Abstract
Endemic animal rabies causes >99% of all human rabies cases; elimination of animal rabies reduces the rate of human infections. The most recent animal rabies cases in the Gangwon and Gyeonggi provinces of Korea occurred in November 2012 and February 2013, respectively. Here we explore ways to ensure that Korea remains animal rabies non-occurrence. The government must prevent rabies recurrence by vaccinating dogs, distributing bait vaccine in regions with a high rabies risk, performing laboratory-based surveillance, preventing the flow of rabies-suspect animals from neighboring countries, and enhancing border quarantine. As has already been shown in several developed countries, careful and ongoing rabies control will allow Korea to remain animal rabies-free.
Keywords: Rabies, Elimination, Oral rabies vaccination
Introduction
The World Health Organization (WHO), the World Organization for Animal Health (OIE), and the Food and Agriculture Organization of the United Nations (FAO) have set a target of “zero human rabies deaths by 2030” [1]. To realize this, the OIE and sub-regional offices have run workshops on international standards for rabies control. Many countries, including Korea, are striving toward these standards [2,3]. According to the Terrestrial Animal Health Code of OIE, animal rabies free country is defined as: (1) the disease is notifiable and any change in the epidemiological situation is reported to the OIE, (2) an ongoing system of disease surveillance has been in operation for the past two years, (3) regulatory measures for the prevention of rabies are implemented, (4) no case of indigenously acquired rabies virus (RABV) infection has been confirmed during the past 2 years, (5) no imported case in the Orders Carnivore or Chiroptera has been confirmed as rabies for the past 6 months [4].
In 1993, Korea was declared animal rabies-free status because no animal rabies case occurred in the 8-year period from 1984 to 1992 [5,6]. Unfortunately, shortly thereafter, rabies transmitted by raccoon dogs was seen in a domestic Korean dog. Between that case and February 2013, raccoon dog-transmitted rabies has occurred in cattle, dogs, feral cats, and deer [7,8]. Rabies has not occurred since 2013.
Maintenance of Korea's animal rabies non-occurrence status requires government action for the ultimate declaration of rabies free status and many challenges are apparent. An enhanced national rabies control program is required, as are detailed guidelines for appropriate distribution of bait vaccine, establishment of a buffer zone near the demilitarized zone (DMZ), enhanced surveillance, better control of animal movement, and an action plan should recurrence develop. We address these topics below.
Operation of a National Rabies Control Program
The need for a national rabies control program is reflected by the fact that raccoon dogs have transmitted rabies to other animals in Korea since 1993. As shown in Table 1, a total of 437 animal rabies cases were identified in Gyeonggi-do (Dongducheon, Gapyeong, Gimpo, Goyang, Hwaseong, Paju, Pocheon, Suwon, Yangju, Yangpyeong, and Yeoncheon), Gangwon-do (Cheorwon, Chuncheon, Goseong, Hongcheon, Hwacheon, Inje, Yanggu, and Yangyang), and Seoul. The epidemiological studies showed that all were attributable to wild raccoon dogs. The five animal species documented as being infected by rabid raccoon dogs in fact included raccoon dogs (n=76) (Table 2). No animal cases of rabies have occurred since February 2013 because of the distribution of bait vaccine for raccoon dogs and parental vaccination of other dogs. Therefore, any strategy for maintaining the animal rabies non-occurrence status of Korea should include a mandatory vaccination component, registration of companion animals, neutering of stray cats, ongoing distribution of bait vaccine in regions with a high rabies risk, enhanced surveillance, serological surveys after vaccination, rapid reporting of issues, management of stray dogs, analysis of any weak points in the strategy via risk assessment, and blocking the importation of rabies-infected animals from other countries.
Table 1. Number of animal rabies cases confirmed in the Gyeonggi and Gangwon provinces since 1993.
