Abstract
Introduction
South Australia (SA) has the highest notification rate of invasive meningococcal disease in Australia with the majority of cases due to serogroup B. Neisseria meningitidis is carried in the pharynx, with adolescents having the highest rates of carriage. A vaccine designed to offer protection against serogroup B (4CMenB) is licensed in Australia. The SA MenB vaccine carriage study aims to assess the impact of 4CMenB on carriage of N. meningitidis in adolescents.
Methods and analysis
This is a parallel cluster randomised controlled trial enrolling year 10, 11 and 12 school students (approximately 16–18 years of age) throughout SA, in metropolitan and rural/remote areas. Schools are randomised to intervention (4CMenB vaccination at baseline) or control (4CMenB vaccination at study completion) with randomisation stratified by school size and socioeconomic status, as measured by the Index of Community Socio-Educational Advantage (Australian Curriculum). Oropharyngeal swabs will be taken from all students at visit 1, and 12 months later from year 11 and 12 students. Students unvaccinated in 2017 will receive vaccine at the 12-month follow-up. Carriage prevalence of N. meningitidis will be determined by PCR at baseline and 12 months following 4CMenB vaccination and compared with carriage prevalence at 12 months in unvaccinated students. A questionnaire will be completed at baseline and 12 months to assess risk factors associated with carriage. The primary outcome of carriage prevalence of disease causing N. meningitidis at 12 months will be compared between groups using logistic regression, with generalised estimating equations used to account for clustering at the school level. The difference in carriage prevalence between groups will be expressed as an OR with 95% CI.
Ethics and dissemination
The study was approved by the Women’s and Children’s Health Network Human Research Ethics Committee (WCHN HREC). The protocol, informed consent forms, recruitment materials, social media and all participant materials have been reviewed and approved by the WCHN HREC and updated on ClinicalTrials.gov. Results will be published in international peer-reviewed journals and presented at national and international conferences. The study findings will be provided in public forums and to study participants and participating schools.
Trial registration number
ACTRN12617000079347. NCT03089086; Pre-results.
Keywords: epidemiology, public health, meningococcal disease, carriage, randomised controlled trial
Strengths and limitations of this study.
A parallel cluster randomised controlled trial will allow a causal determination of the impact of meningococcal B vaccine on oropharyngeal carriage of Neisseria meningitidis.
The primary outcome is an objective measure, laboratory confirmed PCR positivity, which is measured by one centralised laboratory.
This clinical trial will be the largest interventional population study of its kind.
Attrition of participants over the 12-month follow-up may compromise group comparisons.
Control and intervention students are independent but limited school mixing between schools may occur reducing the estimation of impact of 4CMenB on carriage.
Introduction
Neisseria meningitidis infection is an important cause of morbidity (~500 000–1 200 000 cases/year) and mortality (50 000–135 000 deaths/year) worldwide.1 2 Clinically, the most important serogroups are A, B, C, W, X and Y. The global serogroup distribution is dynamic over time and there are regional variations in disease epidemiology.3
Carriage of N. meningitidis
Exposure to N. meningitidis is common in the general population, leading to asymptomatic pharyngeal carriage that may be transient, temporary or long term. Age influences carriage, with a rapid rise from 15 years of age to a peak in carriage at around 19 years, likely due to increases in the number and closeness of social contacts.4 5 Other factors that influence carriage are male gender, concomitant or predisposing respiratory infections, active and passive smoking, and low socioeconomic status.6 Disease is a rare outcome of infection and the relationship between carriage and disease incidence is not fully understood.4 7 Given that carriage and transmission rates are significantly higher in adolescents than other members of the population and very low in infants, a reduction of carriage in adolescents has the potential to provide indirect protection to unvaccinated individuals, including infants.8
Epidemiology in Australia and South Australia
As in many countries, the incidence of invasive meningococcal disease (IMD) in Australia is highest in children under 1 year of age (3.7/100 000), followed by adolescents between the ages of 15 and 19 years (2.6/100 000).9 In 2016, 262 cases of IMD were notified nationally (1.1/100 000), with 28 notifications in South Australia (SA) including one death.10 SA has a population of 1.7 million and has the highest notification rate of IMD in Australia (1.65/100 000), with serogroup B predominating (n=23/28, 82%; 2016).10 The most common serogroup causing IMD nationally between 1999 and 2015 was serogroup B. In 2016, serogroup W notifications exceeded serogroup B notifications nationally (110 vs 93 cases, respectively).10
Meningococcal vaccines and herd protection
