Abstract
Over half of individuals infected with human immunodeficiency virus (HIV) suffer from HIV-associated neurocognitive disorders (HANDs), yet the molecular mechanisms leading to neuronal dysfunction are poorly understood. Feline immunodeficiency virus (FIV) naturally infects cats and shares its structure, cell tropism, and pathology with HIV, including wide-ranging neurological deficits. We employ FIV as a model to elucidate the molecular pathways underlying HIV-induced neuronal dysfunction, in particular, synaptic alteration. Among HIV-induced neuron-damaging products, HIV envelope glycoprotein gp120 triggers elevation of intracellular Ca2+ activity in neurons, stimulating various pathways to damage synaptic functions. We quantify neuronal Ca2+ activity using intracellular Ca2+ imaging in cultured hippocampal neurons and confirm that FIV envelope glycoprotein gp95 also elevates neuronal Ca2+ activity. In addition, we reveal that gp95 interacts with the chemokine receptor, CXCR4, and facilitates the release of intracellular Ca2+ by the activation of the endoplasmic reticulum (ER)-associated Ca2+ channels, inositol triphosphate receptors (IP3Rs), and synaptic NMDA receptors (NMDARs), similar to HIV gp120. This suggests that HIV gp120 and FIV gp95 share a core pathological process in neurons. Significantly, gp95’s stimulation of NMDARs activates cGMP-dependent protein kinase II (cGKII) through the activation of the neuronal nitric oxide synthase (nNOS)-cGMP pathway, which increases Ca2+ release from the ER and promotes surface expression of AMPA receptors, leading to an increase in synaptic activity. Moreover, we culture feline hippocampal neurons and confirm that gp95-induced neuronal Ca2+ overactivation is mediated by CXCR4 and cGKII. Finally, cGKII activation is also required for HIV gp120-induced Ca2+ hyperactivation. These results thus provide a novel neurobiological mechanism of cGKII-mediated synaptic hyperexcitation in HAND.
Author summary
Human immunodeficiency virus (HIV)-associated neurocognitive disorders (HANDs) occur in as many as 50% of individuals infected with HIV, including patients receiving combination antiretroviral therapy (cART). Notably, while neuronal death is mitigated with cART, neuronal dysfunction persists. This study investigates HAND-associated alteration of neuronal function, in particular, synaptic activity. The development of therapies designed to prevent HAND requires a detailed understanding of pathogenic mechanisms—processes difficult to study in humans. Here, we develop a feline immunodeficiency virus (FIV) model to study this question. FIV is genetically and functionally similar to HIV and produces a naturally occurring AIDS that is frequently associated with the development of neurological disease. We demonstrate that FIV and HIV share the core cellular pathway that alters neuronal activity via aberrant neuronal activation of cGMP-dependent protein kinase II. Thus, FIV infection of cats can be a valuable model to investigate the neurobiological mechanisms of HAND-associated neuropathogenesis.
Introduction
Human immunodeficiency virus (HIV)-associated neurocognitive disorders (HANDs) occur in as many as 50% of individuals infected with HIV, including patients receiving combination antiretroviral therapy (cART) [1]. HANDs range from mild neurological disorder (MND) and asymptomatic neurocognitive impairment (ANI) to severe and disabling dementia, and confer an increased risk of early mortality [1,2]. As cART enables individuals infected with HIV to survive to older ages, the prevalence of HAND continues to increase [1], and thus treatments targeting HIV’s pathological processes in the brain are greatly needed. Previous knowledge of HAND neuropathogenesis is dependent on studies that have been predominantly carried out in the pre-ART era [3]. In fact, the majority of basic research on HAND has been focused on evaluating neuronal damage in the context of active viral replication and outcomes related to encephalitis and neuronal death [3]. Despite suffering from HAND, in patients with cART, the classical features of HIV encephalitis and/or brain atrophy often are absent [4]. In fact, the severity of HAND is strongly associated with the loss of synaptic markers in patients on cART [5]. However, the molecular mechanisms underlying HAND-associated synaptic alteration remain largely unclear [6].
One of the major limitations in searching for HAND cures has been the lack of an animal model that recapitulates all of the features of HIV infection in humans [7]. Thus, new animal models to examine how chronicity and aging affect HIV-induced neuropathology are an important current and future need [8]. Previous work has heavily relied on rodent models for the study of HIV pathology [9]. However, results obtained in rodent models are often not easily translated to treatment of humans, given that rodents are not naturally susceptible to HIV infection and do not reflect the in vivo nature of infection [10]. Although nonhuman primates infected with simian immunodeficiency virus (SIV) or genetic chimeras of SIV and HIV have a number of important advantages over small-animal models, they have obvious disadvantages, including considerable genetic variation, that greatly complicate studies using small numbers of animals and high maintenance costs [7]. Moreover, SIV is unable to cause acquired immune deficiency syndrome (AIDS) in its natural host [11,12]. In contrast, feline immunodeficiency virus (FIV) infection in domestic cats represents an animal model of immunodeficiency and shares similarities in pathogenesis with that of HIV in humans [11–13]. Certain strains of FIV can infect the central nervous system (CNS), leading to neurological symptoms similar to those observed in some individuals infected with HIV [13,14]. Importantly, FIV is a naturally occurring virus inducing both AIDS and neurological complications in animal models [15]. Furthermore, the combination of HIV antiretroviral drugs on naturally infected FIV cats in the late phase of the asymptomatic state of the disease significantly reduces viral load, indicating a similar pathogenesis of these viruses [16]. Therefore, FIV infection of cats is an attractive model to study the chronic neuropathogenesis of HAND. Little is known, however, about neuronal mechanisms underpinning overlapping neuropathology between FIV and HIV.
Both HIV and FIV are tropic for lymphocytes and monocytes, utilizing CD4 (HIV) and CD134 (FIV) primary receptors together with the alpha chemokine receptor CXCR4 as a co-receptor to infect cells [17–19]. Even though lentiviral infection in the brain produces cortical and subcortical neuronal loss [20,21], HIV and FIV do not directly infect neurons but instead use a noninfectious interaction between the viral envelope and the neuronal surface [22,23]. Among HIV-induced neuron-damaging products, HIV envelope glycoprotein gp120 is one of the most prominent viral antigens found in the lysates of HIV-infected cells [24]. HIV gp120 indirectly and/or directly interacts with neurons, which enhances excitatory synaptic receptor activity, resulting in synaptic damages, but the mechanisms are not currently understood [25–27]. In neurons, the gp120 interaction with CXCR4 enhances Ca2+-regulating systems through NMDA receptors (NMDARs) in the synaptic membrane and inositol trisphosphate receptors (IP3Rs) in the endoplasmic reticulum (ER), resulting in apoptosis [28–34]. In addition, Ca2+ fluxes through NMDARs promoting the production of nitric oxide (NO) by neuronal nitric oxide synthase (nNOS), which is tethered by the scaffolding protein postsynaptic density 95 (PSD95) [35–39]. NO subsequently exerts its effects by activating cGMP-dependent protein kinase II (cGKII) through the production of cGMP [40]. Notably, the NMDAR-nNOS-cGK pathway has been implicated in HIV-induced neurotoxicity [41,42]. However, the exact cellular role of the pathway on synaptic dysfunction in HAND has not been determined.
We have shown previously that cGKII can phosphorylate serine 1756 in neuronal IP3Rs and increase ER Ca2+ release [43]. cGKII also phosphorylates the AMPA receptor (AMPAR) subunit GluA1, which triggers its synaptic trafficking, a critical step for inducing synaptic plasticity [43,44]. This suggests that cGKII activation is critical for HAND-associated synaptic dysfunction. Here, we demonstrate that FIV envelope glycoprotein, gp95, binds to CXCR4 on the neuronal plasma membrane and utilizes the same pathway as HIV gp120 to significantly increase intracellular Ca2+ activity and synaptic activity in neurons. Thus, our results indicate that FIV serves as a model for HAND-associated synaptic hyperexcitation. Most notably, our study reveals the inclusion of cGKII in both FIV gp95 and HIV gp120-induced Ca2+ hyperactivity, suggesting that cGKII inhibition may be a novel therapeutic target for HAND.
Results
FIV gp95-induced elevation of neuronal Ca2+ activity
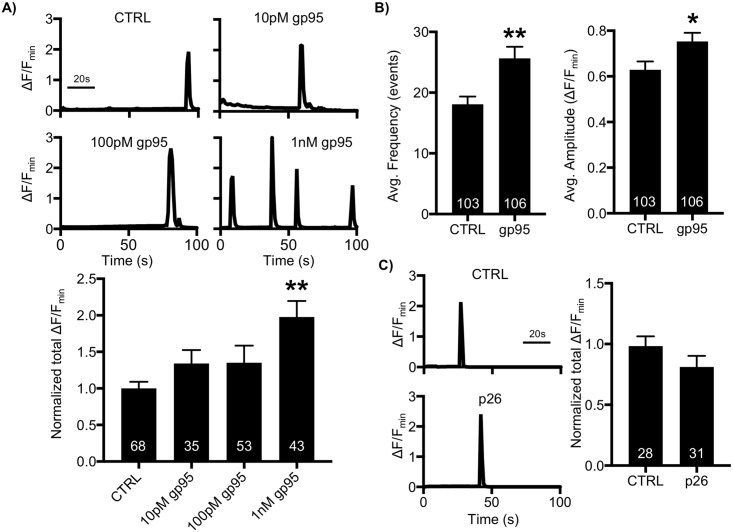
Neuronal Ca2+ is the second messenger responsible for transmitting depolarization status and synaptic activity [45]. These features make Ca2+ regulation a critical process in neurons, and thus altered Ca2+ activity in neurons is one of the major contributors to many neurological disorders, including HAND [45]. It has been found that HIV gp120 increases Ca2+ dynamics in neurons, contributing to neuronal dysfunction [28–34]. We thus hypothesized that FIV gp95 was able to enhance Ca2+ activity in neurons, as seen with HIV gp120. To test this idea, we measured Ca2+ activity in cultured mouse hippocampal neurons transfected with GCaMP5, a genetically encoded Ca2+ indicator, as described previously (S1 Fig) [43,46,47]. First, we acutely treated 12–14 day in vitro (DIV) neurons with 10-pM, 100-pM, and 1-nM gp95 and determined Ca2+ activity immediately after gp95 treatment (Fig 1A). We found active spontaneous Ca2+ transients in control cells (CTRL) and neurons treated with gp95 (Fig 1A). However, total Ca2+ activity in 1-nM gp95-treated cells was significantly higher than in controls (CTRL, 1 ± 0.09 ΔF/Fmin; gp95, 1.98 ± 0.22 ΔF/Fmin, p = 0.0001), confirming that 1-nM gp95 was sufficient to increase neuronal Ca2+ activity, while 10-pM (1.34 ± 0.18 ΔF/Fmin) and 100-pM gp95 (1.35 ± 0.23 ΔF/Fmin) slightly elevated Ca2+ activity but were not significantly different from control cells (Fig 1A). Importantly, the average frequency (CTRL, 18.05 ± 1.26 events; gp95, 25.65 ± 1.89 events, p = 0.001) and amplitude (CTRL, 0.62 ± 0.03 ΔF/Fmin; gp95, 0.73 ± 0.03 ΔF/Fmin, p = 0.018) were significantly elevated in gp95-treated neurons (Fig 1B). Next, we treated neurons with 700-nM FIV p26 capsid protein and found that p26 had no effect on neuronal Ca2+ activity (Fig 1C), suggesting that Ca2+ hyperactivity is caused selectively by FIV gp95.
Fig 1. FIV envelope glycoprotein gp95, not capsid protein p26, increases neuronal Ca2+ activity.
