Abstract
Objective
To explore how persons experienced return to work (RTW) and their work situation 7 to 8 years after a stroke.
Design
An explorative qualitative design with individual interviews. The data analysis was inductive thematic and three researchers collaborated during the analysis process.
Participants
The study population included five women and eight men who had a stroke during 2009–2010, received care at the Sahlgrenska University Hospital in Gothenburg, Sweden and RTW after stroke and it was a heterogenic sample based on age, occupation, stroke severity and time to RTW.
Results
The analysis led to four themes; motivated and RTW while struggling with impairments, mixed feelings in the RTW process, still at work though restricted and social support for a sustainable work situation. The themes revealed that participants were motivated to RTW while struggling with impairments. The RTW process evoked mixed feelings of worry and grief over lost functions but also acceptance and gratitude for being able to work. Although maintaining work 7 to 8 years after experiencing a stroke, most were restricted in some way. Fatigue and cognitive impairments meant having to set limits, omit work tasks and rest at work, but also rest during free time and refraining from social activities in order to manage work. Participants avoided work-related stress if they could because of aggravated symptoms and/or fear of a new stroke. Support from supervisors and colleagues was often crucial for a sustainable work situation.
Conclusion
Maintaining work can be a continuous struggle with invisible impairments many years after a stroke. Strategies for managing work are dependent on each individual work situation, where support and understanding at work seem to be crucial for a sustainable work situation.
Keywords: stroke, qualitative research, rehabilitation medicine, stroke medicine, return to work
Strengths and limitations of this study.
The focus of this study was the perspective of persons who had worked for years since their stroke, but apart from having this in common, they represented a wide range of occupations, stroke characteristics and social backgrounds, gave rich interviews and contributed with experiences of maintaining work life after a stroke.
The patient perspective was integrated throughout the study as the interview guide was developed in cooperation with a patient representative from the Swedish Stroke Association, with whom a pilot interview was conducted, and further in the analysis process the participants were invited to a meeting to discuss and give feedback on the results (participant checking), which gave credibility to the interpretations.
A limitation of this study was that it only considered the perspective of persons who had return to work (RTW) after a stroke and did not include other stakeholders in the RTW process.
This study was performed in the Swedish context and the applicability of the results in other cultural contexts needs consideration.
Introduction
Return to work (RTW) is a term commonly used to refer to resumption of work by a person after a period of sick leave, although a broader view has been suggested to include the whole RTW process, from initial work disability to reaching one’s full potential at work.1 In Sweden, 25 000 to 30 000 people suffer one or the other form of stroke every year, of whom 20% are of working age, in which age group stroke has become more common in recent years.2 The reported rate of RTW between 1 and 3 years after a stroke varies globally from 50% to 74%,3–7 and two Swedish studies have found a RTW rate of 74%.6 7 In Sweden, employers have the most explicit responsibility of rehabilitation concerning their employees' RTW, although they share the responsibility with healthcare, the Social Insurance Office and the Employment Agency (EA). Employers are obliged to adapt work tasks, working hours, start work trials and make technical adjustments, though they are not forced to expand or create new work tasks. The common predictors for RTW in people with non-communicable diseases have been found to be higher socioeconomic status, higher self-efficacy, positive expectations of recovery, less severe illness, better RTW coordination and multidisciplinary interventions including the workplace.8 As regards the stroke, a less severe stroke and a good self-rated health have been reported to be positive predictors for RTW.4 Predictors for no RTW have been reported to be physical dependency at discharge,7 degree of residual disability,9 sick leave-7 or unemployment10 prior to stroke, low socioeconomic status,6 being an immigrant,10 comorbidities,10 older age5 and being female.3
A recent meta-synthesis of qualitative studies on RTW after stroke summarised important factors relative to RTW such as those related to rehabilitation services (availability, accessibility and appropriateness), the person (impairments, coping, adaptation and motivation) and the workplace (demands, adaptations, disability management, work climate and social support).11 Another qualitative study found that an awareness about invisible impairments generated support from employers and colleagues at work and resulted in a positive work experience, whereas the opposite presented a large barrier for RTW.12 A qualitative study suggested the importance of a coordinator for communicating information between stakeholders in the RTW process.13 Work has been found to be of importance for well-being and life satisfaction after a stroke,14 and RTW can be seen as a step towards striving for normality.12 Although many studies have investigated factors influencing return or no RTW after a stroke, only a few have looked at experiences of working in the long run after a stroke.
