Older adults with greater levels of purpose in life are less likely to develop type 2 diabetes or prediabetes over a 4-year follow-up compared to older adults with lower levels of purpose in life.
Keywords: Purpose in life, Hemoglobin A1c, Type 2 diabetes mellitus, Prediabetes
Abstract
Background
Greater purpose in life is associated with lower rates of certain chronic diseases. Whether purpose in life can protect against development of prediabetes or type 2 diabetes is unknown.
Purpose
To examine the association between purpose in life and blood glucose control among adults ≥50 years.
Methods
We conducted a longitudinal cohort study of 3,907 participants of the Health and Retirement Study who at baseline did not have type 2 diabetes or prediabetes. Baseline purpose in life was measured using the Ryff and Keyes’ Scales of Psychological Well-Being and grouped into tertiles (high, medium, and low). We used multivariable linear regression to examine the association between baseline purpose in life and HbA1c over 4 years. Multivariable logistic regression was used to examine the association between baseline purpose and incident prediabetes or type 2 diabetes over the same period.
Results
After adjusting for sociodemographic factors, body mass index, physical activity, and physical and mental health factors, HbA1c was 0.07 percentage points lower among participants with high purpose than those with low purpose (95% confidence interval [CI] −0.12 to −0.02; p = .011). Participants with high purpose had lower odds of developing prediabetes or type 2 diabetes than those with low purpose (adjusted odds ratio 0.78; 95% CI 0.62 to 0.98; p = .037).
Conclusions
Among older adults, greater purpose in life is associated with a lower incidence of prediabetes or type 2 diabetes. Strategies to promote greater purpose in life should be tested as a part of type 2 diabetes prevention efforts.
Introduction
Purpose in life, defined as the belief that one’s life has meaning and direction [1], is a key dimension of psychological well-being [2], and there is growing recognition of its relationship with physical health and longevity [3]. For example, individuals with greater levels of purpose have lower rates of cardiovascular disease [4], cerebrovascular disease [5, 6], sleep disturbance [7], and all-cause mortality [3]. These associations may be mediated, at least in part, by increased engagement in healthy behaviors such as physical activity [8, 9] and routine health screening [10] among individuals with greater levels of purpose. In addition, greater purpose may directly influence physiologic processes, reducing biochemical measures of stress and inflammation that are associated with the development of chronic diseases [11–13].
Despite mounting evidence of the association between purpose and lower incidence of certain chronic conditions, a key area in which the role of purpose is unknown is in the development of type 2 diabetes and its precursor, prediabetes. Understanding the association between purpose in life and blood glucose could have important public health implications given the prevalence of these conditions and their serious health consequences. Within the USA, 29 million individuals—9.3 percent of the population—have type 2 diabetes, a leading cause of cardiovascular disease, kidney disease, blindness, and lower extremity amputation [14]. An additional 86 million individuals are estimated to have prediabetes [14], and 5 to 10 percent of these individuals may develop type 2 diabetes each year [15]. Furthermore, individuals with prediabetes face an elevated risk for cardiovascular disease, stroke, and all-cause mortality compared with individuals with normal blood glucose levels [16].
Several large clinical trials have shown that type 2 diabetes can be prevented or delayed through modest lifestyle change [17–19], and evidence-based Diabetes Prevention Programs (DPPs) are now offered in communities throughout the USA [20, 21]. However, despite the now widespread availability of DPPs and national initiatives that aim to increase program engagement [22–24], the prevalence of type 2 diabetes is projected to continue to increase, with an estimated one-third of U.S. adults developing type 2 diabetes by 2050 [14]. Current strategies to prevent type 2 diabetes may be insufficient to substantially decrease the incidence of type 2 diabetes at the population level for two reasons. First, most individuals who could benefit from enrolling in a DPP do not actually do so even when one is available, thus limiting the reach of these programs [25]. Second, although a variety of biological, psychological [26], and environmental factors [27] contribute to the development of type 2 diabetes, the DPP primarily targets the biologic drivers of the disease by focusing on weight loss and physical activity [28]. This unidimensional approach fails to address important psychological factors such as depression [29], anxiety [30], and stress [31, 32] that increase the risk of type 2 diabetes and may also impede an individual’s ability to engage in healthy behaviors [33, 34]. Additional psychological factors such as purpose in life may be associated with self-efficacy to engage in healthy behaviors [35], thus playing an important role in the development of prediabetes and type 2 diabetes. Yet, it is unknown whether greater purpose in life is indeed associated with blood glucose levels. If this relationship between purpose in life and blood glucose levels exists, it could open the door to development of novel strategies to cultivate greater purpose in life as a means to decrease individuals’ risk of developing prediabetes and type 2 diabetes.
The objectives of our study were to examine the longitudinal associations between baseline purpose in life and subsequent (a) hemoglobin A1c (HbA1c) and (b) development of clinically meaningful categories of abnormal glucose metabolism (i.e., prediabetes or type 2 diabetes) among U.S. adults aged 50 years and older. We hypothesized that greater levels of purpose in life would be associated with smaller increases in HbA1c and lower rates of developing abnormal glucose metabolism compared with lower levels of purpose in life.
Methods
Participants
The Health and Retirement Study (HRS) is a longitudinal survey of a national sample of U.S. adults aged 50 years and older. Since 1992, the HRS has collected extensive data on health status, socioeconomic factors, health service utilization, labor force participation, and family structure every 2 years through telephone or in-person interviews with HRS participants or their proxies. In 2006, half of the HRS sample was randomly assigned to participate in a face-to-face interview, which was enhanced with physical measures, biological measures via blood tests (e.g., HbA1c), and a self-administered mail-back psychosocial questionnaire. The other half of the sample was interviewed by telephone in 2006 and then participated in the enhanced face-to-face interview in 2008. The interview and collection of physical and biological measures (i.e., blood tests) was repeated 4 years after their initial interview (i.e., 2010 or 2012, respectively). The full details regarding HRS recruitment procedures and participant characteristics have been previously described [36].