(A) Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in control, 10-pM, 100-pM, and 1-nM gp95-treated neurons showing that 1-nM gp95 treatment significantly increases neuronal Ca2+ activity (n = number of neurons, **p < 0.01, one-way ANOVA, uncorrected Fischer’s LSD, F (3,195) = 5.204, p = 0.0018). (B) Average frequency and amplitude of Ca2+ activity in control and gp95-treated neurons showing that gp95 elevates both frequency and amplitude of Ca2+ activity (n = number of neurons, *p < 0.05 and **p < 0.01, unpaired two-tailed Student t tests). (C) FIV capsid protein 700-nM p26 treatment has no effect on neuronal Ca2+ activity (n = number of cells). A scale bar indicates 20 seconds. FIV, feline immunodeficiency virus; LSD, Least Significant Difference.
Cellular pathway of gp95-induced Ca2+ overactivation
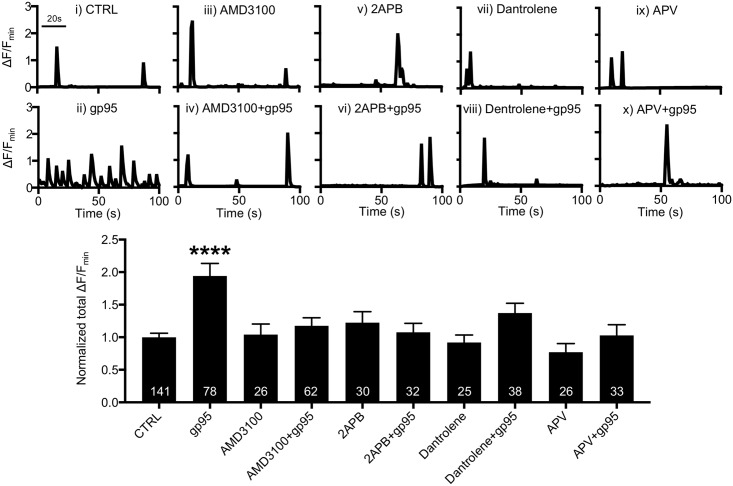
HIV gp120 interacts with CXCR4 on neurons, subsequently elevating intracellular Ca2+ through mobilizing ER Ca2+ [48], as well as by NMDARs [32]. Similarly, FIV gp95 also interacts with CXCR4 [18,49,50]. We thus hypothesized that HIV gp120 and FIV gp95 shared a core Ca2+ hyperexcitation pathway in neurons. Using GCaMP5, we confirmed that 1-nM gp95 was sufficient to increase Ca2+ activity compared with control neurons (CTRL, 1 ± 0.06 ΔF/Fmin; gp95, 1.94 ± 0.19; ΔF/Fmin p < 0.0001) (Fig 2i and 2ii). We used 200-nM bicyclam derivative plerixafor hydrochloride (AMD3100) to block the interaction between gp95 and CXCR4 and identified that AMD3100 treatment was sufficient to inhibit gp95-induced Ca2+ hyperactivity (1.18 ± 0.12 ΔF/Fmin, p < 0.0001) (Fig 2iv), while 200-nM AMD3100 alone had no effect on Ca2+ activity (1.04 ± 0.16 ΔF/Fmin) (Fig 2iii). This suggests that CXCR4 is required for the gp95 effects on Ca2+ activity. HIV gp120 binds to CXCR4, promoting ER Ca2+ release through a rapid hydrolysis of phospholipase C to generate IP3, which then activates ER Ca2+ channels, IP3Rs [51–53]. To confirm whether gp95 increased Ca2+ activity via IP3Rs, we treated neurons with 25-μM 2APB, an IP3R blocker and found that 2APB blocked the gp95-induced elevation of Ca2+ activity (1.08 ± 0.13 ΔF/Fmin, p < 0.0001) (Fig 2vi). However, 25-μM 2APB alone was unable to alter GCaMP5 activity (1.22 ± 0.17 ΔF/Fmin) (Fig 2v). Ryanodine receptors (RyRs) are another ER-associated Ca2+ channel [54]. To test whether RyRs were involved in gp95-induced Ca2+ hyperactivity, we treated neurons with 10-μM dantrolene, a RyR blocker, and found that inhibition of RyRs also abolished gp95 effects (1.37 ± 0.15 ΔF/Fmin, p = 0.0047) (Fig 2viii). Treatment with 10-μM dantrolene alone had no effect on Ca2+ activity (0.92 ± 0.11 ΔF/Fmin) (Fig 2vii). This suggests that the gp95-induced elevation of Ca2+ activity is dependent on ER Ca2+ release. Finally, we treated neurons with 1-nM gp95 and 50-μM DL-APV, a NMDAR antagonist, and found that 50-μM DL-APV completely inhibited GCaMP5 activity in both control and gp95-treated cells (DL-APV, 0.13 ± 0.04 ΔF/Fmin, p<0.0001; DL-APV+gp95, 0.1 ± 0.06 ΔF/Fmin, p < 0.0001) (S2 Fig). However, a lower dose of DL-APV (25 μM) was unable to affect basal Ca2+ activity (0.77 ± 0.13 ΔF/Fmin) (Fig 2ix). We thus used 25-μM DL-APV to avoid the inhibition of basal Ca2+ activity and directly assay the gp95 effects. Importantly, 25-μM DL-APV was sufficient to block gp95 effects (1.03 ± 0.16 ΔF/Fmin, p < 0.0001) (Fig 2x). This suggests that synaptic NMDAR activity is critical for gp95-induced Ca2+ overexcitation. Taking these data together, we confirm that gp95 interacts with CXCR4 and activates ER Ca2+ channels and synaptic NMDARs, enhancing neuronal Ca2+ activity, similar to HIV gp120.
Fig 2. Cellular pathway of gp95-induced Ca2+ hyperactivity.
Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp95, (iii) 200-nM AMD3100, (iv) 200-nM AMD3100 and 1-nM gp95, (v) 25-μM 2APB, (vi) 25-μM 2APB and 1-nM gp95, (vii) 10-μM Dantrolene, (viii) 10-μM Dantrolene and 1-nM gp95, (ix) 25-μM DL-APV, and (x) 25-μM DL-APV and 1-nM gp95, showing that the gp95-induced elevation of neuronal Ca2+ activity is dependent on CXCR4, IP3Rs, RyRs, and NMDARs (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (9,481) = 6.289). A scale bar indicates 20 seconds. AMD3100, bicyclam derivative plerixafor hydrochloride; IP3R, inositol triphosphate receptor; LSD, Least Significant Difference; NMDAR, NMDA receptor; RyR, Ryanodine receptor.
Gp95-induced Ca2+ hyperexcitation is dependent on cGKII-mediated IP3R activation
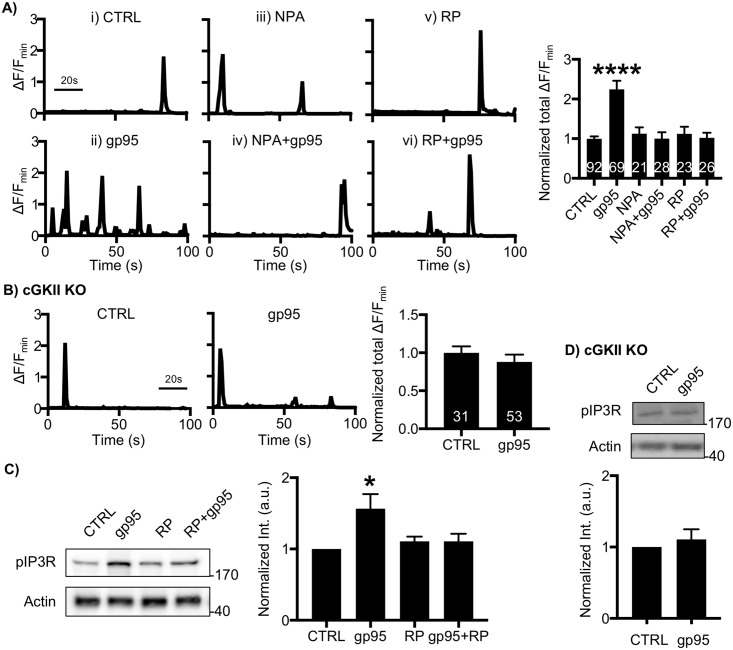
Ca2+ flux through the NMDAR-nNOS pathway activates cGKII by the production of cGMP [40]. We thus hypothesized that gp95 stimulated the NMDAR-nNOS pathway, leading to the activation of cGKII to phosphorylate IP3Rs, resulting in enhanced neuronal Ca2+ dynamics. Indeed, we found that inhibition of nNOS blocked gp95 effects on Ca2+ activity by treating neurons with 2-μM Nω-Propyl-L-arginine hydrochloride (NPA), a nNOS inhibitor (CTRL, 1 ± 0.06 ΔF/Fmin; gp95, 2.24 ± 0.21 ΔF/Fmin, p < 0.0001; NPA+gp95, 0.99 ± -0.16 ΔF/Fmin, p<0.0001) (Fig 3Ai, 3Aii and 3Aiv). Next, we tested the possibility that cGKII was a downstream effector of gp95. We found that gp95 was unable to increase Ca2+ activity when cGKII activity was blocked by treating neurons with 1-μM Rp8-Br-PET-cGMPS (RP), a cGKII inhibitor (1.02 ± 0.13 ΔF/Fmin, p < 0.0001) (Fig 3Avi). Notably, NPA or RP itself was unable to affect GCaMP activity (NPA, 1.12 ± 0.16 ΔF/Fmin; RP, 1.12 ± 0.16 ΔF/Fmin) (Fig 3Aiii and 3Av). We additionally cultured neurons from cGKII knockout (KO) animals as described previously [43] and confirmed that 1-nM gp95 had no effect on Ca2+ dynamics in KO neurons (CTRL, 1 ± 0.08 ΔF/Fmin; gp95, 0.88 ± 0.09 ΔF/Fmin, p = 0.39) (Fig 3B). This suggests that cGKII activation is required for gp95-induced Ca2+ hyperactivity. Significantly, cGKII can phosphorylate serine 1756 in neuronal IP3Rs (pIP3Rs), increasing Ca2+ currents in neuronal tissues [43,55]. We thus tested whether neuronal IP3R phosphorylation was altered by gp95 treatment. As expected, 1-nM gp95 treatment for 1 hour was sufficient to increase pIP3Rs, while RP by itself had no effect on IP3R phosphorylation (Fig 3C), consistent with elevated Ca2+ activity (Fig 3A). However, pharmacological inhibition of cGKII activity or genetic deletion of the cGKII gene abolished the gp95-mediated elevation of pIP3Rs (Fig 3C and 3D). In summary, gp95 interacts with CXCR4, promoting IP3 production and NMDAR-nNOS-cGKII-mediated IP3R phosphorylation, resulting in ER Ca2+ release.
Fig 3. Gp95-induced Ca2+ hyperactivity is mediated by nNOS-cGKII activation.
(A) Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp95, (iii) 2-μM NPA, (iv) 2-μM NPA and 1-nM gp95, (v) 1-μM RP, and (vi) 1-μM RP and 1-nM gp95 showing that nNOS activity and cGKII activity are required for gp95-induced Ca2+ hyperactivity (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (5,253) = 12.38). A scale bar indicates 20 seconds. (B) gp95 is unable to induce neurotoxic effects when the cGKII gene is deleted (n = number of neurons). A scale bar indicates 20 seconds. (C) Representative immunoblots and quantitative analysis of pIP3R(S1756) levels in each condition showing that gp95 treatment is able to increase pIP3Rs, which are dependent on cGKII activity (n = 4 experiments, *p < 0.05, one-way ANOVA, uncorrected Fischer’s LSD, F (3,20) = 3.795, p = 0.0264). (D) Representative immunoblots and quantitative analysis of pIP3R(S1756) levels in WT and cGKII KO neurons showing that gp95 treatment has no effect on IP3R phosphorylation (n = 4 experiments). cGKII, cGMP-dependent protein kinase II; IP3R, inositol triphosphate receptor; KO, knockout; LSD, Least Significant Difference; nNOS, neuronal nitric oxide synthase; NPA, Nω-Propyl-L-arginine hydrochloride.