The aim of this study was to explore the experience of returning to work and maintaining work 7 to 8 years after experiencing a stroke.
Methods
Study design
This is an explorative qualitative study using individual interviews and inductive thematic analysis, which can be referred to a realist or essentialist paradigm.15 The Consolidated criteria for reporting qualitative research guidelines for reporting qualitative research were used.16
Patient and public involvement
The research questions were developed with the aim of learning more about the experiences of persons who had returned to work after having had a stroke. A patient representative from the Swedish Stroke Association was involved in the development and pilot testing of the interview guide. Patients were involved in the conduct of the study in form of individual interviews and also were invited to a meeting to hear the results and to discuss their interpretation with the authors. The preliminary results of the analysis have been communicated to the study participants in writing.
Participants
Participants were identified in the Extended Stroke Arm Longitudinal study at the University of Gothenburg. The inclusion criteria were having suffered an ischaemic or haemorrhagic stroke in the years 2009–2010, having received care at the Sahlgrenska University Hospital in Gothenburg, Sweden, residing in the Gothenburg urban area, being of working age (18–64 years) and having RTW after a stroke. Eighty-two persons were potentially eligible for our study and a letter including information about the purpose of the study, brief information about the clinical and research experience of the interviewer (AP) and information about the research team was sent out to a purposive sample of 37 persons to achieve a heterogeneous study population based on age, gender, occupation, stroke severity (NIH Stroke Scale (0–46)) and time to RTW. The letter was followed up by a telephone call by AP to confirm participation and to schedule interviews. If a person could not be reached by telephone, another letter was sent encouraging the person to make contact if he or she was interested in participating. Fourteen persons agreed to participate, but one was excluded due to not having RTW after stroke. The participants were asked to complete a form about demographics and employment. This is presented in table 1 together with data retrieved from medical charts.
Table 1.
Demographic and clinical characteristics of the study population
| Study population (n=13) | |
| Age, mean years (min–max) | 50 (39–64) |
| Gender: | |
| Female/Male | 5/8 |
| Country of birth: | |
| Sweden | 10 |
| Middle East or African country | 3 |
| Current living conditions: | |
| Living alone | 5 |
| Living with partner/ children | 3/5 |
| Type of stroke: | |
| Ischaemic stroke | 9 |
| Intracerebral haemorrhage | 4 |
| Stroke severity (NIH Stroke Scale): | |
| Mild (0 – 4) | 10 |
| Moderate (5–15) | 2 |
| Severe (16–46) | 1 |
| Stroke localisation: | |
| Right hemisphere | 4 |
| Left hemisphere | 3 |
| Bilateral | 1 |
| Not specified | 5 |
| Discharged from stroke unit: | |
| Discharged home / to rehab centre | 9/4 |
| Education: | |
| <9 years | 5 |
| 10 – 12 years | 3 |
| >12 years | 5 |
| Occupations: | |
| Accountant | |
| Assistant nurse | |
| Civil Engineer | |
| Cleaner (n=2) | |
| Commander on ferry | |
| Dentist | |
| Economist | |
| Police inspector | |
| Production worker | |
| Service technician | |
| Terminal worker | |
| Vehicle fitter | |
| Work-related characteristics: | |
| Time to RTW (period of full time sick leave) | Range: 2 months to 2 years |
| Same employer as before stroke | 11 |
| Lost job before RTW | 1 |
| Lost job after RTW | 1 |
| Percent of employment at the time of the interview: | |
| 100 % | 10 |
| 75 % | 2 |
| 50 % | 1 |
| Employment: | |
| Employed in public sector | 5 |
| Employed in private sector | 5 |
| Self-employed | 1 |
| Employed in sheltered work | 2 |
RTW, return to work.
Data collection
Individual face-to-face interviews were conducted by the first author (AP) who has a PhD in medicine, is a registered physiotherapist, has previous experience in performing qualitative studies, with no previous relation to the participants and is a woman with interest in work ability. A semistructured interview guide with open-ended questions was used and is presented in figure 1. The interview guide was discussed and revised in cooperation with a patient representative from the Swedish Stroke Association with whom it was first tested in a pilot interview. Thirteen interviews were performed during April to September 2017. Three took place in the participants’ homes and 10 at the rehabilitation medicine research unit facilities. On request of one participant, the interview was conducted in the presence of the next of kin who clarified answers due to language difficulties. The duration of interviews ranged from 40 to 90 min. All interviews were audio-recorded and transcribed verbatim by the first author (AP). No field notes were taken during the interviews. After 13 interviews, no new relevant knowledge was being obtained from new participants and hence data saturation was considered to be achieved.16
Figure 1.