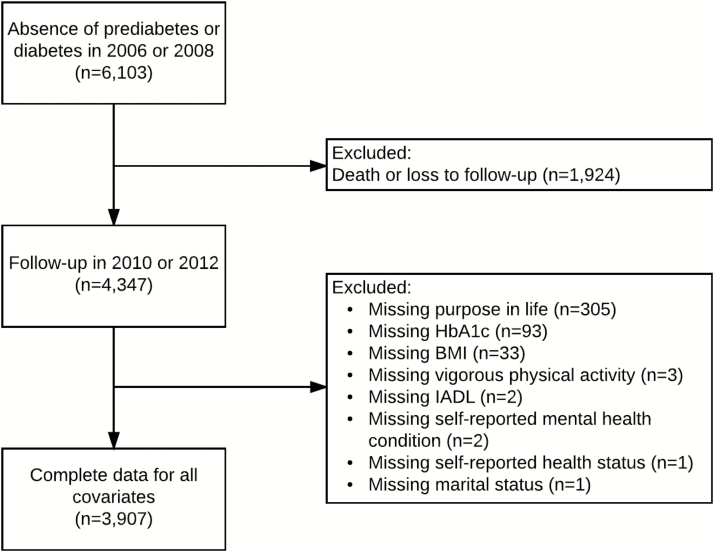
Inclusion criteria for our analytic sample were (a) having participated in the interview during 2006 or 2008 (i.e., baseline); (b) having normoglycemia (i.e,. an HbA1c < 5.7%) at baseline as defined by American Diabetes Association guidelines [37]; and (c) not self-reporting a diagnosis of type 2 diabetes at baseline (n = 6,103). Of the individuals who met the study inclusion criteria, 4,347 participated in a 4-year interview (in 2010 or 2012, respectively). We excluded from the analyses individuals who were missing an HbA1c value at 4-year follow-up and also those with missing data for any of the baseline covariates (Fig. 1). A total of 3,907 individuals were included in multivariable analyses.
Fig. 1.
Flow diagram showing cohort selection. BMI body mass index; HbA1c hemoglobin A1c; IADL instrumental activities of daily living.
Measures
Dependent variables
The primary outcomes at 4-year follow-up were (a) HbA1c and (b) incident abnormal glucose metabolism. HbA1c levels were determined by blood-spot analysis using kits from Biosafe Laboratories (Chicago, IL). Although HbA1c is a continuous measure, expert guidelines [2] specify cut points for HbA1c values to indicate clinically relevant categories of prediabetes (5.7 ≤ HbA1c < 6.5 percent) and type 2 diabetes (HbA1c ≥ 6.5 percent). Therefore, to evaluate the clinical implications of our findings, we created a dichotomous measure of abnormal glucose metabolism, defined as an HbA1c ≥ 5.7% or self-report of a type 2 diabetes diagnosis at 4-year follow-up.
Explanatory variables
Purpose in life
The main independent variable, purpose in life, was measured using a validated adaptation of Ryff and Keyes’ Scales of Psychological Well-Being [2]. The scale comprises the seven items listed in Table 1. On a six-point Likert scale ranging from “strongly disagree” to “strongly agree” respondents were asked to choose their agreement with each of the seven statements. The index score was derived by reverse coding negatively worded items and then averaging the scores across all the seven items to create a score ranging from 1 to 6. Higher scores indicate greater purpose in life (Cronbach coefficient α: 0.75).
Table 1.
Items Included in Purpose in Life Questionnairea
| 1. I enjoy making plans for the future and working to make them a reality. |
| 2. My daily activities often seem trivial and unimportant to me. |
| 3. I am an active person in carrying out the plans I set for myself. |
| 4. I don’t have a good sense of what it is I’m trying to accomplish in life. |
| 5. I sometimes feel as if I’ve done all there is to do in my life. |
| 6. I live life one day at a time and don’t really think about the future. |
| 7. I have a sense of direction and purpose in my life. |
aResponses ranged from “strongly disagree” to “strongly agree” on a six-point Likert scale; negatively worded items were reverse coded and the score was averaged across all seven items.
Among our study sample, the purpose in life scores were non-normally distributed and skewed toward higher scores, with 95 percent of the sample (3,700 individuals) having purpose scores ≥ 3. As a result, the linear relationship between baseline purpose in life and our dependent variable, HbA1c at 4-year follow-up, could not be reliably estimated across the low range of purpose scores (i.e., purpose scores < 3) because of the inadequate sample size. Additionally, to our knowledge, the interval properties of the purpose in life scale have not been established. Thus, purpose scores from this scale may be more characteristic of ordinal data [38]. We therefore created tertiles of purpose in life (categorized as high purpose, medium purpose, and low purpose) to account for (a) the non-normal distribution of purpose scores; (b) the imprecise estimate of the association between baseline purpose in life and HbA1c at 4-year follow-up at the low end of the purpose scale; and (c) the possibility of noninterval purpose scale properties.
Covariates
To evaluate the independent effect of purpose in life on the outcome measures (i.e., HbA1c and incident abnormal glucose metabolism), we adjusted for covariates including demographic and socioeconomic factors, physical health and physical functioning factors, and mental health factors, which have been previously associated with subjective well-being [39, 40] and type 2 diabetes [26, 29, 41]. All covariates included in the analysis were measured at baseline (i.e., 2006 or 2008, respectively).