| Gyeonggi (case) | Gyeonggi (head) | Gangwon (case) | Gangwon (head) | Seoul (case) | Total | |
|---|---|---|---|---|---|---|
| 1993 | 0 | 0 | 1 | 1 | 0 | 1 |
| 1994 | 8 | 8 | 11 | 12 | 0 | 19 |
| 1995 | 3 | 3 | 3 | 3 | 0 | 6 |
| 1996 | 2 | 3 | 0 | 0 | 0 | 2 |
| 1997 | 4 | 4 | 10 | 10 | 0 | 14 |
| 1998 | 50 | 50 | 18 | 20 | 0 | 68 |
| 1999 | 29 | 30 | 13 | 13 | 0 | 42 |
| 2000 | 21 | 25 | 3 | 3 | 0 | 24 |
| 2001 | 17 | 30 | 15 | 15 | 0 | 32 |
| 2002 | 57 | 69 | 21 | 26 | 0 | 78 |
| 2003 | 19 | 20 | 11 | 13 | 0 | 30 |
| 2004 | 7 | 7 | 19 | 22 | 0 | 26 |
| 2005 | 6 | 6 | 8 | 9 | 0 | 14 |
| 2006 | 11 | 11 | 7 | 9 | 1 | 19 |
| 2007 | 0 | 0 | 3 | 3 | 0 | 3 |
| 2008 | 1 | 1 | 13 | 13 | 0 | 14 |
| 2009 | 0 | 0 | 18 | 18 | 0 | 18 |
| 2010 | 0 | 0 | 10 | 10 | 0 | 10 |
| 2011 | 0 | 0 | 4 | 5 | 0 | 4 |
| 2012 | 4 | 4 | 3 | 3 | 0 | 7 |
| 2013 | 6 | 6 | 0 | 0 | 0 | 6 |
| 2014 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2015 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2016 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2017 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 245 | 277 | 191 | 208 | 1 | 437 |
Data associated with animal rabies cases are obtained from KAHIS program (http://www.kahis.go.kr).
Table 2. Number of rabid animals confirmed since 1993 in Korea, by species.
| Cattle | Dogs | Raccoon dogs | Feral cats | Deer | Total | |
|---|---|---|---|---|---|---|
| No. of rabid cases | 179 (41.0) | 177 (40.5) | 76 (17.4) | 4 (0.9) | 1 (0.2) | 437 |
| No. of rabid animals | 221 (45.5) | 184 (37.9) | 76 (15.6) | 4 (0.8) | 1 (0.2) | 486 |
Values are presented as number (%).
In total, six human rabies cases were confirmed between 1999 and 2004. Human rabies has not been reported in Korea since 2005.
Mandatory Vaccination of Animals
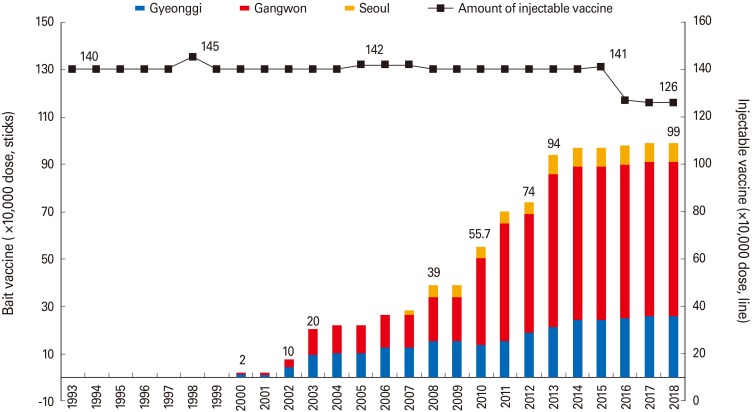
It is well-known that mass vaccination is the best means of preventing animal rabies cases [9,10]. As shown in Fig. 1, since 1993, the Korean government has supplied about 1.4 million doses of parenteral rabies vaccine for dogs nationwide. Mass dog vaccination programs subsume both technical and regulatory aspects. The OIE defines a rabies vaccine as a standardized formulation containing a defined amount of immunogenic antigen. It is well-known that rabies vaccines protect against all RABV variants of the phylogroup 1 lyssaviruses. As shown in Table 3, 13 rabies vaccines (5 live-attenuated, 6 inactivated, and 2 oral bait vaccines) have been licensed for use in animals in Korea. The OIE has recommended that cell culture-grown, inactivated, rabies vaccines with adjuvants or RABV glycoprotein vector vaccines should be given to all dogs and cats, except pregnant animals or those <3 months of age in all rabies-endemic regions [11]. As live attenuated rabies vaccine, ERA (Evelyn-Rokitnick-Abelseth) strain, injected into raccoons have been reported to cause rabies, they are no longer used in Canada [12]. But, the ERA strain has been used as a vaccine strain for dogs in Korea since 1980. Therefore, it is necessary to stop using the current live rabies vaccine strain, which was licensed in the 1980s and replace it with a safer vaccine, such as one based on the ERAGS strain, which contains two mutations at position 194, 333 of the G protein related to pathogenicity [13], or an inactivated vaccine containing adjuvants.
