Abstract
Background
The impact of degree of prematurity at birth on premature infant gut microbiota has not been extensively studied in comparison to term infants in large cohorts.
Methods
To determine the effect of gestational age at birth and postnatal exposures on gut bacterial colonization in infants, we analyzed 65 stool samples from 17 premature infants in the neonatal intensive care unit, as well as 13 samples from 13 mostly moderate-to-late premature infants and 189 samples from 176 term infants in the New Hampshire Birth Cohort Study. Gut colonization patterns were determined with 16S rDNA microbiome profiling.
Results
Gut bacterial alpha-diversity differed between premature and term infants at 6 weeks of age, after adjusting for exposures (p=0.027). Alpha-diversity varied between extremely premature (<28 weeks gestation) and very premature infants (≥28 but <32 weeks, p=0.011), as well as between extremely and moderate-to-late premature infants (≥32 and <37 weeks, p=0.004). Newborn antibiotic use among premature infants was associated with lower Bifidobacterium and Bacteroides abundance (p=0.015 and p=0.041).
Conclusion
Gestational age at birth and early antibiotic exposure have significant effects on the premature infant gut microbiota.
INTRODUCTION
Premature infants have an immature gastrointestinal tract, with a gut epithelium that has diminished barrier function and increased permeability. This allows for translocation of bacteria from the gut to the bloodstream, leading to systemic inflammation or sepsis (1–6). In premature infants it has been hypothesized that antibiotic use, coupled with the infants’ underdeveloped immune systems and gut epithelia, promotes intestinal bacterial communities that are less diverse and enriched with potential pathogens (7–11). Prematurity, lack of diversity in the gut bacterial communities, and the presence of pathogenic bacteria have also been associated with systemic inflammation and the development of sepsis as well as necrotizing enterocolitis, all of which are important complications of prematurity (8,12,13). The bacteria that premature intestinal tracts lack include taxa frequently found to colonize the gut of healthy term infants, as well as bacteria that are associated with immune training, metabolic function, and ultimately decreased risk of lifelong health issues such as obesity and allergy (11,14–16).
The factors responsible for the altered colonization patterns observed in premature infants compared to their healthy term counterparts are not well-defined. Physiological differences in the premature gut epithelium likely fosters abnormal colonization patterns from birth. Premature infants’ exposure to antibiotics before, during, and after birth, likely further contributes to aberrant gut bacterial colonization. Understanding how infant gut bacterial communities vary by gestational age at birth and how they are shaped by exposures can help inform future treatment in the hopes of decreasing pathogen colonization and increasing abundance of beneficial bacteria.
In this study, we aimed to evaluate how gut bacterial community structure varies across the spectrum of gestational age at birth and to assess the effects of various exposures, such as newborn antibiotic administration, delivery mode, and breastmilk feeding, on the gut microbiota of preterm infants.
METHODS
Ethical Approval
Institutional review board approval was obtained from the Committee for the Protection of Human Subjects at Dartmouth College with yearly renewal. Parents provided written, informed consent.
Subject Cohorts and Inclusion Criteria
We studied 17 premature infants hospitalized in a New Hampshire neonatal intensive care unit (NICU) and an additional 13 premature infants enrolled in the New Hampshire Birth Cohort Study (NHBCS) (Table 1). We compared these with 176 term infants also enrolled in the NHBCS. Inclusion criteria for the cohort of infants hospitalized in the NICU were appropriate size for gestational age (AGA) and ≤ 14 days of age at the time of enrollment. We excluded infants with major anomalies, such as trisomies, other genetic syndromes, and clinical syndromes. Major birth defects such as gastroschisis, complex congenital heart disease, or renal anomalies were excluded. Infants had a length of stay in the NICU between 29 and 174 days. 3 infants in the NICU had sepsis, none had necrotizing enterocolitis, and 5 had bronchopulmonary dysplasia. A subset of these infants have been previously studied (17,18). The NHBCS is a prospective longitudinal large epidemiological cohort study of pregnant women and their children (19,20). Pregnant women aged 18–45 in New Hampshire are enrolled at approximately 24 to 28 weeks of gestation. Inclusion criteria for mothers include having a singleton pregnancy, a private drinking well at home, and no plans to move. We included infants with no noted congenital abnormality. Gut microbiome data on a large proportion of these infants has been previously described (21).
Table 1. Subject cohort demographics.
