Abstract
Background: Disability of the upper limb is one of the consequences of distal radius fracture (DRF). The outcome of DRF treatment is based on objective clinical variables, as strength or range of movement (ROM); sometimes these variables do not correlate with the functional level of the patient. The principal objective of our study was to assess the repercussion of conservative treatment of DRF on upper limb disability. Methods: This is a retrospective review of prospectively collected data. We collected data of 61 nonconsecutive DRFs treated conservatively from July 2007 to August 2008. Results: Average Disabilities of the Arm, Shoulder and Hand (DASH) score before fracture was 20.8 points; average DASH score after the fracture was 42.6. There was a significant increase in the upper limb disability after 1 year of follow-up in the patients treated conservatively (P < .001; size effect, 1.06). Average radial inclination, radial tilt, and radial length were 18.18°, 3.35°, and 5.76 mm, respectively. Average ROM for flexion-extension was 100.6° and for pronation-supination 144.0°. ROM for flexion-extension of the unaffected wrist was 128.2° and for pronation-supination 172.4°. We did not find any significant statistical correlation between the increase in disability and the decrease in the ROM (P > .05). We did not find any significant statistical correlation between the increase in the disability and the worsening in the radiological parameters (P > .05). Our results confirm the hypothesis that the conservative treatment of DRF produced an increase in the upper limb disability after 1 year of follow-up. Conclusions: Our study does not show a correlation between the increase in upper limb disability and the decrease in wrist ROM. Our study did not find a correlation between radiological measures and DASH scores.
Keywords: DASH, PRO, distal radius fractures, conservative treatment, disability
Introduction
Distal radius fracture (DRF) is one of the most common types of fractures, and the most common fracture treated in emergency departments all over the world.23,24 The incidence of this fracture has been increasing in past years especially in older adulthood due to the aging of the global population that expect to be living independent lives. And because life expectancy is improving, DRFs will continue to be one of the most commonly treated injuries in emergency departments.22
According to our hospital’s emergency records of fractures, 150 DRFs were treated from 2007 to 2008, accounting for 11.25% of all the fractures treated in the emergency department during that period. These data are similar to what has been previously found in literature.22,24
Traditionally, the outcome of DRF treatment is based on objective clinical variables, for example, strength or range of movement, but sometimes these variables do not correlate with the functional level of the patient.13,14
Moreover, these traditional instruments of measuring wrist function do not take into account these other aspects related to analysis outcome, such as the patient’s ability to carry out activities of daily living, the ability to return to previous occupations, and pain.7
The principal objective of our study was to assess the effect of conservative treatment of fractures of the distal radius on upper limb disability. Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire was self-administered at the moment of the diagnosis of the fracture and after a year of follow-up. Functional and radiological assessment was also performed.
Materials and Methods
Patients
This is a retrospective review of prospectively collected data. We collected data of nonconsecutive fractures of the distal radius treated conservatively in the emergency departments of our hospital from July 2007 to August 2008. A total of 150 DRFs were treated during that period.
Patients with open physis at the moment of the diagnosis of the fracture, patients incapable of responding to DASH questionnaire, patients presenting bilateral fractures or polytraumatism, and patients who were operated on were excluded from the review.
Patients with unstable fractures (volar tilt < −10°, shortening ≥3 mm, articular step-off ≥2mm)19-21 were sent to surgery.
Fracture Treatment
Once the fracture was diagnosed, we proceeded to perform a closed reduction under haematoma block. The manipulation was controlled under imaging amplification, and the wrist was immobilized with an antebraquial circular plaster cast. All the patients underwent a closed reduction.
After the reduction maneuver, posteroanterior and lateral radiographs views were performed on each patient to check the correct reduction of the fracture. After this radiological control, we decided whether the fracture was going to be treated conservatively or surgically following the instability criteria mentioned formerly. Patients with radiographs showing a radial shortening of more than 3 mm, dorsal tilt of more than 10°, or intra-articular step-off of more than 2 mm were considered to be surgically treated.21
Patients were radiographed again in the emergency room a week later to check whether there were any secondary displacements in the fracture. If radial shortening was more than 3 mm, dorsal tilt was more than 10°, or intra-articular step-off was more than 2 mm, the patient was sent to surgery. The rest of the patients were sent to the clinics where their casts were removed between the fourth and sixth weeks after the fractures occurred.