The interview guide.
Data analysis
The transcribed interviews were analysed by inductive thematic analysis15 as described in table 2.
Table 2.
The steps of thematic analysis according to Braun and Clarke15
| Steps | Description |
| 1 | Familiarisation with data: transcribing, reading, re-reading, noting down initial ideas |
| 2 | Generating initial codes: coding interesting features across the entire data set |
| 3 | Searching for themes: collecting codes into potential themes, gathering all data relevant to each potential theme |
| 4 | Reviewing themes: checking if the themes work in relation to the coded extracts and the entire data set, generating a thematic map of the analysis |
| 5 | Defining and naming themes: ongoing analysis to refine the specifics of each theme |
| 6 | Producing the report: the final opportunity for analysis, selection of vivid, compelling extract examples, relating back of the analysis to the research question and literature, producing a report of the analysis |
First, the transcribed interviews were read and re-read by two of the authors (AP and MT). MT has a PhD (the first social worker with a PhD at the medical faculty) and more than 30 years of experience as a social worker with a knowledge of qualitative research methodology. The interviews were read separately by the two authors to familiarise themselves with the text and to obtain a sense of the whole study. In this process, initial codes were noted separately by the two authors. Second, the authors coded the interviews together and searched for potential themes. The themes were then reviewed and refined by all three authors together and differences were discussed until a consensus was reached, with the aim of enhancing the credibility of the analysis. The third author (KSS) is a MD, stroke specialist and professor in rehabilitation medicine with more than 25 years of clinical and research experience in neurological diagnoses. KSS contributed with stroke-specific knowledge in discussions concerning revising and refining the themes. The analysis process moved continuously back and forth between the whole and parts of the text to ensure the validity of the themes in relation to the data set. The study participants were invited to a meeting to hear the results and to discuss their interpretation with the authors. Examples of the coding process are provided in table 3.
Table 3.
Examples illustrating the coding tree
| Data extract | Code | Theme |
| [My boss says] “I see that you are tired, you need to rest. You need a break. Sit down there in the corner in my recliner and rest, I can see it in your eyes that you need a break, so I’m ‘shutting you down’ (like a machine) a little and I’ll keep working.” | Acknowledging symptoms and encouraging rest at work | Social support for a sustainable work situation |
| “They warned me that I’d be fatigued and stuff like that, but I thought I could handle it quite well with the gradual steps that I took. And there were planned rest days… And then the doctor said: people manage to start working pretty well, but it’s important that you have longer recovery times, that are not broken up.” | Experience of RTW at just the right pace | Motivated and returned to work while struggling with impairments |
RTW, return to work.
Results
Four themes were identified; motivated and RTW while struggling with impairments, mixed feelings in the RTW process, still at work though restricted, which includes two subthemes, and social support for a sustainable work situation (figure 2). The themes are illustrated with quotes from the participants.
Figure 2.
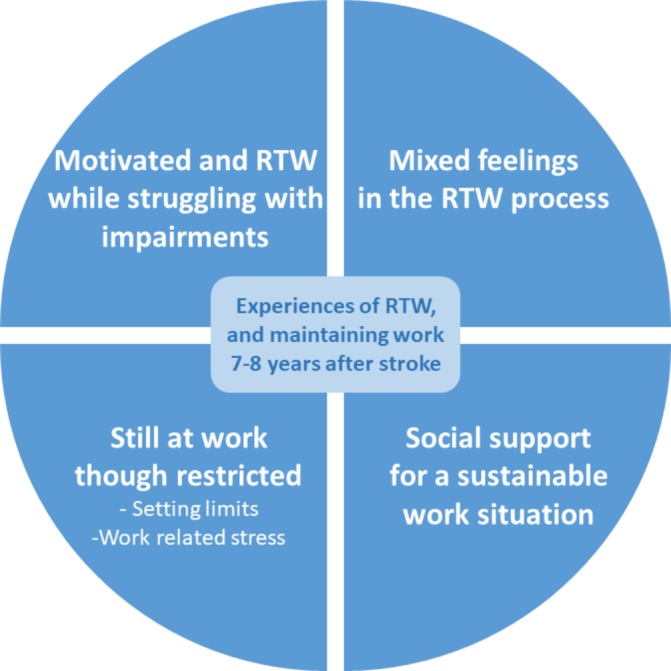
The themes and subthemes developed in the analysis. RTW, return to work.
