Abstract
We examined the use of automated voice recognition (AVR) messages targeting smokers from primary care practices located in underserved urban and rural communities to promote smoking cessation. We partnered with urban and rural primary care medical offices (n = 7) interested in offering this service to patients. Current smokers, 18 years and older, who had completed an office visit within the previous 12 months, from these sites were used to create a smoker's registry. Smokers were recruited within an eight county region of western New York State between June 2012 and August 2013. Participants were contacted over six month intervals using the AVR system. Among 5812 smokers accrued 1899 (32%) were reached through the AVR system and 55% (n = 1049) continued to receive calls. Smokers with race other than white or African American were less likely to be reached (OR = 0.71, 0.57–0.90), while smokers ages 40 and over were more likely to be reached. Females (OR = 0.78, 0.65–0.95) and persons over age 40 years were less likely to opt out, while rural smokers were more likely to opt out (OR = 3.84, 3.01–4.90). Among those receiving AVR calls, 30% reported smoke free (self-reported abstinence over a 24 h period) at last contact; smokers from rural areas were more likely to report being smoke free (OR = 1.41, 1.01–1.97). An AVR-based smoking cessation intervention provided added value beyond typical tobacco cessation efforts available in these primary care offices. This intervention required no additional clinical staff time and served to satisfy a component of patient center medical home requirements for practices.
Keywords: Adults, Smoking cessation, Telemedicine
1. Introduction
Tobacco use remains as the leading cause of preventable death in the United States (US) and is responsible for > 480,000 deaths per year and over $300 billion in healthcare expenses and productivity losses annually (Jamal et al., 2015; NYS Department of Health, 2014). Smoking prevalence has declined in the US with 15.5% of adults age 18 or older currently smoking cigarettes in 2016, compared to 20.9% in 2005, and likely reflects the impact of comprehensive tobacco control policies such as taxation, smoke-free legislation, mass media campaigns and expanded access to tobacco cessation counseling and medications (Jamal et al., 2018).
Rates of cigarette smoking are higher among males (17.5%) compared to females (13.5%), among persons with lower levels of education (40.5% with GED compared to 4.5% with a graduate degree), among persons living below the poverty level (25.3% compared to 14.3% above poverty level), among adults with a disability/limitation (21.2% compared to 14.4% with no disability/limitation), and among adults with serious psychological distress (35.8% compared to 14.7% without serious psychological distress) (Jamal et al., 2018). Moreover, low socioeconomic status (SES) is associated with poorer health outcomes and disparities in smoking rates appear to be a significant contributor to this (Cokkinides et al., 2008).
Automated voice response (AVR), also referred to as interactive voice response systems (IVR) are increasingly common in business settings and their use has been extended to facilitate management of chronic health conditions (Finkelstein and Friedman, 2000). AVR systems include the use of computer software combined with an automated telephone system where patients are called at specified times and intervals, and a human voice asks questions and/or delivers instructions while respondents provide short verbal responses and/or interact with the telephone keypad to provide responses. The use of AVR for smoking cessation has been studied at the Ottawa Heart Institute where quit rates of 44% were noted 6 months after discharge among 1276 cardiac patients identified as smoking and who were provided with counseling support, NRT and 3 AVR calls after discharge. However, that study relied on the provision of extensive resources including specification of smoking status following hospitalization, identification of smoking status on the patient chart, standard orders for NRT pharmacotherapies to support cessation and the use of dedicated personnel (counselor and administrative support), along with expenses related to the AVR system (Reid et al., 2006). The addition of AVR calls to identify potential relapse among recently quit smokers receiving standard quit line services did not increase rates of cessation (McDaniel et al., 2015).
Utilizing AVR technology to promote smoking cessation, as an adjunct to standard services available in primary care medical offices, has great potential to provide additional support to smokers. To date, AVR has had limited application in the primary care setting. An AVR system has been used to screen for tobacco use and then to provide that information to clinicians, however that study did not report on cessation outcomes (McDaniel et al., 2005).
This paper reports findings from a study examining the use of AVR technology to deliver smoking cessation messages to more effectively promote smoking cessation among smokers seen in diverse primary care/safety net settings.
