. Surgeon experience was categorized by training grade (senior house officer: junior orthopedic trainee; specialist registrar and staff grade and associate specialist: senior orthopedic trainees), or consultant subspecialty (consultant orthopedic surgeon or consultant orthopedic hand surgeon).
Quality of Reduction
Fracture reduction was assessed from the postoperative radiographs, using parameters linked to clinical outcomes. Measures of an unsatisfactory reduction on the posteroanterior (PA) radiograph included radial inclination less than 12°27; loss of radial height of more than 2 mm; or a gap or step in the articular surface of 2 mm.16 On the lateral view, dorsal tilting beyond neutral or a gap or step in the articular surface of more than 2 mm were considered unsatisfactory.17 The quality of reduction was further stratified into 4 groups: anatomical, good (reduction satisfactory on PA and lateral radiographs), moderate (reduction satisfactory on only one view), and poor (reduction unsatisfactory on both PA and lateral views).
Plate Positioning
The postoperative radiographs were assessed for adequacy of plate positioning. Intra-articular screw penetration (distal radioulnar joint [DRUJ] or radiocarpal joint) was recorded. Prominence of the distal extent of the VLP beyond the volar rim of the distal radius was assessed by the method described by Soong et al22 using the best postoperative lateral radiograph (Figure 1) and accordingly plates were classed as grade 0, 1, or 2. Plates not fixed flush to the volar cortex were documented as suboptimal technique.
Figure 1.

Lateral radiograph with red line drawn along volar cortex of the distal radius and parallel green line drawn at volar rim. Used to assess plate position as described by Soong.22
Incorrect screw/peg positioning was also reviewed. If a screw/peg was completely missing the distal radius or protruded beyond the dorsal cortex, they were classified as a poor outcome if the patient developed extensor tendon irritation or pain. If no symptoms were present from the incorrectly placed screw, then it was documented as suboptimal technique.
Summary Assessment of Radiographic Appearance
For an overall assessment of the fixation, the analysis of quality of reduction and the technical aspects of the hardware positioning were combined and each fixation categorized as having either appearances that were “Satisfactory,” technically “Suboptimal” (but not linked to poor outcome), or “Linked to poor outcome.”
The criteria for being classed as “Linked to poor outcome” are listed in Table 1. Fixations were classified as “Suboptimal” if the criteria in Table 1 were not met but: the plate was not flush to bone, if it was too distal, or if the plate was overhanging in the mediolateral plane. Fixations were “Satisfactory” if none of the criteria for “Linked to poor outcome” or “Suboptimal” could be applied.
Table 1.
Criteria for Fixation as Having Radiographic Appearances Linked to Poor Outcome.
| Criteria for radiographic appearances being “Linked to poor outcome” |
|---|
| Quality of reduction |
| Radial inclination < 12° |
| Loss of radial height >2mm |
| Articular gap or step >2mm |
| Dorsal tilting beyond neutral |
| Metalwork positioning |
| Plate prominent beyond volar rim (Soong Grade 2) |
| Intra-articular screw/peg |
| Screw/peg prominence + documented symptoms |
| Entirely extra-osseous screw placement |
These groupings were generated in an ordinal fashion (“Satisfactory” indicating the best radiographic appearance and “Linked to poor outcome” representing the worst radiographic appearance) to facilitate statistical analysis.
Statistical Analysis
We compared many factors such as surgeon experience, AO classification, and type of plate used with quality of reduction. These categorical data and similar analyses were performed using the chi-square test (or Fisher exact test if expected values were less than 1, or 20% were less than 5). Mann-Whitney U tests were used for continuous variables with nonnormal distributions. Independent samples t tests were used to compare means where a normal distribution was present. Binary regression was used to look for factors that may be associated to a less favorable reduction. Regression analysis was also performed to evaluate effect sizes and for factors which may be associated with flexor tendon complications specifically and complications more generally. Ordinal regression was used to identify factors associated with the overall radiographic appearance of the fixations. Statistical analysis was carried out using SPSS 20 (SPSS Inc, Chicago, Illinois).
Results
DVR plates were used in 228 cases (37%) and VariAx in 388 (63%). The right distal radius was fixed in 262 patients (42%). The average age of the patient was 56.5 years (95% confidence interval [CI], 55.1-57.9) with a mean follow-up duration of 17.7 weeks for the DVR plate and 17.3 weeks for the VariAx plate. Details of tourniquet time and time to surgery are shown in Supplemental Table 1.