Number of subjects in each cohort and number of stool samples collected. Premature infants are infants born at a gestational age of less than 37 weeks. Gestational age (GA) at birth for all cohorts combined ranged from 24–43 weeks.
| # of Subjects | # of Samples | GA Range | |
|---|---|---|---|
| Preterm/NICU Cohort | 17 | 65 | 24–32 weeks |
| NHBCS - Preterm | 13 | 13 | 29–36 weeks |
| NHBCS - Term | 176 | 189 | 37–43 weeks |
Infant Exposures
Data was collected on the following exposures: newborn antibiotic exposure (antibiotics given during the first days after birth while in hospital), delivery mode (vaginal delivery or Caesarean section), and breastmilk exposure (still consuming breastmilk at time of sample collection) (Table 2). Antibiotic administration data was abstracted from the infant’s hospital medical record. For infants hospitalized in the NICU, delivery and breastmilk feeding information was also abstracted from the medical record; for NHBCS subjects, these exposures were ascertained by telephone follow-up questionnaires with mothers. Additional exposure data was collected for the premature infants in the NICU, such as antibiotic exposure on day of sample collection and exclusive breastmilk feeding at time of sample collection (Table 3).
Table 2. Distribution of exposures in groups of infants based on gestational maturity.
Extremely preterm infants are infants born at a gestational age (GA) of less than 28 weeks. Very preterm infants are infants born at a gestational age of greater than or equal to 28 weeks but less than 32 weeks, though we did not have any infants born at 28 weeks. Moderate-late preterm infants are born at a gestational age of 32 weeks or greater but less than 37 weeks. Term infants are born at 37 weeks or greater. Newborn antibiotics are antibiotics given to the infants in the first few days of life. Delivery mode was either a C-section (Caesarean section) or a vaginal delivery. Current breastmilk exposure is defined as subject was still consuming breastmilk at time of sample collection. Information on newborn antibiotic or breastmilk exposure was not always available, and thus the number of subjects or samples with this data available was noted in the table.
| Extremely Preterm (GA 24–27 weeks, 11 infants) | Very Preterm (GA 29–31 weeks, 5 infants) | Moderate-Late Preterm (32–36 weeks, 14 infants) | Term Infants (37–43 weeks, 176 infants) | |
|---|---|---|---|---|
| Newborn Antibiotic Exposure | 11/11 subjects (100%) | 4/4 (100%) | 4/13 (29%) | 4/172 (2%) |
| Delivery Mode (# C-sections/total) | 7/11 subjects (64%) | 5/5 (100%) | 6/14 (43%) | 52/176 (30%) |
| Current Breastmilk Exposure | 41/43 samples (95%) | 16/16 (100%) | 15/17 (88%) | 165/177 (93%) |
Table 3. NICU Premature Infant Cohort Exposures.
Newborn antibiotics are antibiotics given to the infants in the first few days of life. A stool sample was considered to have antibiotic exposure if antibiotics were administered on same day as sample collection. Delivery mode was either a C-section (Caesarean section) or a vaginal delivery. Breastmilk exposure at time of sample collection was if the child was receiving breastmilk at time of stool collection. A stool sample was considered to belong to an infant who was exclusively fed breastmilk if no milk fortifier or formula was given before or on day of stool sample collection.
| Exposure | Frequency |
|---|---|
| Newborn Antibiotic Exposure | 16/17 subjects (94%) |
| Antibiotic Exposure on Day of Sample Collection | 14/65 samples (22%) |
| Delivery Mode (# C-sections/total) | 13/17 subjects (76%) |
| Breastmilk Exposure at Time of Sample Collection | 61/65 samples (94%) |
| Exclusive Breastmilk Feeding at Time of Sample Collection | 15/65 samples (23%) |
Sample Collection
In the NICU cohort, stool samples were collected weekly beginning with first meconium and ending with hospital discharge. Samples were collected from diapers using sterile wooden depressors, transferred to sterile tubes, and aliquoted and stored at −80°C. In the NHBCS, stool samples were collected at two time points: at time of first stool after passing of meconium (“transitional” stool, 0–3 days of life) and at 6 weeks. Most NHBCS infants contributed samples at only one of these 2 time points. Premature infants from NHBCS born at <36 weeks gestation only contributed 6-week stool, so it was unlikely that they were hospitalized at time of sample collection. Stool was immediately frozen at home at −20°C after collection. Then stool samples were delivered in cold pack, thawed to 4°C, aliquoted in sterile tubes, and suspended in RNAlater. After 24 hours in RNAlater in refrigerator, samples were moved to −80°C long term storage.
Sample processing
For the samples from the preterm infants in the NICU, DNA extraction was performed after thawing of samples using the MoBio Powersoil bacterial DNA isolation kit (MoBio, Carlsbad, California), as previously described (18). DNA was extracted from thawed NHBCS stool samples using Zymo Research’s ZR fecal DNA MiniPrep Kit, also described previously (21). Both kits include a bead-beating step. The MoBio kit used 0.7 mm garnet beads, while the Zymo kit used 0.5 mm high density ceramic beads.
Sample Sequencing and Data Analysis
Sequencing of the V4–V5 hypervariable region of 16S ribosomal DNA was performed using the Illumina MiSeq platform. Details of sequencing methods, taxonomic assignment, and data analysis are described in Supplemental Methods.