Motivated and returned to work while struggling with impairments
Participants described a wide range of impairments that initially affected their RTW (table 4).
Table 4.
Impairments affecting work initially in the return to work process and 7–8 years after stroke, as expressed by participants
| Initial impairments | Residual impairments |
| Altered mental functions | |
| Disorientation in time | |
| Disorientation in space | |
| Lack of initiative | |
| Difficulties concentrating | Difficulties concentrating |
| Difficulties multitasking | Difficulties multitasking |
| Difficulties processing information and impressions | Difficulties processing information and impressions |
| Difficulties with numbers and letters | |
| Memory difficulties | |
| Depression | |
| Fatigue | Fatigue |
| Altered sensory functions and pain | |
| Sensitivity to sound | |
| Sensory loss and alterations | |
| Headache | Headache |
| Balance difficulties | Vertigo and balance difficulties |
| Altered neuromusculoskeletal functions | |
| Muscle weakness on one side of the body | Muscle weakness on one side of the body |
| Coordination difficulties | |
| Altered voice and speech functions | |
| Losing volume of voice | |
Full-time sick leave was prescribed for all participants and lasted from 2 months up to 2 years. Motivational factors for returning to work were an urge to leave the role of the sick person behind, regaining a meaningful daily activity, strong work ethics and work identity, economic needs and striving for normality.
The best rehabilitation for me has been starting to work again and getting away from the being sick part, and I wanted to get out and, like, meet people…. It was a way to start to function normally again. (a 39-year-old man)
All participants returned to work gradually in an individually adjusted pace and all of them except one person returned to their previous job, and that one person found a new full-time job. The RTW was sometimes too early or the gradual escalation was sometimes too rapid. This was related to high ambition in combination with impairments and resulted in setbacks, such as fatigue and emotional stress, which forced a backward step in the RTW process. This was frustrating, but manageable when focusing on striving forward in the RTW process. Experiences of RTW at just the right pace or later than appropriate were also reported. The participants in this case were restrained by doctors, work supervisors or family members, raising feelings of disappointment or discouragement, but also feelings of being cared for.
They warned me that I’d be fatigued and stuff like that, but I thought I could handle it quite well with the gradual steps that I took. And there were planned rest days… And then the doctor said:people manage to start working pretty well, but it’s important that you have longer recovery times that are not broken up. (a 58-year-old man)
In the RTW process, individual adaptations of work time, work tasks and the work environment were performed in partnership with the employer.
He [my boss] has given me a good room and good nurses and good support, so like, a lot of stuff around me, he has been up for making sure I have calm surroundings and a stable room and do not need to change between a bunch of different nurses, I have the same ones, so he’s been very supportive in that way… (a 57-year-old woman)
Work demands were adjusted by refraining from work tasks and responsibilities. Some found that there was no need for adaptation and were content with their work demands.
Mixed feelings in the RTW process
Uncertainty about consequences of stroke and prognosis of recovery raised worries about the future, including work life. Speculations about whether impairments were age- or stroke-related were expressed. Expectations of a fast recovery sometimes led to disappointment later when still struggling with impairments, or to satisfaction when the recovery rate turned out as expected. Some had been told by doctors that they would fully recover but when still struggling with impairments and work tasks 7–8 years after the stroke, they wondered how and when that would happen. However, a feeling of gratitude was evident in some participants for functioning well despite the stroke when considering how life might have turned out; they had been given a second chance in life and could work.
I’m happy to be able to work 75%, because I had a large stroke, so the idea that I’m able to work at all, that’s completely amazing. (a 57-year-old woman)
Acceptance of impaired functions as well as a more relaxed attitude towards work life were expressed. Participants described satisfaction with regained functions, but also frustration and grief over lost functions and disappointment at having been deprived of career opportunities.
Still at work though restricted
Seven to 8 years after the stroke, impairments were less obvious than initially post stroke, though most participants had impairments that still interfered with work (table 4).
Setting limits
Setting limits for colleagues, patients and customers to create opportunities for rest and undisturbed work was one strategy used to manage work demands. It was hard and time-consuming to shift focus and get back on track with their own work tasks after being disrupted by others, forcing participants to set limits for interaction with colleagues in order to focus on their own tasks. Limiting ambition was a way to avoid fatigue, and this could mean delegating work tasks or accepting a more subordinate work role. When demands on multitasking and information processing were too high, this could lead to confusion, insecurity and refraining from work tasks. Difficulties setting limits at work were experienced when expressed needs were not heard by supervisors or colleagues. Sometimes, participants chose not to participate in social activities at work due to fatigue, forced to focus on work tasks and nothing else.