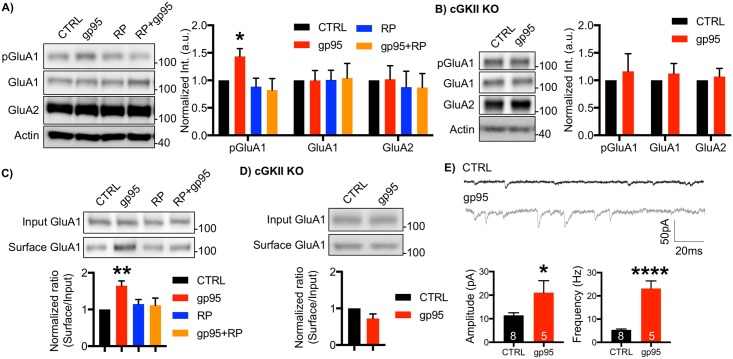
Gp95 increases surface expression of the AMPAR GluA1 subunit via cGKII activation
cGKII mediates phosphorylation of serine 845 of GluA1 (pGluA1), important for activity-dependent trafficking of GluA1-containing AMPARs, and increases the level of extrasynaptic receptors [43,44]. Moreover, cGKII-mediated GluA1 phosphorylation is critical for hippocampal long-term potentiation (LTP) and learning and memory [43,44]. As gp95 was sufficient to induce cGKII activation (Fig 3), we hypothesized that gp95-induced cGKII activation increased GluA1 phosphorylation, which led to enhanced AMPAR-mediated synaptic activity. To test this idea, we first biochemically measured GluA1 phosphorylation levels when gp95 was applied. Mouse cultured cortical neurons were treated with 1-nM gp95 for 1 hour, and synaptosomes were isolated as described previously [47] (S3 Fig). We found that gp95 treatment was sufficient to increase GluA1 phosphorylation, while total GluA1 and GluA2 levels were not affected (Fig 4A). To confirm whether such an increase was dependent on cGKII, we treated neurons with gp95 and 1-μM RP for 1 hour and measured pGluA1 levels. We revealed that inhibition of cGKII activity abolished the gp95 effects, while RP by itself was unable to affect AMPAR synaptic expression (Fig 4A). To further confirm the role of cGKII in the elevation of GluA1 phosphorylation, we used cGKII KO neurons and found that gp95 treatment had no effect on GluA1 phosphorylation in KO neurons (Fig 4B). Given that GluA1 phosphorylation promotes AMPAR surface expression, we next measured surface GluA1 levels by biotinylation after 1-nM gp95 was applied for 1 hour. We found that gp95 treatment increased surface GluA1 levels, which was blocked by pharmacological and genetic inhibition of cGKII (Fig 4C and 4D). Notably, cGKII inhibition by itself had no effect on GluA1 surface expression (Fig 4C). Furthermore, gp95 treatment was unable to alter GluA2 and NMDAR subunit NR1 surface expression (S4 Fig). This suggests that cGKII is required for gp95-induced GluA1 up-regulation. To further confirm whether such an increase in surface expression of AMPARs elevates AMPAR-mediated synaptic transmission, we measured miniature excitatory postsynaptic currents (mEPSCs) in DIV14-17 cultured mouse hippocampal neurons (Fig 4E). We found that acute treatment of 1-nM gp95 significantly increased both average mEPSC amplitude (CTRL, 11.45 ± 1.07 pA; gp95, 21.07 ± 5.06, p = 0.04) and frequency (CTRL, 5.35 ± 0.37 Hz; gp95, 23.17 ± 3.29, p < 0.0001) (Fig 4E). This suggests that gp95-induced activation of cGKII increases surface expression of AMPARs, contributing to enhanced synaptic transmission.
Fig 4. Gp95 increases surface expression of the AMPAR GluA1 subunit via cGKII activation.
(A) Representative immunoblots and quantitative analysis of the synaptosome fraction from cultured cortical neurons in each condition showing that gp95 is capable of elevating GluA1 S845 phosphorylation (pGluA1), which is mediated by cGKII (n = 3 experiments, *p < 0.05, one-way ANOVA, uncorrected Fischer’s LSD, F (3,22) = 3.884, p = 0.0228). (B) Representative immunoblots and quantitative analysis of the synaptosome fraction from cultured WT and cGKII KO cortical neurons showing that gp95 is unable to increase pGluA1 in cGKII KO neurons (n = 5 experiments). (C) Representative immunoblots and quantitative analysis of surface biotinylation in each condition showing that gp95 is able to increase surface GluA1 via cGKII activation (n = 6 experiments, *p < 0.05, one-way ANOVA, uncorrected Fischer’s LSD, F (3,20) = 3.839, p = 0.0254). (D) Representative immunoblots and quantitative analysis of surface biotinylation in WT and KO hippocampal neurons showing that cGKII is required for gp95-induced GluA1 surface trafficking (n = 5 experiments). (E) Representative traces of mEPSC recordings in control and gp95-treated neurons showing average mEPSC amplitude and frequency are significantly increased by gp95 treatment (n = number of neurons, *p < 0.05 and ****p < 0.0001, unpaired two-tailed Student t tests). AMPAR, AMPA receptor; cGKII, cGMP-dependent protein kinase II; KO, knockout; LSD, Least Significant Difference; mEPSC, miniature excitatory postsynaptic current.
Activity-dependent gp95 effects on AMPAR-mediated Ca2+ hyperactivity
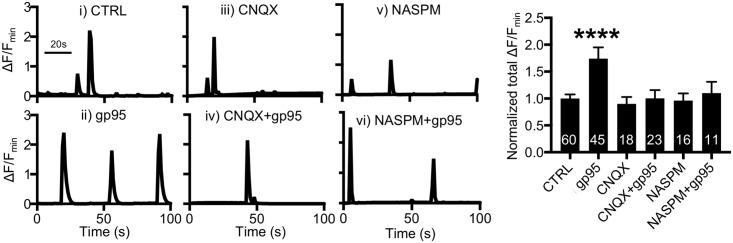
We next examined whether an elevation of AMPAR function was responsible for gp95-induced Ca2+ hyperactivity. We carried out Ca2+ imaging in the presence of an AMPAR inhibitor, 6-Cyano-7-nitroquinoxaline-2,3-dione (CNQX) (Fig 5). Treatment with 30-μM CNQX significantly blocked GCaMP5 activity in both control and gp95-treated neurons (S5 Fig). However, 10-μM CNQX alone had no effect on Ca2+ activity (0.9 ± 0.12 ΔF/Fmin) (Fig 5iii); thus, we used 10-μM CNQX to avoid the inhibition of basal Ca2+ activity and directly assay the gp95 effects. Notably, the gp95-induced increase in Ca2+ activity (CTRL, 1 ± 0.07 ΔF/Fmin; gp95, 1.74 ± 0.21 ΔF/Fmin, p < 0.0001) (Fig 5i and 5ii) was completely inhibited by treating neurons with a lower dose of CNQX (1.00 ± 0.15 ΔF/Fmin, p = 0.009) (Fig 5iv), suggesting that gp95-induced elevated AMPAR activity is required for Ca2+ hyperactivity. Notably, there are two general types of AMPARs formed through combination of the subunits, Ca2+-impermeable GluA2-containing and Ca2+-permeable, GluA2-lacking/GluA1-containing receptors [56]. Ca2+-permeable AMPARs (CP-AMPARs) are generally sensitive to polyamine block [57]. As we found that gp95 selectively elevated GluA1 surface expression (Fig 4 and S4 Fig), these AMPARs could be CP-AMPARs. We thus used 20-μM 1-naphthyl acetyl spermine (NASPM), an antagonist of CP-AMPARs, to determine if CP-AMPARs were responsible for the gp95-mediated Ca2+ hyperactivity. We found that 20-μM NASPM treatment was sufficient to block the gp95 effects on Ca2+ activity (1.10 ± 0.20 ΔF/Fmin, p = 0.02) (Fig 5vi), while NASPM alone was able to alter Ca2+ dynamics (0.96 ± 0.13 ΔF/Fmin) (Fig 5v). To further test whether the gp95 effects were dependent on neuronal activity, we treated neurons with 1-μM tetrodotoxin (TTX) and found that TTX treatment completely blocked GCaMP5 activity in both control and gp95-treated neurons (S6A Fig). Taking these data together, FIV gp95-induced Ca2+ hyperexcitation is dependent on AMPAR- and NMDAR-mediated neuronal activity.
Fig 5. Activity-dependent gp95 effects on AMPAR-mediated Ca2+ hyperactivity.
Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp95, (iii) 10-μM CNQX, (iv) 10-μM CNQX and 1-nM gp95, (v) 20-μM NASPM, and (vi) 20-μM NASPM and 1-nM gp95, showing that CP-AMPARs are required for gp95-induced Ca2+ hyperactivity (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (7,179) = 12.1). A scale bar indicates 20 seconds. AMPAR, AMPA receptor; CNQX, 6-Cyano-7-nitroquinoxaline-2,3-dione; CP-AMPAR, Ca2+-permeable AMPAR; LSD, Least Significant Difference; NASPM, 1-naphthyl acetyl spermine.
FIV gp95-induced Ca2+ hyperactivity in cultured feline hippocampal neurons
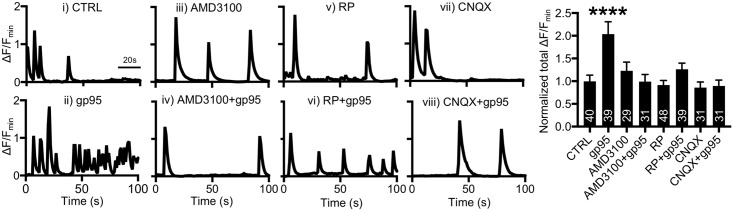
We next examined gp95-induced Ca2+ overactivation in cultured feline neurons. We first treated 14–16 DIV cultured feline hippocampal neurons with 1-nM gp95 and determined Ca2+ activity. Consistent with the findings in cultured mouse neurons (Fig 1A), total Ca2+ activity in 1-nM gp95-treated feline cells was significantly higher than in controls (CTRL, 1 ± 0.13 ΔF/Fmin; gp95, 2.03 ± 0.27 ΔF/Fmin, p < 0.0001) (Fig 6i and 6ii), indicating that 1-nM gp95 was also capable of increasing neuronal Ca2+ activity in feline neurons. To determine whether CXCR4 was involved in the gp95 effect on cat neurons, we treated neurons with 200-nM AMD3100, which was sufficient to inhibit gp95-induced Ca2+ hyperactivity (0.99 ± 0.15 ΔF/Fmin, p < 0.0001) (Fig 6iv). We also treated neurons with 10-μM RP and revealed that inhibition of cGKII was sufficient to block gp95 effects (1.26 ± 0.12 ΔF/Fmin, p < 0.0001) (Fig 6vi). This confirms that cGKII activation is also required for gp95-induced Ca2+ hyperactivity in feline neurons. We finally inhibited AMPAR function by treating neurons with 10-μM CNQX and revealed that gp95 was unable to elicit Ca2+ overactivation when AMPARs were inhibited (0.89 ± 0.13 ΔF/Fmin, p < 0.0001) (Fig 6viii). Notably, inhibitors by themselves had no effect on Ca2+ activity in feline neurons as well (AMD3100, 1.22 ± 0.19 ΔF/Fmin; RP, 0.91 ± 0.1 ΔF/Fmin; CNQX, 0.85 ± 0.12 ΔF/Fmin) (Fig 6iii, 6v and 6vii). This suggests that FIV gp95 is also sufficient to induce activity-dependent Ca2+ hyperexcitation in cultured feline neurons.
Fig 6. Gp95-induced Ca2+ hyperactivity in feline cultured hippocampal neurons.
Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp95, (iii) 200-nM AMD3100, (iv) 200-nM AMD3100 and 1-nM gp95, (v) 10-μM RP, (vi) 10-μM RP and 1-nM gp95, (vii) 10-μM CNQX, and (viii) 10-μM CNQX and 1-nM gp95, showing that the gp95-induced Ca2+ hyperactivity in cat hippocampal neurons is dependent on CXCR4, cGKII, and AMPARs (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (7,260) = 5.296). A scale bar indicates 20 seconds. AMD3100, bicyclam derivative plerixafor hydrochloride; AMPAR, AMPA receptor; cGKII, cGMP-dependent protein kinase II; CNQX, 6-Cyano-7-nitroquinoxaline-2,3-dione; LSD, Least Significant Difference.
cGKII activation is required for HIV gp120 and SDF-1-induced Ca2+ hyperactivity
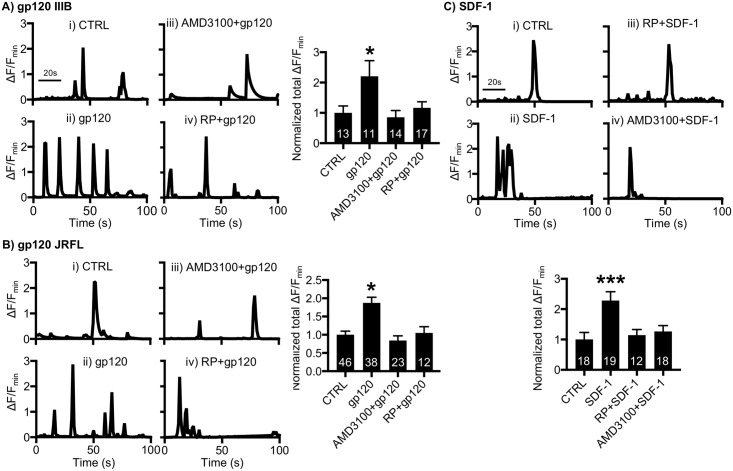
We finally investigated whether cGKII activation was required for HIV gp120-induced Ca2+ hyperactivity. We treated 12–14 DIV cultured mouse hippocampal neurons with 1-nM CXCR4-tropic gp120 (IIIB) and determined Ca2+ activity (Fig 7A). As expected, total Ca2+ activity in gp120-treated cells was significantly higher than in controls (CTRL, 1 ± 0.22 ΔF/Fmin; gp120 (IIIB), 2.20 ± 0.51 ΔF/Fmin, p = 0.0075) (Fig 7Ai and 7Aii), consistent with previous findings [27, 58]. Furthermore, 200-nM AMD3100 treatment was sufficient to inhibit gp120-induced Ca2+ hyperactivity (0.85 ± 0.22 ΔF/Fmin, p = 0.0025) (Fig 7Aiii), confirming that CXCR4 is required for gp120-induced Ca2+ overexcitation. Importantly, neurons treated with 1-μM RP and gp120 together exhibited no increased Ca2+ activity (1.16 ± 0.20 ΔF/Fmin, p = 0.0141) (Fig 7Aiv), suggesting that cGKII activity is critical for CXCR4-tropic gp120 (IIIB)-induced aberrant Ca2+ activation. Unlike T-cell tropic viruses that use CXCR4, macrophage-tropic HIV uses a chemokine receptor CCR5 as a co-receptor [59]. We next treated neurons with 1-nM CCR5-tropic gp120 (JRFL) and found that gp120 (JRFL) was also able to induce Ca2+ overactivation (CTRL, 1 ± 0.09 ΔF/Fmin; gp120 (JRFL), 1.87 ± 0.15 ΔF/Fmin, p < 0.0001) (Fig 7Bi and 7Bii), which was abolished by RP treatment (1.05 ± 0.16 ΔF/Fmin, p = 0.0014) (Fig 7Biv). This suggests that cGKII activation is required for CXCR4 and CCR5-tropic gp120-indcued Ca2+ hyperactivity. We further examined whether CXCR4 inhibition affected the CCR5-tropic gp120 (JRFL) effects on Ca2+ activity by treating neurons with 1-nM gp120 (JRFL) and 200-nM AMD3100 together. We found that AMD3100 treatment was also able to block gp120 (JRFL)-induced Ca2+ hyperexcitation (0.84 ± 0.13 ΔF/Fmin, p < 0.0001) (Fig 7Biii). This suggests that there is cross talk between the two chemokine receptors. Additionally, the natural agonist of CXCR4, stromal cell-derived factor-1 (SDF-1), is by itself neurotoxic [60,61]. We thus examined whether SDF-1 was sufficient to induce cGKII-dependent Ca2+ overactivation. Notably, 20-nM SDF-1 treatment was able to increase neuronal Ca2+ activity (CTRL, 1 ± 0.23 ΔF/Fmin; SDF-1, 2.28 ± 0.29 ΔF/Fmin, p = 0.0002) (Fig 7Ci and 7Cii), which was abolished by RP or AMD3100 treatment (RP, 1.14 ± 0.18 ΔF/Fmin, p = 0.0029; AMD3100, 1.26 ± 0.19 ΔF/Fmin, p = 0.0028) (Fig 7Ciii and 7Civ), confirming that CXCR4 stimulation is sufficient to induce cGKII-dependent Ca2+ overactivation. In summary, we confirm that both FIV gp95 and HIV gp120 interact with CXCR4 and subsequently promote cGKII-mediated Ca2+ hyperexcitation.
Fig 7. cGKII activation is required for HIV gp120 and SDF-1-induced Ca2+ hyperactivity.
(A) Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp120 (IIIB), (iii) 200-nM AMD3100 and 1-nM gp120 (IIIB), and (iv) 1-μM RP and 1-nM gp120 (IIIB), showing that an increase in Ca2+ activity by 1-nM CXCR4-tropic gp120 (IIIB) treatment is dependent on CXCR4 and cGKII (n = number of neurons, *p < 0.05, one-way ANOVA, uncorrected Fischer’s LSD, F (3,51) = 3.936, p = 0.0133). A scale bar indicates 20 seconds. (B) Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 1-nM gp120 (JRFL), (iii) 200-nM AMD3100 and 1-nM gp120 (JRFL), and (iv) 1-μM RP and 1-nM gp120 (JRFL), showing that an increase in Ca2+ activity by 1-nM CCR5-tropic gp120 (JRFL) treatment is dependent on CXCR4 and cGKII (n = number of neurons, *p < 0.05, one-way ANOVA, uncorrected Fischer’s LSD, F (3,115) = 3.903, p = 0.0107). A scale bar indicates 20 seconds. (C) Representative traces of GCaMP5 fluorescence intensity and a summary graph of normalized average of total Ca2+ activity in (i) control neurons and neurons treated with (ii) 20-nM SDF-1, (iii) 1-μM RP and 20-nM SDF-1, and (iv) 200-nM AMD3100 and 20-nM SDF-1, showing that 20-nM SDF-1 induces cGKII- and CXCR4-dependent Ca2+ overactivation (n = number of neurons, ***p < 0.001, one-way ANOVA, uncorrected Fischer’s LSD, F (3,63) = 6.234, p = 0.0009). A scale bar indicates 20 seconds. AMD3100, bicyclam derivative plerixafor hydrochloride; cGKII, cGMP-dependent protein kinase II; LSD, Least Significant Difference; SDF-1, stromal cell-derived factor-1.
Discussion
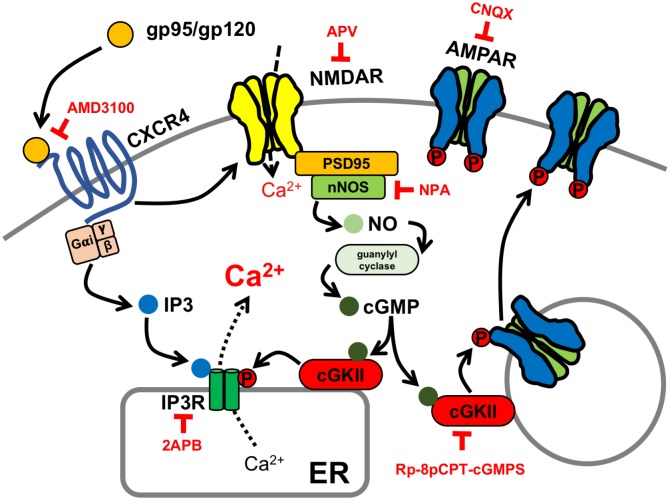
Although synaptic dysfunction, not neuronal death, is strongly associated with HAND [5], the molecular mechanisms underlying HAND-associated synaptic impairment remain largely unclear [6]. Previous studies document that FIV envelope proteins also elevate neuronal Ca2+ and induce cell death in neurons [22,62,63]. However, cellular mechanisms of such FIV envelope protein-induced neurotoxic effects are unknown. We reveal that FIV envelope glycoprotein gp95 binds to CXCR4 on the neuronal plasma membrane and subsequently elevates intracellular Ca2+ through mobilizing ER Ca2+ via the stimulation of IP3Rs, as well as NMDARs, the same pathway of HIV gp120-induced Ca2+ overactivation [18,49,50] (Fig 8). Most notably, our study identifies that gp95-stimulated NMDARs activate the nNOS-cGMP-cGKII pathway, which subsequently phosphorylates IP3Rs and AMPAR subunit GluA1, leading to the elevation of surface GluA1 expression and AMPAR-mediated synaptic activity, a cellular basis of synaptic dysfunction in HAND (Fig 8). Moreover, we show that cGKII activation is required for Ca2+ hyperactivity caused by HIV gp120 (Fig 7A and 7B), suggesting that cGKII activation plays crucial roles in synaptic dysfunction in both HIV and FIV models and there is a conserved cellular pathophysiology from mice and cats to humans.
Fig 8. Model for gp95/120-induced activity-dependent synaptic hyperexcitation.
Both FIV gp95 and HIV gp120 stimulate CXCR4 and NMDARs, inducing activity-dependent synaptic dysfunction via cGKII activation. The gp95/120 stimulation of NMDARs activates nNOS, production of NO, leading to activation of soluble guanylyl cyclase and the production of cGMP, which in turn activates cGKII. Both the production of IP3 by the gp95/120 stimulation of CXCR4 and cGKII-induced phosphorylation of IP3Rs enhance ER Ca2+ release, contributing to Ca2+ hyperactivity. In addition, gp95-induced cGKII activation increases GluA1 phosphorylation, promoting elevation of surface AMPARs, which leads to the elevation of synaptic excitation. Therefore, the gp120/gp95-induced stimulation of cGKII is critical for synaptic hyperexcitation in HAND pathophysiology. AMD3100, bicyclam derivative plerixafor hydrochloride; AMPAR, AMPA receptor; cGKII, cGMP-dependent protein kinase II; cGMP, cyclic GMP; CNQX, 6-Cyano-7-nitroquinoxaline-2,3-dione; ER, endoplasmic reticulum; FIV, feline immunodeficiency virus; HAND, HIV-associated neurocognitive disorder; HIV, human immunodeficiency virus; IP3R, inositol triphosphate receptor; NMDAR, NMDA receptor; nNOS, neuronal nitric oxide synthase; NO, nitric oxide; NPA, Nω-Propyl-L-arginine hydrochloride; PSD95, postsynaptic density 95.
Although treatment of a lower dose of CNQX or DL-APV was unable to inhibit basal Ca2+ activity, lower doses in combination completely inhibited Ca2+ activity in both control and gp95-treated neurons (S5 Fig), suggesting that inhibition of both receptors induces additive effects on Ca2+ activity. Given that there is NMDAR-independent Ca2+ influx via L-type voltage-gated Ca2+ channels [64], a lower dose of DL-APV alone is unable to block neuronal Ca2+ activity completely. In fact, we found that 10-μM nifedipine, an antagonist of L-type voltage-gated Ca2+ channels, was sufficient to abolish GCaMP5 activity in both control and gp95-treated cells (S6B Fig). In addition, NMDARs significantly contribute to signaling at rest in the absence of AMPAR activity [65], although Ca2+ permeability through NMDARs at negative membrane potentials is restricted because of their blockade by extracellular Mg2+ ions [66,67]. Taken together, although AMPAR-mediated dendritic depolarization is required for removal of Mg2+ ions for NMDAR activity, both receptors can also contribute to neuronal Ca2+ activity in parallel.