RESULTS
Sequencing
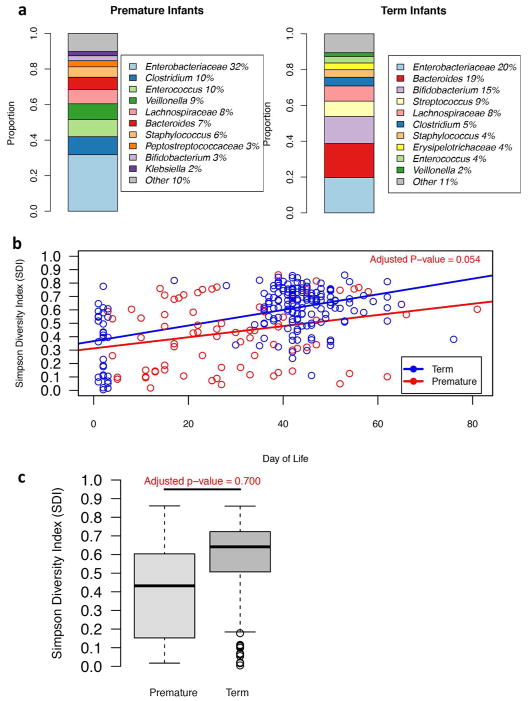
After excluding 25 samples due to low read counts, 78 samples from 30 premature infants and 189 samples from 176 term infants were evaluated. The range of gestational ages for infants in each group is shown in Table 1. Sequencing of these samples resulted in a total of 22,012,483 reads for the 267 (mean: 82443.76, range: 14,002–1,072,107). The dominant bacteria identified in premature infant stool samples was Enterobacteriaceae, making up 32% of normalized reads, followed by the genera Clostridium (10%), Enterococcus (10%), and Veillonella (9%) (Figure 1a). In term infants, bacterial genera from the family Enterobacteriaceae were also the most common, making up 20% of all normalized reads, followed by Bacteroides (19%), Bifidobacterium (15%), and Streptococcus (9%) (Figure 1a). Bacteroides, Bifidobacterium, and Streptococcus made up only 7%, 3% and 2% of total normalized reads among premature infants, respectively (Figure 1a).
Figure 1. Top 10 most abundant taxa (a) and bacterial alpha-diversity differences between premature and term infants (b, c).
(a) Bar charts depicting the percentage of normalized reads that a bacterial taxon makes up in the stool of premature infants and term infants. The top 10 most dominant taxa are depicted. (b, c) Bacterial alpha-diversity differences (b) over time and (c) across all time points. The bacterial alpha-diversity (SDI) of stool samples from premature and term infants is indicated on the y-axis. P-value is adjusted for exposures (newborn antibiotics, delivery mode, and breastmilk feeding at time of sample collection) and age (day of life). (b) Straight lines were fitted to the bacterial alpha-diversity data, and indicate the change in stool bacterial alpha-diversity over time (slope) in premature infants (red) and term infants (blue). The p-value represents the significance of the difference in slopes, and is adjusted for exposures. On the x-axis is the day of life at which a stool sample was collected. (c) Box-plots showing bacterial alpha-diversity differences between premature and term infants across all time points.
Bacterial Alpha-Diversity and Abundance Differences Between Premature and Term Infants
Bacterial alpha-diversity, which was measured by Simpson’s Diversity Index (SDI), varied throughout the 6 weeks of life for individual premature infants with longitudinal stool samples (Figure 1b). After adjusting for the effects of exposures, including delivery mode, newborn antibiotics, and breastmilk exposure at time of sample collection, there was not a significant difference in the change in bacterial alpha-diversity between term and premature infants over time (p=0.054, Figure 1b). Across all time-points, bacterial alpha-diversity was not statistically significantly different between term and premature infants after adjusting for exposures (p=0.700, Figure 1c).
Differences in bacterial abundance between premature and term infants were also assessed. After adjusting for exposures in addition to age at time of stool sample collection, there were no statistically significant differences in bacterial abundance between premature and term infants.