Since the early 2000s, countries that offer universal vaccination against meningococcal serogroup C (MenC) have seen a dramatic decrease in the incidence of serogroup C disease.11–13 Aligned to this, where adolescents have been targeted for vaccination, carriage of serogroup C in adolescents has reduced, resulting in indirect protection through reduced transmission and herd protection, with disease rates reduced across all age groups as a consequence.12 13 The ability of a meningococcal vaccine to impact colonisation and transmission of meningococci and, in turn, provide indirect effects through herd protection has important implications for evaluating the population impact and risk/benefit of the vaccine and for determining vaccine policy. As a result, there is high interest in assessing meningococcal B vaccines in relation to their impact on carriage, ideally in a large postlicensure population study.14
In Australia, 4CMenB is registered for use in persons ≥2 months of age for the prevention of invasive disease caused by serogroup B meningococci and is recommended by the Australian Technical Advisory Group on Immunisation for children <2 years of age and adolescents 15–19 years of age.15 However, 4CMenB is only available through purchase on the private market in Australia as it has not been included on the National Immunisation Program. The Pharmaceutical Benefits Advisory Committee, Commonwealth Government, which reviewed the cost-effectiveness of a meningococcal B vaccine programme in 2013, identified lack of data on effectiveness in a population programme (prior to implementation of the infant programme in the UK) and herd protection to inform cost-effectiveness estimates.16
In contrast to serogroups A, C, W and Y, the poor immunogenicity of the meningococcal serogroup B polysaccharide capsule, coupled with the marked genetic variability of the immunodominant serogroup B surface proteins, has prevented the development of a universal serogroup B vaccine. As the meningococcal B vaccines have been developed with novel technologies, their ability to induce herd protection is unknown.14 In Australia, based on the Meningococcal Antigen Typing System data, approximately 76% of 373 MenB isolates from invasive disease collected from 2007 to 2011 were predicted to be covered by this vaccine with the predicted coverage for SA at that time being 90%. A recent longitudinal study covering the past 15-year (2000–2014) history of meningococcal disease in Western Australia, a neighbouring state, indicates that although there was fluctuation over time in MenB vaccine coverage, the overall 15-year average remained high (60% with an annual range of 40% to 82%).17
Vaccine effectiveness in an infant 4CMenB population programme in the UK has been reported as 82.9% (95% CI 24.1 to 95.2).18
In the UK, a randomised, multicentre controlled study was conducted to examine carriage in university students 18–24 years old pre-vaccination and at serial follow-up points post-vaccination with 4CMenB.19 From 3 months after dose 2, 4CMenB vaccination resulted in significantly lower carriage of any meningococcal genogroup (18.2% (95% CI 3.4 to 30.8) carriage reduction) and 26.6% (95% CI 10.5 to 39.9) reduction in genogroups BCWY. A significant carriage reduction for disease-associated sequence types of capsular B meningococci compared with controls was not observed (12.6% (95% CI −15.9 to –34.1). This non-significant finding may in part be attributable to low acquisition of meningococcal strains, a low level of expression of vaccine antigens in carriage isolates, a slower-than-expected enrolment and limited vaccination prior to or during the period of maximal carriage acquisition.19
The SA MenB vaccine carriage study ‘B Part of It’ aims to assess the impact of 4CMenB on carriage of disease causing N. meningitidis by comparing carriage prevalence at 12 months post-implementation of a MenB vaccine programme in schools, with participating schools randomised to intervention or control.
Methods and analysis
Study design
This parallel cluster randomised controlled trial will measure the impact of 4CMenB on carriage prevalence in adolescents in SA. All 260 schools in metropolitan and rural/remote SA are invited to participate with immunisation provided through the school immunisation programme, managed by the Immunisation Branch, SA Health, in SA. For the purposes of the study, a school is defined as an educational institution at which students in years 10, 11 and 12 physically attend school during the week. Each school year level in SA has a cohort of 19 000–20 000 students aged approximately 16–18 years, with year 12 being the final year of school.
As carriage of the meningococcus is temporary and fluctuates over time and the adolescent years, a control group is essential to assess a causal relationship between the intervention, MenB vaccination and any change in carriage prevalence during this study. Two doses of 4CMenB will be given with a 2-month interval to all students attending school in years 10, 11 and 12. Individuals eligible to be enrolled into this study are South Australian secondary school students in years 10, 11 and 12 in 2017, who provide informed consent, are available at school for at least the first oropharyngeal swab and willing to comply with study procedures. Students are ineligible if they have previously received any doses of Bexsero (4CMenB) or had an anaphylactic reaction to any component of the vaccine or are known to be pregnant.
