Abstract
The current study investigated the relation between postural balance and performance of daily living skills (DLS) in youth with autism spectrum disorder (ASD). Fifty-two youth with ASD (6–17 years; IQ ≥ 67) completed standardized balance testing and parent-reported DLS measures. Results showed a positive association between balance and DLS that was specific to youth with below-average IQ. While balance challenges were evident across the IQ spectrum, youth with above-average IQ did not exhibit an association between balance and DLS, perhaps suggestive of compensatory strategies implemented to offset balance challenges during daily-living tasks. These results underscore the need to better understand the contributions of motor challenges to DLS in youth with ASD within the context of broader cognitive and environmental factors.
Keywords: autism spectrum disorder, daily living skills, balance, motor
Introduction
Daily living skills (DLS) are a major challenge for individuals with autism spectrum disorder (ASD) (Liss et al. 2001; Perry et al. 2009). The ability to complete basic DLS allows individuals to participate independently in the home and community, making it is essential to understand the factors that contribute to DLS challenges in ASD. Current evidence suggests that age, executive function, symptom severity, and IQ are associated with DLS challenges (Bal et al. 2015; Duncan and Bishop 2015; Pugliese et al. 2016; Smith et al. 2012), but factors such as atypical motor skills may additionally contribute to poorer DLS performance. Many individuals with ASD exhibit motor impairments (Fournier et al. 2010), and these motor challenges may affect the performance of DLS tasks such as grooming, dressing, and household chores. Of these motor challenges, postural balance may be particularly difficult for individuals with ASD (Ament et al. 2015), and it is often assumed that balance challenges impact DLS in this population. Indeed, everyday tasks such as stepping out of the shower, cooking at the stove, or dressing become substantially more complex if one cannot consistently rely on steadiness during standing. However, no study has directly examined the link between postural balance and DLS in youth with ASD. The present study addressed this gap by examining the relation between standardized measures of balance and DLS in children and adolescents with ASD, while accounting for factors such as age and IQ.
Only a handful of studies have examined motor contributions to DLS in ASD, but the findings suggest that a number of motor features may be associated with DLS performance in this population. Sensory features, fine motor, and gross motor performance were associated with DLS in preschoolers with ASD, with the strongest relation existing between fine motor skills and DLS (Jasmin et al. 2009). Similarly, motor coordination problems were associated with poorer DLS in school-aged females with ASD and school-aged females with attention deficit/hyperactivity disorder, even when accounting for performance IQ (Kopp et al. 2010). Longitudinal research by Travers et al. (2017) found that manual motor skills (i.e., grip strength and finger-tapping speed) significantly correlated with current and future DLS in individuals with ASD from childhood to mid-adulthood, even after accounting for age and IQ. Taken together, it appears that fine motor and motor coordination challenges relate to DLS in ASD, but there is little evidence regarding the role of balance. Given that many DLS tasks inherently involve standing and weight-shifting, it is important to determine if balance impairments are affecting DLS performance in this population. Understanding this relation could aid in the development of appropriate motor interventions for children and adolescents with ASD in order to promote greater independence in the home and community. Therefore, the aim of the present study was to examine the association between postural balance and DLS performance in children and adolescents with ASD. Based on the theoretical contributions of balance to DLS as well as evidence that other motor domains relate to DLS in ASD, we hypothesized that participants with poorer balance would have poorer performance in DLS, above and beyond the effects of age and IQ.
Methods
Design
To examine the relationship between balance and DLS in children with ASD, a standardized measure of balance and a standardized measure of DLS were combined across three concurrent studies within our lab (i.e., two studies that examined a biofeedback-based balance training and one neuroimaging study that examined brain-motor relations). These measures were collected as part of the intake for all three studies. All measures, regardless of study, were administered and scored by the same research team and were administered prior to any balance training. The current analyses were consistent with the aims of all three studies, as the overarching goal was to better understand motor skills in youth with ASD.
