Abstract
OBJECTIVE.
In 2013, a multidisciplinary group at our Veterans Administration hospital collaborated to improve the diagnosis and treatment of patients with acute cholecystitis (AC) at our facility. Our role in this project was to evaluate the diagnostic accuracies of ultrasound (US) and CT.
MATERIALS AND METHODS.
AC was diagnosed in 60 patients (62 patient encounters) between July 1, 2013, and July 1, 2015. Of these patients, 56 underwent US, 48 underwent CT, and 42 underwent both. For the same time period, 60 patients without AC underwent US and 60 patients without AC underwent CT, and these imaging studies served as comparison studies. The groups were combined for a total of 182 unique patient encounters. A single radiologist reviewed the studies and tabulated the data.
RESULTS.
The sensitivity of CT for detecting AC was significantly greater than that of US: 85% versus 68% (p = 0.043), respectively; however, the negative predictive values of CT and US did not differ significantly: 90% versus 77% (p = 0.24–0.26). Because there were no false-positives, the specificity and positive predictive values for both modalities were 100%. Among the 42 patients who underwent CT and US, both modalities were positive for AC in 25 patients, CT was positive and US was negative in 10 patients, and US was positive and CT was negative in two patients; in five patients, both US and CT were negative.
CONCLUSION.
CT was significantly more sensitive for diagnosing AC than US. CT and US are complementary, and the other modality should be considered if there is high clinical suspicion for AC and the results of the first examination are negative.
Keywords: acute cholecystitis, CT, quality improvement, ultrasound, Veterans Administration medical center
Approximately one-third of people with cholelithiasis will develop acute cholecystitis (AC), and 90–95% of patients with AC have gallstones. Calculous AC occurs secondary to calculous obstruction of the cystic duct, increased intraluminal pressure and distention of the gallbladder, and irritation of the gallbladder wall by bile breakdown products, infection, or prostaglandins [1, 2]. If obstruction of the cystic duct and mural inflammation persist, vascular compromise, necrosis, and perforation may develop [3].
More than 90% of patients in surgical wards are seen for one or more of the following conditions: acute appendicitis, AC, small-bowel obstruction, urinary colic, perforated peptic ulcer, acute pancreatitis, acute diverticular disease, and nonspecific non-surgical abdominal pain [4]. Of these conditions, AC is the most common cause of right upper quadrant abdominal pain. However, assessment of more than one-third of patients initially suspected of having AC will result in an alternative diagnosis [2].
Imaging is often useful because it aids in making the correct diagnosis of AC; decreases time to diagnosis, thus reducing the likelihood of complications; and reveals complications such as gangrenous cholecystitis and perforation, which can be life-threatening [5]. Ultrasound (US) is considered the first-line imaging modality in evaluating AC. The reported sensitivity and specificity of US range from 50% to 100% and from 33% to 100%, respectively, with summary estimates of 81% and 83% [6]. The use of CT in evaluating for AC has increased despite the paucity of evidence concerning its diagnostic accuracy for AC. A comprehensive meta-analysis published in 2012 [6] could not summarize the diagnostic accuracy of CT because only one study could be included. In addition, only a limited number of studies are available that evaluate a head-to-head comparison of CT and US in this setting [6]. Our portion of the quality improvement project included a retrospective study comparing the diagnostic accuracies of US and CT among patients with AC at our hospital. Our results include an overall evaluation of the quality improvement project. This work was originally presented at the Society of Abdominal Radiology 2016 Annual Scientific Meeting and Educational Course, and the abstract was published in Abdominal Radiology [7].
Materials and Methods
This study was part of the Specialty and Surgical Care Collaborative (SSCC) at the Veterans Administration (VA). Surgeons, emergency medicine physicians, hospitalists, and radiologists at the Raymond G. Murphy VA Medical Center in Albuquerque, NM, collaborated on this quality improvement project. For our retrospective study, the patients were being cared for as part of the SSCC. From July 1, 2013, to July 1, 2015, AC was diagnosed in 62 patient encounters, with two patients being studied twice. US was performed at 56 (90%) of these patient encounters and CT at 48 (77%). CT was performed without contrast material secondary to poor renal function in 11 patients (23%), and CT was performed with contrast material in 37 patients (77%).