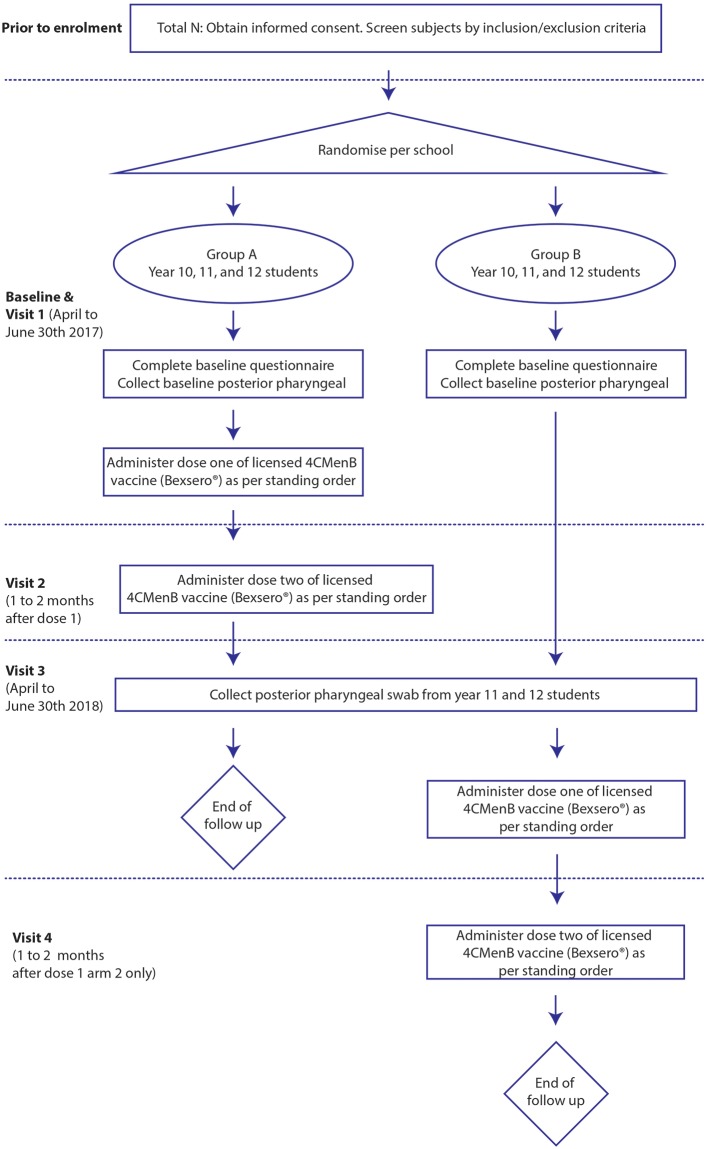
All students will undergo baseline oropharyngeal swab sampling, with schools randomised for students to receive either 4CMenB in 2017 (group A) or 4CMenB in 2018 (group B) (figure 1). The latter will receive 4CMenB at the 12-month follow-up swab visit. As follow-up swabs will only be available for year 10 and 11 students, the primary outcome is PCR positivity in year 10 and 11 students enrolled in the study. Year 12 students will undergo baseline posterior oropharyngeal swabs only. Year 12 students in group B will be offered 4CMenB vaccine in 2018 at designated immunisation clinics as the majority will have completed school in 2017. The advantages of conducting a study in school rather than university students include the opportunity to vaccinate prior to rapid carriage acquisition and the relatively closed accessible environment with an existing vaccination programme infrastructure. Year 12 students are included as they are likely to have the highest carriage rates and mixing of unimmunised year 12 students with immunised year 10 and 11 students could potentially reduce any vaccine impact on carriage.
Figure 1.
Study design.
Primary objective
Estimate the difference in overall carriage prevalence of disease causing genogroups of N. meningitidis (A, B, C, W, X, Y) following the 12-month pharyngeal swab in year 10 and 11 students who received two doses of Bexsero, compared with unvaccinated students.
Secondary objectives
Estimate the difference in carriage prevalence of each disease causing genogroup of N. meningitidis (A, B, C, W, X, Y) following the 12-month pharyngeal swab in year 10 and 11 students who received two doses of Bexsero, compared with unvaccinated students.
Estimate the difference in carriage prevalence of all genogroups of N. meningitidis following the 12-month pharyngeal swab in year 10 and 11 students who received two doses of Bexsero, compared with unvaccinated students.
Estimate the difference in acquisition (negative at baseline, positive at 12-month follow-up) of carriage of disease-causing genogroups of N. meningitidis (A, B, C, W, X, Y) over a 12-month period in students who received two doses of Bexsero, compared with unvaccinated students.
Estimate the difference in acquisition (negative at baseline, positive at 12-month follow-up) of carriage of all genogroups of N. meningitidis over a 12-month period in students who received two doses of Bexsero, compared with unvaccinated students.
Identify characteristics associated with carriage prevalence of all genogroups of N. meningitidis in South Australian school students at baseline and 12 months.
Identify characteristics associated with carriage prevalence of disease causing genogroups of N. meningitidis (A, B, C, W, X, Y) in South Australian school students at baseline and 12 months.
Randomisation
Randomisation will take place at the school level and will be stratified by school size (<60, 60 to 119, and ≥120 students per year level) and school socioeconomic status, as measured by the Index of Community Socio-Educational Advantage (ICSEA); (ICSEA <970, 970 to 1020, >1020).20 All schools agreeing to participate will be randomised to intervention (4CMenB vaccine) in 2017 or control (vaccination at the follow-up visit in 2018) (figure 1). The randomisation schedule will be generated by an independent statistician not otherwise involved in the study using Stata V.14. Schools and students will be unaware of their allocation to intervention or control until the day of the study immunisation provider visit. Laboratory personnel are blinded to assignment of intervention or control for the duration of the study.