Participants
All three studies were approved by the University of Wisconsin-Madison Institutional Review Board. All parents provided written informed consent, and all children provided informed assent. Fifty-two children and adolescents with ASD (6–17 years old; 90.4% male) completed the measures. To be included in these analyses, all participants were required to have a previous diagnosis of ASD that was supported by meeting criteria for ASD on Modules 3 or 4 of the Autism Diagnostic Observation Scale-2nd edition (ADOS-2) (Lord et al. 2012). Individuals were excluded from the study if they had a previous diagnosis of intellectual disability, a known medical cause of ASD (i.e., fragile-X), hypoxia-ischemia, seizure disorder, or other neurological disorders. The sample was representative of the racial composition of the USA, per the 2011–2015 estimates of the U.S. Census Bureau (http://factifinder.census.gov): 65.4% White, Non-Hispanic; 11.5% Black/African American; 7.7% Asian; 7.7% White, Hispanic, and 7.7% more than one race. See Table 1 for additional demographic information.
Table 1.
Demographic characteristics of the sample.
| N=52 participants with ASD (90% male) | ||
|---|---|---|
| Mean(SD) | Range | |
| Age (years) | 12.60(3.34) | 6.41–17.85 |
| Full Scale IQ | 103.25(14.29) | 67–135 |
| VABS-II Daily Living Skills Standard Score | 90.40(15.98) | 66–117 |
| BOT-2 Balance Score (0–37 range) | 27.50(5.88) | 9–37 |
| BOT-2 Percentile | 14.04(13.01) | 1st-62nd |
ASD= Autism Spectrum Disorder; BOT-2 = Bruininks-Oseretsky Test of Motor Proficiency, 2nd edition; VABS-II = Vineland Adaptive Behavior Scales, 2nd edition
Measures & Materials
Bruininks–Oseretsky Test of Motor Proficiency– 2nd Edition (BOT-2) (Bruininks and Bruininks 2005)
The BOT-2 short form and balance subscale were used to assess overall motor percentiles and balance. The BOT-2 is a standardized assessment of motor abilities that measures manual coordination, body coordination and balance, strength and agility, and fine motor skills. The balance subscale uses two-footed and one-footed postures under various conditions (eyes open, eyes closed, and balance beam) to evaluate static and dynamic motor skills essential for maintaining posture while standing and walking. Balance scores range from 0–37, with higher scores indicating better balance. The BOT-2 is normed for ages 4–21 years and has demonstrated strong test–retest reliability, strong internal reliability, and high interrater reliability. Within our lab, all BOT-2 assessments were live-coded by two separate raters, who used videos of administration and consensus coding to reconcile any discrepancies.
Vineland Adaptive Behavior Scale, Second edition (VABS-II) (Sparrow et al. 2005)
The VABS-II was administered as a parent/caregiver report, and the Daily Living Scale was used to assess age-normed DLS. The Daily Living Scale specifically measures age-normed performance of daily living tasks such as household chores, dressing, and grooming. DLS standard scores were used, with higher scores indicating stronger DLS. The VABS-II has shown strong internal consistency and test-retest reliability.
Wechsler Abbreviated Scale of Intelligence-2nd edition (WASI-II) (Wechsler and Hsiao-pin 2011)
The WASI-II is an abbreviated measure of intelligence for ages 6–90 years with strong reliability and validity. The WASI-II includes four subtests (block design, vocabulary, matrix reasoning, and similarities) to assess verbal comprehension, perceptual reasoning, and general intellectual ability (full scale IQ). Full scale IQ also has been shown to be reliably assessed with the two-subtest version of the WASI-II (block design and vocabulary), although verbal comprehension and perceptual reasoning cannot be assessed with two subtests. In the present sample, 75% (39) of participants received the four-subtest version of the WASI-II (used by two of the three studies). The other 25% of participants received the two-subtest version (used by one of the three studies).
Procedures
The intake session was similar across all three studies. Specifically, after informed consent and assent forms were signed, the participant completed the ADOS-2, WASI-II, and BOT-2. While the participant completed these assessments, parents completed the VABS-II.