2. Methods
2.1. Study design
This study utilized a cross-sectional design to deliver scripted messages encouraging cessation to smokers from selected primary care medical offices in urban and rural medical offices located in medically underserved communities. The research was approved by the Institutional Review Board.
2.2. Study population
The four urban and three rural primary care offices included federally qualified community health centers (FQHCs), academic sites and private practices, were located in medically underserved communities, and provided an electronic file of all smokers in their practice. This smokers registry included patients > 18 years old identified as tobacco users who had completed an office visit within the preceding 12 months (n = 5812).
2.3. AVR intervention
The AVR system attempted calls during predefined sessions (late morning, afternoon, early evening) on both weekdays (9 am to 8 pm) and weekends (10 am to 6 pm). If there was no answer, the date and time of call was recorded and another call was attempted after several hours; after 3 calls with “no answer” within 30 days, additional calls were deferred until the next month. If a “busy” signal was encountered, another call attempt was made in 15 min; after 3 busy signals in the same day, additional calls were deferred until the next day. For phone numbers which were invalid, incorrect or not in service, the data base was checked for alternative numbers, otherwise the outcome and date and time of call was recorded and no further calls to that number were attempted. If a “hang-up” was encountered, another call was attempted after 1 week; 2 “hang-ups” within a month resulted in deferring additional calls until the following month. For answered calls, the identity of the smoker was confirmed. If the smoker was not available we attempted to secure a call back time/date or an alternative number. The caller identification of AVR messages noted the smoker's primary care office and smokers were also given the option to “opt out” of further AVR calls.
The “stages of change” model was applied to cigarette smoking as a strategy to classify smokers into one of several platforms leading to behavior change (Velicer et al., 1995). Stages of change plays an important role in smoking cessation, and stage-matched health messaging was considered when promoting and reinforcing cessation behaviors. The AVR system asked a brief series of items in order to classify a smoker into various groups with regard to their level of interest in quitting smoking: precontemplation (not thinking about stopping smoking), contemplation (thinking about quitting in the next 6 months), preparation (planning to quit in the next 30 days), action (committed to behavior change, sets a quit date, acquire pharmacotherapy and maintenance (a continued commitment to sustaining their smoke free behavior).
If relapse occurred, the smoker was reassessed regarding their level of motivation for making another quit attempt. Respondents had the option of being transferred to either their primary care office or to the state smokers quit line for additional assistance with quitting. Although the AVR system did not permit tracking of these transfers, we estimate that this was uncommon based on feedback from the participating practices.
The content of these calls was consistent with accepted approaches for brief interventions delivered to smokers (Fiore et al., 2008): the precontemplation group was reminded that quitting smoking represents the single most important step to improve overall health and the availability of office/quit line resources, those in the contemplation group were messaged about the barriers to and benefits of quitting (e.g., costs of smoking, benefits of quitting) and evidence-based medications for cessation, those in the preparation group were encouraged to develop a plan for quitting (e.g., setting a quit date, acquiring pharmacotherapy, nicotine addiction, cues/triggers for smoking and motivation for quitting), those in the action group received messages regarding changing behaviors, identifying social support, and building self-efficacy and those self-identifying as “smoke-free” (maintenance group) were offered congratulations and encouraged to focus on the health benefits of continued cessation. In addition, this message content delivered within the stages of change model was modified based upon feedback from several focus groups of smokers, identified from underserved rural and urban community-based primary care medical offices, at which the content of potential messages and general approaches were discussed (Rodriguez et al., 2016). This formative research process assured that the cessation messaging was relevant to population of interest. AVR messages were finalized with clinical and research team input.
Following several weeks of AVR calls, it was noted that some smokers had received multiple call while others had no call attempts, and refinements were implemented to 1) limit the number of calls attempted during each week, 2) vary call times, based on both the time of day (e.g., late morning, afternoon, early evening) and day of the week (e.g., weekday versus weekend), and 3) randomize the starting point for each session of calls.
2.4. Independent variables
The smokers' registry included the following variables: medical office, patient sex, age, race, ethnicity, and name and phone number.
2.5. Dependent variables
The primary study outcome was self-reported smoking cessation based upon responses to the questions: “Since we last contacted you were you able to stop smoking for at least 24 hours?” and “How many cigarettes are you smoking per day now?” Successful quitters were defined as persons who reported quitting for at least 24 h and who responded “none/zero” to the item on amount currently smoked per day. Secondary outcomes included the number of call attempts and percentage of completed calls.