Study processes
Immunisation providers will be trained in all aspects of the study processes, including collection of a posterior oropharyngeal swab, using a standardised technique. A flocculated swab will be wiped across the posterior oropharynx from one tonsillar area to the other and the swab placed immediately in STGG (skim milk, tryptone, glucose, glycerine; Thermo-Fisher Scientific Australia) transport medium.21 Swab vials will be labelled and placed in a portable cooler and delivered to the nearest SA Pathology collection centre.
School immunisation providers and the study team will approach all schools in SA to confirm their involvement in the study. Consent forms and information sheets will be sent home to parents and both parental consent and student assent will be obtained. Consent forms will be collected from the schools by the immunisation nurses, checked for completeness and data entered into the designated ‘B Part of It’ study web-based database established by Adelaide Health Technology Assessment (AHTA), The University of Adelaide.
Immunisation providers will explain the process of swab collection and immunisation to each student prior to any procedures being performed. All students will have an oropharyngeal swab taken and complete the risk factor questionnaire from 1 April to 30 June 2017. All group A students will be administered the first dose of 4CMenB (figure 1).
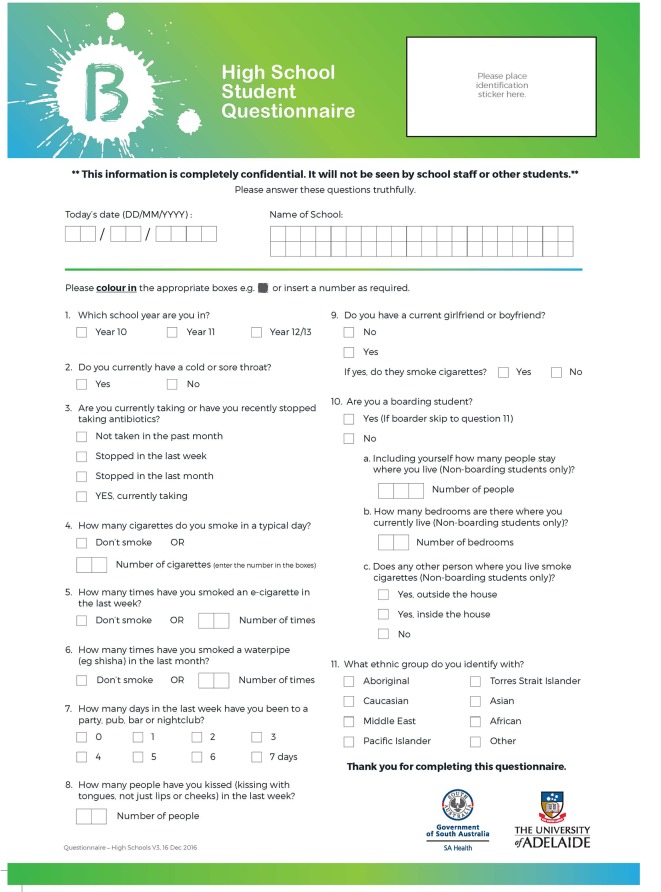
Participants will be asked to complete a one page de-identified questionnaire to collect information on characteristics that may be relevant to carriage of N. meningitidis (eg, smoking history, household size, recent antibiotic use) at each swab visit (figure 2). The questionnaire will be re-identified by subject number to link questionnaire data with carriage data.
Figure 2.
High school questionnaire.
Participants will be offered a A$20 iTunes card for completion of the questionnaire and oropharyngeal swabs to compensate them for their time. An SMS reminder will be sent 2 days prior to the school visits to notify parent/participants of the first and follow-up school visits
All collected data (student consent forms, questionnaires and swab analysis results) will be securely stored on a database held by AHTA, The University of Adelaide, with access to the database controlled by password protection. Range and logic checks will be performed on all collected data. Any data presented will be de-identified prior to presentation.
Patient and public involvement
The research question was developed in response to policy advisors’ recommendations. Study materials were reviewed by a Youth Advisory Group at several stages during study design. Feedback was also sought through social media including Twitter, Instagram, Facebook and enquires/feedback on the study website, early in development of the website. Student, parent and immunisation ambassadors will support awareness of the study and recruitment through schools.
The three Education Sectors (public, independent and Catholic schools) in SA will provide information to schools and support the study within schools. A communications officer will work with stakeholders on establishing appropriate and accessible avenues of communication. Involving students in the planning and delivery of communication strategies is expected to facilitate communication and provide opportunities for students to engage in research. A multimedia strategy will be overseen by the University of Adelaide, with the support of a public relations/communications company and SA Health. Key activities include website development (www.bpartofit.com.au),22 brand identity ‘B Part of It’, advertising and creation of supporting materials, ambassador engagement, public relations management and media training, social media strategy and amplification and bespoke content development. Study results will be provided to students through communication to schools and presentations at public forums. Results will also be reported in the media including television, radio and print media.
