Despite favourable outcome data [1], surgical stabilisation of severe rib fractures (SSRF) is employed in only the minority of cases of chest wall injuries [2]. One barrier to widespread adoption of this procedure is concern about the operative morbidity [3]. We recently reported our technique for open SSRF, which employs minimal incisions and muscle splitting whenever possible [4]. However, this technique (and any open technique) remains limited by 1) the need for longer skin incisions; 2) the need for partial division of the lattisimus dorsi and trapezius muscles at the extremes of exposure in some fracture patterns; 3) the need for scapular retraction to gain exposure to subscapular fractures; 4) plate placement on the outer cortex of the ribs, which may be palpable by thinner patients; 5) risk of pulmonary or cardiac injury from drilling and screwing in an internal direction; and 6) the inability to routinely visualise the pleural space (unless a thoracotomy is performed). Herein we describe a case of totally thoracoscopic, intra-pleural SSRF, including fixation to the inner rib cortex, a technique which addresses each of the aforementioned limitations of the open approach.
Case report
The patient is a 63-year-old man who fell on a sheet of ice while intoxicated. Past medical history was significant for non-insulin-dependent diabetes mellitus, hypertension, and alcohol abuse. He was brought in by ambulance alert, oriented, and with normal vital signs. Imaging with CXR, followed by CT chest, revealed a left hydro-pneumothorax and severely displaced lateral fractures of left ribs 6–9 (Fig. 1). Initial management involved regional analgesia with a percutaneous para-vertebral catheter (OnQ Silver Soaker®, 19 cm, 4.5F, Kimberly–Clark, Roswell, GA) and pulmonary toilet. The patient was offered SSRF based upon the fracture pattern of ≥ 3 contiguous fractures with bicortical displacement [4]. The patient agreed to proceed, and written informed consent was obtained.
Fig. 1.
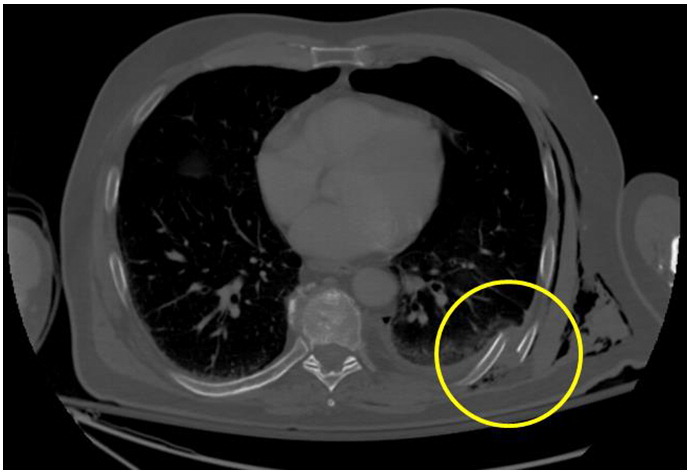
Pre-operative CT chest showing severely displaced left posterolateral 8th rib fracture.
The following day, the patient was taken to the operating room for SSRF. We began with flexible bronchoscopy, and scant bloody mucous secretions in the segmental bronchi were lavaged and suctioned. Prior to removing the bronchoscope, a 7-French, bifurcated bronchial blocking catheter (E-Z-blocker, Rusch/Teleflex Inc., Westmeath, Ireland) was passed under bronchoscopic vision with termination at the carina and inflation of the L main stem bronchus balloon with 12 cc of normal saline (Fig. 2). This effectively achieved left lung isolation. The patient was positioned in right lateral decubitus on a bean bag, with the left arm suspected by an airplane table attachment. Antimicrobial and VTE prophylaxis with intravenous cefazolin and subcutaneous heparin, respectively, were administered within 30 minutes prior to skin incision. A total of four, 10 mm port sites were used: 8th intercostal space, anterior axillary line; 6th intercostal space, posterior scapular line; 3rd intercostal space, mid-axillary line; and 8th intercostal space, posterior axillary line.