Epidemiological Data and Mechanism of Injury
We collected all basic epidemiological data and mechanisms of injury, as well as descriptions of the patients’ work activity.
Fracture Classification
All the initial fractures of the patients were classified by the same author using the AO classification. Six radiographs were lost due to fire damage that affected the server of the Radiology Department in December 12, 2007.
DASH Questionnaire
Patients were asked to complete the DASH questionnaire (Spanish validated version)25 referring to their health status before the fracture. After 1 year, the patients were asked to complete the questionnaire again.
Radiographic Evaluation
Postreduction radiographs (posteroanterior and lateral views) were used to evaluate the radial tilt, the radial inclination, and the radius length (measured in millimeters), according to predefined published measurements.16
Radial length was defined as the axial difference between the distal radial and ulnar articular surfaces on a posteroanterior radiograph of the wrist4,18,27 as shown in Figure 1a. Ten to twelve millimeters is the average radial length.27 Ten millimeters was set as normal.6
Figure 1.
Radiographic measurements of distal radius. (a) On posteroanterior (PA) radiography, the radial length (RL) is distance between 2 tangents drawn at the radial styloid and the ulnar pole, perpendicular to their shaft axes. (b) On a lateral radiography, radial tilt (RT) is the angle between the articular surface and a line perpendicular to the radial shaft. (c) The radial inclination (RI) is the angle subtended by a perpendicular to the long axis of the radius and a line reflecting the articular surface of the radius, on a PA view.
Radial inclination was determined on a posteroanterior radiograph as shown in Figure 1a. We set 22° as average radial tilt.6 Radial tilt was also determined in a lateral radiograph as shown in Figure 1b. Normal radial tilt was defined as 11.5°.3,6,27
Radiological measurements were taken 1 year after the fracture and were compared with the normal parameters given previously.
Functional Outcome
After at least 1 year of follow-up, patients were examined to determine the wrist range of movement (flexion-extension and pronation-supination). We utilized a manual goniometer, and the measurement was taken in degrees. We used the unaffected wrist as a control. We measured pain using a visual analog scale (VAS). The Wilcoxon test was used to compare DASH before and after fracture, as the sample does not follow a normal distribution. Correlation coefficients were determined by the Spearman rho correlation test.
All data were analyzed by SPSS 15.0 software (IBM Corp., New York).
Results
Epidemiological Data and Mechanism of Injury
Initially, we had 61 patients with DRF. After 1 year, we had 38 patients (5 men and 33 women), with an average age of 62.6 years (range, 18-91) and an average follow-up of 13.53 months. We lost 23 patients: 2 of them died due to unrelated causes to the fracture, 12 were unable to be contacted by telephone or post, 2 of them were not able to come to the appointment because of systemic problems, and 7 were excluded because they were operated on in other hospitals. Nineteen fractures happened in the right wrist and 18 in the left. Nineteen of the fractures occurred on the dominant side.
Seventeen patients were of working age (less than 65 years old). Of these, 14 were women (8 housewives, 2 secretaries, 3 housekeepers, and 1 teacher). The 3 men were a receptionist, a baker, and a student, respectively. The vast majority of the patients did not do heavy manual work.
The main mechanism of injury was a fall from standing, except in 2 of the cases where the fracture occurred in a traffic accident, and 3 cases where it involved sporting activity.
DASH Questionnaire
The average score of DASH questionnaire before fracture was 19.6 points, whereas the average DASH score after the fracture was 42.1 (Figure 2).
Figure 2.
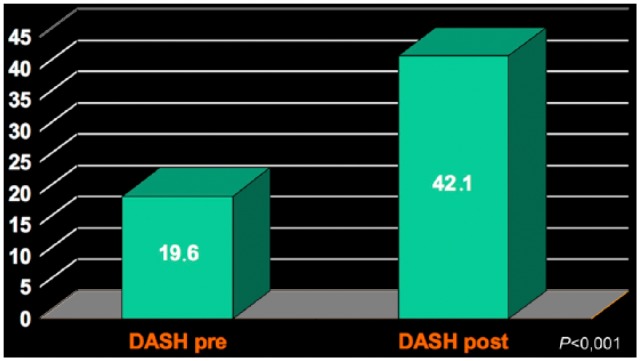
Disabilities of the Arm, Shoulder and Hand (DASH) variation in the follow-up time.