Study safety monitoring and surveillance
Vaccine safety will be monitored through the South Australian Vaccine Safety Surveillance, an enhanced passive surveillance system used for timely detection of signals suggestive of an increase in adverse events following immunisation. Serious adverse events (SAEs) considered possibly or probably related to administration of 4CMenB vaccine will be reported to the Research Ethics Committee, the study sponsor, the Therapeutic Goods Administration (Australian Government) and the vaccine manufacturer within 72 hours of the site becoming aware of the SAE. A study vaccine safety committee including independent vaccine safety experts has been established and will review all participant-reported safety data in accordance with a vaccine safety surveillance protocol.
Monthly summaries of all adverse events reported will be provided to the International Scientific Advisory Committee (ISAC) and the vaccine manufacturer. The ISAC has oversight of the study and has decision-making capacity over the scientific, technical and logistical aspects of study conduct.
Training of immunisation providers
Training for the study has been conducted in metropolitan Adelaide and major rural locations. A detailed training manual and standard medication order has been provided to all immunisation providers. Nurses are trained in and practice swab collection at the scheduled training days to ensure standardised and adequate posterior oropharyngeal swab collection technique. Schools will be randomly selected for monitoring of protocol-related study processes including throat swab technique.
Laboratory processes
On receipt of samples, DNA will be extracted using an automated extraction on the Roche MagnaPure system and subjected to PCR screening for the presence of specific meningococcal DNA (using PorA gene detection). Any samples yielding a positive PCR will be identified and cultured for Neisseria species on selective and non-selective agar and incubated overnight in CO2 at 35°C. Plates will be examined daily for isolates for up to 72 hours. N. meningitidis will be identified by standard diagnostic laboratory bacteriological methods using oxidase reaction and MALDI ToF with further PCR testing to determine the capsular group (A, B, C, W, X, Y).
Quantitative PCR will be applied to the positive screen samples for estimation of the density of carriage of the Neisseria species.23 A standard curve will be generated allowing comparison of crossing point values from the specimen analysis with the standard curve allowing the estimation of Neisseria density in the specimen. Samples will be stored long term in STGG broth at −80°C for future whole genome sequencing.24
Sample size and analysis plan
Students attending school have been chosen as the study population, as carriage of N. meningitidis increases from around 15 years of age4 and a funded programme for adolescents would likely be introduced in this age group. Study results will then predict the likelihood of indirect effects of 4CMenB in a national immunisation programme, which includes adolescents.
Consistent with previous published carriage rates in school students,25 26 we estimate the overall carriage prevalence in unvaccinated South Australian adolescents will be 6%–8%.
With around 80% uptake and 20% attrition, we anticipate 12 160 vaccinated and 12 160 unvaccinated year 10 and 11 students with a 12-month oropharyngeal swab. Assuming the carriage rate among the unvaccinated cohort is 8%, this sample size will provide 90% power to detect a 20% relative reduction in carriage to 6.4% in vaccinated participants (two tailed alpha=0.05). These calculations incorporate a design effect of 2.19, based on an average of 120 students per school providing 12-month swab data and an intraclass correlation coefficient estimate of 0.01 as reported in other studies involving students in schools.27 Should uptake or study completion be suboptimal, the study will still have 80% power provided that at least 8970 participants per arm contribute 12-month swab results.
All analyses will be undertaken according to a pre-specified statistical analysis plan. Available outcome data for students will be analysed according to the randomised group of their school (intention-to-treat principle). A sensitivity per-protocol analysis of the primary outcome will also be conducted in vaccine group students who followed a two-dose schedule of 4CMenB and control group students who did not receive 4CMenB before the 12-month follow-up.
The primary outcome of carriage of disease causing N. meningitidis genogroups detected by PCR at 12 months (yes/no) will be compared between groups using logistic regression, with generalised estimating equations (GEEs) used to account for clustering at the school level. The difference in carriage between groups will be expressed as an OR with 95% CI. Adjustment will be made for baseline carriage, randomisation strata (school size, ICSEA) and other baseline variables pre-specified for adjustment. Missing data on the primary outcome will be addressed using multiple imputation. All secondary outcomes will be compared between groups using logistic GEEs. In planned subgroup analyses of the primary and secondary outcomes, the effect of the 4CMenB vaccine will also be examined separately for metropolitan and rural schools and year 10 and year 11 students. Effect modification by these factors will be assessed separately by including an interaction term involving randomised group within each statistical model.
Discussion
This study is being conducted in SA which has (1) the highest IMD notification rate in Australia with a predominance of serogroup B, and (2) IMD notifications that are uniquely higher in adolescents than children. The predominant genotype over the past decade in SA is the B P1.7–2.4, which is the New Zealand epidemic strain and the PorA type contained in 4CMenB. While 4CMenB is available and recommended in Australia, uptake on the private market has been low and should not impact on baseline carriage rates.