Demographic and socioeconomic factors at baseline included age in years (analyzed as a continuous variable), gender, race (white/black/other), ethnicity (Hispanic/non-Hispanic), years of formal education (<12, 12, >12), spousal status (partnered/not partnered), and total household wealth (analyzed as a continuous variable).
Physical health and functioning factors at baseline included body mass index (BMI), self-reported physical activity, self-rated health (SRH), activities of daily living (ADL), and instrumental activities of daily living (IADL). We calculated BMI using the participants’ weight and height, which were measured in the interview by trained HRS research staff. Physical activity was assessed by asking participants how often (daily; > once per week; once per week; 1–3 times per month; never) they take part in sports or activities that are vigorous (e.g., jogging, swimming), moderate (e.g., gardening, dancing), or mild (e.g., vacuuming, laundry). As was done in prior research [42], we created dichotomous variables to indicate at least twice weekly engagement in each level of physical activity (i.e., vigorous activity, moderate activity, and light activity) [42], as the question responses do not reflect current physical activity guidelines [43]. We assessed SRH with responses to the question: “In general, would you say your health is excellent, very good, good, fair or poor?” We created a dichotomous measure indicative of fair/poor health status as SRH is commonly dichotomized in this way throughout the literature [44]. We also created a dichotomized indicator of having difficulty in at least one ADL and one IADL.
We used two measures to assess mental health: (a) the eight-item Center for Epidemiologic Studies Depression (CES-D) scale [45] and (b) participant self-report of having received a mental health diagnosis. The CES-D scale measures depressive symptoms using six negative and two positive items. Consistent with prior literature [46, 47], we used a cutoff of four or more symptoms to create a dichotomous variable to indicate depression. Participant self-report of having a psychiatric diagnosis was assessed by the question “Has a doctor ever told you that you have any emotional, nervous, or psychiatric problems?” and dichotomized (yes/no).
Statistical analysis
To assess whether there were significant differences in the baseline characteristics of participants across different tertiles of baseline purpose in life, we used one-way analysis of variance tests for continuous variables and Pearson’s chi-squared tests for categorical variables. To examine the relationship between different tertiles of baseline purpose in life and HbA1c at 4-year follow-up, we estimated multivariable linear regression models. To estimate the odds of transitioning from baseline normoglycemia to abnormal glucose metabolism for different tertiles of baseline purpose in life, we estimated multivariable logistic regression models.
For each type of multivariable regression model (i.e., linear or logistic), we added covariates sequentially in a series of five models. In Model 1, the only independent variables were baseline purpose in life and HbA1c. In Model 2, we added sociodemographic factors (age, gender, race, ethnicity, educational attainment, marital status, household income, and insurance status) as covariates. To assess the potential role of health conditions as mediators, in the next two models we examined whether the relationship between purpose and HbA1c weakened after inclusion of health measures into our model. Model 3 had the same independent variables as Model 2 and also adjusted for physical health and functional factors (e.g., BMI, physical activity, SRH, ADLs, IADLs). Model 4 had the same independent variables as Model 2 and also adjusted for psychological factors (e.g., CES-D score and self-reported psychiatric diagnoses). The final model (Model 5) included all covariates. All models were implemented using the SVY commands in Stata version 14.0 and sample weights to account for the complex multistage, clustered sample design and survey nonresponse. Sample weights were applied to all models. Our a priori threshold for statistical significance was p < .05.
Sensitivity analyses
Among individuals in our baseline sample who met our study inclusion criteria (n=4,347), 7% (n=305) had missing data for baseline purpose in life, whereas less than 1% had missing data for other covariates (Fig. 1). To assess the potential for bias due to missing data on baseline purpose in life, we used multiple imputation to re-estimate each regression model using imputed values for baseline purpose in life. To obtain these imputed values, we used the MI command in Stata version 14.0. We employed an ordered logit model and included all covariates as predictors in our imputation model. All analyses using the imputed data were adjusted to account for the complex multistage, clustered sample design and nonresponse and incorporated sample weights. The relationships between purpose in life and our outcome measures did not differ when we used the imputed data set in place of the complete data set, and thus, we present only the complete case analyses.
Results
Baseline Characteristics
There were significant differences in baseline characteristics across tertiles of purpose in life (Table 2). Compared to individuals with medium or low purpose in life, individuals with high purpose in life were less likely to be Hispanic (4.6% vs. 4.9% vs. 7.7%, respectively, p < .001); were more likely to have completed more than 12 years of education (38.4% vs. 35.0% vs. 25.1%; p < .001); were more likely to be partnered (78.3% vs. 74.4% vs. 68.0%; p < .001); and were more likely to have a higher mean household income, measured in 10,000 U.S. dollars (80.9 vs. 63.8 vs. 48.7; p < .001). Additionally, these individuals were more likely to engage in physical activity, including vigorous activity (36.8% vs. 31.2% vs. 22.1%; p < .001), moderate activity (71.5% vs. 63.2% vs. 56.3%; p < .001), and light activity (72.8% vs. 72.2% vs. 63.9%; p < .001); were less likely to report poor health status (9.5% vs. 14.0% vs. 26.7; p < .001); were less likely to have difficulty with at least one ADL (5.7% vs. 7.8% vs. 14.4%) or IADL (2.7% vs. 4.4% vs. 10.4%; p < .001); and were less likely to be depressed (6.2% vs. 10.2% vs. 27.4%) or self-report a mental health condition (9.5% vs. 14.0% vs. 21.9%; p < .001). There was no significant difference in baseline HbA1c across the three purpose groups (5.31 vs. 5.33 vs. 5.32; p=0.16).
Table 2.