Radiographic Assessment
Seventy-five percent of the fractures corresponded to 23A of AO classification and the rest to the type 23B. No C-type fractures were found. No subset analyses were done to compare the difference between type A and B fractures.
Radiological measurements were taken after 1 year of follow-up. The average radial inclination was 18.18°, and average radial tilt was 3.35°. The average radial length was 5.76 mm (Figure 3).
Figure 3.
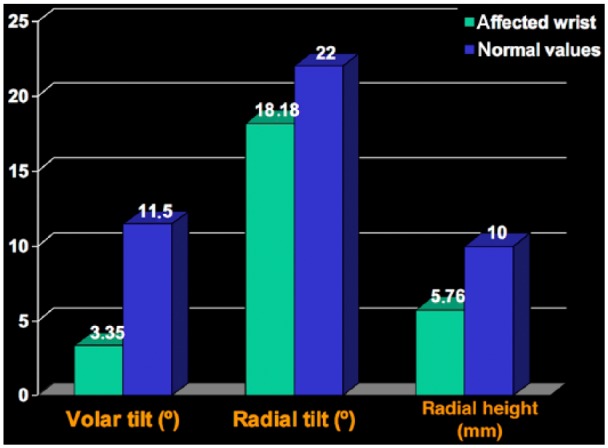
Radiological measurements comparing radiological parameters in both affected and unaffected wrists.
Functional Assessment
The average range of motion for flexion-extension was 100.6°, and the pronation-supination was 144.0°. The range of movement for flexion-extension of the unaffected wrist was 128.2° and 172.4° for pronation-supination (Figure 4). The average VAS after the fracture was 3.5. Only 23% of the patients had no pain (VAS = 0) after 1 year. We found an increase of upper limb disability after 1 year of conservative treatment of DRF. We did not find any significant statistical correlation between the disability and the decrease in the range of movement (P > .05).
Figure 4.
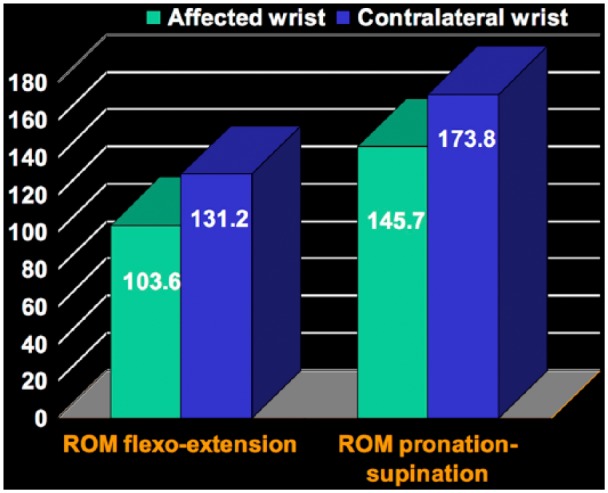
Range of movement (ROM) comparing both affected and unaffected hands.
There was a significant increase in the upper limb disability after 1 year of follow-up in the patients treated conservatively (P < .001; Figure 5). We did not find any significant statistical correlation between the increase in disability and the decrease in the range of movement (P > .05), even when using age as a cofactor.
Figure 5.
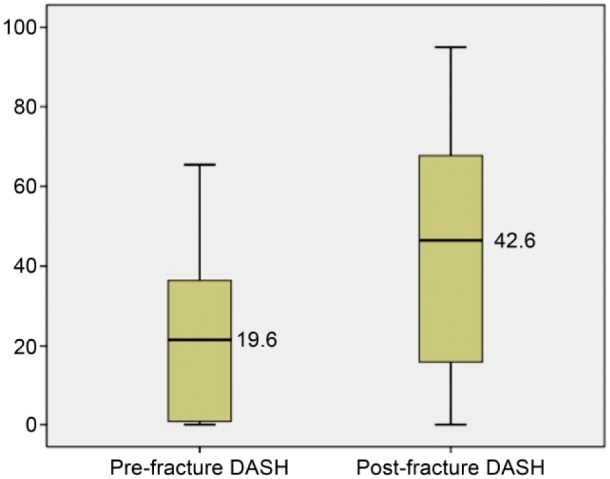
Significant increase in the upper limb disability after 1 year of follow-up in the patients treated conservatively (P < .001).