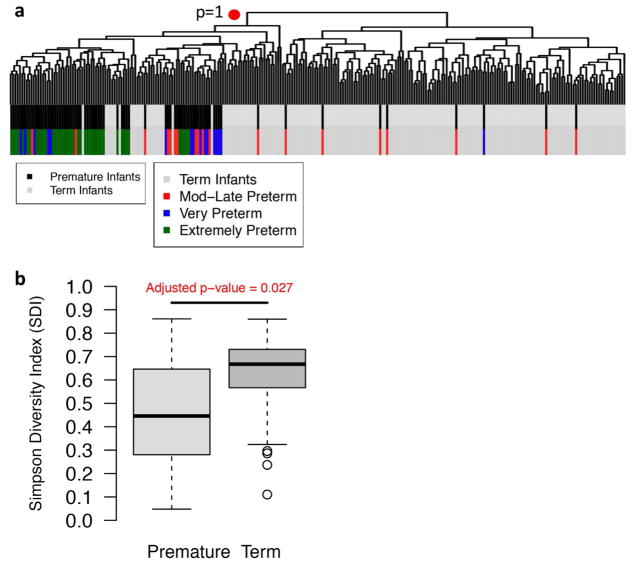
Hierarchical Clustering
Hierarchical clustering analysis revealed that premature infant samples clustered separately from term infant samples, however, the clustering was not statistically significant (p=1 for the cluster containing mostly premature infant samples, Figure 2a). Moderate and late preterm infant samples (32 weeks to <37 weeks) interspersed between the extremely (<28 weeks) and very preterm (<32 weeks) and term samples (Figure 2a).
Figure 2. Hierarchical clustering of stool samples of term and premature infants (a), and bacterial alpha-diversity differences at 6 weeks of age (b).
(a) Below the dendrogram are bars depicting which samples belong generally to premature (black) or term infants (gray), as well as which samples belong to extremely preterm infants (green), very preterm (blue), or moderate-late preterm infants (red). (b) The bacterial alpha-diversity (SDI) of stool samples from premature and term infants is indicated on the y-axis. P-value is adjusted for exposures.
Bacterial Alpha-Diversity and Abundance Differences at 6 weeks
At approximately 6 weeks of age, the difference in bacterial alpha-diversity, after accounting for exposures, was statistically significant (p=0.027), with premature infants having lower bacterial alpha-diversity than term infants at 6 weeks (Figure 2b). However, there were no statistically significant differences in bacterial abundance in premature infants compared to term infants at 6 weeks of age.
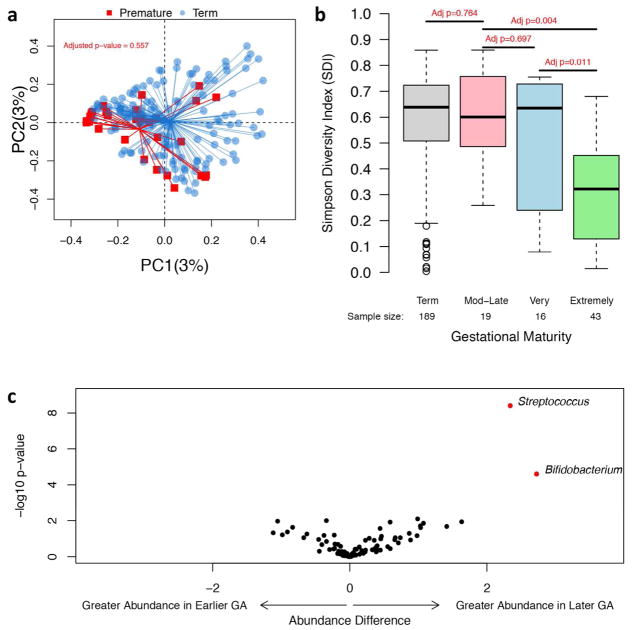
Bacterial Phylogenetic Relatedness Differences Between Premature and Term Infants
Bacterial phylogenetic relatedness differences between premature and term infants were evaluated at the 6-week time point to address the more mature, established microbiome in both groups. After adjusting for exposures (but not repeated measures, see Methods), the difference in phylogenetic relatedness between the two groups of infants was not significant (p=0.557, Figure 3a).
Figure 3. Bacterial phylogenetic relatedness differences between term and premature infants at 6 weeks of age (a), and bacterial alpha-diversity differences based on gestational maturity (b) and bacterial abundance differences between infants born at an earlier or later gestational age (c).
(a) Principal Coordinates Analysis plot showing bacterial phylogenetic relatedness differences between 6-week stool samples from premature (red) and term infants (blue). P-value is adjusted for exposures. PC1 = principal coordinate 1, PC2 = principal coordinate 2. Percentage refers to percentage of variance explained by the principal coordinate. (b) The bacterial alpha-diversity (SDI) of infant stool samples is indicated on the y-axis. P-value is adjusted for exposures and age (day of life). Infants are divided into groups based on gestational age at birth. Term is infants born at ≥37 weeks of gestation, moderate-late (Mod-Late) preterm infants are born at ≥32 weeks of gestation but <37 weeks, very preterm infants are born between 28 and <32 weeks of gestation, and extremely preterm infants are born between 24 and <28 weeks of gestation. Number of stool samples for each group is noted. However, exposure data for infants was occasionally not available, so number of samples evaluated for the adjusted analyses may be lower. (c) Bacterial taxa were evaluated for differences in abundance between infants born at a later compared to earlier gestational age at birth after with adjustment for exposures and age (day of life). On the x-axis, an abundance difference of greater than zero indicates that the bacterial taxon is found in greater abundance in infants born at a later gestational age (GA ≥32 weeks), while an abundance difference of less than zero indicates that the taxa is found in greater abundance in infants born at an earlier gestational age (GA <32 weeks). On the y-axis is the −log10 of the p-value for the abundance difference. A greater −log10 of the p-value indicates a more significant p-value. Red circles indicate taxa whose abundance difference is significant (p-value is <0.05) after adjusting for multiple comparisons.
