Abstract
Unruptured intracranial aneurysms are common. Rupture is rare, but associated with considerable morbidity and mortality. Screening for unruptured intracranial aneurysms is indicated in certain patient populations, but many patients request screening outside of established guidelines. In addition, intracranial aneurysms may be discovered incidentally. The presence of an intracranial aneurysm has a negative effect for the patient seeking life insurance. This commentary provides a perspective on insurance underwriting in individuals with unruptured intracranial aneurysms and offers points for clinicians to consider when counseling patients seeking screening.
Insurance underwriting is the process of stratifying risk based on predictors of the insured outcome. For life insurance, the outcome is death. Populations with higher-risk profiles are either denied underwriting altogether or required to pay higher premiums than standard-risk populations. The presence of an unruptured intracranial aneurysm places a patient at risk for subarachnoid hemorrhage, an outcome associated with considerable morbidity and mortality. Current guidelines support the screening of patients who have 2 or more family members with intracranial aneurysms, a history of subarachnoid hemorrhage, or a genetic disease known to predispose to intracranial aneurysms.1 However, patients may also request screening for intracranial aneurysms when it is not necessarily indicated. In addition, aneurysms may be discovered incidentally on intracranial angiography studies obtained for unrelated clinical indications. Once an intracranial aneurysm is discovered, the patient and clinician are often faced with a complicated decision between monitoring vs repair, and an intervention may not always be favored.2 In addition to the anxiety associated with the discovery of an aneurysm, a patient seeking life insurance may also experience difficulty in obtaining policy underwriting because of the morbidity and mortality associated with rupture. To help clinicians understand the business side of this medical condition, informal industry interviews and email communications were conducted with leading insurance brokers to frame the issue from the standpoint of life insurance brokers. The underwriting guidelines from 10 major insurance companies (including the 2 largest life insurance companies in the United States) were incorporated into our analysis. Insurance brokers from each company were queried to develop an underwriting composite for intracranial aneurysm. Specific decision algorithms were not available for this commentary because of the proprietary nature of insurance underwriting policy. This brief commentary offers an underwriting perspective for clinicians with patients who have or request screening for unruptured intracranial aneurysms.
Assessing risk
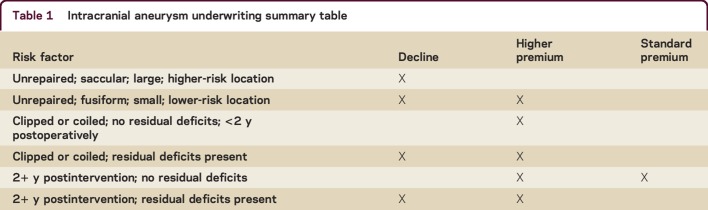
Although the presence of an intracranial aneurysm does not automatically disqualify a patient from obtaining life insurance, it has an adverse effect on underwriting (table 1). Insurance decisions take into account many of the risk factors associated with rupture, including the size, morphology, location, multiplicity, stability, and treatment history of the aneurysm, in addition to any associated neurologic deficits.3,4 Typically saccular aneurysms carry higher risk and are subject to substandard rates or denials. The location and number of aneurysms also affect the final underwriting decision. Multiple intracranial aneurysms or the presence of a genetic disease predisposing to aneurysm formation is likely to result in a decision to decline underwriting. Unrepaired aneurysms found in the circle of Willis and basilar artery are also more likely to result in a decision to decline. Aneurysms found to be enlarging on serial imaging studies are believed to have a higher likelihood of rupture and face adverse underwriting decisions. Comorbidities including tobacco dependence, cardiovascular disease, chronic obstructive pulmonary disease, and hypertension increase baseline risk.
Table 1.
Intracranial aneurysm underwriting summary table
A major consideration in life insurance underwriting is whether an unruptured intracranial aneurysm has been repaired and remained stable following repair. A repaired aneurysm without residual clinical deficits and follow-up vascular imaging demonstrating complete obliteration may qualify for standard rates after a year. There is recognition among insurance underwriters that endovascular coiling as a treatment for unruptured intracranial aneurysm does not always result in complete obliteration of the lesion. Such partially treated aneurysms also may be declined. Conversely, unrepaired intracranial aneurysms will be declined by most underwriters unless determined to be small, located anteriorly, and stable in size. There is no fixed definition of what constitutes a small aneurysm, but less than 7–10 mm is a typical cutoff. Aneurysms originating in the cavernous segment of the internal carotid artery are more favorable from an underwriting perspective. Aneurysm stability is usually understood to mean the absence of aneurysmal growth over a 2-year interval of surveillance.