Note. DASH = Disabilities of the Arm, Shoulder and Hand.
We also did not find any significant statistical correlation between the increase in the disability and the worsening in the radiological parameters either (P > .05).
Discussion
Our results confirm the hypothesis that the conservative treatment of DRF produced an increase in the upper limb disability after 1 year of follow-up.
Some authors, including Colles’ first publication on this matter,9 defended the successful result of the conservative treatment of DRF, with good adaptation to the patient’s daily life activities, even in the ones with wrist deformities.
Young and Rayan,29 in their retrospective study, demonstrated good functional results after displaced DRFs treated conservatively.
More recently, Arora et al published a retrospective study comparing the surgical treatment (open reduction and plate fixation) with cast immobilization in patients older than 70 years affected with unstable DRF. They did not find any significant difference in the range of movement, strength, or function (measured with DASH, Patient-Rated Wrist Evaluation [PRWE], and Green and O’Brien questionnaires), but they found better radiological outcomes in the surgical group.3
Many studies showed that a radiological malalignment led to a bad outcome (Table 1). Fuji et al demonstrated that fractures with 6 mm or more of radial shortening after 1 year of consolidation had a worse outcome.10 Aro and Koivunen found that in a 92-patient study, even a minimal radial shortening produced a greater risk of permanent disability.2
Table 1.
Characteristics of the Reviewed Studies.
| Author | Study design | n | Age | Treatment | Radiological parameters | PRO scales | Results |
|---|---|---|---|---|---|---|---|
| Karnezis and Fragkiadakis (2002)17 | Prospective cohort, FU 1 y | 30 | 46 | CR + KW + cast | RS/RT/VT | PRWE | Correlation between VT and pain |
| Gliatis et al12 | Retrospective | 160 | 35 | Several | RS/RT/VT/articular gap | Modified PEM | Correlation between RS >10° and pain |
| Chung et al (2007)8 | Prospective cohort, FU 1 y | 66 | 49 | ORIF | RS/RT/VT/articular gap | MHQ | Correlation between gap articular and MHQ at 3-mo FU (not 1-y FU) |
| Kumar et al18 | Prospective cohort, FU 1 y | 95 | 67 | CR | RS/RT/VT | DASH/MHQ | Correlation between RS <15° and “satisfactory” scores |
| Jaremko et al15 | Prospective cohort, FU 6 mo | 74 | 68 | CR | RS/RT/VT/articular gap | DASH/SF12 | No correlation |
| Wilcke (2007)28 | Retrospective, FU 22 mo | 78 | 59 | CR | RS/RT/VT | DASH | No correlation |
| Anzarut et al (2004)1 | Prospective, FU 1 y | 74 | 68 | CR | RS/RT/VT | DASH/SF12 | No correlation |
| Grewal et al14 | Prospective, FU >1 y | 222 | 58 | CR | RS/RT/UV ulnar styloid fracture | DASH/PRWE | Correlation in <65-year-olds; no correlation in >65-year-olds |
| Barton et al4 | Retrospective | 60 | 70 | KW | RS/RT/VT | PRWE | No correlation |
Note. KW = closed reduction with Kirschner wires; RS = radial shortening; RT = radial tilt; VT = volar tilt; PRWE = Patient-Rated Wrist Evaluation; PEM = Patient Evaluation Measure; MHQ = Michigan Hand Outcomes Questionnaire; DASH = Disabilities of the Arm, Shoulder and Hand; UV = ulnar varianza; PRO = patient-rated outcome; FU = follow-up; CR = closed reduction; ORIF = open reduction internal fixation.
Eighty-five patients with displaced Colles fractures were reviewed in another study.17 The authors concluded that radial shortening measured at the moment of the fracture and after 10 years of follow-up showed a positive correlation. Dorsal angulation affected the disability on a short-term basis, but not at the 10-year follow-up.