Fig. 1. Comparison of the distribution of a VRG bait vaccine (Y axis on the left) and injectable vaccine (Y axis on the right) to animals. As raccoon dogs transmit animal rabies in Korea, the Veterinary Authority decided to distribute a rabies bait vaccine in 2000. The injectable vaccine has been distributed to all municipal governments where the vaccine is injected into dogs and cattle via intramuscular route. The bait vaccine has also been distributed to only three rabies risk regions, Gyeonggi-do, Gangwon-do, and Seoul. Data related to injectable and bait vaccine are obtained from the Livestock Disease Prevention Plan issued by Ministry of Agriculture, Food and Rural Affairs.
Table 3. Rabies vaccines licensed for commercial use in Korea up to 2018.
| Produced by | Type of vaccine | Dose/ Route | For use in animals |
|---|---|---|---|
| Korea BNP | Live | 1 mL/IM | Dog, cattle, horse, sheep, goat |
| Daesung Micro | Live | 1 mL/IM | Dog, cattle, horse, sheep, goat |
| Green Cross | Live | 1 mL/IM | Dog, cattle, horse, sheep, goat |
| Komipharm | Live | 1 mL/IM | Dog, cattle, horse, sheep, goat |
| Choongang Vac | Live | 1 mL/IM | Dog, cattle, horse, sheep, goat |
| Merial Inc. | Inactivated | 1 mL/IM or SC | Dog, cattle |
| Zoetis (Nobivac) | Inactivated | 1 mL/IM or SC | Dog, cat |
| Virbac | Inactivated | 1 mL/IM or SC | Dog, cat |
| Choongang Vac | Inactivated | 1 mL/IM or SC | Dog, cat, cattle |
| Zoetis (Diffensor) | Inactivated | 1 mL/IM or SC | Dog, cat, cattle, sheep |
| Komipharm | Inactivated | 1 mL/IM or SC | Dog, cattle, horse, sheep, goat |
| Virbac | Bait | 2 mL/Oral | Raccoon dog, badger, fox |
| Merial Inc. | Bait | 1.8 mL/Oral | Raccoon dog |
Data on licensed rabies vaccines are obtained from the veterinary drug information management system of Animal & Plant Quarantine Agency (http://www.medi.qia.go.kr).
IM, intramuscular; SC, subcutaneous.
Turning to regulatory matters, the Korean central government supports national rabies control programs by assisting local governments with vaccination costs. Local governments have added funds to those allocated centrally to perform vaccinations between March and April, and September and October. When a dog reaches 3 months of age, rabies vaccination is required. Therefore, vaccinations must be available throughout the year. Dogs and cattle in regions with a high rabies risk, and dogs in regions that do not have a high risk, must be vaccinated; owner cooperation is thus required.
In 2014, the Animal Welfare Act introduced a companion animal registration system to prevent straying and promote owner responsibility. Currently, only dogs >3 months old must be registered, but this provision is to be expanded to include cats, ferrets, and raccoons. Registration entails internal microchipping, and placement of an external radio identification device and an identification tag (associated with rabies vaccination status). Thus, owners register their pets, which are vaccinated.
Zoos contain various species susceptible to rabies; in one zoo, an African civet was reportedly infected [14]. If a rabid animal is introduced into a zoo, the risk of transmission of rabies to other susceptible animals is high. Therefore, zoo animals require regular rabies vaccinations with inactivated or bait vaccines.
Distribution of Bait Vaccine for Raccoon Dogs
Raccoon dog-transmitted rabies first appeared in 1993 and, as 68 cases of animal rabies were confirmed in 1998, the Veterinary Authority (through the Korean government) distributed rabies bait vaccine in Gyeonggi and Gangwon provinces in 2000; the bait is taken by wild raccoon dogs [6,7]. As shown in Fig. 1, the amount of vaccine distributed has gradually increased, reaching 990,000 doses in 2017. Table 1 shows that rabies cases numbered 78 in 2002, and then gradually decreased to zero in 2014. Thus, the bait vaccine is as effective in Korea as in Western Europe [15].
Despite there being no report of rabies over the 4-year period since February 2013, Korea remains at risk. First, although the bait vaccine has been distributed in regions where rabies cases have been reported since 1993, this was done without consideration of the designation of a region as high-risk or animal rabies-free. It is necessary to regulate these designations, where high-risk regions may vary from year to year. The amounts of bait vaccine could be adjusted accordingly by distributing it only in current and projected high-risk regions.