Some days are a lot, and you get interrupted the whole time during your breaks and stuff…though I try and work around that by not going on break when everyone else does. Sometimes I’ve thought that my brain needs to rest a little, it’s fun to sit and chat with the others so I’m part of the group, but some days I feel… I want to take the opportunity to have a break when the others have gone so I can have a little bit of peace. (a 48-year-old woman)
When trying to keep up appearances to compete with colleagues, one participant avoided setting limits. However, some found it easier to set limits now than before their stroke, and they mentioned being able to stand up for themselves and knowing more about their rights.
Independent work was described as being allowed for work at their own pace, providing opportunities to prepare and plan work according to their own functional level. Fatigue was described as a dominant impairment that was coped with by taking pauses at work, which was allowed at some workplaces but not at others.
Then there’s the fatigue, if I’m going to have a more complicated meeting with a customer, or if I need to have a wage renegotiation meeting or performance review, I always have them in the morning. I always plan them for the mornings, because in the afternoon I get more fatigued, unfortunately. (a 45-year-old woman)
Gaining insight post stroke into the importance of taking care of their own health sometimes led to prioritising physical exercise in order to be able to function better at work. But finding the energy for exercise was sometimes impossible when they were stuck in the vicious circle of fatigue and work demands. Some described exercising less than before the stroke, due to the fear of a new stroke. Participants described an excessive need for rest, before and after work. Spare-time activities were often neglected due to lack of energy and were replaced by rest and sleep to manage work.
Before I had my stroke I had an allotment, so when I was finished at work I’d go and dig and do some work there. I rode my bike there. Now I just can’t manage it… I feel that things are different to before, but I want to live like that, like, I don’t want to push the limits, I want to try and live the way I am able to. (A 59-year-old man)
Work-related stress
Work demands of being constantly available to customers, patients or colleagues and a competitive work environment, lack of control over workload and irregular inflow of work created stress. Also, having to adjust to changing work schedules, being forced to work overtime or having to manage the same work demands as before stroke were stressful.
When exposed to stress at work, participants described having symptoms like the ones they had at stroke onset, such as sensations of numbness, tingling and headache, which gave rise to the fear of having a new stroke.
So every time you get a headache you start to think negatively, think if it’s another thing like that that is happening (a new stroke) … before I had the stroke, you could say I was very stressed out. But now I don’t stress as much. I think, nah, it will take the time it takes and not stress too much, it’s just that way. So, like at work right now, you work but not as intensively as you did before, and you have to think about your own health too. (a 46-year-old man)
The participants tried to avoid work-related stress but when this proved impossible, one of them started his own business to regain control over his workload. Others were forced to accept stress at work and endured recurrent symptoms such as headache, fatigue, vertigo or high blood pressure and felt trapped because of economic needs or were too exhausted to change jobs.
Social support for a sustainable work situation
Participants felt looked after and privileged when they were supported by their supervisor. A supervisor could advocate work task adaptations, acknowledge symptoms and encourage rest at work, or could accept flexible working hours.
[My boss says] I see that you are tired, you need to rest. You need a break. Sit down there in the corner in my recliner and rest, I can see it in your eyes that you need a break, so I’m ‘shutting you down’ (like a machine) a little and I’ll keep working. (A 48-year-old woman)
Some participants did not feel supported by their supervisor, who ignored them and their needs, which created a strenuous work situation. One supervisor gave mixed signals, both being supportive and setting unreasonable demands at the same time. One participant had been discouraged by the supervisor at a rehabilitation meeting but stood up against the supervisor and gained support that way. One participant felt actively discouraged by the supervisor and had the experience of the supervisor trying to force a resignation.
And she, my boss, doesn’t accept the doctor’s certificate but it’s, I don’t know what to say, they’re against me…In 2 weeks I’m going to work nights, but I…they want me to take the week off unpaid. Last time it was a late shift I took holiday leave… (A 59-year-old man)
Participants said that it felt safe to return to the same work team, and they got along well with colleagues when they could communicate openly and joke about their symptoms at work. When impairments did not interfere with work, some appreciated being treated like anyone else, but when impairments affected work, some appreciated to be relieved of work tasks and receive social support from colleagues.
Societal support could mean assistance from a labour union, the Swedish Social Insurance Agency or the EA in the RTW process. One could feel supported but also exposed by contact with these authorities.