It is feasible to conduct a large population study of this kind in SA due to the infrastructure and partnerships between the University of Adelaide, SA Health, the Women’s and Children’s Health Network, the National Health and Medical Research Council SA Academic Health Science and Translation Research Centre and Education sectors (Department of Education, Independent and Catholic Schools). The school immunisation programme that successfully delivers vaccines to adolescents supports the feasibility and potential high engagement in this study. We are cognisant of the risk of potential bias in having a control group with vaccination at study completion and potential for disproportionate withdrawal from this group; however, we will encourage continual involvement in the study and document any privately accessed vaccines in these individuals. We are also aware of the risk of interoperator variability in oropharyngeal swab collection in a study of this size. To mitigate this risk, all immunisation providers have been trained in a standardised technique for posterior oropharyngeal swab collection, which includes face-to-face training and unlimited access to a video outlining the swab collection technique.
As IMD is rare, the impact of the vaccine on carriage is an important component of cost-effectiveness analyses. This study will allow assessment of any association between the intervention and changes in carriage prevalence, to predict the likelihood of indirect effects of 4CMenB in reduction in disease in a national immunisation programme, which includes adolescents. A single 12-month time point for repeat oropharyngeal swabs has been chosen for a number of reasons including to void any seasonal variation in carriage prevalence and to ensure enough time to measure a vaccine effect but also to ensure such an effect is sustained in order to be confident about a herd immunity impact at a population level. This time point is approximately 10 months after the second dose of vaccine (12 months post first dose), with a previous vaccine effect shown 3 months after the second dose in the Read et al study.19 A single time point was chosen for feasibility reasons as 6 months post dose 2 would occur during the examination period and following holidays and there would likely be large numbers of students lost to follow-up. The timing of the swabs took into account the calendar year and avoided the busy periods where there would be competing priorities such as school commencement and other school immunisation programmes and enough time for parents and students to learn about the study and return consent forms and eligibility checklists for careful review by the immunisation nurses.
The question of the ability of any vaccine to provide indirect effects on the unvaccinated population (ie, herd protection) has important implications for vaccine policy. This is a particularly important question for meningococcal vaccines due to the unique epidemiology of asymptomatic pharyngeal carriage and more critically important for protein-based MenB vaccines, where limited information exists. High rates of serogroup B meningococcal disease, despite very low rates of carriage in infants, are likely explained by transmission from older age groups where carriage rates are relatively high. Understanding the potential impact of this vaccine on carriage in older age groups has important public health implications with the potential to inform worldwide policy on the implementation of adolescent MenB vaccination programmes.
This will be the first study to assess the impact of a large population 4CMenB programme on N. meningitidis carriage. Understanding any effects on carriage will assist Australian regulatory authorities and authorities in other countries in assessing the potential indirect effects to assist in the cost-effectiveness estimates of a MenB vaccine for inclusion in a national immunisation programme. A study to examine the impact of 4CMenB and MenB:fHBp (Pfizer) on carriage is planned for commencement in the UK in 2018 (personal communication Dr Matthew Snape, Oxford University). Carriage data will also inform the vaccine type and age group for implementation.8 In particular, it will be of interest to establish whether the remarkable herd protection effect seen with introduction of the conjugate meningococcal C vaccines is replicated for meningococcal B vaccine, 4CMenB.12 In addition, the data gathered in this study will be invaluable for the development of mathematical models to predict the outcome of a national 4CMenB immunisation programme.
Supplementary Material
Acknowledgments
B Part of It study team: Su-san Lee, Philippa Rokkas, Kathryn Riley, Christine Heath, Mary Walker, Bing Wang, Michelle Clarke, Sara Almond, Maureen Watson, Melissa Cocca. University of Adelaide: Sarah Scott, Lynette Kelly, Roberta Parshotam, Jamie Dunnicliff, Frances Doyle. Adelaide Health Technology Assessment team: Emma Knight, Andrew Holton, Primalie de Silva, Mark Armstrong, Tristan Stark, Scott Wilkinson. SA Pathology: Luke Walters, Mark Turra, Daryn Whybrow. Council immunisation providers: Berri Barmera Council, Booleroo Medical Centre, Broughton Clinic, City of Charles Sturt, Coorong District Council, Country Health SA Local Health Network, Eastern Health Authority, Health and Immunisation Management Services, Kadina Medical Associates, District Council of Karoonda East Murray, District Council of Lower Eyre Peninsula, District Council of Loxton Waikerie, Mallee Medical Practices, Mid Murray Council, City of Mitcham, Mount Barker District Council, Nganampa Health Council Inc., City of Onkaparinga, District Council of Peterborough, City of Playford, Pop Up Medics, City of Port Lincoln, Renmark Paringa Council, Royal Flying Doctors Service, Streaky Bay Medical Clinic, Tatiara District Council, City of Tea Tree Gully, District Council of Tumby Bay, Wakefield Plains Medical Clinic, City of West Torrens, Whyalla City Council, Watto Purrunna Aboriginal Primary Health Care Service, Wudinna District Council, District Council of Yankalilla. Reference Group: Don Roberton, Ann Koehler, Maureen Watson, Noel Lally, Paddy Philips, Monica Conway, Carolyn Grantskalns, Ann-Marie Hayes, Naomi Dwyer, Andrew Lawrence, Amo Fioravanti, Lyn Olsen, Alistair Burt, Sarah Robertson, Steve Wesselingh, David Johnson, Debra Petrys, Larissa Biggs, Tahlia Riessen. We acknowledge the assistance of members of the B Part of It Youth Advisory Group, the Women’s and Children Health Network Youth Advisory Group and the B Part of It study ambassadors.