Second, there is a need to improve the bait vaccine distribution process. To date, people familiar with raccoon dog densities and the geographical features of particular areas have distributed the vaccine around livestock farms [7]. However, this method requires many people, is slow, and may not reach some target animals. Aerial distribution (as used in many other countries) can overcome these limitations.
Third, the region 10 km south of the DMZ may be regarded as a rabies buffer zone, in which the bait vaccine is also distributed. Since 1993, rabies has occurred in all regions adjacent to the DMZ, where rabies is presumed to circulate. Based on the molecular epidemiology, Korean RABV isolated from rabid animals including raccoon dogs showed the closest relationship with RABV isolated in eastern China and Russia [16]. In future, rabid animals in the DMZ are likely to migrate southward, spreading rabies. Therefore, it is necessary to involve North Korea in a collaborative project; the bait must be distributed to the north of the DMZ.
Strengthening Surveillance
Rabies surveillance is the most important aspect of any eradication program [17,18]. The rabies surveillance that has been currently running in Korea is a passive surveillance. In other words, when animal suspected of rabies is found, it is firstly referred to local Animal Service Laboratories for diagnosis. A strengthened surveillance of risk regions is required at the point of maintaining animal rabies non-occurrence status, in addition to passive surveillance of non-risk regions. During active surveillance, animals such as wild raccoon dogs, guard dogs, and hunting dogs are constantly evaluated to maintain animal rabies non-occurrence status. Many rabies-suspected samples, including dead animals (‘road-kill’), are available from wild animal rescue centers and the Korea Highway Corporation. Rabies tests are performed in local Animal Service Laboratories; the technicians must be vaccinated and trained in the performance of the direct fluorescent antibody test (FAT), virus isolation, histological identification, and polymerase chain reaction. However, the laboratory supervisors tend to change frequently and regular training programs are therefore needed. If rabies is detected, it is advisable to perform molecular analysis, which provides insight into viral transmission.
Rapid Reporting
Rabies is clinically diagnosed when an animal exhibits neurological symptoms such as extremely aggressive behavior, anger, or paralysis. However, it is not easy to accurately determine rabies status in the absence of mass testing of rabies-suspect animals [18]. Therefore, rabies should be confirmed by the FAT (a brain evaluation) because there is no viremia. When animals including raccoon dogs are suspected of rabies, it is imperative to contact regional Animal Service Laboratories immediately. Currently, Korea has 13 wildlife rescue centers that treat wild animals and these centers are likely to encounter such animals. Thus, there is a need for cooperation between wildlife rescue centers and Animal Service Laboratories, where rapid reporting of suspected rabies cases would render it possible to reduce the risk of secondary outbreaks.
Serological Surveys after Vaccination
Although it is mandatory to vaccinate all dogs and cattle in regions with a high rabies risk, some are not vaccinated for a variety of reasons such as handling difficulties, young age, owner refusal, lack of any owner, pregnancy, or illness. Sero-surveillance is often used in endemic regions to assess the efficacy of mass parenteral vaccination [19], and can effectively prevent recurrence and monitor the overall immune status of animals. Therefore, since 2002, sero-surveillance has been conducted on cattle and dogs in 21 counties of the Gyeonggi and Gangwon provinces. Additional vaccination was recommended in regions where the seropositive rate was <70%. This policy must be maintained, because it helps to prevent rabies recurrence. With respect to the animal blood obtained, the regions where animal sera are obtained should be those identified as high-risk regions. Since 1993, there have been no rabies risk regions despite the existence of a region where rabies has not occurred for 10 years, and has been designated only continuously. Therefore, a region where rabies occurred should be immediately designated as a rabies risk region and a region, while one in which rabies has not occurred for 10 years should be release the designation of rabies risk region.
Stray Animal Management and Neutering Programs
In many Asian countries, stray dogs transmit rabies [20]. An increase in the number of strays can increase the incidence of rabies. As shown in Table 2, four feral cats in Korea that presumably came into contact with rabid raccoon dogs were confirmed to have rabies. Dogs and cats stray when owners discard them or the pet get lost. Therefore, owners must assume a high level of responsibility to reduce the number of stray dogs and thus decrease the incidence of rabies; accountability should be promoted in the mass media. Currently, only 3-month-old puppies are required to be enrolled in stray animal management and neutering programs; in future, 3-month-old kittens should also be included. In addition, livestock disease prevention law states that stray dogs suspected of contagious disease can be captured and euthanized. However, the culling of stray dogs does not effectively eliminate dog rabies [21]. Another way to reduce the number of stray animals is to link culling to the trap-neuter-release (TNR) program, which was implemented in all Korean municipalities since 2014. Feral cats vaccinated during the TNR program exhibited an excellent immune response [22]. The TNR is a kind of program, through which free-ranging cats are humanely trapped, brought to a veterinarian to be spayed or neutered, then returned to the locations where they were caught. This program needs to be extended to free-roaming dogs in certain suburbs.