Baseline Characteristics of the Study Population (n=3,907)
| Characteristics | Tertiles of purpose | |||
|---|---|---|---|---|
| Low n = 1,461 |
Medium n = 1,236 |
High n=1,210 |
p-valuea | |
| Mean purpose (SD) | 3.7 (0.55) | 4.9 (0.24) | 5.7 (0.25) | NA |
| Mean age in years (SD) | 67.7 (9.2) | 66.6 (8.6) | 66.7 (8.4) | .002 |
| Female, n (%) | 870 (59.5) | 705 (57.0) | 715 (59.1) | .39 |
| Race, n (%) | ||||
| White | 1,307 (89.5) | 1,122 (90.8) | 1,081 (89.3) | .094 |
| Black | 105 (7.2) | 72 (5.8) | 100 (8.3) | |
| Other | 49 (3.4) | 42 (3.4) | 29 (2.4) | |
| Hispanic, n (%) | 112 (7.7) | 60 (4.9) | 56 (4.6) | <.001 |
| Education, n (%) | ||||
| Less than high school | 272 (18.6) | 119 (9.6) | 108 (8.9) | <.001 |
| High school/GED | 822 (56.3) | 685 (55.4) | 637 (52.6) | |
| More than high school | 367 (25.1) | 432 (35.0) | 465 (38.4) | |
| Partnered, n (%) | 993 (68.0) | 920 (74.4) | 948 (78.3) | <.001 |
| Mean total household wealth in 10,000 U.S. dollars (SD) | 48.7 (92.5) | 63.8 (11.1) | 80.9 (15.6) | <.001 |
| Mean body mass index in kg/m2 (SD) | 27.6 (5.8) | 27.1 (4.8) | 27.0 (4.8) | .003 |
| More than once per week | ||||
| Light physical activity, n (%) | 933 (63.9) | 893 (72.2) | 881 (72.8) | <.001 |
| Moderate physical activity, n (%) | 822 (56.3) | 781 (63.2) | 865 (71.5) | <.001 |
| Vigorous physical activity, n (%) | 323 (22.1) | 386 (31.2) | 445 (36.8) | <.001 |
| Self-reported health, n (%) Poor/fair |
390 (26.7) | 173 (14.0) | 115 (9.5) | <.001 |
| Difficulty with at least one ADL | 211 (14.4) | 97 (7.8) | 69 (5.7) | <.001 |
| Difficulty with at least one IADL | 152 (10.4) | 55 (4.4) | 33 (2.7) | <.001 |
| CES-D score <4, n (%) | 401 (27.4) | 126 (10.2) | 75 (6.2) | <.001 |
| Self-reported mental health condition, n (%) | 320 (21.9) | 173 (14.0) | 115 (9.5) | <.001 |
| Baseline HbA1c | 5.32 (0.28) | 5.33 (0.28) | 5.31 (0.28) | .15 |
ADL activities of daily living; CES-D Center for Epidemiologic Studies Depression; GED general education diploma; HbA1c hemoglobin A1c; IADL instrumental activities of daily living; SD standard deviation.
a p-values were derived using one-way analysis of variance tests for continuous variables and Pearson’s chi-squared tests for categorical variables.
Table 3 shows the associations between baseline levels of purpose in life and HbA1c at 4-year follow-up. In our initial linear regression model, which adjusted only for baseline HbA1c (Model 1), HbA1c at 4-year follow-up was 0.05 percentage points lower among individuals with medium purpose (95% confidence interval [CI] −0.10 to 0.00, p = .04) and 0.08 percentage points lower among individuals with high purpose (95% CI −0.13 to −0.03, p = .002) compared with individuals with low purpose. We then adjusted for sociodemographic factors and baseline HbA1c (Model 2) and did not observe a change in the relationship between purpose and HbA1c. The relationship between purpose and HbA1c remained stable when adjusting for physical health and physical functioning variables (Model 3) and mental health variables (Model 4). We included all covariates in a final model (Model 5) and found that HbA1c at 4-year follow-up was 0.04 percentage points lower (95% CI −0.09 to 0.01) among individuals with medium purpose (p = .09) and 0.07 percent lower (95% CI −0.13 to −0.02) among individuals with high purpose (p = .01) compared with individuals with low purpose. There was no significant difference in HbA1c at 4-year follow-up among individuals with high purpose compared with individuals with medium purpose (coefficient −0.03, 95% CI −0.08 to 0.017; p = .21).
Table 3.
Associations Between Baseline levels of Purpose in Life and Hemoglobin A1c at 4-Year Follow-up
| Characteristics | Tertiles of purpose | |||||
|---|---|---|---|---|---|---|
| Low n=1,466 |
Medium n=1,238 |
High n=1,210 |
||||
| Model | Covariates | Coefficient | Coefficient | p-value | Coefficient | p-value |
| 1 | Baseline HbA1c | 0.0 (reference) |
−0.05 (−0.10 to −0.00) |
.04 | −0.08 (−0.13 to −0.03) |
.002 |
| 2 | Baseline HbA1c + sociodemographic factors1 | 0.0 (reference) |
−0.04 (−0.09 to 0.00) |
.06 | −0.07 (−0.12 to −0.02) |
.004 |
| 3 | Model 2 + physical health and functioning factors2 | 0.0 (reference) |
−0.04 (−0.08 to 0.01) |
.13 | −0.07 (−0.12 to −0.01) |
.02 |
| 4 | Model 2 + mental health factors3 | 0.0 (reference) |
−0.05 (−0.09 to −0.00) |
.042 | −0.08 (−0.13 to −0.03) |
.004 |
| 5 | All covariates4 | 0.0 (reference) |
−0.04 (−0.09 to 0.01) |
.09 | −0.07 (−0.13 to −0.02) |
.01 |
HbA1c hemoglobin A1c.
1Sociodemographic factors include age in years (continuous variable), gender, race (white/black/other), Hispanic ethnicity (Hispanic/non-Hispanic), years of formal education (<12, 12, >12), marital status (married / not married), and total household wealth (quartiles).