Discussion
Findings
The analysis led to four themes revealing that participants were motivated to RTW while struggling with impairments in the RTW process. The RTW process evoked mixed feelings of worry and grief over lost functions but also acceptance and gratitude for being able to work. Although maintaining work 7–8 years after the stroke, most were restricted in some way. Fatigue and cognitive impairments meant having to set limits, omit work tasks and rest at work but also rest during spare time and omit social activities to manage work life. Participants avoided work-related stress if they could because of aggravated symptoms and/or fear of a new stroke. Support from supervisors and colleagues was often crucial for a sustainable work situation, but when not supported or even discouraged at work, it could mean a lonesome struggle enduring impairments and stress-related symptoms while pushing their limits to manage work demands.
Strengths and limitations
A strength of this study was that the interview guide was developed in cooperation with a patient representative from the Swedish Stroke Association with whom a pilot interview was conducted. Another strength was the heterogeneity of the study population, representing a wide range of occupations, stroke characteristics and social backgrounds. The participants gave rich interviews and contributed with a wide range of experiences. In the analysis process, two authors with different professional backgrounds (medical social worker and physiotherapist) coded separately and then jointly, ensuring a thorough coding process with the aim of capturing all relevant data. When developing, revising and refining themes, open discussions involving all three authors on coherency, consistency and distinctiveness led to a consensus, which contributed to the credibility of the study.15 When invited to a meeting (participant checking), participants gave feedback on the results, which were taken into account and gave further credibility to the interpretations. A limitation of this study was that it only considered the perspective of persons who had RTW after stroke and did not include other stakeholders in the RTW process. Also, this study was performed in the Swedish context and the application of results to other cultural contexts needs consideration.
Comparison with existing literature and guidelines
In this study, we gained a profound perspective of RTW from the point of view of persons with stroke who had managed to RTW and stay at work for many years. Work seemed to be important to the participants, who were all motivated to RTW. This can be interpreted in the light of previous findings stating work as an important part of life, identity and social context.17 Being motivated to RTW has also been found to be a facilitator for RTW after stroke from an employer perspective.18 However, high ambition in the RTW process could generate setbacks, as shown in this study. Disagreements with doctors, employers or family members could be a concern when readiness for RTW is uncertain, which has also previously been reported.19 The importance of achieving appropriate, gradual RTW in combination with formal adjustments provided by the employer needs to be addressed, as previously suggested.11
Although having successfully RTW and still working 7–8 years after stroke, life was often restricted for participants in this study. Setting limits at work, omitting leisure and social activities to meet an excessive need for rest, as well as trying to avoid work-related stress were central strategies used to manage work life, in line with previous findings.12 Consequently, this could mean prioritising work and rest, having no spare energy for other life activities. On the other hand, having gained a more relaxed approach to work after stroke, some participants prioritised well-being and leisure activities and were content with a less senior work role or with working part-time when possible. The importance of work for well-being and life satisfaction after stroke has been emphasised.14 We argue that maintaining work could be a continuous struggle many years after the stroke and the use and success of coping strategies are dependent on each individual’s work situation, where the question of support from employers has a great impact on working conditions.
Some felt supported by their employer and others did not, maintaining work life at the expense of their own well-being, which could lead to the risk of future resignation, as previously presented.12 Receiving no support from their employer could be related to difficulties in communicating impairments and adjustment needs, in particular when impairments were invisible, such as cognitive difficulties and fatigue. This could be a concern for managing work in the long run, as hidden impairments acting as key barriers for RTW has previously been suggested.11 Employers’ lack of medical knowledge, especially regarding cognitive impairments, could restrict them in making adequate adjustments.13 Apart from gaining stroke-specific knowledge from their employees, employers have used the internet as their primary source of information.18 Thus, the communication of impairments and need for adjustments to the employer seems crucial for receiving the support needed in the RTW process. To facilitate this communication, a stroke coordinator, who would support patients and stakeholders during the RTW process, has been suggested by other researchers.13 20
Clinical and policy implications
In this study, most participants had a mild stroke and were discharged from the hospital directly to their homes. Nevertheless, most still experienced cognitive impairments and fatigue that interfered with work life many years later. Cognitive impairments persisting for many years after stroke, also in people with mild stroke, have been presented previously.21 Further, cognitive function has been found to predict RTW in people with mild to moderate stroke,22 and although returning to work, people with mild stroke have been reported not being able to perform their jobs as previously due to cognitive impairments.23 However, cognitive rehabilitation interventions have received little focus in this group.22 24 In relation to this and the findings of our study, we suggest that more attention should be paid to rehabilitation of the invisible cognitive impairments experienced by people with mild to moderate stroke in the RTW process. However, a systematic review of RTW interventions found the evidence of effectiveness of cognitive rehabilitation by itself or along with work-directed interventions to be low for people with acquired brain injury.25
Based on the results of our study and previous findings, the strategies used to cope with invisible impairments in the RTW process after stroke seem to be essential.11 12 Development of strategies such as balancing activity and rest, setting limits and avoiding work-related stress could be supported by stroke rehabilitation teams. However, interventions for managing fatigue after stroke have insufficient evidence.26
It seems important to encourage patients to contact their workplace early in order to facilitate communication about their individual impairments and needs in the RTW process, to receive adjustments and social support from their employer. Rehabilitation meetings with the patient and involved stakeholders could be an avenue for such information sharing. In line with our suggestion, there is strong evidence for the effect of interventions including a combination of work-directed components and education and coaching on RTW.25
Future research
Investigating aspects of work life many years after stroke, quantitative studies or studies using mixed methods to combine patient perspectives with quantitative data on work stability, cognitive impairments and fatigue would add to the existing generalisable knowledge.