The type of fracture (according to the AO Classification of fractures) is shown in Supplemental Table 2. The proportion of cases performed according to surgeon seniority is displayed in Figure 2. The results for quality of reduction are shown in Figure 3.
Figure 2.
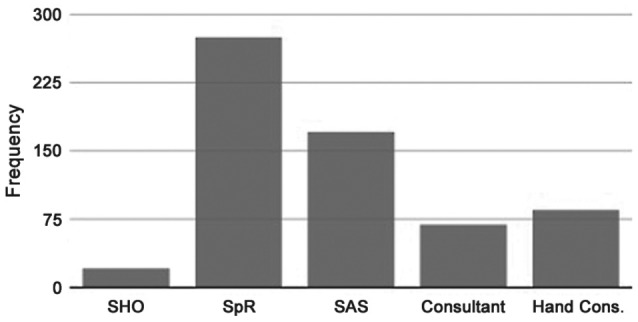
Number of surgeries performed categorized by surgeon seniority/specialization. SHO = senior house officer; SpR = specialist registrar; SAS = staff grade and associate specialist.
Figure 3.
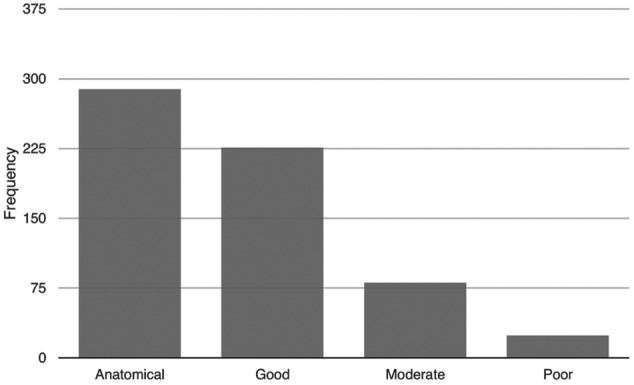
Number of cases performed according to the quality of reduction achieved.
Plate prominence assessed according to the method described by Soong et al22 found 133 (21.3%) sitting proud of the volar rim (Group 2). The majority of cases showed the plate to be either level with the volar lip (Group 1, 56.8%) or recessed behind it (Group 0, 21.2%). When taking into account the quality of reduction, plate position, and screw placement, over a third of cases had radiographic features that have a link to poor outcome (Supplemental Table 3).
Fracture reduction was correlated with the seniority and grade of the operating surgeon and seniority of the supervising surgeon. Both comparisons showed no significant difference (P = .94). As multiple factors may have influenced the complexity of case, binary regression was performed, including time to surgery, severity of injury (C3 fracture), and operating surgeon grade in the model. The dependent variable used was satisfactory or unsatisfactory reduction. Only “time to surgery” was found to be a significant variable, altering the likelihood of a satisfactory reduction (P = .020, odds ratio: 1.036). This equates to an increased absolute risk of unsatisfactory reduction of 0.5% for each day of delay, or a relative risk of 3% per day.
Overall, there were 144 complications in 109 patients (Figure 4). The presence of a flexor tendon rupture or evidence of flexor tenosynovitis was compared with plate prominence, using Fisher exact test. This revealed a statistically significant association between a proud plate (Soong Grade 2) and flexor tendon problems with an odds ratio of 4.7 (95% CI, 1.6-13.7) (P = .005).
Figure 4.