2Physical health and functioning factors include body mass index (continuous variable), physical activity (dichotomized to indicate ≥ twice weekly engagement in light, moderate, and/or vigorous activity), self-rated health (dichotomized to indicate fair/poor health), activities of daily living (dichotomized to indicate having difficulty in at least one ADL), and instrumental activities of daily living (dichotomized to indicate having difficulty in at least one IADL).
3Mental health factors include the eight-item Center for Epidemiological Studies Depression Scale (dichotomized to indicate ≥ 4 symptoms) and self-reported psychiatric diagnoses (yes/no).
4Full model details are shown in Appendix 1.
Table 4 demonstrates the association between levels of purpose in life and development of abnormal glucose metabolism at 4-year follow-up. In our initial logistic regression model (Model 1), rates of abnormal glucose metabolism were lower among individuals with medium purpose compared with low purpose (odds ratio [OR] 0.08, 95% CI 0.64 to 0.99; p = .04) and high purpose compared with low purpose (OR 0.71, 95% CI 0.58 to 0.87; p = .001). We adjusted for sociodemographic characteristics (Model 2), which somewhat weakened the association between purpose and abnormal glucose metabolism. There was no additional attenuation of the relationship between purpose and abnormal glucose metabolism in models that adjusted for physical health and physical functioning variables (Model 3) or mental health variables (Model 4). After controlling for all covariates (Model 5), individuals with high levels of baseline purpose were less likely to have abnormal glucose metabolism at 4-year follow-up compared with individuals with low purpose (OR 0.78, 95% CI 0.62 to 0.99; p = .04). There was no significant difference in incident abnormal glucose metabolism at 4-year follow-up among individuals with high purpose compared with individuals with medium purpose (OR 0.92, 95% CI 0.73 to 1.15; p = .44).
Table 4.
Associations Between Baseline Purpose in Life and Abnormal Glucose Metabolism at 4-Year Follow-up
| Tertiles of purpose | ||||||
|---|---|---|---|---|---|---|
| Low n=1,466 |
Medium n=1,238 |
High n=1,210 |
||||
| Model | Covariates | Odds ratio | Odds ratio (95% CI) |
p-value | Odds ratio (95% CI) | p-value |
| 1 | Baseline HbA1c | 1.0 (reference) | 0.80 (0.64–0.99) |
.04 | 0.71 (0.58–0.87) |
.001 |
| 2 | Baseline HbA1c + sociodemographic factorsa | 1.0 (reference) | 0.84 (0.68–1.04) |
.12 | 0.77 (0.61–0.96) |
.02 |
| 3 | Model 2 + physical health and functioning factorsb | 1.0 (reference) | 0.84 (0.68–1.05) |
.13 | 0.78 (0.62–0.98) |
.04 |
| 4 | Model 2 + mental health factorsc | 1.0 (reference) | 0.84 (0.68–1.04) |
.11 | 0.77 (0.61–0.97) |
.03 |
| 5 | All covariatesd | 1.0 (reference) | 0.85 (0.68–1.05) |
.13 | 0.78 (0.62–0.99) |
.04 |
HbA1c hemoglobin A1c.
aSociodemographic factors include age in years (continuous variable), gender, race (white/black/other), Hispanic ethnicity (Hispanic/non-Hispanic), years of formal education (<12, 12, >12), marital status (married / not married), and total household wealth (quartiles).
bPhysical health and functioning factors include body mass index (continuous variable), physical activity (dichotomized to indicate ≥ twice weekly engagement in light, moderate, and/or vigorous activity), self-rated health (dichotomized to indicate fair/poor health), activities of daily living (dichotomized to indicate having difficulty in at least one ADL), and instrumental activities of daily living (dichotomized to indicate having difficulty in at least one IADL).
cMental health factors include the 8-item Center for Epidemiological Studies Depression Scale (dichotomized to indicate ≥ 4 symptoms) and self-reported psychiatric diagnoses (yes/no).
dFull model details are shown in Appendix 1.
Adjusted coefficients and adjusted ORs for all covariates included in the complete model (Model 5) are shown in Appendix 1.
Discussion
In a national study of older Americans with normal baseline glucose levels, we found that individuals with high baseline purpose in life had lower HbA1c levels at 4-year follow-up compared with individuals with low baseline purpose in life. Though these differences in HbA1c levels at 4-year follow-up were small in magnitude, they correlated with a significant decrease in the 4-year incidence of prediabetes and type 2 diabetes among individuals with high versus low baseline purpose in life. Given the prevalence of prediabetes and type 2 diabetes, these findings may have important population health implications.
We tested several hypotheses of why purpose might be associated with lower risk of abnormal glucose metabolism and found that the association was independent of demographic and socioeconomic factors and not explained by physical activity, BMI, or mental health. This study suggests that the association between purpose in life and blood glucose is not explained by known risk factors for prediabetes and type 2 diabetes. Prior studies have demonstrated similar independent associations between purpose in life and development of chronic conditions such as cardiovascular disease and stroke [4, 5].
Although our data did not permit us to elucidate the exact mechanism through which purpose in life may influence glucose metabolism, there are several possibilities that should be examined closely in future research. First, individuals with greater levels of purpose in life are more likely to use preventive health services [10], which may facilitate early identification and management of risk factors for chronic diseases such as weight gain. Second, greater purpose may increase one’s investment in maintaining good health and thus facilitate behaviors which are independently associated with a lower risk of type 2 diabetes. This hypothesis is supported by the observation that, at baseline, individuals with high purpose had lower BMIs, higher levels of physical activity, and better self-reported health than those with low purpose. The relationship between purpose in life and blood glucose was not attenuated by the addition of these variables to our model. However, other health behaviors known to protect against the development of type 2 diabetes that were not measured—for example, adequate sleep [48] and healthful dietary habits [49]—may also be more prevalent among high purpose compared with low purpose individuals and could mediate the relationship between purpose in life and blood glucose. Third, greater levels of purpose in life may increase one’s psychological flexibility and overall capacity to manage stressful events [50], which may result in lower levels of the stress hormones that are implicated in the pathogenesis of type 2 diabetes [51].