Differences Among Premature Infants by Gestational Age at Birth
To test the hypothesis that gut bacterial community structure varied with degree of gestational immaturity at birth, we divided the premature infants into 3 groups: extremely premature infants (gestational age at birth <28 weeks), very premature infants (28≤ GA <32 weeks), and moderate-late premature infants (GA ≥32 weeks). We observed differences in bacterial alpha-diversity between extremely premature and moderate-late premature, and between extremely and very premature infants after adjusting for age and exposures (p=0.004 and p=0.011, respectively, Figure 3b). We did not find differences in bacterial alpha-diversity between very and moderate-late premature infants after accounting for exposures and age (p=0.697, Figure 3b). There were differences in bacterial phylogenetic relatedness at 6 weeks of age between extremely and very premature infants (p=0.033) after adjusting for exposures but not between very and moderate-late premature infants (p=0.138) or extremely and moderate-late premature infants (p=0.160).
Earlier Gestational Age at Birth Compared to Later Gestational Age at Birth
Given the clustering of many moderate-late premature samples with term samples, we divided the infants into two groups: those who had an earlier gestational age at birth (GA <32 weeks) and those who had a later gestational age (GA ≥32 weeks). Infants born at a later gestational age had greater abundance of Streptococcus and Bifidobacterium (p≪0.001, p=0.001, respectively, Figure 3c). At 6 weeks of age, after adjusting for exposures, infants born >32 weeks gestation had greater abundance of Bacteroides, while earlier GA infants < 32 weeks had greater abundance of Parabacteroides (p≪0.001 and p=0.005, respectively, Supplemental Figure S1). Across all time points, bacterial alpha-diversity was greater in later GA infants than in earlier GA infants, even after adjusting for exposures and age (day of life) (p=0.015, Figure 4a). Bacterial alpha-diversity did not, however, change differently over time between earlier and later GA infants (p=0.298). Similarly, at 6 weeks of age, bacterial alpha-diversity, after accounting for exposures, remained distinct between earlier and later GA infants (p=0.014). Bacterial phylogenetic relatedness differences between earlier versus later GA infants at 6 weeks of age, after adjusting for exposures, were marginally statistically significant (p=0.088, Figure 4b).
Figure 4. Bacterial alpha-diversity (a) and phylogenetic relatedness differences (b) between infants with an earlier or later gestational age at birth.
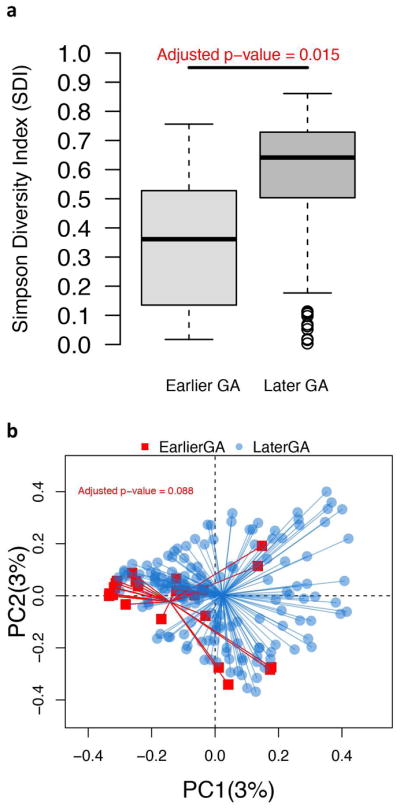
(a) Bacterial alpha-diversity differences in infants with an earlier gestational age at birth (<32 weeks GA, i.e. Earlier GA) and a later gestational age at birth (≥ 32 weeks, i.e. Later GA). P-value is adjusted for exposures and age (day of life). (b) Principal Coordinates Analysis plot showing bacterial phylogenetic relatedness differences between 6-week stool samples from infants with an earlier gestational age at birth (<32 weeks GA, shown in red) and a later gestational age at birth (≥ 32 weeks, shown in blue). P-value is adjusted for exposures. PC1 = principal coordinate 1, PC2 = principal coordinate 2. Percentage refers to percentage of variance explained by the principal coordinate.