Sixty right upper quadrant US examinations and 60 CT examinations from the same time period of different patients with an indication for imaging of abdominal pain were randomly selected for a comparison population. The demographic characteristics of the comparison group were similar to those of the AC group. The AC and comparison examinations were combined and randomized. A single radiologist with more than 20 years of experience reviewed the studies and tabulated the data. The quality of each US examination based on visualization of the entire gallbladder and gallbladder neck was graded as excellent, fair, or poor.
The following findings were recorded for each US study: gallstones; gallbladder distention (defined as > 4 cm in transverse dimension), gallbladder wall thickening (defined as > 3 mm), pericholecystic fluid; “Murphy” sign, common bile duct dilatation (defined as > 6 mm), and presence of so-called “dirty shadowing,” which is a finding that is concerning for air within the gallbladder lumen or wall. These criteria were retrospectively recorded as positive or negative for AC, and the initial reported interpretation was recorded as positive or negative for AC.
The following findings were recorded for each CT study: presence of IV contrast material, gallstones, gallbladder distention (defined as > 4 cm in transverse dimension), gallbladder wall thickening (defined as > 3 mm), pericholecystic inflammation, pericholecystic fluid, increased enhancement of the adjacent liver, common bile duct dilatation (defined as > 6 mm), choledocholithiasis, indistinct gallbladder wall, increased gallbladder wall attenuation, air within the gallbladder lumen or wall, and poor gallbladder wall enhancement. These findings were retrospectively positive or negative for AC, and the initial reported interpretation was recorded as positive or negative for AC. A positive retrospective diagnosis of AC was made on the basis of the presence of at least two of the mentioned findings, although no specific set of findings was used to make the diagnosis of AC.
Helical CT was performed on 16- and 64-MDCT scanners using a 3-mm collimation. The patients who received IV contrast material were administered 100 mL of iopromide 300 (Ultravist 300, Bayer Healthcare) at a rate of 3 mL/s. US examinations were performed by one of four US technologists with 14–20 years of experience using a US unit (Logiq 9, GE Healthcare). Color-flow Doppler imaging was used at the technologist’s discretion.
The clinical services physicians used the Tokyo Guidelines [8] as part of their practice management and as a tool to involve general surgeons earlier in the triage and treatment of patients with AC. According to an algorithm developed in collaboration with general surgeons, general internal medicine physicians, and gastroenterology physicians, patients with AC underwent surgery for cholecystectomy, underwent an interventional radiology procedure for cholecystostomy tube placement, or received medical management on the internal medicine service. In most cases, the decision about which therapy to use was based on the comorbid diagnoses of the patients and the preoperative evaluation of risk. When no fluid sample from the cholecystostomy tube or surgical tissue was available, then the diagnosis was made using primarily clinical and radiologic criteria. Clinical diagnosis and treatment were obtained through a chart review of each patient.
Results
Sixty patients, 56 men and four women, with AC who underwent imaging between July 1, 2013, and July 1, 2015, were included retrospectively in our study. The study group ranged in age from 31 to 94 years (mean, 66 years). Of the 62 patient encounters (two patients treated twice), 32 (52%) were treated with cholecystectomy, 18 (29%) with cholecystostomy tubes, and 12 (19%) medically. Treatment was clinically directed depending on comorbidities. The mean time from imaging to treatment with cholecystectomy was 3.1 days. Eighteen patients underwent surgery within 24 hours of imaging; nine patients, 1–2 days after imaging; four patients, 4–10 days after imaging; and one patient, 43 days after imaging. The mean time from imaging to treatment with cholecystostomy tube placement was 2.1 days. Ten patients had a cholecystotomy tube placed within 24 hours after imaging, three at 1–2 days after imaging, and five at 3–6 days after imaging.
Of the 62 patient encounters, 14 patients (23%) underwent only US, six patients (10%) underwent only CT, and 42 patients (68%) underwent both US and CT (Fig. 1). When both examinations were performed, they occurred within 48 hours of each other except in one patient, whose US and CT examinations occurred within 72 hours of each other and the findings were concordant. Nine patients underwent US first (21%), and 33 patients underwent CT first (79%).