Clinical implications
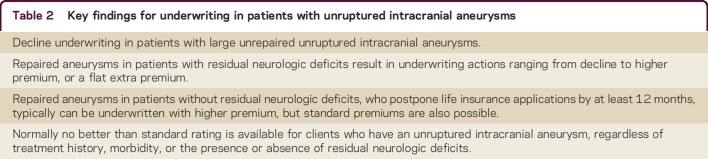
The personal, social, economic, and societal burden of living without life insurance has not been empirically studied, to our knowledge. The catastrophic nature of death (even if not untimely) is likely to impose both emotional and financial costs for dependents of the deceased. Although the decision to screen for intracranial aneurysms is a medical one, it has profound insurance implications and should be made in an informed capacity. Key points concerning the insurance implications of this decision are outlined in table 2. Ideally, a patient should be informed of the insurance risks before screening for intracranial aneurysms. In addition, the patient must be informed of the possibility that no treatment may be recommended even if an aneurysm is found, resulting in loss of insurability.2 When intracranial vascular imaging must be obtained for other indications, the insurance implications of incidentally discovered aneurysms should not bias clinical decision-making. Adherence to proper indications for intracranial vascular imaging will reduce the unintended negative insurance consequences of incidental findings. For example, specialty society guidelines have been developed to mitigate the adverse effects from discovery of incidental findings for patients with chronic headache disorders who request neuroimaging.5 To our knowledge, the prevalence of incidentally discovered unruptured intracranial aneurysm in non-guideline-based patient-initiated intracranial aneurysm screening requests is unknown. From an insurance underwriting perspective, if a patient anticipates a current or future life insurance need, it would be advisable to apply for life insurance coverage and complete insurance underwriting requirements prior to elective screening for the presence of an intracranial aneurysm. Once a life insurance policy has been issued, the rate is locked in and guaranteed for the duration of the policy. Thus, a potential health condition screened for, discovered, or developed after a life insurance policy has been issued are immaterial from an insurance perspective, and no increase in premium or loss of coverage will ensue. Ultimately, before electing to screen for the presence of an intracranial aneurysm, it would be advisable for patients to contact insurers for specific underwriting policies regarding the insurance implications of unruptured intracranial aneurysms.
Table 2.
Key findings for underwriting in patients with unruptured intracranial aneurysms
AUTHOR CONTRIBUTIONS
Eugene Scharf: design and conceptualization of the study, analysis and interpretation of the data, drafting and revising the manuscript for intellectual content. Sean Pelkowski: design and conceptualization of the study, analysis and interpretation of the data, drafting and revising the manuscript for intellectual content. Bogachan Sahin: analysis and interpretation of the data, drafting and revising the manuscript for intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
E. Scharf and S. Pelkowski report no disclosures. B. Sahin has received speaker honoraria from Medtronic and receives research support from New York State Department of Health Empire Clinical Research Investigator Program (ECRIP). Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Thompson BG, Brown RD Jr, Amin-Hanjani S, et al. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:2368–2400. [DOI] [PubMed] [Google Scholar]
- 2.Etminan N, Brown RD Jr, Beseoglu K, et al. The unruptured intracranial aneurysm treatment score: a multidisciplinary consensus. Neurology 2015;85:881–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morita A, Kirino T, Hashi K, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 2012;366:2474–2482. [DOI] [PubMed] [Google Scholar]
- 4.Wiebers D, Whisnant JP, Huston J, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:103–110. [DOI] [PubMed] [Google Scholar]
- 5.Mitsikostas DD, Ashina M, Craven A, et al. European Headache Federation consensus on technical investigation for primary headache disorders. J Headache Pain 2015;17:5. [DOI] [PMC free article] [PubMed] [Google Scholar]