Additionally, when comparing moderate-late premature infants to term infants, there were no apparent differences in bacterial alpha-diversity after adjusting for exposures and age (p=0.764), though the number of moderate-late premature compared to term samples was small (n=16 compared to n=174 after omitting samples missing exposure data). Bacterial phylogenetic relatedness differences at 6 weeks were not evident between moderate-late and term infants after accounting for exposures (p=0.354). The abundance of Pantoea was statistically significantly greater in moderate-late premature infants compared to term infants after adjusting for exposures and age (p=0.034), but there were no other statistically significant differences in bacterial abundance between these two groups of infants. These results indicate that moderate-late premature infants most likely have a community structure that more closely resembles term infants.
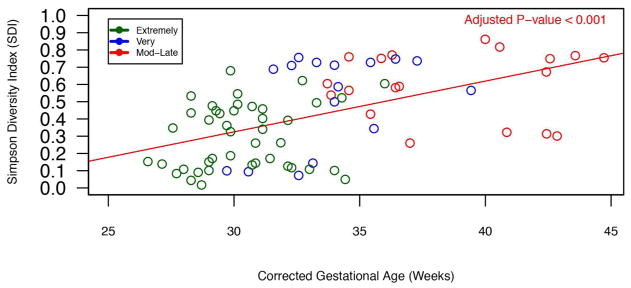
Analysis of Corrected Gestational Age in Premature Infants
Corrected gestational age was defined at gestational age at birth + day of life at time of sample collection. We compared bacterial composition in premature infants born at different gestational ages when they were at similar corrected gestational ages at time of sample collection (Supplemental Figure S2). While composition appears roughly different between infants born at different gestational ages, there were no significant differences in bacterial alpha-diversity between these groups of infants after accounting for exposures (Supplemental Table 1). Bacterial alpha-diversity does appear to increase as corrected gestational age increases (p=0.003, Figure 5).
Figure 5. Bacterial alpha-diversity in premature infants across corrected gestational age at time of sample collection.
The bacterial alpha-diversity (SDI) of stool samples from premature indicated on the y-axis. A straight line was fitted to the bacterial alpha-diversity data, and indicates the change in stool bacterial alpha-diversity over corrected gestational age (slope) in premature infants. The p-value is adjusted for exposures, and represents the independent effect of corrected gestational age on bacterial alpha-diversity. On the x-axis is the corrected gestational age (gestational age at birth + day of life) at which a stool sample was collected.
Associations with Exposures Among Premature Infants
We identified 3 potential exposures thought to affect premature infant gut microbial structure, which included newborn antibiotic exposure, delivery mode, and breastmilk exposure (Table 2). Additionally, we collected additional exposure data from the premature infants in the NICU, such as antibiotic exposure on day of sample collection and exclusive breastmilk feeding at time of sample collection (Table 3). Corrected gestational age at time of stool sample collection was also adjusted for. Among the premature infants, none of the three exposures (antibiotics in the first few days of life, a vaginal vs. C-section delivery, or breastmilk exposure) had statistically significant independent effects on bacterial alpha-diversity (p=0.311, p=0.324, p=0.660) after adjustment for corrected gestational age. Earlier gestational age at birth negatively associated with bacterial alpha-diversity, but it was not significant after adjusting for exposures and corrected gestational age (p=0.390). We also evaluated the effects of exposures and corrected gestational age on the abundance of the bacterial genera known to be abundant in term infants, such as Streptococcus, Bifidobacterium, Bacteroides, and Lactobacillus. Newborn antibiotic use was associated with lower Bifidobacterium and Bacteroides abundance (p=0.015 and p=0.041). Vaginal delivery was associated with greater Bacteroides abundance (p=0.007), while breastmilk exposure at time of sample collection was associated with a decreased abundance of Lactobacillus (p=0.017). Corrected gestational age at time of sample collection was positively associated with greater Lactobacillus and Streptococcus abundance (p=0.031 and p<0.001, respectively).
In the premature infant cohort in the NICU, after adjusting for corrected gestational age, no exposure was found to have significant independent effects on bacterial alpha-diversity, though corrected gestational age at time of sample collection had a positive independent effect (p=0.015). Consumption of breastmilk at time of sample collection had marginally significant effects on bacterial phylogenetic relatedness at 6 weeks after adjusting for other exposures and corrected gestational age (p=0.054). Antibiotics and corrected gestational age, but not delivery mode, exclusive breastmilk feeding or any breastmilk consumption at time of sample collection, had significant effects on bacterial abundance of Streptococcus, Bacteroides, and Lactobacillus. Antibiotic use at time of sample collection was associated with greater Bacteroides and Lactobacillus abundance (p=0.047 and p=0.042). Corrected gestational age at time of sample collection was positively associated with greater Lactobacillus and Streptococcus abundance (p=0.017 and p=0.021, respectively).