Fig. 1—
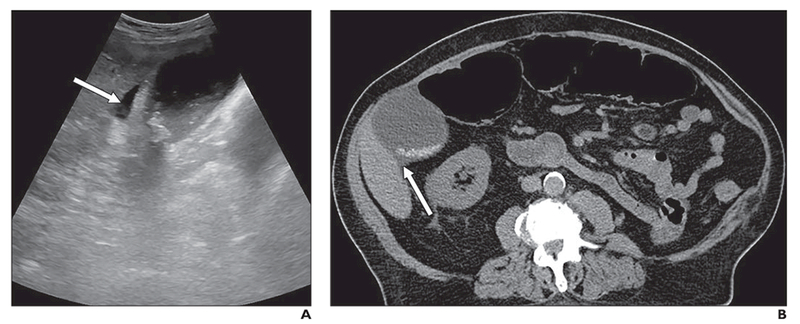
Acute calculous cholecystitis in 84-year-old man with end-stage renal disease, diabetes mellitus type 2, hypertension, and history of renal cell carcinoma and prostate cancer. Patient presented to emergency department with abdominal pain and constipation.
A and B, Ultrasound (A) and CT (B) images show cholelithiasis, gallbladder distention and wall thickening, and pericholecystic fluid (arrow). Sonographic “Murphy” sign was positive. Because of multiple comorbidities, patient was poor surgical candidate and was treated medically.
Of the 62 patient encounters, 40 patients (65%) underwent CT as the first or only imaging examination. Of these 40 patients, 35 were seen in the emergency department (ED) and five were inpatients; three (7.5%) had AC as the primary differential consideration, whereas 37 (92.5%) had an alternative primary differential diagnosis. Twenty-two patients (35%) underwent US as the first or only imaging examination. Of these 22 patients, 20 were seen in the ED and two were inpatients; 20 (91%) had AC as the primary differential consideration, and two (9%) had an alternative primary differential diagnosis.
US had a sensitivity of 68% (38/56) and negative predictive value (NPV) of 77% (60/78). CT had a sensitivity of 85% (41/48) and an NPV of 90% (60/67). There were no false-positives in either group, yielding specificity and positive predictive values (PPVs) of 100%. CT and US both correctly made the diagnosis of AC in 25 of the 42 patients (60%) who underwent both US and CT (Fig. 1). The diagnosis of AC was made on CT and not on US in 10 patients (24%) (Fig. 2). The opposite was true in two patients (5%) with AC diagnosed on US and missed on CT (Fig. 3). AC was missed on both CT and US in five patients (12%). Of these five patients, the diagnosis of AC was confirmed on cholescintigraphy in three patients and at surgery in one patient, and one patient was treated medically.
Fig. 2—
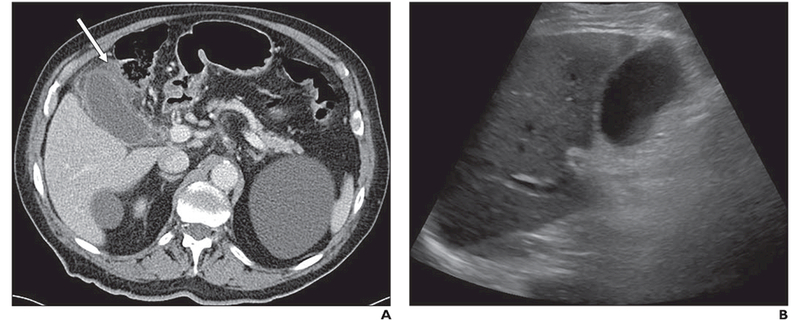
Acute acalculous cholecystitis in 85-year-old man who presented to emergency department with 2-day history of cramping right upper guadrant pain, which worsened with eating, and nausea.
A, CT image shows pericholecystic inflammation (arrow), wall thickening, and gallbladder distention.
B, Ultrasound image obtained before CT but on same day as CT is occult for acute cholecystitis. Cholecystectomy was subseguently performed.