We found that both amplitude and frequency of Ca2+ activity and mEPSCs are significantly elevated in gp95-treated neurons (Figs 1B and 4E). Although the current study identifies cellular mechanisms of gp95-induced postsynaptic changes, it is possible that there can be gp95-induced presynaptic processes that induce synaptic hyperexcitation. Notably, neuroinflammatory processes mediated by activated microglia have been strongly implicated in a number of neurodegenerative diseases, including HAND [68]. Similar to neuronal mechanisms, HIV gp120 interacts with microglial CXCR4 and stimulates cGMP-dependent kinase, leading to microglial activation during neurodegenerative inflammation [69]. Importantly, gp120 elevates synaptic receptor activity by enhancing the release of pro-inflammatory cytokines from activated microglia [70,71]. Among those cytokines, tumor necrosis factor alpha (TNFα) induces a rapid increase in mEPSC amplitude and frequency [72–74], as seen in gp95-treated neurons (Fig 4E). Although we used Neurobasal Medium designed for significantly less proliferation of glia [75], we were unable to completely remove microglia in our culture. This thus suggests that microglial activation by gp120 and gp95 can promote TNFα release, resulting in elevation of mEPSC frequency and amplitude.
Both HIV gp120 and FIV gp95 interact with CXCR4 to produce IP3, which can induce IP3R-mediated Ca2+ efflux from the ER (Fig 2). However, we found that TTX completely abolished Ca2+ activity (S6 Fig). This suggests that IP3 production through the interaction between gp120/gp95 and CXCR4 is not sufficient to increase neuronal Ca2+ activity in the absence of neuronal activity. Furthermore, gp95-induced stimulation of AMPARs and NMDARs is insufficient to elevate Ca2+ activity in neuronal cell bodies in the absence of IP3R-mediated ER Ca2+ release (Fig 8), as indicated by decreased Ca2+ activity via the inhibition of ER Ca2+ channels (Fig 2). In our model, we thus propose that neuronal activity–driven stimulation of extracellular Ca2+ influx through L-type voltage-gated Ca2+ channels and NMDARs and Ca2+ efflux from the ER coordinate and contribute to somatic Ca2+ activity (Fig 8). Further work is necessary to differentiate the roles of these Ca2+ channels on HIV-induced neuronal hyperexcitability.
The chemokine receptors CCR5 and CXCR4 are co-receptors together with CD4 for HIV entry into target cells [17]. Macrophage-tropic HIV viruses use CCR5 as a co-receptor [76–80], whereas T-cell line–tropic viruses use CXCR4 [81,82]. Given that most of the HIV-infected cells in the brain are macrophages and microglia, it is thought that CCR5 strains of HIV are the predominant viral species in the brain [83,84]. However, once HIV infection is established, dual tropic and CXCR4-preferring viruses slowly evolve from macrophage-tropic HIV viruses as an indication of progression to AIDS and HIV-associated dementia [17, 85–88]. Moreover, CXCR4- and dual-tropic strains of HIV have been isolated from the brains of infected individuals [86]. Therefore, CXCR4-tropic strains of HIV also play critical roles in the pathogenesis of HAND. Several studies have shown that the HIV gp120 binding to both CCR5 and CXCR4, even without CD4, contributes to neuronal injury and death both in vitro and in vivo [29–31, 89–93]. Interestingly, a CCR5 antagonist prevents gp120 neurotoxicity [94, 95], and natural CCR5 ligands confer protection upon neurons against gp120 toxicity [61]. Conversely, HIV-induced apoptosis can be prevented by AMD3100, a CXCR4 antagonist, both in vitro and in vivo [96–98]. This suggests that CXCR4-mediated signaling can trigger HIV-induced neurotoxicity while CCR5 either protects or disrupts the CNS, depending on the context, ligand characteristics, and resultant signaling pathway. Surprisingly, CCR5-tropic gp120 (JRFL) also requires cGKII activation to induce Ca2+ hyperexcitation (Fig 7B). It has been shown that chemokines and their receptors coordinate the signaling at the immunological synapses. In fact, during T-cell activation, CXCR4 and CCR5 chemokine receptors are recruited into the immunological synapse by antigen-presenting cell-derived chemokines [99]. In addition, the co-stimulatory properties of CCR5 and CXCR4 depend on their ability to form heterodimers [100]. Thus, gp120 (JRFL)-induced stimulation to CCR5 can interact with CXCR4, resulting in cGKII activation. Notably, the natural ligand of CXCR4, SDF-1, is also sufficient to induce cGKII-dependent Ca2+ overactivation (Fig 7C). Taken together, CCR5–CXCR4 stimulation is sufficient to induce hyperexcitation in neurons. While both CXCR4 and CCR5 are important in the neuropathogenesis of HIV, it is clear that further study of the downstream pathways of CCR5 and CXCR4 activation in neurons will widen the understanding of HIV-induced neuronal toxicity. Given that FIV also targets primary CD4 T cells but uses CD134 instead of CD4 as a primary receptor and uses its sole co-receptor CXCR4 for efficient infection of target cells, similarly to T cell–tropic strains of HIV [18,19,49], FIV infection of cats is an ideal in vivo model to investigate CXCR4-mediated neuropathology in chronic HIV infection.
Our work extends beyond understanding of molecular mechanisms underlying HIV-induced neuronal dysfunction. One of the challenges that the HAND research community has faced in the treatment of this disorder is the lack of a viable target [1]. By identifying cGKII as the downstream effector of the gp95/120-induced synaptic hyperexcitation, our study completes the pathway and identifies cGKII as a new therapeutic target for limiting gp95/120-induced synaptic dysfunction. Moreover, we reveal that CCR5-tropic gp120-induced Ca2+ overactivation is also dependent on cGKII (Fig 7B). This thus suggests that cGKII activation is important for CCR5 and CXCR4-dependent neuropathology in HAND. Inhibition of cGKII may be superior as a therapeutic target to other forms of ER Ca2+ release control, as its inhibition will limit the NMDAR-induced and IP3R phosphorylation–dependent Ca2+ increase specifically, which are likely to be elevated under hyperexcitable conditions, while leaving basal functions unchanged. Thus, use of cGKII inhibition as a means for neuroprotection in individuals infected with HIV is a novel and innovative approach to this therapeutically challenging disease pathway.
Materials and methods
Ethics statement
Colorado State University’s Institutional Animal Care and Use Committee reviewed and approved the animal care and protocol (16-6779A).
Mouse and feline neuron culture
Mouse hippocampal and cortical neuron cultures were prepared as described previously [43,46,47]. Neurons were isolated from embryonic day 17–18 or postnatal day 0.5 C57Bl6 or cGKII KO mouse embryonic brain tissues. For feline hippocampal neurons, embryos were obtained by cesarean section at approximately 35–40 days gestation from specific pathogen-free cats. Hippocampi were isolated from embryos and digested with 10 U/mL papain (Worthington Biochemical Corp., NJ). Mouse cortical neurons were plated on polylysine-coated 15-cm dishes (25 million cells per dish) and 6-well dishes (500,000 cells per well) for biochemical experiments. Mouse and feline hippocampal cells were prepared in glass-bottom dishes (500,000 cells in the glass bottom) for Ca2+ imaging. Mouse hippocampal neurons were also plated on 12-mm coverslips for electrophysiology (200,000 cells per coverslip). Cells were grown in Neurobasal Medium with B27 and 0.5 mM Glutamax and penicillin/streptomycin (Life Technologies).
Reagents
Expression, amplification, and purification of FIV envelope glycoprotein gp95 and capsid p26 recombinant proteins were performed using previously described methods [50,101]. Briefly, gp95 was purified from Chinese hamster ovary (CHO) cells, and the human Fc tag, in frame with either protein, served as a means to purify the proteins using Staphylococcus Protein A-Sepharose [102,103], or was isolated following transfection of HEK 293S cells with an expression vector. Gag antigen was expressed in Escherichia coli and purified using a GST-tag [101]. HIV CXCR4-tropic gp120 (IIIB) was obtained through the NIH AIDS Reagent Program, Division of AIDS, NIAID, NIH: HIV-1 IIIB gp120 Recombinant Protein from ImmunoDX, LLC. HIV CCR5-tropic gp120 (JRFL) was obtained from Dr. C.A.L. Kassuya at the Federal University of Grande Dourados, Brazil [104]. The following inhibitors were used in this study: 200-nM AMD3100 (Tocris), 25-μM 2APB (Abcam), 10-μM Dantrolene (Abcam), 25-μM or 50-μM DL-APV (Abcam), 2-μM NPA (Tocris), 1-μM or 10-μM Rp8-Br-PET-cGMPS (Tocris) for cultured mouse or feline neurons, respectively, 10-μM or 30-μM CNQX (Abcam), 1-μM TTX (Tocris), 10-μM nifedipine (Abcam), and 20-nM human SDF-1 (Abcam).
GCaMP5 Ca2+ imaging
GCaMP5 Ca2+ imaging was carried out by a modification of the previously reported method [43,46,47]. DIV4 Neurons were transfected with pCMV-GCaMP5 (a gift from Douglas Kin and Loren Looger, Addgene plasmid #31788) [105] by using Lipofectamine 2000 (Life Technologies) according to the manufacturer’s protocol. The transfection efficiency is about 5%, and obvious cellular toxicity has not been observed. Neurons were grown in Neurobasal Medium without phenol red supplemented with B27 and 0.5-mM Glutamax and penicillin/streptomycin (Life Technologies) for 8–12 days after transfection and during the imaging. Glass-bottom dishes were mounted on a temperature-controlled stage on Olympus IX73 and maintained at 37 °C and 5% CO2 using a Tokai Hit heating stage and digital temperature and humidity controller. The imaging was captured for periods of 50 milliseconds using a 60× oil-immersion objective. A total of 100 images was obtained with 1-second interval, and Ca2+ activity in the cell body (excluding dendrites) was analyzed using the Olympus CellSens software. Fmin was determined as the minimum fluorescence value during the imaging. Total Ca2+ activity was obtained by combining 100 values of ΔF/Fmin = (Ft − Fmin)/Fmin in each image, and values of ΔF/Fmin < 0.2 were rejected due to bleaching. Twenty to thirty neurons were used for imaging in one experiment, and one individual neuron was assayed in one imaging.
Synaptosome purification, surface biotinylation, and immunoblots
Synaptosomal fractions from DIV14 primary cortical neurons were prepared as described previously [43,46,47]. Surface biotinylation was performed according to the previous studies [43,46,47]. For IP3R phosphorylation, whole cell lysates were collected as described previously [43]. Equal amounts of protein were loaded on 10% SDS-PAGE gel and transferred to nitrocellulose membranes. Membranes were blotted with GluA1 (Millipore, 1:2,000), GluA2 (Abcam, 1:2,000), pGluA1(S845) (Millipore, 1:1,000), pIP3R(S1756) (Cell signaling, 1:1,000), tubulin (Sigma, 1:5,000), PSD95 (Neuromab, 1:2,000), synaptophysin (Sigma, 1:5,000), NR1 (Millipore, 1:1,000), and actin (Abcam, 1:2,000) antibodies and developed with ECL (Thermo Fisher Scientific). Synaptosomes were isolated from at least three independent cultures, and immunoblots were at least duplicated for quantitative analysis.
Electrophysiology
To record mEPSCs, aCSF contained bicuculline (20 μM), TTX (1 μM), and glycine (1 μM). The recording chamber contained aCSF with a composition of (in mM) 119 NaCl, 5 KCl, 2.5 CaCl2, 1.5 MgCl2, 30 glucose, and 20 HEPES and was kept at a constant temperature of 31.0 °C. Patch pipettes were filled with (in mM) 120 KGlu, 20 KCl, 2 MgCl2, 10 HEPES, 2 MgATP, 200-μM GTP, and 12.5 mg sucrose and were pH’d with KOH to 7.4. Cells were voltage clamped at −70 mV and input resistance and series resistance were monitored throughout experiments. mEPSCs were amplified and recorded using pClamp10.3. Mini Analysis Program Demo (Synaptosoft, GA) was used to measure the peak mEPSC amplitude and decay time. CellSens software (Olympus) was used to visualize cells. Patching pipettes were pulled from borosilicate capillary tubing (Sutter Instruments, CA) and the electrode resistance was typically 4–6 mOhms.