Data Analysis
Data analysis was completed using R version 3.2.2 (R Core Team 2015). To examine DLS as a function of balance, we fit a standard multiple regression model. Because IQ and age are known to affect DLS (Liss et al. 2001; Smith et al. 2012), age, a quadratic term for age (age2), IQ, and their interactions were included alongside balance as potential variables in the regression model. The leaps package (Lumley, 2017) was used in an exhaustive search to find which subset of these variables accounted for the most variance, using adjusted R2 to account for the number of predictor variables in each model. This procedure led to the final model: DLS standard scores ~ intercept + balance scores + IQ + age + age2 + balance*IQ. To reduce the likelihood of multicollinearity, all independent variables were mean-centered. All regression assumptions for the final model were examined and met.
Results
The overall multiple regression predicting DLS as a function of balance, IQ, and age was significant, F(5,46) = 6.77, p < .001, R2 =. 424 (95% confidence interval: .248–.599), adjusted R2 = .361. The unstandardized beta coefficients, their 95% confidence intervals, standard errors, and t-tests are shown in Table 2. Contrary to our predictions, there was not a conditional (“main”) effect for balance. However, we found a significant interaction between balance and IQ and a main effect for age and age2. The main effects for age and age2 suggest that DLS standard scores showed a slight decrease (with an inverted U-shape) as a function of age within this ASD group. The interaction between balance and IQ is shown in Figure 1. While the interaction between balance and IQ in the regression model was between two continuous variables, Figure 1 simplifies this interaction by showing the relation between balance and DLS scores in those with above-median IQ and those with below-median IQ (median = 104).
Table 2.
Summary of unstandardized beta coefficients from multiple regression analysis examining predictors of daily living skills (DLS) standard scores (n=52).
| b | 95% CI | SE | t-value | p-value | |
|---|---|---|---|---|---|
| Intercept | 96.88 | 91.06, 102.71 | 2.89 | 33.48 | <.001 |
| Balance | 0.44 | −0.21, 1.08 | 0.32 | 1.36 | .18 |
| IQ | 0.22 | −0.05, 0.49 | 0.12 | 1.64 | .11 |
| Age | −1.98 | −3.09, −0.88 | 0.55 | −3.62 | <.001 |
| Age2 | −0.57 | −0.98, −0.15 | 0.20 | −2.76 | .008 |
| Balance X IQ | −0.04 | −0.08, −0.00007 | 0.02 | −2.02 | .04 |
Note: Significant effects are bolded.
Figure 1.
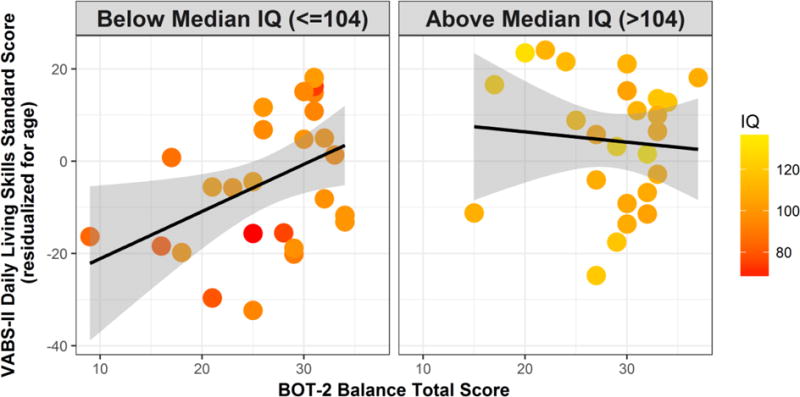
Daily living skills (DLS) standard scores as a function of balance and full scale IQ. Balance was found to significantly interact with IQ to predict DLS, suggesting that balance and DLS were related only in those with lower IQ scores. To illustrate the nature of this interaction, we performed a median split for IQ (median=104) and plotted the relation between balance and DLS in those with higher and lower IQs. However, we also used color to demonstrate individual differences in IQ, as IQ was used as a continuous variable in all of the analyses. The points on the scatterplot are adjusted for the main effect of age, as age was a significant predictor in the model.