Fig. 3—
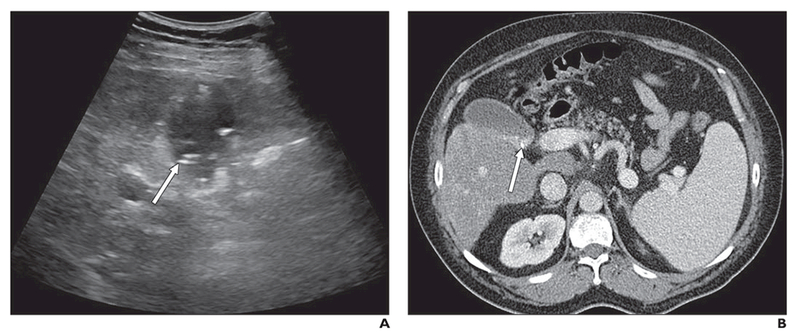
Acute calculous cholecystitis in 53-year-old man who presented to emergency department with recurrent postprandial right upper guadrant abdominal pain and tenderness.
A, Ultrasound image shows gallbladder wall thickening and cholelithiasis (arrow). Sonographic “Murphy” sign was positive.
B, Cholelithiasis (arrow) is evident on CT image obtained later same day as ultrasound (A); however, there are no other CT findings suggestive of acute cholecystitis.
Patient was not good surgical candidate secondary to alcoholic cirrhosis and thrombocytopenia and was treated medically.
Using the sensitivity data from the set of 42 patients in the AC group who underwent both US and CT, the McNemar test of concordance-discordance was significant (p = 0.043), some what in favor of CT. To compare the NPVs of US and CT, we used patients who underwent either US or CT, not both. The US data of this group consisted of the 60 non-AC cases and 14 AC cases who underwent US only. The CT data of this group consisted of the 60 non-AC cases and six AC cases who underwent CT only. Among these AC cases, the diagnosis of AC was missed on US in three patients and on CT in 0 patients. Both the Fisher test and the chi-square test for two proportions showed a lack of a significant difference in the NPVs (p = 0.24 and 0.26, respectively).
Review of the reports from the initial examination interpretations showed a sensitivity of 71% and NPV of 80% for the US examinations and a sensitivity of 73% and NPV of 82% for CT. As with the retrospective analysis, there were no false-positives.
There was pathology or imaging evidence of gangrenous cholecystitis in 11 cases and emphysematous cholecystitis in nine cases. Acute cholecystitis was without evidence of complication in 48 cases. The most common finding of AC in the US group was gallbladder wall thickening (77% of patients) followed by cholelithiasis (68%) and gallbladder distention (59%) (Table 1). In contrast, the most common findings in the CT group were gallbladder distention (75%) and pericholecystic inflammation (75%) followed by gallbladder wall thickening (65%) (Table 2).
TABLE 1:
Ultrasound (US) Findings in 56 Patients With Acute Cholecystitis
| US Finding | No. (%) of Patients |
|---|---|
| Gallstones | 38 (68) |
| Gallbladder distention (> 4 cm) | 33 (59) |
| Thickened gallbladder wall (> 3 mm) | 43 (77) |
| Pericholecystic fluid | 29 (52) |
| Positive sonographic “Murphy” sign | 12 (21) |
| Common bile duct dilatation (> 6 mm) | 12 (21) |
| Air in gallbladder wall or lumen | 4 (7) |
TABLE 2:
CT Findings in 48 Patients With Acute Cholecystitis
| CT Findings | No. (%) of Patients |
|---|---|
| CT findings independent of contrast material (n = 48) | |
| Gallstones | 29 (60) |
| Gallbladder distention (> 4 cm) | 36 (75) |
| Thickened gallbladder wall (> 3 mm) | 31 (65) |
| Pericholecystic inflammation | 36 (75) |
| Pericholecystic fluid | 25 (52) |
| Air in gallbladder wall or lumen | 3 (6) |
| Common bile duct dilatation (> 6 mm) | 11 (23) |
| Choledocholithiasis | 1 (2) |
| Increased attenuation of the gallbladder wall | 5 (10) |
| Contrast-enhanced findings (n = 37) | |
| Poor gallbladder wall enhancement | 27 (73) |
| Increased pericholecystic hepatic enhancement | 3 (8) |
| Unenhanced finding (n = 11) | |
| Indistinct gallbladder wall | 7 (64) |
Gallstones were present at surgery or pathology in 24 of the 32 surgically treated patients. Five of the eight patients without gallstones identified at surgery or pathology had stones seen on imaging. Stones were seen on six CT examinations and were not detected on US. The opposite was true in eight examinations in which stones not apparent on CT were detected on US. One CT examination was false-positive for cholelithiasis because the reviewer misinterpreted enhancing vessels as stones.