DISCUSSION
In our study, we identified differences in gut bacterial composition between premature and term infants in the first 6 weeks of life, using data from a cohort of premature infants in the NICU, as well as premature and term infants enrolled in a large, comprehensive molecular epidemiology study, the NHBCS. We found that dominant taxa differ between premature and term infants; however, there are no statistically significant differences in bacterial alpha-diversity, abundance, and phylogenetic relatedness after adjustment for the effects of exposures such as newborn antibiotic administration, delivery mode, and breastmilk exposure at time of sample collection. We also evaluated the effects of various exposures on the premature infant intestinal microbiota, but also did not find any significant effects on bacterial alpha-diversity or phylogenetic relatedness. We did find significant differences in gut bacterial alpha-diversity between premature infants depending on gestational age at birth, as well as between premature and term infants at 6 weeks of age.
The primary difference between premature and term infants with respect to dominant taxa was the decreased abundance of the genera Bifidobacterium, Bacteroides, and Streptococcus. We also observed decreased abundances of Bifidobacterium, Bacteroides, and Streptococcus in the earlier GA at birth infants compared to those born at a later GA. A paucity of Bacteroides, Bifidobacterium, Streptococcus, and Lactobacillus in premature infants have been described previously (14,16). Bifidobacterium, some species of which may help prevent colonization of the infant gut by pathogenic organisms (22), is not well established in the gut of premature infants born at a gestational age earlier than 33 weeks (15). In other studies of term, vaginally delivered infants, there is high abundance of Bacteroides and Bifidobacterium less than a week after birth (23). Bifidobacterium and Bacteroides are bacterial genera considered health-promoting and interact directly with the burgeoning immune system in infancy (22,24,25). Bacteroides fragilis has been found to produce a bacterial polysaccharide that aids in the maturation of the immune system and production of regulatory T cells (24–26), and in a murine model noted for gut barrier defects, oral treatment with B. fragilis reduced gut permeability and altered microbial composition (27). We did find that early antibiotic use was associated with lower Bifidobacterium and Bacteroides abundance in premature infants, suggesting that early antibiotic exposure can affect future gut bacterial composition among premature infants. Streptococcus is also known to be one of the first colonizers of the gut in term infants (28,29), and in our study, we found that it was not among the top 10 dominant taxa in premature infants, while it was among the top 4 dominant tax in our term infants. Caesarean-section delivery has been associated with depletion of Lactobacillus (30); however, we did not find that delivery mode was associated with Lactobacillus abundance in the premature infants in our study.
We found that after performing hierarchical clustering, extremely and very preterm infants clustered together (GA <32 weeks), but moderate-late preterm (32≤ GA <37) infant samples were interspersed among both the extremely and very preterm samples and the term samples. Furthermore, we found significant differences in the premature infant gut microbiota based on gestational age at birth. Extremely premature infants (born before 28 weeks of gestational age) had significantly lower bacterial alpha-diversity compared to very premature (GA ≥28 but <32 weeks) and moderate-late premature infants (GA ≥32 but <37 weeks) even after adjusting for exposures. There were also significant differences in bacterial phylogenetic relatedness between the extremely and very premature infants. These results suggest that gestational age at birth has important associations with gut bacterial structure in premature infants, whether it be related to the maturity of the intestinal tract and the bacteria that are able to colonize this intestinal environment, or potentially related to medical treatment and length of stay in a hospital environment.
We compared bacterial alpha-diversity and phylogenetic relatedness between the moderate-late preterm infants and term infants, and found that they did not differ even after accounting for exposures, supporting the finding of moderate-late preterm and term samples clustering together. Comparing the extremely and very preterm infants (GA <32 weeks) to the moderate-late preterm and term infants (GA ≥32 weeks), differences in bacterial alpha-diversity were identified. In an analysis of premature infants only, earlier gestational age was negatively associated with bacterial alpha-diversity, suggesting that greater gestational immaturity at birth is related to a less diverse gut microbiome. These results all together appear to suggest that infants born between 32 and 37 weeks of gestation have gut bacterial communities in the first 6 weeks of life are more similar to those of term infants than those of infants born before 32 weeks of gestation. This may point to the potential benefit of probiotic supplementation in extremely and very preterm infants, as their gut bacterial communities differ significantly from those of infants with a later gestational age at birth (≥32 weeks). Additionally, these differences in gut bacterial composition between infants born at an earlier versus a later gestational age may reflect differences in environmental exposures between these two groups of infants, as more premature infants were hospitalized, exposed to more antibiotics and other medical interventions, while moderate-late preterm and term infants likely hospitalized for much shorter periods or not hospitalized at all, and were much less likely to have experienced medical interventions.
We did observe an upward trend in bacterial alpha-diversity with increasing corrected gestational age in the premature infants. Though we did not observe significant similarities in bacterial composition among premature infants of different degrees of gestational prematurity at birth when they were at similar corrected gestational ages, there were no significant differences in bacterial alpha-diversity between groups of infants. Corrected gestational age had a significant positive independent effect on bacterial alpha-diversity in premature infants, as well as a positive effect on the abundance of the bacterial genera Lactobacillus and Streptococcus.