From Figure 1, we see that there was a positive relation between balance and DLS performance in individuals with below-median IQ but not in those with above-median IQ. Follow-up partial correlational analyses (controlling for age) confirmed that those with below-median IQ (<=104) demonstrated a significant, medium-to-large, positive relation between balance and DLS, r = +.44, p = .02, whereas those with higher IQ (>104) did not exhibit a relation between balance and DLS, r = −.09, p = .68. To examine if balance scores differed between the below-median-IQ group and the above-median-IQ group, we performed an independent-samples t-test. Similar balance scores were observed in both the below-median-IQ group (M = 26.59, SD = 6.25) and the above-median-IQ group (M = 28.48, SD = 5.42), t(50) = 1.16, p = .25, Cohen’s d = 0.323.
Discussion
The present study is the first, to our knowledge, to investigate the relation between postural balance and DLS performance in youth with ASD. Our results suggest that poorer balance was associated with poorer DLS performance (above-and-beyond the effects of age) but only in individuals who had below-average IQ (IQs of 67–104). In those with above-average IQ (IQs of 105–135), there was no relation between balance and DLS performance. These results extend upon previous motor research to suggest that in addition to manual motor skills (Travers et al. 2017), sensorimotor features (Jasmin et al. 2009), and motor coordination (Kopp et al. 2010), balance challenges may contribute to difficulties with DLS in individuals with ASD. However, in contrast to previous research, the relation between balance and DLS was specific to those who scored lower on the IQ assessment, even though no participant in this study had a diagnosis of co-occurring intellectual disability. It is unclear whether other motor skills, such as fine motor skills, also interact with IQ to predict DLS. However, this is a key avenue for future research, as the present results suggest that cognition may be an important factor to consider when examining the impact of motor skills on DLS, even in youth with ASD without co-occurring intellectual disability.
Notably, the results suggest that those with lower IQ scores had similar balance challenges to those with higher IQ scores, even though the relation between balance and DLS was observed only in the youth with lower IQ scores. One possible explanation for this pattern of results is that individuals with higher IQ may have developed strategies or routines to compensate for balance challenges during DLS (i.e. sitting down while dressing, using structural supports to lean on while completing daily tasks, etc.). In other words, children and adolescents with ASD with higher IQ may be finding ways around relying on balance during daily tasks. While our current measure of DLS did not provide information on compensatory strategies, past research has found that youth with developmental coordination disorder (Missiuna et al. 2008) and cerebral palsy (Klotz et al. 2013) use cognitive and behavioral strategies to manage motor challenges during DLS. However, future research is needed to directly test this possibility in ASD either by inquiring about potential strategies used during DLS performance or by observing DLS performance in naturalistic environments.
These results have important implications for interventions that target DLS performance in youth with ASD. The present results suggest that based on cognitive and motor profiles, different DLS interventions may be warranted for different individuals. Therefore, assessing both motor and cognitive skills prior to any DLS intervention may inform the best course of action for teaching DLS to an individual with ASD. Specifically, for youth who are found to have both balance challenges and lower IQ scores, it is possible that targeting the balance challenges through balance practice, physical therapy, or occupational therapy, may have cascading benefits on DLS. Moreover, balance training in conjunction with teaching and rehearsing DLS may lead to the greatest gains in DLS in this group. In contrast, youth with ASD who have higher IQ scores may be strategically compensating for balance challenges in DLS. Therefore, we likely need to develop and implement different intervention strategies, as balance interventions are unlikely to improve DLS performance in individuals who already have methods for accommodating their balance deficits. For this group with higher IQ scores, teaching further behavioral strategies to manage balance challenges may be a more efficacious approach to improving DLS performance than trying to enhance balance itself.