2.6. Statistical analysis
Patient characteristics and outcomes are reported as frequencies and relative frequencies since all covariates are categorical variables. Chi-square testing was used to compare group differences. Binary logistic regression was conducted to assess the factors associated with the outcomes of interest. A two-sided p-value of < 0.05 was considered to be statistically significant. Because medical office and region (e.g., urban or rural area) were 89% correlated (p < 0.0001), only region was included in the fitted models. All statistical analyses were conducted using SPSS software (version 21) and SAS software (version 9.4).
3. Results
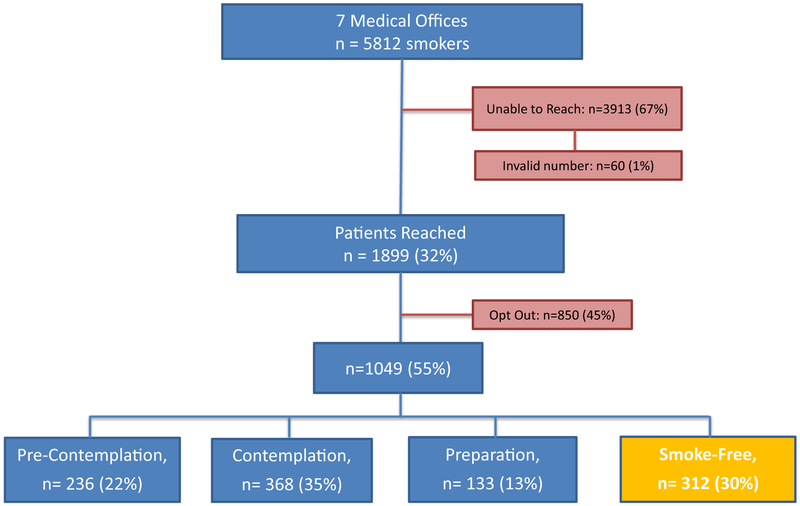
Overall, 1899 of 5812 smokers (32%) were reached by the AVR system; 67% were unable to be contacted (i.e., no answer, answering machine picked up, busy signal) and 1% had an invalid phone number (see Fig. 1). Among those reached, 45% (n = 850) elected to opt out of further calls, leaving 1049 (55%) smokers enrolled in the AVR intervention. The average number of attempted calls to smokers was 44 (median = 51).
Fig. 1.
Outcomes of IVR calls to smokers' registry.
As presented in Table 1, smokers with race other than white or African American were less likely to be reached (OR = 0.71, 95% confidence interval 0.57–0.90), while smokers ages 40 and over were more likely to be reached (see Table 1); contact rates did not vary by sex or by office location (urban vs rural). Females (OR = 0.78, 0.65–0.95) and persons over age 40 years were less likely to opt out, while rural smokers were more likely to opt out (OR = 3.84, 3.01–4.90); opt-outs did not vary by racial group (see Table 2).
Table 1.
Call outcome, by selected demographic variables, univariate and multivariate analyses, n = 5812.
| Not reached (n = 3913) |
Reached (n = 1899) |
OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| # | % | # | % | |||
| Sex | Male | 1656 | 67.1% | 813 | 32.9% | 1.00 (ref) |
| Female | 2257 | 67.5% | 1086 | 32.5% | 1.02 (0.91–1.14) |
|
| Race | White | 2403 | 66.8% | 1193 | 33.2% | 1.00 (ref) |
| AA | 1177 | 66.5% | 593 | 33.5% | 1.04 (0.90–1.20) |
|
| All others | 333 | 74.7% | 113 | 25.3% | 0.71 (0.57–0.90) |
|
| Age range | 18–39 | 1225 | 75.3% | 401 | 24.7% | 1.00 (ref) |
| 40–49 | 849 | 67.5% | 409 | 32.5% | 1.49 (1.27–1.76) |
|
| 50–59 | 1067 | 65.1% | 572 | 34.9% | 1.66 (1.43–1.94) |
|
| 60 + | 772 | 57.1% | 517 | 42.9% | 2.13 (1.79–2.48) |
|
| Urban vs rural offices |
Urban | 2174 | 67.4% | 1054 | 32.7% | 1.00 (ref) |
| Rural | 1739 | 67.3% | 845 | 32.7% | 0.92 (0.80–1.05) |
|
AA, African American; OR, odds ratio; CI, confidence interval.