Eighteen (32%) of the US examinations were graded excellent quality; 22 (39%), fair; and 16 (29%), poor. The quality of the US examinations in the comparison group were similar to the AC group. Eighteen of the US examinations in the AC group did not show findings concerning for AC: three (17%) were graded excellent; four (22%), fair; and 11 (61%), poor. Of the 48 CT examinations in the AC group, 37 were performed with IV contrast material and 11 without contrast material. The results of seven of the CT examinations were false-negative for AC, and IV contrast material had been used in all seven of these CT examinations.
Discussion
Several factors make the veteran population in our quality improvement project different from the random populations with AC in most studies. Although gallstones and cholecystitis are more prevalent in women [9], the veteran population is unique in that most of the VA’s patients are male, leading to an overwhelmingly high ratio of male-to-female patients. During the study period at the Raymond G. Murphy VA Medical Center, there were 60 patients with a diagnosis of AC. The age range for this group was 31 to 94 years old with a mean age of 66 years. The distribution of patients by sex was 56 men and four women. The fact that the population was skewed toward older and male patients presented a number of challenges. Only a minority of patients presented with a typical picture of right upper quadrant pain, fever, nausea, vomiting and anorexia. Most presented with a variety of complaints including but not limited to chest pain, vague abdominal pain, anorexia, isolated fevers, and back pain. Although the studies in the literature suggest that US is the most appropriate initial test for AC, the atypical presentations at our VA facility led to a higher incidence of CT as the initial radiologic test ordered.
In our study, 52% of patients with the diagnosis of AC underwent surgery, 29% had a cholecystostomy tube placed, and 19% were treated with medical management only. As mentioned in Appendix 1, in the third year of our study, the surgeons operated on 89% of the patients. Most of the treatment decision was based on the comorbid diagnoses of the patient and the preoperative evaluation of risk. When no surgical tissue was obtained or no fluid was drained from the cholecystostomy tube, then the AC diagnosis was made using clinical and radiologic criteria.
The goals of creating the practice guidelines were to decrease the length of hospital stay and time to surgery in patients with AC. Analyzing the data from the first 2 years after the creation of the practice guidelines, the mean time to surgery has improved from 60.0 to 26.7 hours. The length of hospital stay for AC has decreased from a mean of 5.6 to 4.2 days. As part of this study, the surgery department asked the ED physicians to call the surgery department when patients present with upper abdominal pain instead of admitting them directly to the department of medicine. Before our study, up to 70% of patients were being admitted to the department of medicine first before the department of surgery was called. By creating a practice guideline, which begins with presentation to the ED and was cocreated by the departments of internal medicine and general surgery, we found a significant decrease in both time to surgery and length of hospital stay. These improvements were enhanced by the surgery department increasing available operation times including nights, weekends, and holidays.
US is the initial imaging modality of choice when AC is suspected clinically. Advantages include its widespread availability, lack of ionizing radiation, rapid time to image acquisition, and relatively low cost. Another advantage of US is its ability to diagnose AC on the basis of the presence of the Murphy sign. The Murphy sign is a useful tool, in conjunction with cholelithiasis, having a PPV for AC of 92% [10]. Cholescintigraphy has been shown to have a higher sensitivity and specificity for AC than US and CT [6]. Cholescintigraphy is generally reserved for ambiguous cases because of logistic issues and the relatively long examination time. A lengthy examination is prohibitive because many patients undergoing evaluation for AC are seen in the ED where rapid diagnosis is necessitated. CT is also easily accessible and can be completed rapidly, although its drawbacks include ionizing radiation and high cost. CT is often used to evaluate patients with an unclear clinical presentation, wide differential diagnosis, and pain not solely localized to the right upper quadrant [1].