Additionally, it is possible that the strength of the relationship between purpose in life and blood glucose varies among different types of individuals. For example, neighborhood characteristics such as crime rates, poverty, and racial segregation can increase the risk of type 2 diabetes through chronic stress exposure [27, 52] and, in this environmental context, the association between purpose in life and glucose metabolism may be reduced. We were not able to test for such moderation of the effects of purpose on life on glucose metabolism, and future studies should aim to identify any such factors.
Given the growing evidence that greater purpose in life is associated with lower chronic disease incidence, research efforts should explore strategies to enhance purpose in life as a strategy to prevent chronic disease, either alone or in combination with other approaches. Previous literature suggests that psychological and spiritual well-being—constructs that are closely related to purpose in life—can be modified through interventions [53, 54], and similar approaches may be effectively used to enhance purpose in life. For example, strategies such as cognitive behavioral therapy, mindfulness training, and individual life coaching can increase psychological well-being [53], whereas meaning-centered psychotherapy has been shown to increase spiritual well-being [54]. Screening tools may be used to identify individuals with low purpose in life, and these individuals could then be connected with targeted interventions to increase their sense of purpose as a strategy to prevent type 2 diabetes and other chronic conditions.
Limitations
We analyzed observational data over two time points, limiting our ability to establish causality. Although we included multiple covariates in our model, there may be unmeasured confounders of the relationship between purpose in life and glucose metabolism. Additionally, the effect of purpose on glucose metabolism may be moderated by additional factors such as religiosity, social connectedness, and external stressors which we were not able to evaluate in our analyses. Future studies should consider the potential influence of these factors as well as others that may modify the strength of the relationship between purpose in life and glucose metabolism. Finally, although our study cohort consisted of a national sample of middle-aged and older Americans, the results may not be generalizable to younger populations or individuals in other countries.
Conclusions
To our knowledge, our study is the first to demonstrate a longitudinal association between greater levels of baseline purpose in life and more favorable glucose metabolism. Future research should seek to identify the potential mechanisms of this association and factors that influence the strength of this relationship. Additionally, strategies that seek to enhance purpose in life should be developed and tested to prevent type 2 diabetes and prediabetes, either alone or as a complement to existing evidence-based strategies such as DPPs.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Dina Hafez, Michele Heisler, HwaJung Choi, Claire Ankuda, and Tyler Winkelman declare that they have no conflict of interest. Dr. Kullgren has received consulting fees from SeeChange Health and HealthMine, and a speaking honorarium from AbilTo, Inc.
Supplementary Material
Acknowledgments
Acknowledgments Drs. Hafez, Ankuda, and Winkelman acknowledge support from the Robert Wood Johnson Foundation in their role as Clinical Scholars. Dr. Heisler acknowledges support from the National Institute of Diabetes and Digestive and Kidney Diseases (P30DK092926). Dr. Kullgren is a VA HSR&D Career Development awardee at the Ann Arbor VA. Dr. Kullgren also received grants from the Robert Wood Johnson Foundation, from the US Department of Veterans Affairs, and from the Donaghue Foundation. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. The HRS was approved by the Institutional Review Board at the University of Michigan. Prior to each interview, written informed consent is obtained from study participants.
Appendix 1. Adjusted Coefficient and Adjusted Odds Ratio for Covariates Included in the Complete Model (Model 5)
| HbA1c at 4-year follow-up | Incident abnormal glucose metabolism at 4-year follow-up | |
|---|---|---|
| Adjusted coefficient (95% CI) | Adjusted OR (95% CI) | |
| Purpose | ||
| Low | 1.0 (reference) | 1.0 (reference) |
| Medium | −0.04 (−0.09 to 0.01) | 0.84 (0.68 to 1.05) |
| High | −0.07 (−0.13 to −0.02)* | 0.78 (0.62 to 0.99)* |
| Baseline HbA1c | 0.45 (0.38 to 0.52)* | 6.19 (4.18 to 9.16)* |
| Age | 0.005 (−0.02 to 0.03) | 1.00 (0.88 to 1.14) |
| Female gender | −0.03 (−0.06 to 0.00)* | 0.78 (0.69 to 0.90)* |
| Race | ||
| White | 1.0 (reference) | 1.0 (reference) |
| Black | 0.06 (−0.01 to 0.14) | 1.62 (1.17 to 2.25)* |
| Other | 0.09 (−0.01 to 0.18) | 1.55 (0.91 to 2.66) |
| Hispanic ethnicity | 0.02 (−0.06 to 0.10) | 1.11 (0.77 to 1.59) |
| Education | ||
| < 12 years | 1.0 (reference) | 1.0 (reference) |
| 12 years | 0.02 (−.05 to 0.1) | 1.06 (0.76 to 1.47) |
| >12 years | −0.003 (−0.07 to 0.08) | 0.98 (0.69 to 1.39) |
| Partnered | −0.01 (−0.05 to 0.02) | 0.84 (0.68 to 1.03) |
| Total household wealth | ||
| Bottom 25% | 1.0 (reference) | 1.0 (reference) |
| 25%–50% | 0.03 (−0.02 to 0.08) | 0.96 (0.75 to 1.23) |
| 50%–75% | 0.02 (−0.03 to 0.07) | 0.93 (0.73 to 1.20) |
| Top 25% | 0.002 (−0.05 to 0.06) | 0.78 (0.55 to 1.10) |
| Body mass index kg/m2 | 0.01 (0.00 to 0.01)* | 1.03 (1.01 to 1.05)* |
| More than once per week | ||
| Light physical activity | 0.02 (−0.01 to 0.05) | 0.89 (0.70 to 1.12) |
| Moderate physical activity | 0.003 (−0.04 to 0.04) | 0.88 (0.71 to 1.10) |
| Vigorous physical activity | −0.03 (−0.06 to 0.05) | 0.90 (0.75 to 1.10) |
| Poor self-reported health status | 0.005 (−0.06 to 0.07) | 0.89 (0.70 to 1.14) |
| Difficulty with ≥ ADL | 0.023 (−0.06 to 0.11) | 1.00 (0.72 to 1.40) |
| Difficulty with ≥ IADL | 0.01 (−0.10 to 0.12) | 1.01 (0.66 to 1.55) |
| CES-D < 4 | −0.004 (−0.06 to 0.05) | 0.97 (0.73 to 1.28) |
| Self-reported mental health condition | −0.04 (−0.10 to 0.02) | 1.08 (0.80 to 1.46) |
ADL activities of daily living; CES-D Center for Epidimiologic Studies Depression; CI confidence interval; HbA1c hemoglobin A1c; IADL instrumental activities of daily living; OR odd ratio.