Footnotes
Contributors: HSM wrote the first draft with assistance from MMcM. AK, AL, JMML, MCJM, MR, SNL, CT, RB, AF, TS, PR, CMK, JW and KV contributed to the manuscript and all authors approved the final version for publication.
Funding: This study was funded by GlaxoSmithKline Biologicals SA.
Disclaimer: This study was provided by GlaxoSmithKline Biologicals SA. The funder is independent of study management and analysis of the data. GlaxoSmithKline Biologicals SA was provided the opportunity to review a preliminary version of this manuscript for factual accuracy, but the authors are solely responsible for final content and interpretation. The authors received no financial support or other form of compensation related to the development of the manuscript.
Competing interests: HSM is supported by a NHMRC CDF APP1084951 and is a member of the Australian Technical Advisory Group on Immunisation, Australian Government. HSM is an investigator on vaccine trials sponsored by Industry (GSK, Novavax, Pfizer). HSM’s and MMcM’s institution receives funding for investigator-led studies from Industry (Pfizer, GSK). HSM and MMcM receive no personal payments from Industry. CT has received a consulting payment from GSK and an honorarium from Sanofi Pasteur. RB performs contract research on behalf of Public Health England for GSK, Pfizer and Sanofi Pasteur. PR is an investigator on vaccine trials sponsored by Industry (GSK, Novavax, Pfizer). PR’s institution receives funding for investigator-led studies from Industry (Pfizer, GSK, CSL). PR has been a member of scientific vaccine advisory boards for Industry (Pfizer, GSK, Sanofi) but has not received any personal payments from Industry. AF’s institution is in receipt of research funding from GlaxoSmithKline, Pfizer and consultancy fees from Alios BioPharma/Johnson & Johnson, BioNet-Asia and VBI Vaccines. AF is a member of the UK Department of Health’s Joint Committee on Vaccination, Chair of the WHO European Technical Advisory Group of Experts and President of the European Society for Paediatric Infectious Diseases, which receives sponsorship for its annual meeting from vaccine manufacturers. KV and JW are employees of the GSK group of companies and hold shares in the GSK group of companies as part of their employee remuneration.
Patient consent: Obtained.
Ethics approval: Women’s and Children’s Health Network Human Research Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: Trademarks: Bexsero is a trademark owned by GSK group of companies.
References
- 1. Chang Q, Tzeng YL, Stephens DS. Meningococcal disease: changes in epidemiology and prevention. Clin Epidemiol 2012;4:237–45. 10.2147/CLEP.S28410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jafri RZ, Ali A, Messonnier NE, et al. . Global epidemiology of invasive meningococcal disease. Popul Health Metr 2013;11:17 10.1186/1478-7954-11-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Halperin SA, Bettinger JA, Greenwood B, et al. . The changing and dynamic epidemiology of meningococcal disease. Vaccine 2012;30(Suppl 2):B26–36. 10.1016/j.vaccine.2011.12.032 [DOI] [PubMed] [Google Scholar]
- 4. Christensen H, May M, Bowen L, et al. . Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis 2010;10:853–61. 10.1016/S1473-3099(10)70251-6 [DOI] [PubMed] [Google Scholar]
- 5. MacLennan J, Kafatos G, Neal K, et al. . Social behavior and meningococcal carriage in British teenagers. Emerg Infect Dis 2006;12:950–7. 10.3201/eid1206.051297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caugant DA, Maiden MC. Meningococcal carriage and disease—population biology and evolution. Vaccine 2009;27(Suppl 2):B64–70. 10.1016/j.vaccine.2009.04.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Olsen SF, Djurhuus B, Rasmussen K, et al. . Pharyngeal carriage of Neisseria meningitidis and Neisseria lactamica in households with infants within areas with high and low incidences of meningococcal disease. Epidemiol Infect 1991;106:445–57. 10.1017/S0950268800067492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marshall H, Wang B, Wesselingh S, et al. . Control of invasive meningococcal disease: is it achievable? Int J Evid Based Healthc 2016;14:3–14. 10.1097/XEB.0000000000000048 [DOI] [PubMed] [Google Scholar]
- 9. Lahra MM, Enriquez RP. National Neisseria Network. Australian meningococcal surveillance programme annual report, 2015. Commun Dis Intell Q Rep 2016;40:E503–11. [PubMed] [Google Scholar]
- 10. The Department of Health. Invasive Meningococcal disease surviellance report. 2017. (cited 9 Jan 2017).