Statistics
Statistical comparisons were analyzed with the GraphPad Prism6 software. Unpaired two-tailed Student t tests were used in single comparisons. For multiple comparisons, we used one-way ANOVA followed by Fisher’s Least Significant Difference (LSD) test to determine statistical significance. Results were represented as mean ± SEM, and p < 0.05 was considered statistically significant.
Supporting information
An example of time-lapse images and their responses. A scale bar indicates 10 μm.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that a higher dose of DL-APV completely blocks Ca2+ activity in both control and gp95-treated neurons, while a lower dose of DL-APV selectively inhibits the gp95 effects (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (5,304) = 9.238). A scale bar indicates 20 seconds. LSD, Least Significant Difference; NMDAR, NMDA receptor.
(TIF)
The quality of synaptosomes used in Fig 4A and 4B has been monitored by immunoblots of synaptic proteins in sequential fractions showing that synaptic proteins such as GluA2, PSD95, and synaptophysin are highly enriched in the synaptosome fractions. PSD95, postsynaptic density 95.
(TIF)
Representative immunoblots and quantitative analysis of surface biotinylation in each condition showing that gp95 has no effect on surface expression of (A) GluA2 (n = 12 experiments) and (B) NR1 (n = 5 experiments, CTRL). Actin is used as an intracellular negative control and absent in the biotinylated samples.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that a higher dose of CNQX completely blocks Ca2+ activity in both control and gp95-treated neurons, while a lower dose of CNQX selectively inhibits the gp95 effects. Furthermore, lower doses of DL-APV and CNQX in combination completely inhibited Ca2+ activity in both control and gp95-treated neurons, suggesting that inhibition of both receptors induces additive effects on Ca2+ activity (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (7,179) = 5.933). A scale bar indicates 20 seconds. AMPAR, AMPA receptor; CNQX, 6-Cyano-7-nitroquinoxaline-2,3-dione; LSD, Least Significant Difference.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that inhibition of (A) neuronal activity by TTX and (B) L-type Ca2+ channels abolish GCaMP5 activity in both control and gp95-treated neurons (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, (A) F (3,220) = 25.61 and (B) F (3,206) = 17.17). A scale bar indicates 20 seconds. LSD, Least Significant Difference; TTX, tetrodotoxin.
(TIF)
(XLSX)
Acknowledgments
We thank members of the Kim and VandeWoude laboratory for their generous support. We thank Gavin Ryan for technical assistance. We also thank Drs. Edward Ziff, Michael Tamkun, Susan Tsunoda, Jozsef Vigh, and Colin Clay for helpful discussion. Esther Musselman and Jennifer Kopanke assisted with collection of feline tissues. Britta Wood synthesized stocks of FIV p26. We also thank Dr. C.A.L. Kassuya at the Federal University of Grande Dourados, Brazil, for CCR5-tropic gp120 (JRFL).
Abbreviations
- 2APB
2-aminoethoxydiphenyl borate
- a.u.
arbitrary unit
- AIDS
acquired immune deficiency syndrome
- AMD3100
bicyclam derivative plerixafor hydrochloride
- AMPAR
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
- ANI
asymptomatic neurocognitive impairment
- cART
combination antiretroviral therapy
- CCR5
C-C chemokine receptor type 5
- CD
cluster of differentiation
- cGKII
cGMP-dependent protein kinase II
- cGMP
cyclic guanosine monophosphate
- CHO
Chinese hamster ovary
- CNQX
6-Cyano-7-nitroquinoxaline-2,3-dione
- CNS
central nervous system
- CP-AMPAR
Ca2+-permeable AMPAR
- CXCR4
C-X-C chemokine receptor type 4
- DIV
day in vitro
- DL-APV
DL-2-Amino-5-phosphonopentanoic acid
- ER
endoplasmic reticulum
- FIV
feline immunodeficiency virus
- HAND
HIV-associated neurocognitive disorder
- HIV
human immunodeficiency virus
- IP3
inositol triphosphate
- IP3R
inositol triphosphate receptor
- KO
knockout
- LSD
Least Significant Difference
- LTP
long-term potentiation
- mEPSC
miniature excitatory postsynaptic current
- MND
mild neurological disorder
- NASPM
1-naphthyl acetyl spermine
- NMDAR
N-methyl-D-aspartate receptor
- nNOS
neuronal nitric oxide synthase
- NO
nitric oxide
- NPA
Nω-Propyl-L-arginine hydrochloride
- PSD95
postsynaptic density 95
- RyR
Ryanodine receptor
- SDF-1
stromal cell-derived factor-1
- SIV
simian immunodeficiency virus
- TNFα
tumor necrosis factor alpha
- TTX
tetrodotoxin
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
NIH (grant number T35 OD015130). Received by KS. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. NIH (grant number F32 DE026679). Received by CM. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. NIH (grant number R01 AI25825). Received by JE and SV. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Colorado State University (grant number 1-686232). Received by SK. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Colorado State University (grant number 1-326522). Received by SK. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. NIH (grant number R01 DA040965). Received by TEB. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Saylor D, Dickens AM, Sacktor N, Haughey N, Slusher B, Pletnikov M, et al. HIV-associated neurocognitive disorder—pathogenesis and prospects for treatment. Nat Rev Neurol. 2016;12(4):234–48. 10.1038/nrneurol.2016.27 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellis RJ, Deutsch R, Heaton RK, Marcotte TD, McCutchan JA, Nelson JA, et al. Neurocognitive impairment is an independent risk factor for death in HIV infection. San Diego HIV Neurobehavioral Research Center Group. Arch Neurol. 1997;54(4):416–24. . [DOI] [PubMed] [Google Scholar]
- 3.Gelman BB. Neuropathology of HAND With Suppressive Antiretroviral Therapy: Encephalitis and Neurodegeneration Reconsidered. Curr HIV/AIDS Rep. 2015;12(2):272–9. 10.1007/s11904-015-0266-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Everall I, Vaida F, Khanlou N, Lazzaretto D, Achim C, Letendre S, et al. Cliniconeuropathologic correlates of human immunodeficiency virus in the era of antiretroviral therapy. J Neurovirol. 2009;15(5–6):360–70. 10.3109/13550280903131915 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellis R, Langford D, Masliah E. HIV and antiretroviral therapy in the brain: neuronal injury and repair. Nat Rev Neurosci. 2007;8(1):33–44. 10.1038/nrn2040 . [DOI] [PubMed] [Google Scholar]
- 6.McArthur JC, Brew BJ. HIV-associated neurocognitive disorders: is there a hidden epidemic? AIDS. 2010;24(9):1367–70. 10.1097/QAD.0b013e3283391d56 . [DOI] [PubMed] [Google Scholar]
- 7.Hatziioannou T, Evans DT. Animal models for HIV/AIDS research. Nat Rev Microbiol. 2012;10(12):852–67. 10.1038/nrmicro2911 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraft-Terry SD, Buch SJ, Fox HS, Gendelman HE. A coat of many colors: neuroimmune crosstalk in human immunodeficiency virus infection. Neuron. 2009;64(1):133–45. 10.1016/j.neuron.2009.09.042 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaeger LB, Nath A. Modeling HIV-associated neurocognitive disorders in mice: new approaches in the changing face of HIV neuropathogenesis. Dis Model Mech. 2012;5(3):313–22. 10.1242/dmm.008763 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fox HS, Gendelman HE. Commentary: Animal models of neuroAIDS. J Neuroimmune Pharmacol. 2012;7(2):301–5. 10.1007/s11481-012-9368-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Apetrei C, Kaur A, Lerche NW, Metzger M, Pandrea I, Hardcastle J, et al. Molecular epidemiology of simian immunodeficiency virus SIVsm in U.S. primate centers unravels the origin of SIVmac and SIVstm. J Virol. 2005;79(14):8991–9005. 10.1128/JVI.79.14.8991-9005.2005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gardner MB. The history of simian AIDS. J Med Primatol. 1996;25(3):148–57. . [DOI] [PubMed] [Google Scholar]
- 13.Dow SW, Poss ML, Hoover EA. Feline immunodeficiency virus: a neurotropic lentivirus. J Acquir Immune Defic Syndr. 1990;3(7):658–68. . [PubMed] [Google Scholar]
- 14.Podell M, March PA, Buck WR, Mathes LE. The feline model of neuroAIDS: understanding the progression towards AIDS dementia. J Psychopharmacol. 2000;14(3):205–13. 10.1177/026988110001400303 . [DOI] [PubMed] [Google Scholar]
- 15.Elder JH, Lin YC, Fink E, Grant CK. Feline immunodeficiency virus (FIV) as a model for study of lentivirus infections: parallels with HIV. Curr HIV Res. 2010;8(1):73–80. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomez NV, Fontanals A, Castillo V, Gisbert MA, Suraniti A, Mira G, et al. Evaluation of different antiretroviral drug protocols on naturally infected feline immunodeficiency virus (FIV) cats in the late phase of the asymptomatic stage of infection. Viruses. 2012;4(6):924–39. 10.3390/v4060924 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michael NL, Moore JP. HIV-1 entry inhibitors: evading the issue. Nature medicine. 1999;5(7):740–2. 10.1038/10462 . [DOI] [PubMed] [Google Scholar]
- 18.de Parseval A, Chatterji U, Sun P, Elder JH. Feline immunodeficiency virus targets activated CD4+ T cells by using CD134 as a binding receptor. Proc Natl Acad Sci U S A. 2004;101(35):13044–9. 10.1073/pnas.0404006101 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willett BJ, Picard L, Hosie MJ, Turner JD, Adema K, Clapham PR. Shared usage of the chemokine receptor CXCR4 by the feline and human immunodeficiency viruses. J Virol. 1997;71(9):6407–15. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Everall IP, Luthert PJ, Lantos PL. Neuronal number and volume alterations in the neocortex of HIV infected individuals. J Neurol Neurosurg Psychiatry. 1993;56(5):481–6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wiley CA, Masliah E, Morey M, Lemere C, DeTeresa R, Grafe M, et al. Neocortical damage during HIV infection. Ann Neurol. 1991;29(6):651–7. 10.1002/ana.410290613 . [DOI] [PubMed] [Google Scholar]
- 22.Bragg DC, Meeker RB, Duff BA, English RV, Tompkins MB. Neurotoxicity of FIV and FIV envelope protein in feline cortical cultures. Brain research. 1999;816(2):431–7. . [DOI] [PubMed] [Google Scholar]
- 23.Brenneman DE, Westbrook GL, Fitzgerald SP, Ennist DL, Elkins KL, Ruff MR, et al. Neuronal cell killing by the envelope protein of HIV and its prevention by vasoactive intestinal peptide. Nature. 1988;335(6191):639–42. 10.1038/335639a0 . [DOI] [PubMed] [Google Scholar]
- 24.Schneider J, Bayer H, Bienzle U, Hunsmann G. A glycopolypeptide (gp 100) is the main antigen detected by HTLV-III antisera. Med Microbiol Immunol. 1985;174(1):35–42. . [DOI] [PubMed] [Google Scholar]
- 25.Kettenmann H, Kirchhoff F, Verkhratsky A. Microglia: new roles for the synaptic stripper. Neuron. 2013;77(1):10–8. 10.1016/j.neuron.2012.12.023 . [DOI] [PubMed] [Google Scholar]