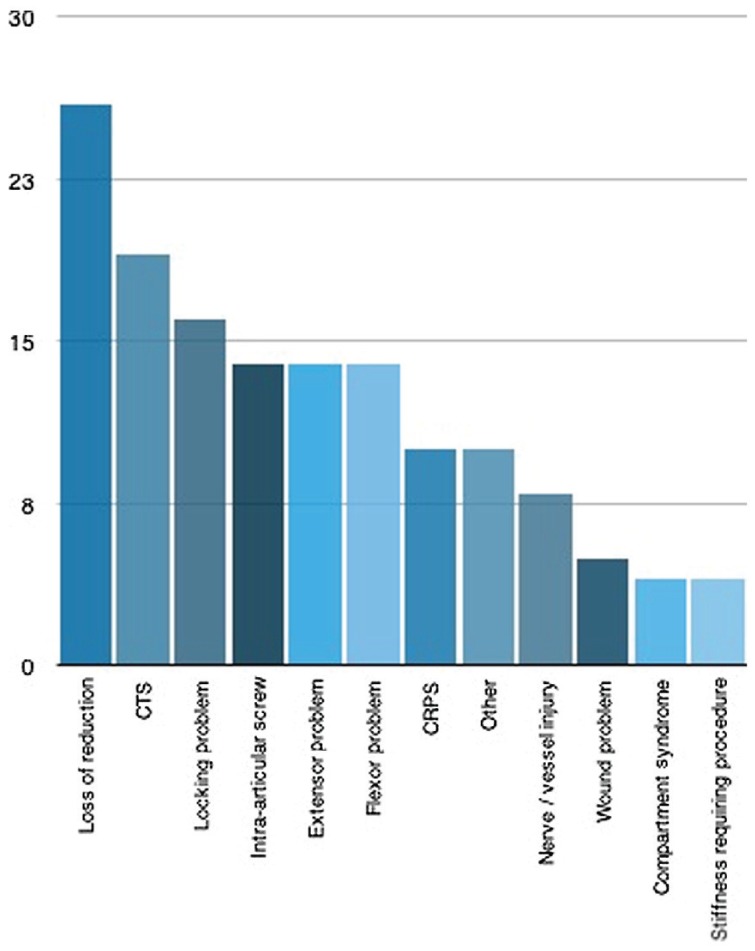
Frequency of different types of complication. CTS = carpal tunnel syndrome; CRPS = complex regional pain syndrome.
Regression analysis was performed to look for an association between patient age, delay to surgery, plate type, initial reduction, and severity of injury with results shown in Table 2. We identified a significant increase in complication rate with a delay to surgery. Type AO C3 fractures were associated with higher complication rates; satisfactory reduction was associated with a lower complication rate.
Table 2.
Variables Relating to Occurrence of Any Complication.
| Significance (P value) | Odds ratio | 95% CI | |
|---|---|---|---|
| Age (years) | .304 | 1.01 | 0.99-1.03 |
| Delay to surgery (days) | .026 | 1.05 | 1.01-1.09 |
| Plate (VariAx) | .799 | 1.06 | 0.68-1.65 |
| Satisfactory reduction | .013 | 0.52 | 0.19-0.87 |
| Severe injury (C3 fracture) | .014 | 1.77 | 1.12-2.78 |
Note. Significant factors shown in bold. CI = confidence interval.
To compare the VariAx and DVR plates, we ensured age, delay to surgery, follow-up duration, and proportion of C3 fractures were comparable between the 2 groups (Table 3). The proportion of plates used for different AO categories (A, B, or C) was also examined using a chi-square test.
Table 3.
Comparison of Baseline Variables and Follow-up Duration for the DVR and VariAx Plate Groups.
| Parameter | DVR | VariAx | Significance (P value) |
|---|---|---|---|
| Mean age (years) | 56.9 | 56.3 | .900 |
| Mean time to surgery (days) | 6.3 | 5.8 | .389 |
| Proportion with C3 fractures (%) | 26 | 26 | .953 |
| Follow-up duration (weeks) | 17.7 | 17.3 | .732 |
Note. DVR = Distal Volar Radial.
A comparison of complications and technical errors between the 2 plates is shown in Table 4. The VariAx plates were positioned on or beyond the volar rim of the distal radius in a significantly higher number of cases compared with the DVR plates. Twelve instances of flexor tendon rupture or symptomatic tenosynovitis were recorded in the VariAx group, while only 2 cases were identified in the DVR group. All of the other parameters also showed trends that the DVR had fewer complications and fewer instances where removal was required, although no significant P value was reached in any parameter.
Table 4.
Comparison of Technical Problems and Complications for the DVR and VariAx Plate Groups.
| DVR % (number) | VariAx % (number) | Significance (P value) | |
|---|---|---|---|
| Intra-articular screw | 5 (11) | 5 (18) | .968 |
| Plate not flush to bone | 8 (19) | 13 (51) | .306 |
| Plate too distal | 14 (33) | 16 (61) | .590 |
| Plate too prominent (Soong grade 2) | 14 (32) | 26 (100) | <.001 |
| All complications | 17 (38) | 18 (70) | .611 |
| Complication attributable to metalware | 7 (16) | 11 (41) | .129 |
| Flexor complication | 1 (2) | 3 (12) | .071 |
| Metalware removal | 5 (11) | 8 (30) | .150 |
Note. Significant factors shown in bold. DVR = Distal Volar Radial.