Prevention of the Entry of Rabies from Other Countries
Movement of both people and their companion animals between countries has increased and the rate of importation of wild animals, such as raccoons and ferrets, is increasing annually in Korea, making it more likely that rabies-infected animals may enter the country. It has been reported that the probability of rabies entering the UK is highly dependent on compliance of policies such as quarantine, the Pet Travel Scheme and the EU Pet Movement Policy after assessing the risk by estimating the annual probability of rabies [23]. Thus, quarantine of imported animals must be strengthened. The International Health Code of the OIE states that only dogs and cats with rabies antibody levels ≥0.5 IU/mL can be imported into Korea. In recent years, Chinese ferret badgers and Formosan gem-faced civets have been identified as long-term terrestrial reservoirs of rabies in Taiwan [24]. Therefore, importation of Asian ferret badgers requires enhancement of the quarantine procedure. Wild animals imported from other countries should also be tested for rabies antibodies, and only animals with satisfactory levels thereof should be admitted.
Conclusion
Korea has successfully implemented a national rabies control program including mass vaccination of domestic dogs and distribution of a rabies bait vaccine for raccoon dogs, resulting in an animal rabies non-occurrence status since February 2013. Such preventative actions serve as a good model for eradication of rabies throughout Asia. Before any formal declaration of rabies-free status, the Korean government should make sure that it fully complies with the requirements of the OIE. Furthermore, active surveillance of dogs and raccoon dogs in regions with a high rabies risk should be increased because of fluctuations in rabies antibody levels among dogs and possible re-entry of rabid raccoon dogs via the DMZ. Also, measures to prevent animal smuggling through airports or seaports must be strengthened.
Footnotes
No potential conflict of interest relevant to this article was reported.
This study was supported by a grant (2016-217) from the Food, and Rural Affairs (MAFRA), Republic of Korea.
References
- 1.Fooks AR, Cliquet F, Finke S, et al. Rabies. Nat Rev Dis Primers. 2017;3:17091. doi: 10.1038/nrdp.2017.91. [DOI] [PubMed] [Google Scholar]
- 2.Lionel Harischandra PA, Gunesekera A, Janakan N, Gongal G, Abela-Ridder B. Sri Lanka takes action towards a target of zero rabies death by 2020. WHO South East Asia J Public Health. 2016;5:113–116. doi: 10.4103/2224-3151.206247. [DOI] [PubMed] [Google Scholar]
- 3.Miranda LM, Miranda ME, Hatch B, et al. Towards canine rabies elimination in Cebu, Philippines: assessment of health economic data. Transbound Emerg Dis. 2017;64:121–129. doi: 10.1111/tbed.12350. [DOI] [PubMed] [Google Scholar]
- 4.World Organization for Animal Health (OIE) Terrestrial animal health code (chapter 8.14: infection with rabies) [Internet] Paris: OIE; 2018. [cited 2018 May 1]. Available from: http://www.oie.int/standard-setting/terrestrial-code/access-online. [Google Scholar]
- 5.Joo YS, Lee JH, Lee KK, Bang HA, Lee WC. Retrospective study of extensive vaccination programs for canine rabies control and public health in Korea. Jpn J Infect Dis. 2011;64:513–515. [PubMed] [Google Scholar]
- 6.Kim CH, Lee CG, Yoon HC, et al. Rabies, an emerging disease in Korea. J Vet Med B Infect Dis Vet Public Health. 2006;53:111–115. doi: 10.1111/j.1439-0450.2006.00928.x. [DOI] [PubMed] [Google Scholar]