Table 2.
Opt Out status, by selected demographic variables, univariate and multivariate analyses, n = 1899.
| Opt out (n = 850) |
Did not opt out (n = 1049) |
OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| # | % | # | % | |||
| Gender | Male | 409 | 50.3% | 404 | 49.7% | 1.00 (ref) |
| Female | 441 | 40.6% | 645 | 59.4% | 0.78 (0.65–0.95) |
|
| Race | White | 587 | 49.2% | 606 | 50.8% | 1.00 (ref) |
| AA | 206 | 34.7% | 387 | 65.3% | 1.27 (0.98–1.61) |
|
| All others | 57 | 50.4% | 56 | 49.6% | 1.26 (0.83–1.89) |
|
| Age range | 18–39 | 197 | 49.1% | 204 | 50.9% | 1.00 (ref) |
| 40–49 | 184 | 45.0% | 225 | 55.0% | 0.74 (0.55–0.99) |
|
| 50–59 | 222 | 38.8% | 350 | 61.2% | 0.53 (0.41–0.70) |
|
| 60 + | 247 | 47.8% | 270 | 52.2% | 0.67 (0.50–0.88) |
|
| Urban vs rural offices |
Urban | 336 | 31.9% | 718 | 68.1% | 1.00 (ref) |
| Rural | 514 | 60.8% | 331 | 39.2% | 3.84 (3.01–4.90) |
|
AA, African American; OR, odds ratio; CI, confidence interval.
Among those receiving AVR calls, 30% reported that they were smoke free (self-reported abstinence over a 24 h period) at last contact (see Fig. 1). Smokers from rural medical offices were more likely to report being smoke free (OR = 1.41, 1.01–1.97); smoke free status did not vary by sex, racial group or age category (see Table 3).
Table 3.
Smoking status at last contact, by selected demographic variables, univariate and multivariate analyses, n = 1049.
| Smoke-free (n = 312) |
Smoking (N = 737) |
OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| # | % | # | % | |||
| Gender | Male | 130 | 32.2% | 274 | 67.8% | 1.00 (ref) |
| Female | 182 | 28.2% | 463 | 71.8% | 0.87 (0.66–1.15) | |
| Race | White | 201 | 33.2% | 405 | 66.8% | 1.00 (ref) |
| AA | 98 | 25.3% | 289 | 74.7% | 0.83 (0.59–1.17) | |
| All others | 13 | 23.3% | 43 | 76.8% | 0.66 (0.34–1.27) | |
| Age range | 18–39 | 62 | 30.4% | 142 | 69.6% | 1.00 (ref) |
| 40–49 | 64 | 28.4% | 161 | 71.6% | 0.88 (0.58–1.35) | |
| 50–59 | 97 | 27.7% | 253 | 72.3% | 0.82 (0.56–1.21) | |
| 60 + | 89 | 33.0% | 181 | 67.0% | 1.02 (0.68–1.52) | |
| Urban vs rural sites |
Urban | 191 | 26.6% | 527 | 73.4% | 1.00 (ref) |
| Rural | 121 | 36.6% | 210 | 63.4% | 1.41 (1.01–1.97) | |
AA, African American; OR, odds ratio; CI, confidence interval.
4. Discussion
Similar to national patterns, rates of smoking in New York State (NYS) have demonstrated a continued decline; NYS recently ranked as having the 9th lowest rate among adults in the US (Jamal et al., 2018). Smoking rates for Erie County (18.8%) and Chautauqua County (24.7%), the two areas where medical offices were recruited, are consistently higher than the state as a whole (14.4%) (NYS Department of Health, 2016).