Heavy utilization of CT in this study is noted, with CT being performed as the first or only imaging study in 40 of the 62 (65%) patient encounters. Most of these patients (37/40, 93%) presented with a variety of complaints such as chest pain, vague abdominal pain, anorexia, isolated fevers, and back pain. When AC was initially clinically suspected, US was usually performed first (20/23, 87%).
The reported sensitivity of US for AC (81%) [6] is greater than that seen in our study (68%). The decreased sensitivity of US in this study may be secondary to the unique patient population of the VA. Although gallstones and cholecystitis are more prevalent in the female population [9], our study population was composed of mostly men (56 men and four women), often of elderly and obese patients, potentially leading to poor-quality examinations (29%). Additionally, the US service is run by body and general radiologists as opposed to dedicated US radiologists, and many examinations were interpreted after hours without a radiologist available in house, so interpretations were performed by teleradiologists. These factors may also contribute to the statistically significant increased sensitivity of CT (85%) compared with US.
Limitations of this study are noted. The radiologist reviewing the studies knew that the studies were of patients with AC and patients without AC, creating a potential retrospective bias. The AC and normal examinations were randomly combined, and prospective reports were blinded to reduce this bias. It is unlikely that the results were significantly affected given that the sensitivity and NPV of the original interpretations were higher than those of the retrospective evaluation. This difference in sensitivities and NPVs is understandable because the original readers had the results of prior examinations, whereas the retrospective reader did not. There were no false-positive examinations, yielding a specificity of 100% for US and CT. Historically, wide ranges of sensitivities (50–100%) and specificities (33–100%) have been reported in the literature [6]. Comparing the sensitivity and NPV of CT and US in evaluating AC was limited by the small sample sizes. The number of false-positives among patients who underwent either US or CT, but not both, was too low to be certain whether there was a true difference between the NPVs.
Although several signs of AC have been studied [11], a consensus has not yet been made for the exact imaging definition of a positive examination. Twenty-six studies from a fairly recent meta-analysis gave at least 14 different definitions for a positive examination on US [6]. Major and minor criteria have been proposed with a resulting decrease in sensitivity [12]. The Tokyo Guidelines [8] have been widely adopted for the clinical diagnosis of AC. The guidelines incorporate a combination of local signs of inflammation, such as right upper quadrant pain and a positive Murphy sign; systemic signs of inflammation, including elevated C-reactive protein value, WBC count, and fever; and imaging findings suggestive of AC. CT, US, or cholescintigraphy is necessary to make a definitive diagnosis of AC [8].
Multiple studies have recommended further evaluation with CT when AC is suspected clinically and the initial US study is equivocal, negative, or limited by obesity or gaseous distention. The opposite is also true—that is, US is recommended to further evaluate a patient with equivocal or negative CT findings when AC is suspected clinically [12, 13]. Also, because CT will fail to detect up to 20% of patients who have gallstones, if CT shows findings of AC without gallstones, we recommend US.
Conclusion
The sensitivity of US (68%) and CT (85%) for AC were not as good as sensitivities reported in prior studies: 81% for US and 94% for CT [6]. CT at our institution was statistically significantly better for the diagnosis of AC than US, most likely because of an unclear clinical picture, the patient population, and a high proportion of poor-quality US examinations. However, US is still our first test of choice if AC is suspected clinically, whereas CT is performed when the clinical picture is unclear. US and CT are complementary: If the initial test is negative and there is clinical suspicion of AC or if the initial examination is equivocal, the other examination should be performed. In our practice if both studies are negative for AC and clinical suspicion is high for AC, hepatoiminodiacetic acid scanning is performed.
Acknowledgment
We thank Yiliang Zhu (of the University of New Mexico Department of Internal Medicine; Division of Epidemiology, Biostatistics and Preventive Medicine; and Clinical & Translational Science Center) for providing statistical support for this study.