A limitation of the present study is that the parent-report DLS measure assessed performance across a number of daily tasks rather than assessing tasks that might specifically require balance. This may have led to an underestimation of the role of balance in daily living tasks. Future research that links balance challenges to specific daily living tasks will be critical to inform intervention. Therefore, there is a need to develop and utilize functional assessment tools that measure motor skills during daily tasks such as upper and lower extremity dressing or bringing a utensil to the mouth for feeding. An assessment that measures balance and other motor skills during a functional task would provide the specificity needed to understand the underlying causes of the observed deficits in both balance and DLS in ASD. Further, a functional assessment may be able to exhibit if and how individuals are compensating for balance challenges during functional tasks, which our current measure of DLS was unable to do. The use of more comprehensive, functional assessments could assist in tailoring specific motor-based interventions for this population.
In all, while postural balance is often assumed to impact DLS performance in youth with ASD, the present results suggest that balance challenges relate to DLS performance only in youth with ASD who have below-average IQ scores. This finding suggests a potential interaction between cognition and motor skills that should be accounted for when trying to understand the underlying causes of poorer DLS performance in ASD. These findings raise the question of how motor challenges in ASD combine with other factors known to be associated with DLS, such as executive function and symptom severity. Further, these results from individuals without a history of co-occurring intellectual disability raise the question of how balance skills relate to DLS performance in individuals with ASD and co-occurring intellectual disability. Most daily living tasks require some type of motor involvement. Thus, understanding the contributions of motor skills in combination with other cognitive and environmental factors will enhance the design and efficacy of interventions that target DLS challenges in youth with ASD.
Acknowledgments
Funding: This study was funded by the Brain and Behavior Research Foundation’s NARSAD Young Investigator Award, the Hartwell Foundation’s Individual Biomedical Award, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P30 HD003352 and U54 HD090256).
This work was supported by the Brain and Behavior Research Foundation’s NARSAD Young Investigator Award [to BGT], the Hartwell Foundation’s Individual Biomedical Award [to BGT], and the Eunice Kennedy Shriver National Institute of Child Health and Human Development [P30 HD003352 and U54 HD090256 to the Waisman Center]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Development or the National Institutes of Health. We thank Sarah Brill, Sarah Crook, Olga Dadalko, Ashley Dinges, Dana Dobbe, Nikki Erickson, Isabelle Gallagher, Andres Gomez, Larissa Hacker, Lauren Hoover, Sarah Jacquot, Brooke Koehn, Jenna Lent, Nicole Marczak, Rachel Matz, Kristine McLaughlin, Claire Melin, Molly Pearcy, Carli Peters, Kirstin Peters, Katie Phillips, Jenna Radke, Kailey Sabel, Rachel Samz, Sean Sekelsky, Michele Severson, Olivia Surgent, Elise Suttner, Josh Tarnoff, Desiree Taylor, Jake Tenaglia, David Turner, Amin Tmimi, Caitie Van Sloun, Matthew Walczak, Shannon Wittel, and Oskar Zarzycki for their contributions to this project. We sincerely thank all the families who participated in this study.
Footnotes
Conflict of Interest: Brittany G. Travers declares that she has no conflict of interest. Courtney Engel declares that she has no conflict of interest. Aubrey Fisher declares that she has no conflict of interest. Robyn Geist declares that she has no conflict of interest. Kristin Lillie declares that she has no conflict of interest. Sagui Lutman declares that he has no conflict of interest.
Research ethics: This project was approved the University of Wisconsin-Madison Education and Social/Behavioral Science Institutional Review Board (protocol #2014-1248) and Health Sciences Institutional Review Board (protocols #2014-1499 and #2016-0441)
Author Note
At the time of this study, Courtney Engel, Aubrey Fisher, Robyn Geist, Kristin Lillie, Sagui Lutman, and Brittany G. Travers were at the University of Wisconsin-Madison (Madison, WI, USA).