Randomised controlled trials focusing on strategies to cope with and communicate cognitive impairments and fatigue in the RTW process for persons with mild to moderate stroke are needed. Interventions could be based on strategies for managing work life after stroke as presented in this study.
Supplementary Material
Acknowledgments
The authors would like to thank Anders Andersson from the Swedish Stroke Association for collaboration in developing the interview guide. We would also like to express our gratitude to all participants for sharing their experiences. We would also like to thank Dr. Kate Bramley-Moore for language editing and translation assistance.
Footnotes
Contributors: AP, MT and KSS contributed to the design of the study. AP conducted and transcribed the interviews and analysed the data together with MT, involving KSS in the final stages of analysis. AP and MT wrote the first version of the manuscript, which was reviewed by KSS. All three authors contributed to and approved the final manuscript. This is an original article written by AP, MT and KSS. The manuscript is new and is not under consideration by any other journal. Each of the authors has contributed substantially to the manuscript.
Funding: The study was funded by the Swedish Research Council for Health, Working Life and Welfare (FORTE) (grant number 2016-00137), the Swedish Research Council, the Norrbacka-Eugenia foundation, Wilhelm and Martina Lundgren’s foundation, the Swedish Brain Foundation, the Swedish Heart and Lung Foundation and the Swedish Stroke Association.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The Regional Ethics Committee in Gothenburg, Sweden, on 5 June 2013 (Dnr: 400–13).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Due to ethical restrictions, data are available upon request. Interested researchers may submit requests for data to the authors (contact: ks.sunnerhagen@neuro.gu.se). Complete interview data cannot be made publicly available on ethical and legal grounds in compliance with the Swedish regulations (http://www.epn.se/en/start/regulations/). Public availability would compromise participant confidentiality or privacy. Upon request a list of condensed meaning units or codes can be made available after removal of details that may risk the confidentiality of the participants. To access such data please contact the first author: annie.palstam@gu.se.