*p < .05.
References
- 1. Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989; 57: 1069. [Google Scholar]
- 2. Ryff CD, Keyes CL. The structure of psychological well- being revisited. J Pers Soc Psychol. 1995; 69(4): 719–727. [DOI] [PubMed] [Google Scholar]
- 3. Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med. 2009; 71(5): 574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim E. Purpose in Life and Cardiovascular Health [Internet]. University of Michigan; 2015. [cited 2016 Jun 27]. Available at https://deepblue.lib.umich.edu/bitstream/handle/2027.42/111619/kimeric_1.pdf?sequence=1&isAllowed=y [Google Scholar]
- 5. Kim ES, Sun JK, Park N, Peterson C. Purpose in life and reduced incidence of stroke in older adults: ‘The Health and Retirement Study’. J Psychosom Res. 2013; 74(5): 427–432. [DOI] [PubMed] [Google Scholar]
- 6. Yu L, Boyle PA, Wilson RS, Levine SR, Schneider JA, Bennett DA. Purpose in life and cerebral infarcts in community-dwelling older people. Stroke. 2015; 46(4): 1071–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim ES, Hershner SD, Strecher VJ. Purpose in life and incidence of sleep disturbances. J Behav Med. 2015; 38(3): 590–597. [DOI] [PubMed] [Google Scholar]
- 8. Hooker SA, Masters KS. Purpose in life is associated with physical activity measured by accelerometer. J Health Psychol. 2016; 21(6): 962–971. [DOI] [PubMed] [Google Scholar]
- 9. Holahan CK, Holahan CJ, Velasquez KE, Jung S, North RJ, Pahl SA. Purposiveness and leisure-time physical activity in women in early midlife. Women Health. 2011; 51(7): 661–675. [DOI] [PubMed] [Google Scholar]
- 10. Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A. 2014; 111(46): 16331–16336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ryff CD, Singer BH, Dienberg Love G. Positive health: Connecting well-being with biology. Philos Trans R Soc Lond B Biol Sci. 2004; 359(1449): 1383–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol. 2007; 26(3): 305–313. [DOI] [PubMed] [Google Scholar]
- 13. Walker BR, Soderberg S, Lindahl B, Olsson T. Independent effects of obesity and cortisol in predicting cardiovascular risk factors in men and women. J Intern Med. 2000; 247(2): 198–204. [DOI] [PubMed] [Google Scholar]
- 14. 2014 Diabetes Report Card—diabetesreportcard2014.pdf [Internet]. [cited 2016 May 27]. Available at http://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf
- 15. Gerstein HC, Santaguida P, Raina P et al. Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: A systematic overview and meta-analysis of prospective studies. Diabetes Res Clin Pract. 2007; 78(3): 305–312. [DOI] [PubMed] [Google Scholar]
- 16. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: Systematic review and meta-analysis. BMJ. 2016; 355: i5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tuomilehto J, Lindström J, Eriksson JG et al. ; Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344(18): 1343–1350. [DOI] [PubMed] [Google Scholar]
- 18. Pan XR, Li GW, Hu YH et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997; 20(4): 537–544. [DOI] [PubMed] [Google Scholar]
- 19. Group DPPR. Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(6): 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: The National Diabetes Prevention Program. Am J Prev Med. 2013; 44(4 Suppl 4): S346–S351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vojta D, Koehler TB, Longjohn M, Lever JA, Caputo NF. A coordinated national model for diabetes prevention: Linking health systems to an evidence-based community program. Am J Prev Med. 2013; 44(4 Suppl 4): S301–S306. [DOI] [PubMed] [Google Scholar]
- 22. DoIHavePrediabetes.org . Prevent Type 2 Diabetes [Internet]. DoIHavePrediabetes; [cited 2016. Dec 16]. Available at https://doihaveprediabetes.org/ [Google Scholar]
- 23. National Diabetes Prevention Program | Diabetes | CDC; [Internet]. [cited 2016. Dec 16]. Available at https://www.cdc.gov/diabetes/prevention/index.html [Google Scholar]
- 24. Prevent Diabetes STAT | General Public [Internet]. Prev. Diabetes STAT; [cited 2016. Dec 16]. Available at http://www.preventdiabetesstat.org [Google Scholar]
- 25. Wareham NJ. Mind the gap: Efficacy versus effectiveness of lifestyle interventions to prevent diabetes. Lancet Diabetes Endocrinol. 2015; 3(3): 160–161. [DOI] [PubMed] [Google Scholar]
- 26. Kelly SJ, Ismail M. Stress and type 2 diabetes: A review of how stress contributes to the development of type 2 diabetes. Annu Rev Public Health. 2015; 36: 441–462. [DOI] [PubMed] [Google Scholar]
- 27. Ludwig J, Sanbonmatsu L, Gennetian L et al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med. 2011; 365(16): 1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. National Diabetes Prevention Program—curriculum.pdf [Internet]. [cited 2016. Sep 21]. Available at https://www.cdc.gov/diabetes/prevention/pdf/curriculum.pdf
- 29. Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006; 49(5): 837–845. [DOI] [PubMed] [Google Scholar]