- 26.Kim HJ, Shin AH, Thayer SA. Activation of cannabinoid type 2 receptors inhibits HIV-1 envelope glycoprotein gp120-induced synapse loss. Mol Pharmacol. 2011;80(3):357–66. 10.1124/mol.111.071647 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu H, Bae M, Tovar-y-Romo LB, Patel N, Bandaru VV, Pomerantz D, et al. The human immunodeficiency virus coat protein gp120 promotes forward trafficking and surface clustering of NMDA receptors in membrane microdomains. J Neurosci. 2011;31(47):17074–90. 10.1523/JNEUROSCI.4072-11.2011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng J, Ghorpade A, Niemann D, Cotter RL, Thylin MR, Epstein L, et al. Lymphotropic virions affect chemokine receptor-mediated neural signaling and apoptosis: implications for human immunodeficiency virus type 1-associated dementia. J Virol. 1999;73(10):8256–67. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hesselgesser J, Taub D, Baskar P, Greenberg M, Hoxie J, Kolson DL, et al. Neuronal apoptosis induced by HIV-1 gp120 and the chemokine SDF-1 alpha is mediated by the chemokine receptor CXCR4. Current biology: CB. 1998;8(10):595–8. . [DOI] [PubMed] [Google Scholar]
- 30.Zheng J, Thylin MR, Ghorpade A, Xiong H, Persidsky Y, Cotter R, et al. Intracellular CXCR4 signaling, neuronal apoptosis and neuropathogenic mechanisms of HIV-1-associated dementia. J Neuroimmunol. 1999;98(2):185–200. . [DOI] [PubMed] [Google Scholar]
- 31.Meucci O, Fatatis A, Simen AA, Bushell TJ, Gray PW, Miller RJ. Chemokines regulate hippocampal neuronal signaling and gp120 neurotoxicity. Proc Natl Acad Sci U S A. 1998;95(24):14500–5. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lipton SA, Sucher NJ, Kaiser PK, Dreyer EB. Synergistic effects of HIV coat protein and NMDA receptor-mediated neurotoxicity. Neuron. 1991;7(1):111–8. . [DOI] [PubMed] [Google Scholar]
- 33.Haughey NJ, Mattson MP. Calcium dysregulation and neuronal apoptosis by the HIV-1 proteins Tat and gp120. J Acquir Immune Defic Syndr. 2002;31 Suppl 2:S55–61. . [DOI] [PubMed] [Google Scholar]
- 34.Ballester LY, Capo-Velez CM, Garcia-Beltran WF, Ramos FM, Vazquez-Rosa E, Rios R, et al. Up-regulation of the neuronal nicotinic receptor alpha7 by HIV glycoprotein 120: potential implications for HIV-associated neurocognitive disorder. The Journal of biological chemistry. 2012;287(5):3079–86. 10.1074/jbc.M111.262543 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bredt DS, Snyder SH. Nitric oxide mediates glutamate-linked enhancement of cGMP levels in the cerebellum. Proc Natl Acad Sci U S A. 1989;86(22):9030–3. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garthwaite J, Garthwaite G, Palmer RM, Moncada S. NMDA receptor activation induces nitric oxide synthesis from arginine in rat brain slices. European journal of pharmacology. 1989;172(4–5):413–6. . [DOI] [PubMed] [Google Scholar]
- 37.Kornau HC, Seeburg PH, Kennedy MB. Interaction of ion channels and receptors with PDZ domain proteins. Curr Opin Neurobiol. 1997;7(3):368–73. . [DOI] [PubMed] [Google Scholar]
- 38.Christopherson KS, Hillier BJ, Lim WA, Bredt DS. PSD-95 assembles a ternary complex with the N-methyl-D-aspartic acid receptor and a bivalent neuronal NO synthase PDZ domain. The Journal of biological chemistry. 1999;274(39):27467–73. . [DOI] [PubMed] [Google Scholar]
- 39.Rameau GA, Tukey DS, Garcin-Hosfield ED, Titcombe RF, Misra C, Khatri L, et al. Biphasic coupling of neuronal nitric oxide synthase phosphorylation to the NMDA receptor regulates AMPA receptor trafficking and neuronal cell death. J Neurosci. 2007;27(13):3445–55. 10.1523/JNEUROSCI.4799-06.2007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bredt DS. Nitric oxide signaling specificity—the heart of the problem. Journal of cell science. 2003;116(Pt 1):9–15. . [DOI] [PubMed] [Google Scholar]
- 41.Eugenin EA, King JE, Nath A, Calderon TM, Zukin RS, Bennett MV, et al. HIV-tat induces formation of an LRP-PSD-95- NMDAR-nNOS complex that promotes apoptosis in neurons and astrocytes. Proc Natl Acad Sci U S A. 2007;104(9):3438–43. 10.1073/pnas.0611699104 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krogh KA, Wydeven N, Wickman K, Thayer SA. HIV-1 protein Tat produces biphasic changes in NMDA-evoked increases in intracellular Ca2+ concentration via activation of Src kinase and nitric oxide signaling pathways. Journal of neurochemistry. 2014;130(5):642–56. 10.1111/jnc.12724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim S, Titcombe RF, Zhang H, Khatri L, Girma HK, Hofmann F, et al. Network compensation of cyclic GMP-dependent protein kinase II knockout in the hippocampus by Ca2+-permeable AMPA receptors. Proc Natl Acad Sci U S A. 2015;112(10):3122–7. Epub 2015/02/26. 10.1073/pnas.1417498112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Serulle Y, Zhang S, Ninan I, Puzzo D, McCarthy M, Khatri L, et al. A GluR1-cGKII interaction regulates AMPA receptor trafficking. Neuron. 2007;56(4):670–88. Epub 2007/11/23. 10.1016/j.neuron.2007.09.016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gleichmann M, Mattson MP. Neuronal calcium homeostasis and dysregulation. Antioxid Redox Signal. 2011;14(7):1261–73. 10.1089/ars.2010.3386 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim S, Violette CJ, Ziff EB. Reduction of increased calcineurin activity rescues impaired homeostatic synaptic plasticity in presenilin 1 M146V mutant. Neurobiol Aging. 2015;36(12):3239–46. Epub 2015/10/13. 10.1016/j.neurobiolaging.2015.09.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim S, Ziff EB. Calcineurin mediates synaptic scaling via synaptic trafficking of Ca2+-permeable AMPA receptors. PLoS Biol. 2014;12(7):e1001900 10.1371/journal.pbio.1001900 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Medina I, Ghose S, Ben-Ari Y. Mobilization of intracellular calcium stores participates in the rise of [Ca2+]i and the toxic actions of the HIV coat protein GP120. The European journal of neuroscience. 1999;11(4):1167–78. . [DOI] [PubMed] [Google Scholar]
- 49.Shimojima M, Miyazawa T, Ikeda Y, McMonagle EL, Haining H, Akashi H, et al. Use of CD134 as a primary receptor by the feline immunodeficiency virus. Science. 2004;303(5661):1192–5. 10.1126/science.1092124 . [DOI] [PubMed] [Google Scholar]
- 50.de Parseval A, Elder JH. Binding of recombinant feline immunodeficiency virus surface glycoprotein to feline cells: role of CXCR4, cell-surface heparans, and an unidentified non-CXCR4 receptor. J Virol. 2001;75(10):4528–39. 10.1128/JVI.75.10.4528-4539.2001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dreyer EB, Kaiser PK, Offermann JT, Lipton SA. HIV-1 coat protein neurotoxicity prevented by calcium channel antagonists. Science. 1990;248(4953):364–7. . [DOI] [PubMed] [Google Scholar]
- 52.Pandey V, Bolsover SR. Immediate and neurotoxic effects of HIV protein gp120 act through CXCR4 receptor. Biochem Biophys Res Commun. 2000;274(1):212–5. 10.1006/bbrc.2000.3113 . [DOI] [PubMed] [Google Scholar]
- 53.Hoke A, Morris M, Haughey NJ. GPI-1046 protects dorsal root ganglia from gp120-induced axonal injury by modulating store-operated calcium entry. J Peripher Nerv Syst. 2009;14(1):27–35. 10.1111/j.1529-8027.2009.00203.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bading H. Nuclear calcium signalling in the regulation of brain function. Nat Rev Neurosci. 2013;14(9):593–608. Epub 2013/08/15. 10.1038/nrn3531 . [DOI] [PubMed] [Google Scholar]
- 55.Wagner LE 2nd, Li WH, Yule DI. Phosphorylation of type-1 inositol 1,4,5-trisphosphate receptors by cyclic nucleotide-dependent protein kinases: a mutational analysis of the functionally important sites in the S2+ and S2- splice variants. The Journal of biological chemistry. 2003;278(46):45811–7. 10.1074/jbc.M306270200 . [DOI] [PubMed] [Google Scholar]
- 56.Cull-Candy S, Kelly L, Farrant M. Regulation of Ca2+-permeable AMPA receptors: synaptic plasticity and beyond. Curr Opin Neurobiol. 2006;16(3):288–97. Epub 2006/05/23. 10.1016/j.conb.2006.05.012 . [DOI] [PubMed] [Google Scholar]
- 57.Bowie D. Redefining the classification of AMPA-selective ionotropic glutamate receptors. The Journal of physiology. 2012;590(Pt 1):49–61. Epub 2011/11/23. 10.1113/jphysiol.2011.221689 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shepherd AJ, Loo L, Mohapatra DP. Chemokine co-receptor CCR5/CXCR4-dependent modulation of Kv2.1 channel confers acute neuroprotection to HIV-1 glycoprotein gp120 exposure. PLoS ONE. 2013;8(9):e76698 10.1371/journal.pone.0076698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berger EA. HIV entry and tropism: the chemokine receptor connection. AIDS. 1997;11 Suppl A:S3–16. . [PubMed] [Google Scholar]
- 60.Kaul M, Lipton SA. Chemokines and activated macrophages in HIV gp120-induced neuronal apoptosis. Proc Natl Acad Sci U S A. 1999;96(14):8212–6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kaul M, Ma Q, Medders KE, Desai MK, Lipton SA. HIV-1 coreceptors CCR5 and CXCR4 both mediate neuronal cell death but CCR5 paradoxically can also contribute to protection. Cell Death Differ. 2007;14(2):296–305. 10.1038/sj.cdd.4402006 . [DOI] [PubMed] [Google Scholar]
- 62.Gruol DL, Yu N, Parsons KL, Billaud JN, Elder JH, Phillips TR. Neurotoxic effects of feline immunodeficiency virus, FIV-PPR. J Neurovirol. 1998;4(4):415–25. . [DOI] [PubMed] [Google Scholar]
- 63.Bragg DC, Boles JC, Meeker RB. Destabilization of neuronal calcium homeostasis by factors secreted from choroid plexus macrophage cultures in response to feline immunodeficiency virus. Neurobiology of disease. 2002;9(2):173–86. 10.1006/nbdi.2001.0459 . [DOI] [PubMed] [Google Scholar]
- 64.Moosmang S, Haider N, Klugbauer N, Adelsberger H, Langwieser N, Muller J, et al. Role of hippocampal Cav1.2 Ca2+ channels in NMDA receptor-independent synaptic plasticity and spatial memory. J Neurosci. 2005;25(43):9883–92. 10.1523/JNEUROSCI.1531-05.2005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Espinosa F, Kavalali ET. NMDA receptor activation by spontaneous glutamatergic neurotransmission. Journal of neurophysiology. 2009;101(5):2290–6. 10.1152/jn.90754.2008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mayer ML, Westbrook GL, Guthrie PB. Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurones. Nature. 1984;309(5965):261–3. . [DOI] [PubMed] [Google Scholar]
- 67.Nowak L, Bregestovski P, Ascher P, Herbet A, Prochiantz A. Magnesium gates glutamate-activated channels in mouse central neurones. Nature. 1984;307(5950):462–5. . [DOI] [PubMed] [Google Scholar]
- 68.Gonzalez-Scarano F, Baltuch G. Microglia as mediators of inflammatory and degenerative diseases. Annual review of neuroscience. 1999;22:219–40. 10.1146/annurev.neuro.22.1.219 . [DOI] [PubMed] [Google Scholar]
- 69.Roy A, Fung YK, Liu X, Pahan K. Up-regulation of microglial CD11b expression by nitric oxide. The Journal of biological chemistry. 2006;281(21):14971–80. 10.1074/jbc.M600236200 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sillman B, Woldstad C, McMillan J, Gendelman HE. Neuropathogenesis of human immunodeficiency virus infection. Handb Clin Neurol. 2018;152:21–40. 10.1016/B978-0-444-63849-6.00003-7 . [DOI] [PubMed] [Google Scholar]
- 71.Kaul M, Zheng J, Okamoto S, Gendelman HE, Lipton SA. HIV-1 infection and AIDS: consequences for the central nervous system. Cell Death Differ. 2005;12 Suppl 1:878–92. 10.1038/sj.cdd.4401623 . [DOI] [PubMed] [Google Scholar]