- 11. European Centre for Disease Prevention and Control. Annual Epidemiological Report 2016—Inasive meningococcal disease. 2016. https://ecdc.europa.eu/en/publications-data/invasive-meningococcal-disease-annual-epidemiological-report-2016-2014-data (cited 12 Jul 2017).
- 12. Maiden MC, Ibarz-Pavón AB, Urwin R, et al. . Impact of meningococcal serogroup C conjugate vaccines on carriage and herd immunity. J Infect Dis 2008;197:737–43. 10.1086/527401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Trotter CL, Maiden MC. Meningococcal vaccines and herd immunity: lessons learned from serogroup C conjugate vaccination programs. Expert Rev Vaccines 2009;8:851–61. 10.1586/erv.09.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harrison LH. Vaccines for prevention of group B meningococcal disease: not your father’s vaccines. Vaccine 2015;33(Suppl 4):D32–8. 10.1016/j.vaccine.2015.05.101 [DOI] [PubMed] [Google Scholar]
- 15. Immunise Australia Program: Australian Government. Australian Technical Advisory Group on Immunisation (ATAGI) Statement. Advice for immunisation providers regarding the use of Bexsero®. 2015. http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/atagi-advice-bexsero (cited 16 Aug 2016).
- 16. Australian Government Department of Health. Public summary document: multicomponent meningococcal group B vaccine, 0.5 mL, injection, prefilled syringe, Bexsero®. 2013. http://www.pbs.gov.au/info/industry/listing/elements/pbac-meetings/psd/2013-11/meningococcal-vaccine (cited 12 Jul 2017).
- 17. Mowlaboccus S, Perkins TT, Smith H, et al. . Temporal changes in BEXSERO® antigen sequence type associated with genetic lineages of Neisseria meningitidis over a 15-year period in Western Australia. PLoS One 2016;11:e0158315 10.1371/journal.pone.0158315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parikh SR, Andrews NJ, Beebeejaun K, et al. . Effectiveness and impact of a reduced infant schedule of 4CMenB vaccine against group B meningococcal disease in England: a national observational cohort study. Lancet 2016;388:2775–82. 10.1016/S0140-6736(16)31921-3 [DOI] [PubMed] [Google Scholar]
- 19. Read RC, Baxter D, Chadwick DR, et al. . Effect of a quadrivalent meningococcal ACWY glycoconjugate or a serogroup B meningococcal vaccine on meningococcal carriage: an observer-blind, phase 3 randomised clinical trial. Lancet 2014;384:2123–31. 10.1016/S0140-6736(14)60842-4 [DOI] [PubMed] [Google Scholar]
- 20. ACARA. My School; Guide to understanding ICSEA. Sydney: NSW Australian Curriculum Assessment and reporting Authority (ACARA), 2012. [Google Scholar]
- 21. Thors V, Morales-Aza B, Pidwill G, et al. . Population density profiles of nasopharyngeal carriage of 5 bacterial species in pre-school children measured using quantitative PCR offer potential insights into the dynamics of transmission. Hum Vaccin Immunother 2016;12:375–82. 10.1080/21645515.2015.1090069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The University of Adelaide. B Part of It. 2016. https://www.bpartofit.com.au/ (cited 12 Jul 2017).
- 23. Finn A, Morales-Aza B, Sikora P, et al. . Density distribution of pharyngeal carriage of meningococcus in healthy young adults: new approaches to studying the epidemiology of colonization and vaccine indirect effects. Pediatr Infect Dis J 2016;35:1080–5. 10.1097/INF.0000000000001237 [DOI] [PubMed] [Google Scholar]
- 24. Plikaytis BD, Stella M, Boccadifuoco G, et al. . Interlaboratory standardization of the sandwich enzyme-linked immunosorbent assay designed for MATS, a rapid, reproducible method for estimating the strain coverage of investigational vaccines. Clin Vaccine Immunol 2012;19:1609–17. 10.1128/CVI.00202-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fitzpatrick PE, Salmon RL, Hunter PR, et al. . Risk factors for carriage of Neisseria meningitidis during an outbreak in Wales. Emerg Infect Dis 2000;6:65–9. 10.3201/eid0606.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ingram SB, Wilson BJ, Kemp RJ, et al. . Neisseria meningitidis in a school population in Queensland. Med J Aust 1990;152:332. [DOI] [PubMed] [Google Scholar]
- 27. Killip S, Mahfoud Z, Pearce K. What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Ann Fam Med 2004;2:204–8. 10.1370/afm.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.