- 30. Deschênes SS, Burns RJ, Graham E, Schmitz N. Prediabetes, depressive and anxiety symptoms, and risk of type 2 diabetes: A community-based cohort study. J Psychosom Res. 2016; 89: 85–90. [DOI] [PubMed] [Google Scholar]
- 31. Williams ED, Magliano DJ, Tapp RJ, Oldenburg BF, Shaw JE. Psychosocial stress predicts abnormal glucose metabolism: The Australian diabetes, obesity and lifestyle (AusDiab) study. Ann Behav Med. 2013; 46(1): 62–72. [DOI] [PubMed] [Google Scholar]
- 32. Heraclides A, Chandola T, Witte DR, Brunner EJ. Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: Evidence from the Whitehall II study. Diabetes Care. 2009; 32(12): 2230–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Trief PM, Cibula D, Delahanty LM, Weinstock RS. Depression, stress, and weight loss in individuals with metabolic syndrome in SHINE, a DPP translation study. Obesity (Silver Spring). 2014; 22(12): 2532–2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Delahanty LM, Conroy MB, Nathan DM; Diabetes Prevention Program Research Group Psychological predictors of physical activity in the diabetes prevention program. J Am Diet Assoc. 2006; 106(5): 698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Delahanty LM, Peyrot M, Shrader PJ, Williamson DA, Meigs JB, Nathan DM; DPP Research Group Pretreatment, psychological, and behavioral predictors of weight outcomes among lifestyle intervention participants in the Diabetes Prevention Program (DPP). Diabetes Care. 2013; 36(1): 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Juster FT, Suzman R. An overview of the health and retirement study. J Hum Resour. 1995; 30: S7. [Google Scholar]
- 37. American Diabetes Association. Standards of medical care in diabetes--2014. Diabetes Care. 2014; 37 (Suppl 1): S14–S80. [DOI] [PubMed] [Google Scholar]
- 38. Allen IE, Seaman CA. Likert scales and data analyses. Qual Prog Milwaukee. 2007; 40: 64–65. [Google Scholar]
- 39. Brett CE, Gow AJ, Corley J, Pattie A, Starr JM, Deary IJ. Psychosocial factors and health as determinants of quality of life in community-dwelling older adults. Qual Life Res. 2012; 21(3): 505–516. [DOI] [PubMed] [Google Scholar]
- 40. Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychol Aging. 2000; 15(2): 187–224. [DOI] [PubMed] [Google Scholar]
- 41. Schmitz N, Deschênes S, Burns R, Smith KJ. Depressive symptoms and glycated hemoglobin A1c: a reciprocal relationship in a prospective cohort study. Psychol Med. 2016; 46(5): 945–955. [DOI] [PubMed] [Google Scholar]
- 42. Feng X, Croteau K, Kolt GS, Astell-Burt T. Does retirement mean more physical activity? A longitudinal study. BMC Public Health. 2016; 16: 605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. How much physical activity do older adults need? | Physical Activity | CDC; [Internet]. [cited 2016. Jul 28]. Available at http://www.cdc.gov/physicalactivity/basics/older_adults/index.htm [Google Scholar]
- 44. Zajacova A, Dowd JB. Reliability of self-rated health in US adults. Am J Epidemiol. 2011; 174(8): 977–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993; 5(2): 179–193. [DOI] [PubMed] [Google Scholar]
- 46. Choi H, Burgard S, Elo IT, Heisler M. Are older adults living in more equal counties healthier than older adults living in more unequal counties? A propensity score matching approach. Soc Sci Med. 2015; 141: 82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mezuk B, Bohnert AS, Ratliff S, Zivin K. Job strain, depressive symptoms, and drinking behavior among older adults: Results from the health and retirement study. J Gerontol B Psychol Sci Soc Sci. 2011; 66(4): 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kawakami N, Takatsuka N, Shimizu H. Sleep disturbance and onset of type 2 diabetes. Diabetes Care. 2004; 27(1): 282–283. [DOI] [PubMed] [Google Scholar]
- 49. Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004; 164(20): 2235–2240. [DOI] [PubMed] [Google Scholar]
- 50. McKnight PE, Kashdan TB. Purpose in life as a system that creates and sustains health and well-being: An integrative, testable theory. Rev Gen Psychol. 2009; 13: 242–251. [Google Scholar]
- 51. Joseph JJ, Golden SH. Cortisol dysregulation: The bidirectional link between stress, depression, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2017; 1391(1): 20–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Spencer Bonilla G, Rodriguez-Gutierrez R, M Montori V. What we don’t talk about when we talk about preventing type 2 diabetes-addressing socioeconomic disadvantage. JAMA Intern Med. 2016; 176(8): 1053–1054. [DOI] [PubMed] [Google Scholar]
- 53. Weiss LA, Westerhof GJ, Bohlmeijer ET. Can we increase psychological well-being? The effects of interventions on psychological well-being: A meta-analysis of randomized controlled trials. PLoS One. 2016; 11(6): e0158092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Breitbart W, Poppito S, Rosenfeld B et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012; 30(12): 1304–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.