- 72.Beattie EC, Stellwagen D, Morishita W, Bresnahan JC, Ha BK, Von Zastrow M, et al. Control of synaptic strength by glial TNFalpha. Science. 2002;295(5563):2282–5. 10.1126/science.1067859 . [DOI] [PubMed] [Google Scholar]
- 73.Stellwagen D, Beattie EC, Seo JY, Malenka RC. Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J Neurosci. 2005;25(12):3219–28. 10.1523/JNEUROSCI.4486-04.2005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stellwagen D, Malenka RC. Synaptic scaling mediated by glial TNF-alpha. Nature. 2006;440(7087):1054–9. 10.1038/nature04671 . [DOI] [PubMed] [Google Scholar]
- 75.Brewer GJ. Serum-free B27/neurobasal medium supports differentiated growth of neurons from the striatum, substantia nigra, septum, cerebral cortex, cerebellum, and dentate gyrus. Journal of neuroscience research. 1995;42(5):674–83. 10.1002/jnr.490420510 . [DOI] [PubMed] [Google Scholar]
- 76.Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath PD, et al. The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85(7):1135–48. . [DOI] [PubMed] [Google Scholar]
- 77.Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, et al. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381(6584):661–6. 10.1038/381661a0 . [DOI] [PubMed] [Google Scholar]
- 78.Alkhatib G, Combadiere C, Broder CC, Feng Y, Kennedy PE, Murphy PM, et al. CC CKR5: a RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996;272(5270):1955–8. . [DOI] [PubMed] [Google Scholar]
- 79.Doranz BJ, Rucker J, Yi Y, Smyth RJ, Samson M, Peiper SC, et al. A dual-tropic primary HIV-1 isolate that uses fusin and the beta-chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors. Cell. 1996;85(7):1149–58. . [DOI] [PubMed] [Google Scholar]
- 80.Dragic T, Litwin V, Allaway GP, Martin SR, Huang Y, Nagashima KA, et al. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;381(6584):667–73. 10.1038/381667a0 . [DOI] [PubMed] [Google Scholar]
- 81.Feng Y, Broder CC, Kennedy PE, Berger EA. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272(5263):872–7. . [DOI] [PubMed] [Google Scholar]
- 82.Berson JF, Long D, Doranz BJ, Rucker J, Jirik FR, Doms RW. A seven-transmembrane domain receptor involved in fusion and entry of T-cell-tropic human immunodeficiency virus type 1 strains. J Virol. 1996;70(9):6288–95. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jones G, Power C. Regulation of neural cell survival by HIV-1 infection. Neurobiology of disease. 2006;21(1):1–17. 10.1016/j.nbd.2005.07.018 . [DOI] [PubMed] [Google Scholar]
- 84.Ohagen A, Devitt A, Kunstman KJ, Gorry PR, Rose PP, Korber B, et al. Genetic and functional analysis of full-length human immunodeficiency virus type 1 env genes derived from brain and blood of patients with AIDS. J Virol. 2003;77(22):12336–45. 10.1128/JVI.77.22.12336-12345.2003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kaul M, Garden GA, Lipton SA. Pathways to neuronal injury and apoptosis in HIV-associated dementia. Nature. 2001;410(6831):988–94. 10.1038/35073667 . [DOI] [PubMed] [Google Scholar]
- 86.Gorry PR, Bristol G, Zack JA, Ritola K, Swanstrom R, Birch CJ, et al. Macrophage tropism of human immunodeficiency virus type 1 isolates from brain and lymphoid tissues predicts neurotropism independent of coreceptor specificity. J Virol. 2001;75(21):10073–89. 10.1128/JVI.75.21.10073-10089.2001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kramer-Hammerle S, Rothenaigner I, Wolff H, Bell JE, Brack-Werner R. Cells of the central nervous system as targets and reservoirs of the human immunodeficiency virus. Virus Res. 2005;111(2):194–213. 10.1016/j.virusres.2005.04.009 . [DOI] [PubMed] [Google Scholar]
- 88.Lindl KA, Marks DR, Kolson DL, Jordan-Sciutto KL. HIV-associated neurocognitive disorder: pathogenesis and therapeutic opportunities. J Neuroimmune Pharmacol. 2010;5(3):294–309. 10.1007/s11481-010-9205-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu Y, Liu H, Kim BO, Gattone VH, Li J, Nath A, et al. CD4-independent infection of astrocytes by human immunodeficiency virus type 1: requirement for the human mannose receptor. J Virol. 2004;78(8):4120–33. 10.1128/JVI.78.8.4120-4133.2004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Biard-Piechaczyk M, Robert-Hebmann V, Richard V, Roland J, Hipskind RA, Devaux C. Caspase-dependent apoptosis of cells expressing the chemokine receptor CXCR4 is induced by cell membrane-associated human immunodeficiency virus type 1 envelope glycoprotein (gp120). Virology. 2000;268(2):329–44. 10.1006/viro.1999.0151 . [DOI] [PubMed] [Google Scholar]
- 91.Bagetta G, Corasaniti MT, Aloe L, Berliocchi L, Costa N, Finazzi-Agro A, et al. Intracerebral injection of human immunodeficiency virus type 1 coat protein gp120 differentially affects the expression of nerve growth factor and nitric oxide synthase in the hippocampus of rat. Proc Natl Acad Sci U S A. 1996;93(2):928–33. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bansal AK, Mactutus CF, Nath A, Maragos W, Hauser KF, Booze RM. Neurotoxicity of HIV-1 proteins gp120 and Tat in the rat striatum. Brain research. 2000;879(1–2):42–9. . [DOI] [PubMed] [Google Scholar]
- 93.Acquas E, Bachis A, Nosheny RL, Cernak I, Mocchetti I. Human immunodeficiency virus type 1 protein gp120 causes neuronal cell death in the rat brain by activating caspases. Neurotox Res. 2004;5(8):605–15. . [DOI] [PubMed] [Google Scholar]
- 94.Bachis A, Mocchetti I. Brain-derived neurotrophic factor is neuroprotective against human immunodeficiency virus-1 envelope proteins. Annals of the New York Academy of Sciences. 2005;1053:247–57. 10.1196/annals.1344.022 . [DOI] [PubMed] [Google Scholar]
- 95.Polianova MT, Ruscetti FW, Pert CB, Ruff MR. Chemokine receptor-5 (CCR5) is a receptor for the HIV entry inhibitor peptide T (DAPTA). Antiviral Res. 2005;67(2):83–92. 10.1016/j.antiviral.2005.03.007 . [DOI] [PubMed] [Google Scholar]
- 96.Donzella GA, Schols D, Lin SW, Este JA, Nagashima KA, Maddon PJ, et al. AMD3100, a small molecule inhibitor of HIV-1 entry via the CXCR4 co-receptor. Nature medicine. 1998;4(1):72–7. . [DOI] [PubMed] [Google Scholar]
- 97.Lazarini F, Casanova P, Tham TN, De Clercq E, Arenzana-Seisdedos F, Baleux F, et al. Differential signalling of the chemokine receptor CXCR4 by stromal cell-derived factor 1 and the HIV glycoprotein in rat neurons and astrocytes. The European journal of neuroscience. 2000;12(1):117–25. . [DOI] [PubMed] [Google Scholar]
- 98.Bachis A, Aden SA, Nosheny RL, Andrews PM, Mocchetti I. Axonal transport of human immunodeficiency virus type 1 envelope protein glycoprotein 120 is found in association with neuronal apoptosis. J Neurosci. 2006;26(25):6771–80. 10.1523/JNEUROSCI.1054-06.2006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Contento RL, Molon B, Boularan C, Pozzan T, Manes S, Marullo S, et al. CXCR4-CCR5: a couple modulating T cell functions. Proc Natl Acad Sci U S A. 2008;105(29):10101–6. 10.1073/pnas.0804286105 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Molon B, Gri G, Bettella M, Gomez-Mouton C, Lanzavecchia A, Martinez AC, et al. T cell costimulation by chemokine receptors. Nat Immunol. 2005;6(5):465–71. 10.1038/ni1191 . [DOI] [PubMed] [Google Scholar]
- 101.Wood BA, Carver S, Troyer RM, Elder JH, VandeWoude S. Domestic cat microsphere immunoassays: detection of antibodies during feline immunodeficiency virus infection. J Immunol Methods. 2013;396(1–2):74–86. 10.1016/j.jim.2013.08.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.de Parseval A, Chatterji U, Morris G, Sun P, Olson AJ, Elder JH. Structural mapping of CD134 residues critical for interaction with feline immunodeficiency virus. Nat Struct Mol Biol. 2005;12(1):60–6. 10.1038/nsmb872 . [DOI] [PubMed] [Google Scholar]
- 103.de Parseval A, Grant CK, Sastry KJ, Elder JH. Sequential CD134-CXCR4 interactions in feline immunodeficiency virus (FIV): soluble CD134 activates FIV Env for CXCR4-dependent entry and reveals a cryptic neutralization epitope. J Virol. 2006;80(6):3088–91. 10.1128/JVI.80.6.3088-3091.2006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Piccinelli AC, Morato PN, Dos Santos Barbosa M, Croda J, Sampson J, Kong X, et al. Limonene reduces hyperalgesia induced by gp120 and cytokines by modulation of IL-1 beta and protein expression in spinal cord of mice. Life Sci. 2017;174:28–34. 10.1016/j.lfs.2016.11.017 . [DOI] [PubMed] [Google Scholar]
- 105.Akerboom J, Chen TW, Wardill TJ, Tian L, Marvin JS, Mutlu S, et al. Optimization of a GCaMP Calcium Indicator for Neural Activity Imaging. J Neurosci. 2012;32(40):13819–40. Epub 2012/10/05. 10.1523/JNEUROSCI.2601-12.2012 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An example of time-lapse images and their responses. A scale bar indicates 10 μm.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that a higher dose of DL-APV completely blocks Ca2+ activity in both control and gp95-treated neurons, while a lower dose of DL-APV selectively inhibits the gp95 effects (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (5,304) = 9.238). A scale bar indicates 20 seconds. LSD, Least Significant Difference; NMDAR, NMDA receptor.
(TIF)
The quality of synaptosomes used in Fig 4A and 4B has been monitored by immunoblots of synaptic proteins in sequential fractions showing that synaptic proteins such as GluA2, PSD95, and synaptophysin are highly enriched in the synaptosome fractions. PSD95, postsynaptic density 95.
(TIF)
Representative immunoblots and quantitative analysis of surface biotinylation in each condition showing that gp95 has no effect on surface expression of (A) GluA2 (n = 12 experiments) and (B) NR1 (n = 5 experiments, CTRL). Actin is used as an intracellular negative control and absent in the biotinylated samples.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that a higher dose of CNQX completely blocks Ca2+ activity in both control and gp95-treated neurons, while a lower dose of CNQX selectively inhibits the gp95 effects. Furthermore, lower doses of DL-APV and CNQX in combination completely inhibited Ca2+ activity in both control and gp95-treated neurons, suggesting that inhibition of both receptors induces additive effects on Ca2+ activity (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, F (7,179) = 5.933). A scale bar indicates 20 seconds. AMPAR, AMPA receptor; CNQX, 6-Cyano-7-nitroquinoxaline-2,3-dione; LSD, Least Significant Difference.
(TIF)
Representative traces of GCaMP5 fluorescence intensity and a summary graph of the normalized average of total Ca2+ activity in each condition showing that inhibition of (A) neuronal activity by TTX and (B) L-type Ca2+ channels abolish GCaMP5 activity in both control and gp95-treated neurons (n = number of neurons, ****p < 0.0001, one-way ANOVA, uncorrected Fischer’s LSD, (A) F (3,220) = 25.61 and (B) F (3,206) = 17.17). A scale bar indicates 20 seconds. LSD, Least Significant Difference; TTX, tetrodotoxin.
(TIF)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.