- 7.Cheong Y, Kim B, Lee KJ, et al. Strategic model of national rabies control in Korea. Clin Exp Vaccine Res. 2014;3:78–90. doi: 10.7774/cevr.2014.3.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang DK, Kim HH, Lee KK, Yoo JY, Seomun H, Cho IS. Mass vaccination has led to the elimination of rabies since 2014 in South Korea. Clin Exp Vaccine Res. 2017;6:111–119. doi: 10.7774/cevr.2017.6.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wera E, Mourits MC, Siko MM, Hogeveen H. Cost-effectiveness of mass dog vaccination campaigns against rabies in Flores Island, Indonesia. Transbound Emerg Dis. 2017;64:1918–1928. doi: 10.1111/tbed.12590. [DOI] [PubMed] [Google Scholar]
- 10.Pimburage RMS, Gunatilake M, Wimalaratne O, Balasuriya A, Perera K. Sero-prevalence of virus neutralizing antibodies for rabies in different groups of dogs following vaccination. BMC Vet Res. 2017;13:133. doi: 10.1186/s12917-017-1038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Organization for Animal Health (OIE) Manual of diagnostic tests and vaccines for terrestrial animals. 7th ed. Paris: OIE; 2012. pp. 263–282. [Google Scholar]
- 12.Fehlner-Gardiner C, Nadin-Davis S, Armstrong J, Muldoon F, Bachmann P, Wandeler A. Era vaccine-derived cases of rabies in wildlife and domestic animals in Ontario, Canada, 1989–2004. J Wildl Dis. 2008;44:71–85. doi: 10.7589/0090-3558-44.1.71. [DOI] [PubMed] [Google Scholar]
- 13.Yang DK, Kim HH, Lee SH, Jeong WH, Tark D, Cho IS. A genetically modified rabies vaccine (ERAGS) induces protective immunity in dogs and cattle. Clin Exp Vaccine Res. 2017;6:128–134. doi: 10.7774/cevr.2017.6.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bingham J, Hill FW, Matema R. Rabies incubation in an African civet (Civettictis civetta) Vet Rec. 1994;134:528. doi: 10.1136/vr.134.20.528. [DOI] [PubMed] [Google Scholar]
- 15.Cliquet F, Robardet E, Must K, et al. Eliminating rabies in Estonia. PLoS Negl Trop Dis. 2012;6:e1535. doi: 10.1371/journal.pntd.0001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang DK, Park YN, Hong GS, et al. Molecular characterization of Korean rabies virus isolates. J Vet Sci. 2011;12:57–63. doi: 10.4142/jvs.2011.12.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Velasco-Villa A, Escobar LE, Sanchez A, et al. Successful strategies implemented towards the elimination of canine rabies in the Western Hemisphere. Antiviral Res. 2017;143:1–12. doi: 10.1016/j.antiviral.2017.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Banyard AC, Horton DL, Freuling C, Muller T, Fooks AR. Control and prevention of canine rabies: the need for building laboratory-based surveillance capacity. Antiviral Res. 2013;98:357–364. doi: 10.1016/j.antiviral.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Servat A, Wasniewski M, Cliquet F. Tools for rabies serology to monitor the effectiveness of rabies vaccination in domestic and wild carnivores. Dev Biol (Basel) 2006;125:91–94. [PubMed] [Google Scholar]
- 20.Kasempimolporn S, Sichanasai B, Saengseesom W, Puempumpanich S, Sitprija V. Stray dogs in Bangkok, Thailand: rabies virus infection and rabies antibody prevalence. Dev Biol (Basel) 2008;131:137–143. [PubMed] [Google Scholar]
- 21.Rupprecht CE, Hanlon CA, Slate D. Control and prevention of rabies in animals: paradigm shifts. Dev Biol (Basel) 2006;125:103–111. [PubMed] [Google Scholar]
- 22.Fischer SM, Quest CM, Dubovi EJ, et al. Response of feral cats to vaccination at the time of neutering. J Am Vet Med Assoc. 2007;230:52–58. doi: 10.2460/javma.230.1.52. [DOI] [PubMed] [Google Scholar]
- 23.Ramnial V, Kosmider R, Aylan O, Freuling C, Muller T, Fooks AR. Quantitative risk assessment to compare the risk of rabies entering the UK from Turkey via quarantine, the Pet Travel Scheme and the EU Pet Movement Policy. Epidemiol Infect. 2010;138:1114–1125. doi: 10.1017/S0950268809991221. [DOI] [PubMed] [Google Scholar]
- 24.Lan YC, Wen TH, Chang CC, et al. Indigenous wildlife rabies in Taiwan: ferret badgers, a long term terrestrial reservoir. Biomed Res Int. 2017;2017:5491640. doi: 10.1155/2017/5491640. [DOI] [PMC free article] [PubMed] [Google Scholar]