References
- Ament K, Mejia A, Buhlman R, Erklin S, Caffo B, Mostofsky S, Wodka E. Evidence for specificity of motor impairments in catching and balance in children with autism. Journal of Autism and Developmental Disorders. 2015;45(3):742–751. doi: 10.1007/s10803-014-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bal VH, Kim SH, Cheong D, Lord C. Daily living skills in individuals with autism spectrum disorder from 2 to 21 years of age. Autism: The International Journal of Research and Practice. 2015;19(7):774–784. doi: 10.1177/1362361315575840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruininks RH, Bruininks BB. Bruininks-Oseretsky test of motor proficiency. second. Minneapolis, MN: Pearson Assessment; 2005. [Google Scholar]
- Duncan AW, Bishop SL. Understanding the gap between cognitive abilities and daily living skills in adolescents with autism spectrum disorders with average intelligence. Autism: The International Journal of Research and Practice. 2015;19(1):64–72. doi: 10.1177/1362361313510068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH. Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. Journal of Autism and Developmental Disorders. 2010;40(10):1227–1240. doi: 10.1007/s10803-010-0981-3. [DOI] [PubMed] [Google Scholar]
- Jasmin E, Couture M, McKinley P, Reid G, Fombonne E, Gisel E. Sensori-motor and daily living skills of preschool children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(2):231–241. doi: 10.1007/s10803-008-0617-z. [DOI] [PubMed] [Google Scholar]
- Klotz MCM, Kost L, Braatz F, Ewerbeck V, Heitzmann D, Gantz S, et al. Motion capture of the upper extremity during activities of daily living in patients with spastic hemiplegic cerebral palsy. Gait & Posture. 2013;38(1):148–152. doi: 10.1016/j.gaitpost.2012.11.005. [DOI] [PubMed] [Google Scholar]
- Kopp S, Beckung E, Gillberg C. Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Research in Developmental Disabilities. 2010;31(2):350–361. doi: 10.1016/j.ridd.2009.09.017. [DOI] [PubMed] [Google Scholar]
- Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, et al. Predictors and correlates of adaptive functioning in children with developmental disorders. Journal of Autism and Developmental Disorders. 2001;31(2):219–230. doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule–2nd edition (ADOS-2) Los Angeles, CA: Western Psychological Corporation; 2012. [Google Scholar]
- Lumley T. leaps: Regression Subset Selection. 2017 http://CRAN.R-project.org/package=leaps.
- Missiuna C, Moll S, King G, Stewart D, Macdonald K. Life experiences of young adults who have coordination difficulties. Canadian Journal of Occupational Therapy Revue Canadienne D’ergotherapie. 2008;75(3):157–166. doi: 10.1177/000841740807500307. [DOI] [PubMed] [Google Scholar]
- Perry A, Flanagan HE, Dunn Geier J, Freeman NL. Brief report: the Vineland Adaptive Behavior Scales in young children with autism spectrum disorders at different cognitive levels. Journal of Autism and Developmental Disorders. 2009;39(7):1066–1078. doi: 10.1007/s10803-009-0704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugliese CE, Anthony LG, Strang JF, Dudley K, Wallace GL, Naiman DQ, Kenworthy L. Longitudinal examination of adaptive behavior in autism spectrum disorders: Influence of executive function. Journal of Autism and Developmental Disorders. 2016;46(2):467–477. doi: 10.1007/s10803-015-2584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. https://www.R-project.org/ [Google Scholar]
- Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: The case of daily living skills. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(6):622–631. doi: 10.1016/j.jaac.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla D. Vineland adaptive behavior scales:(Vineland II), survey interview form/caregiver rating form. Livonia, MN: Pearson Assessments; 2005. [Google Scholar]
- Travers BG, Bigler ED, Duffield TC, Prigge MDB, Froehlich AL, Lange N, et al. Longitudinal development of manual motor ability in autism spectrum disorder from childhood to mid-adulthood relates to adaptive daily living skills. Developmental Science. 2017;20(4) doi: 10.1111/desc.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D, Hsiao-pin C. Wechsler abbreviated scale of intelligence (WASI-II) 2nd ed. San Antonio, TX: The Psychological Corporation; 2011. [Google Scholar]