In many other studies, radial shortening had been associated to a poor functional outcome.11,26 Karnezis and Fragkiadakis found a correlation between increasing in radial shortening and a low PRWE score in their series. They also found a correlation between the loss of palmar tilt and the “pain scale” of the PRWE questionnaire.13,17 In the same manner, Gliatis et al showed that more than 10° of dorsal angulation correlated with a lower score in a modified Patient Evaluation Measure (PEM) questionnaire.12 Brogren et al found in their study of DRFs (treated operatively and nonoperatively) that malunion (dorsal tilt exceeding 10° and/or positive ulnar variance) was associated with higher arm-related disability at 1 and 2 years after injury regardless of patient age or sex).5 Kumar et al defended an acceptable correlation between good alignment and good DASH scores, as well as with Michigan Hand Outcomes Questionnaire (MHQ) scores in patients younger than 60 years old. This correlation was lost in elderly patients, in which the functional outcome was not as dependent in the radiological measures as in the younger group.18
Jaremko et al obtained the same conclusion in their work. They studied patients older than 50 years; however, they did not find a significant statistical correlation between unacceptable radiological outcomes and DASH scores. On the contrary, they found a significant statistical correlation between radius malunions and low DASH scores (in patients older than 50 years).15 As with the same results, Grewal et al concluded in their 222-patient group that in patients younger than 65 years, radiological malunion was directly correlated with bad results (especially because of the radial shortening, in contrast to patients older than 65 years, in which this relationship was not found).14
A possible explanation of this poor correlation between radiological and functional outcomes in elderly patients is because of the low demand in this group.5
Our study does not show a correlation between the increase in upper limb disability and the decrease in wrist range of movement. Our study did not find a correlation between radiological measures and DASH scores as well. Other authors have also reached this conclusion as we can see in Table 1.15
In the same way, Grewal et al had published several papers in which they tried to study other patients’ characteristics that could affect the final outcome of the DRF treatment. They found that this complementary data significantly affect neither the disability nor the pain.14
The DASH questionnaire was filled in by the patients in the emergency room the same day of the injury; we did not find many studies in which baseline DASH is reflected, and this is an advantage of our study design.
We used the DASH questionnaire because it is the only available instrument transculturally adapted to Spanish. The DASH score has been shown to be a reliable and valid evaluation tool of outcome after DRF,5,22 but we might have obtained different results if we had had used another more specific instrument based on the site of the fracture or the type of injury.
There are some study limitations. First the DASH score may reflect disability related to upper extremity disorders other than the wrist, and we did not exclude the study patients with previous problems of shoulder or elbow problems. We did not specifically ask the patients about previous upper limb disorders, which would explain the unusually high score of DASH before fracture. Second, we might have a recall bias when we asked patients to refer to their state prior to the fracture; we do not have any other method to assess DASH score as DRF is an acute injury and there is no way to survey patients prior to an injury.
More prospective research using these types of instruments may be needed to study outcomes of conservative treatment of DRFs and to study which factors can be affected in these fractures treated conservatively. This could help determine which patients would benefit from a conservative treatment and which would not.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: The procedures and the experiments performed in this study respect the ethical standards in the Helsinki Declaration of 1975, as revised in 2000, as well as the national law.