Fig. 2.
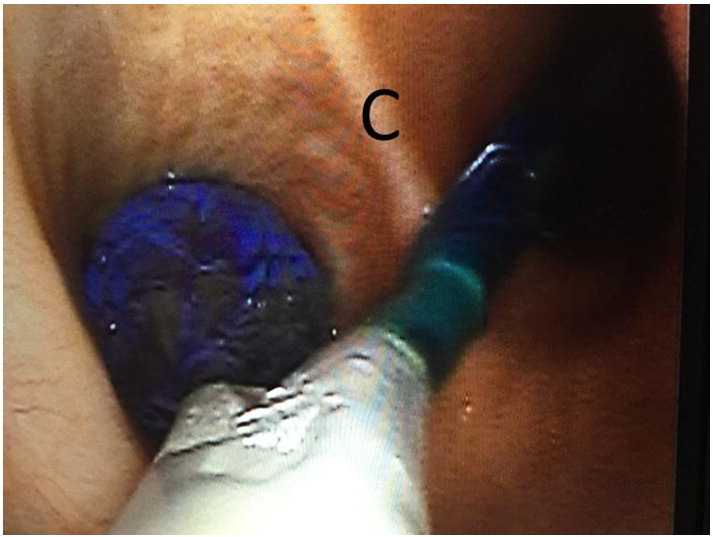
E-Z Blocker © Bronchial Blocker with left mainstem bronchus balloon inflated. C = carina.
Upon insertion of a 10 mm endo-eye camera (Olympus America Inc., Center Valley, PA), the rib fractures were readily identified. Approximately 150 cc of retained hemothorax was removed via suction. The rib fractures were then sequentially exposed by incising the overlying parietal pleura using a hand-held Bovie electrocautery device with a tip extender. Next, the fracture fragments were reduced by making a stab incision in the overlying skin with a no. 11 blade, and passing a no. 2 braided suture around each rib fragment using a Carter Thomason CloseSure suture passer (CareFusion, Inc., UK) under thoracoscopic visualisation. Two stab incisions were required to pass a total of eight sutures (two sutures around each of four rib fractures). The first assistant then pulled up on the sutures to reduce the fracture, and held tension on the suture to maintain reduction. Universal plates (MatrixRib, Depuy Synthes CMF, Inc., Westchester, PA) were then manually bent to match the concavity of the chest wall and introduced into the pleural space on a Kelley clamp though the posterior 8th intercostal space port. With the first assistant holding the sutures to maintain reduction and a second assistant holding the plate against the chest wall on the Kelley clamp, the surgeon introduced a 90° screw driver fashioned with a 12 mm drill bit (90° screwdriver, DePuySynthes CMF, Inc., West Chester, PA) through the anterior 8th intercostal space port. The camera was maintained through the subscapular port. A bicortical hole was then drilled starting with the inner cortex. After the first hole was drilled, a 12 mm screw was partially tightened using a 90° screwdriver. This achieved partial fixation of the plate to the chest wall. Then, using a Kelley clamp, the plate was rotated about the screw until it aligned securely along the rib fragments over all of the screw holes. The next five screws were then sequentially placed after drilling bicortical holes (Fig. 3). As this process was repeated for the lower rib fractures, we alternated between the two 8th intercostal space ports and the axillary port to achieve the best angle for both drill and screw placement. Following SSRF, a 24F straight tube thoracostomy was placed through the anterior 8th interspace port and terminated near the apex. Next, VATS intercostal nerve blocks were performed using 0.25% bupivacaine delivered through a 7 inch, 22 gauge needle. The immediate post-operative CXR is shown in Fig. 4.
Fig. 3.