We observed that smokers from rural based medical practices were more likely to opt out of AVR messaging. However, among smokers who continued to receive AVR messages, rural smokers were more likely to report being smoke free. We did not observe a relationship between smoke-free status and number of calls received, although it is possible that smokers who continued to answer calls represent a sub-population that are either more interested in quitting and/or more successful in quitting. Reasons for these regional differences are unclear. It is possible that smokers who reside in rural communities may become more engaged in cessation support delivered by phone, in contrast to other sources of cessation support which might require travel to various locations. This regional difference demonstrates the continued challenges of finding effective methods to impact smoking behaviors among all smokers. We did examine the proportion of land lines by region and noted that that 64% of rural smokers had phone numbers identified as a land line compared to 49% of urban smokers. Contact rates did not vary by land line versus cell phone.
While the PHS tobacco dependence guidelines (Fiore et al., 2008) recommend that all smokers receive at least a brief intervention as a, a review of medical records within several practices which were also included in present study noted that few smokers appear to have received cessation support as part of routine medical care, suggesting (Mahoney et al., 2014). We successfully reached 32% of smokers and 55% of those reached continued to receive AVR messaging. While no control group was used in our design, our prior work with similar primary care practices (Mahoney et al., 2014) and national surveys suggest very low rates of quitting (e.g., ≤7%) (Babb, 2017). Data from the National Health Interview Survey indicated that in 2015 7.4% of smokers reported having quit smoking in the past year compared to 5.7% in 2000 (Babb, 2017).
AVR platforms in primary care medical offices offer the advantage of avoiding further taxing an often overburdened system. Moreover, AVR has the ability to identify specific times and intervals for monitoring selected health behaviors and outcomes, as well as the ability for real time data capture using the telephone keypad/voice response inputs. Key elements of this system include usability/acceptability of this approach by the general public and by medical practices, as well as information dissemination, benefits to and reactions from patients and a potential improvement in targeted outcomes (Lieberman and Naylor, 2012). In addition, an AVR system may better address tobacco dependence given the hesitancy of many health care professionals and individual patients toward discussing this information.
Results of AVR systems to support smoking cessation have been mixed. A pilot study of 101 community-based smokers studied the impact of 9 AVR calls along with 12 weeks of varenicline, group counseling and a quit smoking booklet. After 12 weeks, 44/101 (43%) had stopped smoking based upon self-reported abstinence and exhaled carbon monoxide (< 10 ppm) (Mcnaughton et al., 2013); quit rates of 44% have been reported with varenicline alone, suggesting little impact from the AVR calls (Nides et al., 2008 lack of efficacy of AVR calls for relapse prevention was noted in both the Mcnaughton et al. (2013) and in a 3 arm randomized study which examined the provision of either 10 or 20 AVR calls over 8 weeks, in addition to standardized cessation counseling (5 telephone calls, Quit for Life program), delivered through a quitline to 1752 recently quit smokers. No incremental benefit in self-reported quit rates at 6 months was observed in either group (overall self-reported quit rate, 61%; intention to treat, 38%). Those receiving up to 20 AVR calls compared to those receiving up to 10 calls reported that the number of risk assessments was too many (36% vs 23% respectively, p < 0.001) and took too much time (28% vs 23%, p = 0.09). Among those getting AVR calls, 95% reported that it was easy to answer questions using the AVR system and 87% noted that the system was helpful, although less than one-third of persons receiving additional calls completed an AVR-transferred counseling call (McDaniel et al., 2015). Additionally, the McDaniel et al. (2015) included an intensive contact schedule and low assessment completion rates (37% of AVR calls and 16% of assessments were completed) which aligns with our observation that more contact is not necessarily better. Identifying the most effective and cost-effective number of contacts should continue to be a focus in future studies using AVR technology.
Although the Ottawa Health Institute (OHI) reported quit rates of 44% six months after discharge among 1276 cardiac patients provided with counseling support, NRT and 3 AVR calls after discharge, the OHI system required extensive resources to assess smoking status at time of hospitalization, define smoking status on the patient chart, implement standardardized order sets for NRT pharmacotherapies to support cessation and personnel (counselor and administrative support), along with expenses for the AVR system (Reid et al., 2006). The system implemented in the present study offers the advantage of scalability at a fixed cost, although covering fixed costs does remain a challenge.