Statement of Informed Consent: Ethical committee was contacted for the design of this study, and it was concluded that there was no need for ethical approval. All the patients included in the study approved by oral or written consent their participation, whenever their intimacy was preserved.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Anzarut A, Johnson JA, Rowe BH, et al. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29(6):1121-1127. doi: 10.1016/j.jhsa.2004.07.002 [DOI] [PubMed] [Google Scholar]
- 2. Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles’ fracture treatment. J Hand Surg Am. 1991;16(3):392-398. doi: 10.1016/0363-5023(91)90003-t. [DOI] [PubMed] [Google Scholar]
- 3. Arora R, Gabl M, Gschwentner M, et al. A comparative study of clinical and radiologic outcomes of unstable Colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23(4):237-242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 4. Barton T, Chambers C, Bannister G. A comparison between subjective outcome score and moderate radial shortening following a fractured distal radius in patients of mean age 69 years. J Hand Surg Eur Vol. 2007;32(2):165-169. doi: 10.1016/j.jhsb.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 5. Brogren E, Hofer M, Petranek M, et al. Relationship between distal radius fracture malunion and arm-related disability: a prospective population-based cohort study with 1-year follow-up. BMC Musculoskelet Disord. 2011;12(1):9. doi: 10.1186/1471-2474-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cardoso R, Szabo RM. Wrist anatomy and surgical approaches. Orthop Clin North Am. 2007;38(2):127-148. doi: 10.1016/j.ocl.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 7. Changulani M, Okonkwo U, Keswani T, et al. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32(1):1-6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868-1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Colles A. Historical paper on the fracture of the carpal extremity of the radius (1814). Injury. 1970;2(1):48-50. [DOI] [PubMed] [Google Scholar]
- 10. Fujii K, Henmi T, Kanematsu Y. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg. 2002;10(1):9-15. [DOI] [PubMed] [Google Scholar]
- 11. Gehrmann SV, Windolf J, Kaufmann RA. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421-429. doi: 10.1016/j.jhsa.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 12. Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25(6):535-543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 13. Goldhahn J, Angst F, Simmen BR. What counts: outcome assessment after distal radius fractures in aged patients. J Orthop Trauma. 2008;22(8)(suppl):S126-S130. doi: 10.1097/BOT.0b013e31817614a1. [DOI] [PubMed] [Google Scholar]
- 14. Grewal R, MacDermid JC, Pope J, et al. Baseline predictors of pain and disability one year following extra-articular distal radius fractures. Hand. 2007;2(3):104-111. doi: 10.1007/s11552-007-9030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jaremko JL, Lambert RGW, Rowe BH, et al. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62(1):65-72. doi: 10.1016/j.crad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 16. Jung H-W, Hong H, Jung HJ, et al. Redisplacement of distal radius fracture after initial closed reduction: analysis of prognostic factors. Clin Orthop Surg. 2015;7(3):377-382. doi: 10.4055/cios.2015.7.3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karnezis IA, Fragkiadakis EG. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84(7):967-970. doi: 10.1302/0301-620x.84b7.12673. [DOI] [PubMed] [Google Scholar]
- 18. Kumar S, Penematsa S, Sadri M, et al. Can radiological results be surrogate markers of functional outcome in distal radial extra-articular fractures? Int Orthop. 2008;32(4):505-509. doi: 10.1007/s00264-007-0355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laino DK, Tejwani N. Indications for operative fixation of distal radius fractures: a review of the evidence. Bull NYU Hosp Jt Dis. 2012;70(1):35-40. [PubMed] [Google Scholar]
- 20. Lichtman D, Bindra R, Boyer M, et al. The treatment of distal radius fractures. J Am Acad Orthop Surg. 2009;93(8):1-191. [DOI] [PubMed] [Google Scholar]
- 21. Lichtman DM, Bindra RR, Boyer MI, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93(8):775-778. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 22. MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2015;29(2):136-145. doi: 10.1016/j.jht.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 23. Mellstrand-Navarro C, Pettersson HJ. The operative treatment of fractures of the distal radius is increasing. Bone Joint J. 2014;96(7):963-969. doi: 10.1302/0301-620X.96B7. [DOI] [PubMed] [Google Scholar]
- 24. Nellans K, Kowalski E. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113-125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rosales RS, Delgado EB. Evaluation of the Spanish version of the DASH and carpal tunnel syndrome health-related quality-of-life instruments: cross-cultural adaptation process and reliability. J Hand Surg Am. 2002;27(2):334-343. doi: 10.1053/jhsu.2002.30059. [DOI] [PubMed] [Google Scholar]
- 26. Souer J-S, Lozano-Calderon SA, Ring D. Predictors of wrist function and health status after operative treatment of fractures of the distal radius. J Hand Surg Am. 2008;33(2):157-163. doi: 10.1016/j.jhsa.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 27. Warwick D, Alam M. (i) Anatomy of the carpus and surgical approaches. Orthop Trauma. 2011;25(5):317-323. doi: 10.1016/j.mporth.2011.07.010. [DOI] [Google Scholar]
- 28. Wilcke MKT, Abbaszadegan H, Adolphson PY. Patient-perceived outcome after displaced distal radius fractures. A comparison between radiological parameters, objective physical variables, and the DASH score. J Hand Ther. 2007;20(4): 290-298; quiz 299. doi: 10.1197/j.jht.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 29. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25(1):19-28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]