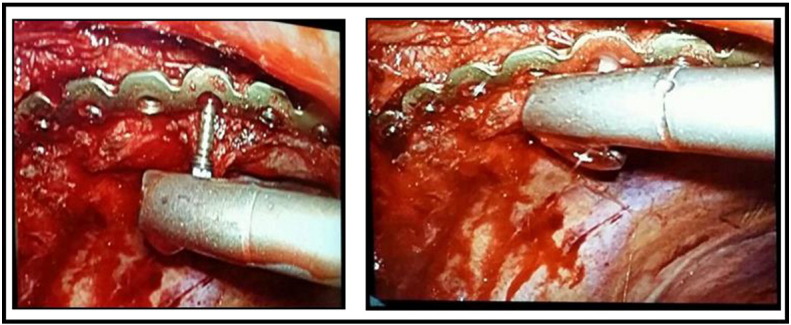
Intra-pleural screw placement using a 90° screwdriver inserted through a 2 cm, subscapular VATS port.
Fig. 4.
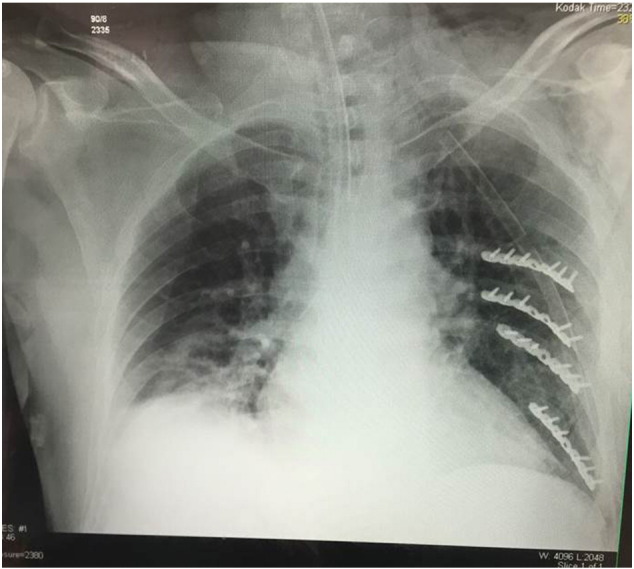
Immediately post-operative CXR showing intra-pleural plates with reversed screw direction.
Posteroperatively, the patient was monitored overnight for alcohol withdrawal in the surgical ICU. Pulmonary function remained stable; the tube thoracostomy was removed on post-operative day one and the patient was discharged home on post-operative day three. At 1 month outpatient clinic follow-up, the patient was off supplemental oxygen and recovering uneventfully.
Discussion
The management of severe rib fractures has plagued trauma surgeons for decades. A variety of techniques, including splinting the entire chest wall, mandatory mechanical ventilation, and epidural pain catheters, have all been in vogue at various times; yet the morbidity of diminished respiratory compliance and ventilation continues to result in atelectasis, pneumonia, chronic pain, and long ICU stays [5]. Despite an increase in the prevalence of SSRF, many trauma, orthopaedic, and thoracic surgeons remain sceptical of the procedure's efficacy. One recurrent concern involves the morbidity of the operation, particularly in patients with multiple high, subscapular fractures, as well as those with multiple fracture lines. Current operative approaches to SSRF range from a traditional posterolateral thoracotomy (with complete division of the latissimus dorsi muscle), to muscle sparring open techniques involving multiple longitudinal incisions, to VATS-assisted techniques that aid in both fracture identification and management of any potential intra-pleural processes (e.g., retained hemothorax)
Each of the aforementioned techniques is hindered by the necessity of both exposure of and fixation to the outer cortex of the rib. Exposure requires either muscle division or retraction, as well as the frequent need for painful scapular retraction. Furthermore, posterior exposure is often limited by articulation with the transverse process. Fixation to the outer cortex also involves drill and screw placement in an internal direction, which risks injury to intra-thoracic structures, ranging from pulmonary parenchymal injury causing an air leak to fatal cardiac injury. Finally, hardware on the outer cortex of the rib may be unpleasantly palpable in thinner patients. Similarly, rubbing of the inner cortex of the scapula against subscapular plates may cause chronic discomfort. Although VATS-assisted SSRF adds the benefit of assessment of the pleural space, it does not overcome the aforementioned limitations of fixation to the outer cortex of the rib. By contrast, a totally thoracoscopic SSRF, including fixation to the inner cortex, affords the opportunity to achieve effective reduction and stabilisation without the disadvantages of the current open approaches.