Analysis was performed with the overall radiographic appearance used as the dependent variable after the radiographs had been split into the 3 groups mentioned previously (Table 1). We performed ordinal regression analysis, selecting time to surgery, type of plate used, operating surgeon grade, and presence of a C3 fracture as the independent variables (Supplemental Table 4). The significant findings were the presence of a C3 fracture being associated with worse postoperative radiographic appearances (P = .005) and that using a DVR plate, rather than a VariAx plate, was associated with better radiographic appearances.
Discussion
The primary goal in treating unstable distal radius fractures is to achieve optimal stable restoration of the disrupted anatomy, allowing rapid return to wrist function while preventing secondary displacement of the fracture. If the joint surface is also disrupted, care must also be taken to secure and maintain anatomic reduction of the articular surface.17 A pain-free, mobile wrist joint without functional limitation is the ultimate aim.
The correlation between radiological parameters and objective physical variables is controversial,10 and the relationship between these traditional objective measurements and the patient-perceived outcome is not entirely clear.14 However, Wilcke et al27 showed that after distal radius fractures, malunion was associated with poorer patient rated outcomes using the DASH score (Disabilities of the Arm, Shoulder and Hand11). This was true for radial shortening, loss of volar tilt, and loss of radial inclination.27 Furthermore, biomechanical studies have shown increases in radiocarpal contact areas and pressures with radial shortening; dorsoulnar migration of contact pressures with increased dorsal inclination; and shifts in the instant center of rotation during pronation and supination with changes in radial height, inclination, and volar tilt.3 However, Forward et al demonstrated that often there was little correlation between radiographic parameters and patient recorded outcome measures in the long term, and imperfect reduction may not result in posttraumatic arthritis.9
Conventional plate and screw constructs require compression between the plate and fragment to produce friction for stability, while a locking plate and its screws act as a single unit, maintaining a fracture reduction even in the presence of impaired bone quality.25 These plate systems provide improved fixation strength, superior stiffness, and axial loading strength compared with nonlocking plates.2 A further advantage of these devices is that they can be positioned along the volar cortex of the distal radius and still control dorsally displaced fractures. This avoids the extensor tendon irritation associated with dorsal plate fixations.21 However, the potential for flexor tendon irritation and other complications needs to be considered.
The overall complication rate in our study was 17% (109 patients). Other series have reported values ranging from 3%7 to 27%.13 Variability in these figures may be due to differences in follow-up times, complication definitions, and exclusion of more complex injury patterns. With reference to complexity of injury, we did find that the presence of a C3 type fracture was associated with an increased chance of a complication (odds ratio: 1.77), as was increasing time to surgery. A satisfactory reduction was an independent factor associated with a lower overall complication rate. These findings are intuitive and may indicate that ensuring prompt treatment and achieving satisfactory reductions could reduce overall complication rates. Identifying the more complex injury patterns may help in patient counseling and warrant increased vigilance for postoperative problems.
Concern with regard to volar prominence of the plate, beyond the volar rim of the distal radius, has been voiced by previous authors. Arora et al defined the watershed line as a transverse ridge that closures the concave surface of the volar radius distally and stated that implants placed over or distal to this line can cause flexor tendon complications.1 This concern was also raised by Cross and Schmidt7 who reported flexor digitorum profundus and flexor pollicis longus (FPL) ruptures where no fracture collapse had occurred. In 2011, Soong et al published the grading system used in this study and showed a tendency for flexor tendon complications if the distal plate extended beyond the volar rim of the distal radius.22 In addition, a detailed anatomical study of the macroscopic and histologic structure of the volar aspect of the distal radius concluded that the medial and lateral bony prominences on the volar radius should be key structures for accurate plate placement to avoid flexor tendon injury.12 We identified a statistically significant association between a prominent plate position and flexor tendon complications and were able to estimate the odds ratio of developing a flexor tendon rupture or symptomatic tenosynovitis to be 4.7 (95% CI, 1.6-13.7).
The motivation to avoid positioning the plate too distal has to be balanced by the requirement for the locking screws or pegs to support subchondral bone.2 Biomechanical studies have shown that the distal-most screws or pegs need to be positioned just beneath the subchondral bone of the articular surface. In a cadaver model, screw fixations placed ≥4 mm proximal to subchondral bone led to double the fracture displacement with cyclic loading, when compared with fixations within the subchondral zone. Furthermore, rigidity at load-to-failure was reduced by half in the proximal fixation group.8 Orbay and Fernandez18 also described this phenomenon in vivo, with loss of volar tilt occurring in 3 of 24 elderly patients. “Settling” occurred until the distal pegs abutted the subchondral plate. Therefore, plate positioning needs to be precise to maintain reduction while avoiding flexor tendon irritation.