References
- 1. Young AE, Roessler RT, Wasiak R, et al. . A developmental conceptualization of return to work. J Occup Rehabil 2005;15:557–68. 10.1007/s10926-005-8034-z [DOI] [PubMed] [Google Scholar]
- 2. Riksstroke. Yearly report (Acute-, TIA- and 3 month follow-up). 2015. www.riksstroke.org/wp-content/uploads/2015/12/Strokerapport_AKUT-TIA_LR.pdf
- 3. Hannerz H, Holbæk Pedersen B, Poulsen OM, et al. . A nationwide prospective cohort study on return to gainful occupation after stroke in Denmark 1996-2006. BMJ Open 2011;1:e000180 10.1136/bmjopen-2011-000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Larsen LP, Biering K, Johnsen SP, et al. . Self-rated health and return to work after first-time stroke. J Rehabil Med 2016;48:339–45. 10.2340/16501977-2061 [DOI] [PubMed] [Google Scholar]
- 5. Endo M, Sairenchi T, Kojimahara N, et al. . Sickness absence and return to work among Japanese stroke survivors: a 365-day cohort study. BMJ Open 2016;6:e009682 10.1136/bmjopen-2015-009682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Glader EL, Jonsson B, Norrving B, et al. . Socioeconomic factors' effect on return to work after first stroke. Acta Neurol Scand 2017;135:608–13. 10.1111/ane.12639 [DOI] [PubMed] [Google Scholar]
- 7. Westerlind E, Persson HC, Sunnerhagen KS. Return to work after a stroke in working age persons; a six-year follow up. PLoS One 2017;12:e0169759 10.1371/journal.pone.0169759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cancelliere C, Donovan J, Stochkendahl MJ, et al. . Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap 2016;24:32 10.1186/s12998-016-0113-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang YC, Kapellusch J, Garg A. Important factors influencing the return to work after stroke. Work 2014;47:553–9. 10.3233/WOR-131627 [DOI] [PubMed] [Google Scholar]
- 10. Virtanen M, Ervasti J, Mittendorfer-Rutz E, et al. . Work disability before and after a major cardiovascular event: a ten-year study using nationwide medical and insurance registers. Sci Rep 2017;7:1142 10.1038/s41598-017-01216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schwarz B, Claros-Salinas D, Streibelt M. Meta-synthesis of qualitative research on facilitators and barriers of return to work after stroke. J Occup Rehabil 2017. [DOI] [PubMed] [Google Scholar]
- 12. Balasooriya-Smeekens C, Bateman A, Mant J, et al. . Barriers and facilitators to staying in work after stroke: insight from an online forum. BMJ Open 2016;6:e009974 10.1136/bmjopen-2015-009974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hellman T, Bergström A, Eriksson G, et al. . Return to work after stroke: Important aspects shared and contrasted by five stakeholder groups. Work 2016;55:901–11. 10.3233/WOR-162455 [DOI] [PubMed] [Google Scholar]
- 14. Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. J Rehabil Med 2003;35:127–31. 10.1080/16501970310010475 [DOI] [PubMed] [Google Scholar]
- 15. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 16. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 17. Christiansen CH. Defining lives: occupation as identity: an essay on competence, coherence, and the creation of meaning. American Journal of Occupational Therapy 1999;53:547–58. 10.5014/ajot.53.6.547 [DOI] [PubMed] [Google Scholar]
- 18. Coole C, Radford K, Grant M, et al. . Returning to work after stroke: perspectives of employer stakeholders, a qualitative study. J Occup Rehabil 2013;23:406–18. 10.1007/s10926-012-9401-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gilworth G, Phil M, Cert A, et al. . Personal experiences of returning to work following stroke: an exploratory study. Work 2009;34:95–103. 10.3233/WOR-2009-0906 [DOI] [PubMed] [Google Scholar]
- 20. Öst Nilsson A, Eriksson G, Johansson U, et al. . Experiences of the return to work process after stroke while participating in a person-centred rehabilitation programme. Scand J Occup Ther 2017;24:349–56. 10.1080/11038128.2016.1249404 [DOI] [PubMed] [Google Scholar]
- 21. Ytterberg C, Dybäck M, Bergström A, et al. . Perceived impact of stroke six years after onset, and changes in impact between one and six years. J Rehabil Med 2017;49:637–43. 10.2340/16501977-2258 [DOI] [PubMed] [Google Scholar]
- 22. van der Kemp J, Kruithof WJ, Nijboer TCW, et al. . Return to work after mild-to-moderate stroke: work satisfaction and predictive factors. Neuropsychol Rehabil 2017;16:1–16. 10.1080/09602011.2017.1313746 [DOI] [PubMed] [Google Scholar]
- 23. O’Brien AN, Wolf TJ. Determining work outcomes in mild to moderate stroke survivors. Work 2010;36:441–7. 10.3233/WOR-2010-1047 [DOI] [PubMed] [Google Scholar]
- 24. Faux SG, Arora P, Shiner CT, et al. . Rehabilitation and education are underutilized for mild stroke and TIA sufferers. Disabil Rehabil 2018;40:1480–4. 10.1080/09638288.2017.1295473 [DOI] [PubMed] [Google Scholar]
- 25. Donker-Cools BH, Daams JG, Wind H, et al. . Effective return-to-work interventions after acquired brain injury: a systematic review. Brain Inj 2016;30:113–31. 10.3109/02699052.2015.1090014 [DOI] [PubMed] [Google Scholar]
- 26. Hinkle JL, Becker KJ, Kim JS, et al. . Poststroke fatigue: emerging evidence and approaches to management: a scientific statement for healthcare professionals from the American Heart Association. Stroke 2017;48:e159–e170. 10.1161/STR.0000000000000132 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.