Supported by the National Institutes of Health (grant no. UL1TR001449).
APPENDIX 1: Results for the Third Year of This Study
Because of the time it took us to prepare this work, we were able to counsel our sonographers on examining the gallbladder to include imaging deep within the abdomen, enabling visualization of the gallbladder neck. We were also able to examine ultrasound (US) studies and CT studies performed from July 1, 2015, to June 30, 2016, of 35 additional patients. Compared with the first 2 years of our study, the quality of the US examinations improved to excellent for 42% of the examinations for this latter group versus 32% of the examinations for our study group; fair, 42% versus 39%; and poor, 26% versus 29%. The sensitivity of US for acute cholecystitis (AC) improved from 68% to 74%. Interestingly, the sensitivity of CT for AC also improved from 85% to 89%. Surgeons also became more aggressive and operated on 31 of 35 (89%) patients compared with 32 of 60 (53%) patients in the first 2 years of our study.
Footnotes
Based on a presentation at the Society of Abdominal Radiology 2016 annual meeting, Waikoloa, HI.
References
- 1.Shakespear JS, Shaaban AM, Rezvani M. CT findings of acute cholecystitis and its complications. AJR 2010; 194:1523–1529 [DOI] [PubMed] [Google Scholar]
- 2.Hanbidge AE, Buckler PM, O’Malley ME, Wilson SR. From the RSNA refresher courses: imaging evaluation for acute pain in the right upper quadrant. Radio Graphics 2004; 24:1117–1135 [DOI] [PubMed] [Google Scholar]
- 3.Charalel RA, Jeffrey RB, Shin LK. Complicated cholecystitis: the complementary roles of sonography and computed tomography. Ultrasound Q 2011; 27:161–170 [DOI] [PubMed] [Google Scholar]
- 4.Marincek B Nontraumatic abdominal emergencies: acute abdominal pain—diagnostic strategies. Eur Radiol 2002; 12:2136–2150 [DOI] [PubMed] [Google Scholar]
- 5.Menu Y, Vuillerme MP. Non-traumatic abdominal emergencies: imaging and intervention in acute biliary conditions. Eur Radiol 2002; 12:2397–2406 [DOI] [PubMed] [Google Scholar]
- 6.Kiewiet JJ, Leeuwenburgh MM, Bipat S, Bossuyt PM, Stoker J, Boermeester MA. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology 2012; 264:708–720 [DOI] [PubMed] [Google Scholar]
- 7. Kielar AZ, Sirlin CB, Ash R, et al. Scientific paper abstracts presented at the society of abdominal radiology 2016 annual scientific meeting and educational course march 13–18, 2016, Waikoloa, Hawaii. Abdom Radiol (NY) 2016; 41:1670–1694 [DOI] [PubMed] [Google Scholar]
- 8.Yokoe M, Takada T, Strasberg SM, et al. ; Tokyo Guidelines Revision Committee. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2013; 20:35–46 [DOI] [PubMed] [Google Scholar]
- 9.Halpin V, Gupta A. Acute cholecystitis. BMJ Clin Evid 2011; 2011:0411. [PMC free article] [PubMed] [Google Scholar]
- 10.Ralls PW, Colletti PM, Lapin SA, et al. Real-time sonography in suspected acute cholecystitis: prospective evaluation of primary and secondary signs. Radiology 1985; 155:767–771 [DOI] [PubMed] [Google Scholar]
- 11.Soyer P, Hoeffel C, Dohan A, et al. Acute cholecystitis: quantitative and qualitative evaluation with 64-section helical CT. Acta Radiol 2013; 54:477–486 [DOI] [PubMed] [Google Scholar]
- 12.Fidler J, Paulson EK, Layfield L. CT evaluation of acute cholecystitis: findings and usefulness in diagnosis. AJR 1996; 166:1085–1088 [DOI] [PubMed] [Google Scholar]
- 13.Pinto A, Reginelli A, Cagini L, et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J 2013; 5(suppl 1): S11. [DOI] [PMC free article] [PubMed] [Google Scholar]