We identified that use of a DVR plate had a significantly lower rate of volar plate prominence (Soong Grade 2) in comparison with the VariAx plate. There are some design features of the device that may account for this. The plate is cutaway in the frontal plane more distal on the radial side than the ulnar side, helping to protect from irritation of the FPL tendon. The plate is also tapered distally in an anterior to posterior direction.23 The DVR plate is designed to be placed just proximal to the watershed line and not project above or beyond this line compared with the VariAx plate which is placed slightly below the distal edge of the radius. Imatani et al highlight plate thickness distally, as excessive plate thickness can negate the theoretical safety of positioning the plate proximal to the watershed line.12 The VariAx plate has a uniform thickness along its length. Soong et al23 also speculated that the design or practical application of the DVR plate helps to limit the risk of tendon irritation. The VariAx plate’s slightly more distal position and its uniform thickness along its length might make it more susceptible to flexor tendon complications although our P value of .071 indicates no significant difference between the plates.
The AcuLoc distal plating system (Acumed, Hillsboro, Oregon) is designed to placed distal to the watershed line, Tanaka et al compared this to the VariAx plate which is designed to be placed proximal to, without overlying, the watershed line. They found similar outcomes at 6 months from surgery with regard to grip strength and wrist range of motion, but a VLP placed distal to the watershed line may delay recovery of wrist motion.24
Extensor tendon complications were as prevalent as flexor tendon problems in this study. There was no significant difference in this complication between the 2 main plate designs. Limiting the dorsal penetration of pegs or screws beyond the dorsal cortex and utilizing a “skyline” view of the distal radius to help identify excessively long implants has been advocated by previous authors to reduce this issue.19 Overall, the proportion of cases requiring metalwork removal was 7% which is comparable with other published studies.1
There are some limitations to this study. The first is the retrospective nature of the review. This can harbor confounding sources of bias and relies on complications being documented in the clinic letters. Also, we were not able to include patient-reported outcome measure scores (PROMS) and use radiographic features as a proxy to PROMS. The radiographic features which have been analyzed have been carefully chosen because they are linked to patient outcomes.10,14,16 The radiographic assessments were performed with blinding from the medical notes information. However, features such as the type of plate used could not be hidden during the analysis that is a further potential source of bias. The assessment of intra-articular fractures was performed using plain radiographs which are less accurate than computed tomographic scans at identifying a significant articular step. Furthermore, associated injuries to the soft tissues or cartilage could not be detected with the available imaging. We also acknowledge that there may be complications which have not been picked up within the follow-up period. Posttraumatic degeneration was not detected in our study and even flexor tendon ruptures have been reported as late as 56 months postsurgery.26 Perhaps the largest limitation has been the change in practice in using fewer VLP and more percutaneous wire fixation since the publication of the Distal Radius Acute Fracture Fixation Trial (DRAFFT) paper in 2014.4,5
This study did not identify a difference between surgeons of different grades regarding complication rate, quality of reduction, or the summary radiographic appearance of the postoperative radiographs. This may be due to several factors which include case selection, with more challenging fractures being directed to more senior surgeons. Different grades of doctor may also possess wide variability in the volume of distal locking plate fixations that they perform. Soong et al found even high-volume surgeons having increased rates of late complications, underlining the complexity of confounding factors at play.23
Conclusion
In conclusion, this retrospective analysis of over 600 patients has indicated that, in comparison with the VariAx plate, the DVR plate had a statistically significant lower rate of volar plate prominence and a lower incidence of flexor tendon complications although this later finding did not reach statistical significance. This study also confirms that more complex fractures (C3) are associated with higher complication rates and worse radiographic outcomes. In addition, delaying surgery is also associated with increasing risks of complications.
It is important surgeons take steps to accurately position distal radius VLPs to avoid volar prominence and intra-articular screw penetration. Careful selection of screw length should be made to avoid extensor tendon irritation.