A pooled analyses examined the use of five AVR calls over 3 months, along with inpatient counseling and free cessation medication, to encourage smokers (n = 878) to quit following hospital discharge. The AVR calls were rated as “very or somewhat helpful” by 70% of participants and 84% noted that they would recommend the program to other smokers. Biochemically validated quit rates 6 months after discharge were 19%; a multivariate model indicated that completing more AVR calls was associated with being quit at 6 months (OR-1.49, 95% CI 1.30–1.70) (Rigotti et al., 2017).
While we did not collect data on satisfaction with the AVR system, AVR technology has been incorporated into common business interactions including banking, cable, credit card companies, and gas, electric and water utilities. AVR programs have been shown to be successful across the age continuum as well as with individuals inexperienced with the use of computer assisted technology and among patients with low literacy skills (Piette et al., 1999). As a result, it appears that AVR systems are acceptable to patients and represent an effective strategy to educate patients and to disseminate messaging strategies for promoting positive changes in health behavior, including smoking cessation.
It is possible that our AVR call intervention was not sufficiently long to identify long term changes in smoking behavior. While many smokers may report a desire or intention to stop smoking, a smaller proportion will note more immediate plans to stop smoking (Hughes et al., 1999). A stages of change model was applied to 18,000 smokers from three different samples of smokers recruited from Delaware, California, and various worksite locations (Velicer et al., 1995) and while 60% of smokers stated that they were ready to stop smoking in the next 6 months, only about 20% considered stopping in the next 30 days. Alternatively a person's future intentions to stop smoking are predictors of smoking cessation (Velicer et al., 1996), therefore AVR messaging may be useful in identifying smokers who might benefit most from specific supportive health messaging and/or additional interventions.
Limitations to this study include reliance upon medical offices to identify smokers within patient panels and the accuracy of that patient information within each medical records system, and the transient nature of the population with frequent changes in phone numbers. Also the AVR system was customized internally resulting in unanticipated technological issues and time delays, and the challenge of long term operational support remains unresolved. Finally, we relied upon self-report of cessation behaviors over a 24 h period to determine smoking status, which may have overestimated the impact of the intervention. These limitations are balanced however by unique strengths of this study including the participation of several primary care medical offices serving medically underserved populations in both urban and rural communities in western New York State, use of an intervention which doesn't require time from medical office staff, a communication platform which is recognizable to patients, broad reach regardless of cell phone or land lines, and the potential to customize messages via voice recordings from individual primary care clinicians. Importantly, even though we did not reach all patients, and others opted out, these findings suggest an incremental benefit from AVR messaging for assisting smokers to quit.
5. Conclusions
These results suggest value in expanded efforts to implement AVR messaging to promote smoking cessation in primary care settings. This study suggests that AVR systems can be successfully implemented in both urban and rural under-served primary care settings and appears to generate positive outcomes with regard to smoking cessation. This AVR based smoking cessation intervention appears to have provided added value beyond usual tobacco cessation efforts available in these primary care offices. This intervention required no additional clinical staff time and served to satisfy a component of patient centered medical home requirements for many of these practices. Building partnerships with primary care medical offices can aid in the further refinement and testing of community-based interventions such as smoking cessation delivered to medically underserved and diverse patient populations via AVR messaging.
Acknowledgements
This study was supported in part by the Western New York Cancer Coalition (WNYC2) Center to Reduce Disparities Grant NIH/NCI/CRCHD U54CA153598 and the Roswell Park Comprehensive Cancer Center and National Cancer Institute (NCI) grant, P30CA016056. We acknowledge the support and collaboration of the Buffalo/Niagara Community Health Centers and the Chautauqua County Health Network to complete this study.