Potential downsides to the totally thoracoscopic approach that were brought to light by this particular case include 1) the inability to measure rib depth. This is a standard step in our open approach in order to ensure bicortical purchase and avoid termination of the screw tip in the lung parenchyma. However, bicortical purchase is readily appreciated by the two characteristic “gives” in drill resistance, the first representing the outer cortex and the second the inner cortex. A similar sensation was appreciated during this case when operating the 90° drill in the pleural space. Furthermore, the consequences of over-estimating screw length are minimised when fixation is to the inner cortex, as the excess screw length will terminate without consequence in overlying muscle. 2) Mechanical limitations of current fixation systems. Because existing fixation systems were not designed for intra-pleural operation, there are several limitations to their capabilities in this setting. The most obvious, as illustrated by this case, is the difficulty with which 90° purchase is possible on the inner cortex of the bone. Due to the concavity of the inner chest wall, both a drill and screwdriver with 180° articulating capabilities are ideally required and should be developed. In this case, approximation of 90° purchase was possible by switching between ports; however, this technique would be cumbersome in more severe fracture patterns. Similarly, existing pre-contoured plates all mimic the curve of the outer cortex; pre-contoured plates matching the concavity of the inner cortex would be helpful in minimising the time necessary to bend the plates intra-operatively. Finally, dropping and ultimately losing a screw in the pleural space could prove to be problematic. Although it did not happen in our case, it is certainly plausible that it would frequently complicate a prolonged VATS procedure. One potential solution to this problem would be a VATS intra-pleural magnetic pad that is placed over the collapsed lung (assuming magnetic screws). 3) Necessity for lung isolation. Single lung ventilation is not necessary in a purely open technique. However, contemporary means of lung isolation, such as the one described herein, add minimal time to the operation, particular if bronchoscopy is performed routinely. 4) Unfamiliarity with advanced thoracoscopic surgical techniques by Acute Care Surgeons. This limitation would be readily addressed by incorporation of the procedure into core competencies of Acute Care Surgery Fellowships.
Given the aforementioned limitations, we cannot presently recommend routine thoracoscopic SSRF. Pending refinements of both the technique and instrumentation, we currently recommend consideration of this technique in patients with relatively straightforward fracture patterns (e.g., ≤ 3 lateral fractures) and coexistent pleural pathology (e.g., retained hemothorax).
In conclusion, we report the first case of a successful totally thoracoscopic, intra-pleural SSRF. There are a number of potential advantages to this technique. However, as with any minimally invasive technique, successful adoption will depend upon refinements in equipment, technique, and outcomes data.
References
- 1.Leinicke J.A., Elmore L., Freeman B.D., Colditz G.A. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann. Surg. 2013;258:914–921. doi: 10.1097/SLA.0b013e3182895bb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dehghan N., de Mestral C., McKee M.D., Schemitsch E.H., Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462–468. doi: 10.1097/TA.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 3.Mayberry J.C., Ham L.B., Schipper P.H., Ellis T.J., Mullins R.J. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J. Trauma. 2009;66:875–879. doi: 10.1097/TA.0b013e318190c3d3. [DOI] [PubMed] [Google Scholar]
- 4.Pieracci F.M., Rodil M., Stovall R.T., Johnson J.L., Biffl W.L., Mauffrey C. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2015;78:883–887. doi: 10.1097/TA.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 5.Fabricant L., Ham B., Mullins R., Mayberry J. Prolonged pain and disability are common after rib fractures. Am. J. Surg. 2013;205:511–515. doi: 10.1016/j.amjsurg.2012.12.007. (discusssion 515–6) [DOI] [PubMed] [Google Scholar]