Supplementary Material
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All study procedures were followed in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent: Informed consent was obtained from all patients included with the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Arora R, Lutz M, Hennerbichler A, et al. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316-322. [DOI] [PubMed] [Google Scholar]
- 2. Buzzell JE, Weikert DR, Watson JT, et al. Precontoured fixed-angle volar distal radius plates: a comparison of anatomic fit. J Hand Surg Am. 2008;33:1144-1152. [DOI] [PubMed] [Google Scholar]
- 3. Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89:2051-2062. [DOI] [PubMed] [Google Scholar]
- 4. Costa ML, Achten J, Parsons NR, et al. Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: randomized controlled trial. BMJ. 2014;349:g4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Costa ML, Jameson SS, Reed MR. Do large pragmatic randomised trials change clinical practice? assessing the impact of the Distal Radius Acute Fracture Fixation Trial (DRAFFT). Bone Joint J. 2016;98-B:410-413. [DOI] [PubMed] [Google Scholar]
- 6. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691-697. [DOI] [PubMed] [Google Scholar]
- 7. Cross AW, Schmidt CC. Flexor tendon injuries following locked volar plating of distal radius fractures. J Hand Surg Am. 2008;33A:164-167. [DOI] [PubMed] [Google Scholar]
- 8. Drobetz H, Bryant AL, Pokorny T, et al. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction—a biomechanic study in a cadaveric model. J Hand Surg Am. 2006;31A:615-622. [DOI] [PubMed] [Google Scholar]
- 9. Forward DP, Davis TR, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008;90-B:629-637. [DOI] [PubMed] [Google Scholar]
- 10. Fuji K, Hemni T, Kanematsu Y, et al. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg. 2002;10(1):9-15. [DOI] [PubMed] [Google Scholar]
- 11. Germann G, Wind G, Harth A. The DASH (Disability of Arm-Shoulder-Hand) Questionnaire—a new instrument for evaluating upper extremity treatment outcome. Handchir Mikrochir Plast Chir. 1999;31:149-152. [DOI] [PubMed] [Google Scholar]
- 12. Imatani J, Akita K, Yamaguchi K, et al. An anatomical study of the watershed line on the volar, distal aspect of the radius: implications for plate placement and avoidance of tendon ruptures. J Hand Surg Am. 2012;37(8):1550-1554. [DOI] [PubMed] [Google Scholar]
- 13. Kamano M, Koshimune M, Toyama M, et al. Palmar plating system for Colle’s fractures—a preliminary report. J Hand Surg Am. 2005;30:750-755. [DOI] [PubMed] [Google Scholar]
- 14. Karnezis IA, Panagiotopoulos E, Tyllianakis M, et al. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005;36:1435-1439. [DOI] [PubMed] [Google Scholar]
- 15. Mignemi ME, Byram IR, Wolfe CC, et al. Radiographic outcomes of volar locked plating for distal radius fractures. J Hand Surg Am. 2013;38:40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ng CY, McQueen MM. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011;93:145-150. [DOI] [PubMed] [Google Scholar]
- 17. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205-215. [DOI] [PubMed] [Google Scholar]
- 18. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29:96-102. [DOI] [PubMed] [Google Scholar]
- 19. Riddick AP, Hickey B, White SP. Accuracy of the skyline view for detecting dorsal cortical penetration during volar distal radius fixation. J Hand Surg Eur. 2011;37:407-411. [DOI] [PubMed] [Google Scholar]
- 20. Rozental TD, Blazar PE, Franko OI, et al. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1837-1846. [DOI] [PubMed] [Google Scholar]
- 21. Ruch DS, Papadonikolakis A. Volar versus dorsal plating in the management of intra-articular distal radius fractures. J Hand Surg Am. 2006;31:9-16. [DOI] [PubMed] [Google Scholar]
- 22. Soong M, Earp BE, Bishop G, et al. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011;93:328-335. [DOI] [PubMed] [Google Scholar]
- 23. Soong M, van Leerdam R, Guitton TG, et al. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011;36:3-9. [DOI] [PubMed] [Google Scholar]
- 24. Tanaka H, Hatta T, Sasajima K, et al. Comparative study of treatment for distal radius fractures with two different palmar locking plates. J Hand Surg Eur. 2016;41:536-542. [DOI] [PubMed] [Google Scholar]
- 25. Trease C, McIff T, Toby EB. Locking versus nonlocking T-plates for dorsal and volar fixation of dorsally comminuted distal radius fractures: a biomechanical study. J Hand Surg Am. 2005;30:756-763. [DOI] [PubMed] [Google Scholar]
- 26. White BD, Nydich JA, Karsky D, et al. Incidence and clinical outcomes of tendon rupture following distal radius fracture. J Hand Surg Am. 2012;37:2035-2040. [DOI] [PubMed] [Google Scholar]
- 27. Wilcke MK, Abbaszadegan H, Adolphson PY. Patient-perceived outcome after displaced distal radius fractures. A comparison between radiological parameters, objective physical variables, and the DASH score. J Hand Ther. 2007;20:290-298. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