References
- Babb S, 2017. Quitting smoking among adults—United States, 2000–2015. MMWR Morb. Mortal. Wkly Rep 65, 1457–1464. [DOI] [PubMed] [Google Scholar]
- Cokkinides VE, Halpern MT, Barbeau EM, Ward E, Thun MJ, 2008. Racial and ethnic disparities in smoking-cessation interventions. Am. J. Prev. Med 34 (5), 404–412. [DOI] [PubMed] [Google Scholar]
- Finkelstein J, Friedman RH, 2000. Potential role of telecommunication technologies in the management of chronic health conditions. Dis. Manag. Health Out 8 (2), 57–63. [Google Scholar]
- Fiore MC, C J, Baker TB, et al. , 2008. Treating tobacco use and dependence: 2008 update U.S. public health service clinical practice guideline executive summary. Respir. Care 53 (9), 1217–1222. [PubMed] [Google Scholar]
- Hughes JR, Cummings KM, Hyland A, 1999. Ability of smokers to reduce their smoking and its association with future smoking cessation. Addiction 94 (1), 109–114. [DOI] [PubMed] [Google Scholar]
- Jamal A, Homa DM, O'Connor E, Babb SD, Caraballo RS, Singh T, King BA, 2015. Current cigarette smoking among adults—United States, 2005–2014. MMWR Morb. Mortal. Wkly Rep 64 (44), 1233–1240. [DOI] [PubMed] [Google Scholar]
- Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, Neff LJ, 2018. Current cigarette smoking among adults—United States, 2016. Morb. Mortal. Wkly Rep 67 (2), 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman G, Naylor MR, 2012. Interactive voice response technology for symptom monitoring and as an adjunct to the treatment of chronic pain. Transl. Behav. Med 2 (1), 93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney MC, Twarozek AM, Saad-Harfouche F, Widman C, Erwin DO, Underwood W, Fox CH, 2014. Assessing the delivery of cessation services to smokers in urban, safety-net clinics. J. Community Health 39 (5), 879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaniel AM, Benson PL, Roesener G, Martindale J, 2005. An integrated computer-based system to support nicotine dependence treatment in primary care. Nicotine Tob. Res 7 (Suppl_1), S57–S66. [DOI] [PubMed] [Google Scholar]
- McDaniel AM, Vickerman KA, Stump TE, Monahan PO, Fellows JL, Weaver MT, … Zbikowski SM, 2015. A randomised controlled trial to prevent smoking relapse among recently quit smokers enrolled in employer and health plan sponsored quitlines. BMJ Open 5 (6), e007260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcnaughton B, Frohlich J, Graham A, Young Q-R, 2013. Extended interactive voice response telephony (IVR) for relapse prevention after smoking cessation using varenicline and IVR: a pilot study. BMC Public Health 13 (1), 824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York State Department of Health, 2014. The health consequences of smoking—50 years of progress: a report of the surgeon general. Retrieved from. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf.
- New York State Department of Health, 2016. County level prevalence of smoking among adults. Retrieved from. https://www.health.ny.gov/prevention/tobacco_control/reports/statshots/volume9/n3_county_adult_smoking_prevalence.pdf.
- Nides M, Glover ED, Reus VI, Christen AG, Make BJ, Billing CB, Williams KE, 2008. Varenicline versus bupropion SR or placebo for smoking cessation: a pooled analysis. Am. J. Health Behav. 32 (6), 664–675. [DOI] [PubMed] [Google Scholar]
- Piette JD, Mcphee SJ, Weinberger M, Mah CA, Kraemer FB, 1999. Use of automated telephone disease management calls in an ethnically diverse sample of low-income patients with diabetes. Diabetes Care 22 (8), 1302–1309. [DOI] [PubMed] [Google Scholar]
- Reid RD, Pipe AL, Quinlan B, 2006. Promoting smoking cessation during hospitalization for coronary artery disease. Can. J. Cardiol 22 (9), 775–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA, Chang Y, Rosenfeld LC, Japuntich SJ, Park ER, Tindle HA, … Gomperts T, 2017. Interactive voice response calls to promote smoking cessation after hospital discharge: pooled analysis of two randomized clinical trials. J. Gen. Intern. Med 32 (9), 1005–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez EM, Twarozek AM, Erwin DO, Widman C, Saad-Harfouche FG, Fox CH, Mahoney MC, 2016. Perspectives on smoking cessation in Northern Appalachia. J. Community Health 41 (2), 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Fava JL, Prochaska JO, Abrams DB, Emmons KM, Pierce JP, 1995. Distribution of smokers by stage in three representative samples. Prev. Med 24 (4), 401–411. [DOI] [PubMed] [Google Scholar]
- Velicer WF, Rossi JS, Prochaska JO, Diclemente CC, 1996. A criterion measurement model for health behavior change. Addict. Behav 21 (5), 555–584. [DOI] [PubMed] [Google Scholar]