Limitations of this study include a relatively small number of premature infants enrolled compared to the number of term infants, and a much smaller number of longitudinal samples among the term infants compared to premature infants. Study subjects were drawn from a relatively homogeneous northern New England population. While this compromises the generalizability of our findings, it also reduces the sources of variation that could affect our observations. Also, two different DNA extraction kits were used, each for a different cohort, potentially confounding results comparing premature and term infants, and earlier GA at birth vs. later GA infants. Few studies have been published comparing the MoBio and Zymo DNA extraction methods, but one study suggests that representation of bacterial genera in samples does not significantly differ across these DNA extraction methods, though this study looked at plaque and saliva samples (31). A research report comparing our two kits showed that significantly different microbiomes were not produced if tested from the same intestinal sample, suggesting that the two kits give comparable results (32).
Our analysis of the effects of diet on the premature gut microbiome was limited since all of our premature infants had exposure to breastmilk at some point. However, recent research involving the NHBCS cohort suggests that infants fed both breastmilk and formula more closely resemble infants that are exclusively formula fed than infants that are exclusively breastmilk fed (21). Thus, while most of our premature infants were consuming breastmilk at time of stool sample collection, they were also often receiving human milk fortifier or formula. We were, however, able to identify a number of samples where the premature infants had only been exposed to breastmilk. Additionally, our premature infants in the NICU were often fed donor breastmilk when maternal breastmilk was not available. Donor breastmilk is pasteurized, which may have affected gut colonization patterns as breastmilk contains commensal bacteria (33). Finally, in the bacterial phylogenetic relatedness analyses, we had to assume that each sample was independent, which may have biased results since not all infants donated the same number of samples.
CONCLUSION
In our study of premature and term infants, we found that premature infants had lower abundance of a number of keystone bacterial genera found in healthy term infants, many of which are considered immune training and health-promoting. We found an association between early antibiotic use and lower Bifidobacterium and Bacteroides abundance in our premature infants, pointing to the effect of early antibiotic exposure on future gut bacterial composition. We also found significant differences in bacterial alpha-diversity between premature infants based on gestational age at birth, with lower bacterial alpha-diversity seen in infants with an earlier gestational age at birth. When we compared infants born at an earlier gestational age (GA <32 weeks) compared to infants born at a later gestational age (GA ≥32 weeks), we found differences in bacterial alpha-diversity (both at 6 weeks of age and across all time points). Bacterial alpha-diversity trended up with increased corrected gestational age. Our results suggest that premature infants with a later gestational age at birth resemble term infants, and that interventions to alter the gut microbiota may be of greatest value in extremely and very preterm infants.
Supplementary Material
Acknowledgments
Statement of Financial Support: NIH grants NIEHS P01 ES022832, US EPA RD83544201, NIGMS P20 GM104416, K01LM011985, R01AI59694, GM103534, GM103506; P20RR16448, 4UH3DK083993; K24AT003683, 5T32DK007301-35, AI116794, R01LM010098, NLM R01LM012723, OD UG3OD023275, the Hearst Foundation, the Joshua Burner Career Development Award through the Hitchcock Foundation (Dartmouth), Neukom Institute, and March of Dimes Ohio Prematurity Research Center Ohio Collaborative.
The authors would like to acknowledge the children and families who participated in our studies, for which we are very grateful. We would also like to acknowledge the nurses and staff involved in the collection of samples and data. Additionally, we’d like to thank Dr. Elizabeth Brickley for her help and suggestions.
Footnotes
Disclosure Statement: The authors declare that they have no competing interests or disclosures.
References
- 1.Duffy LC. Interactions mediating bacterial translocation in the immature intestine. J Nutr. 2000;130:432S–436S. doi: 10.1093/jn/130.2.432S. [DOI] [PubMed] [Google Scholar]
- 2.Sherman MP. New concepts of microbial translocation in the neonatal intestine: mechanisms and prevention. Clin Perinatol [Internet] 2010;37:565–79. doi: 10.1016/j.clp.2010.05.006. [cited 2014 Dec 17] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2933426&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carl Ma, Ndao IM, Springman aC, et al. Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis [Internet] 2014;58:1211–8. doi: 10.1093/cid/ciu084. [cited 2014 May 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24647013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tarr PI, Warner BB. Gut bacteria and late-onset neonatal bloodstream infections in preterm infants. Semin Fetal Neonatal Med [Internet] 2016:1–6. doi: 10.1016/j.siny.2016.06.002. Available from: [DOI] [PubMed]
- 5.Halpern MDDP. The role of intestinal epithelial barrier function in the development of NEC. Tissue Barriers. 2015;3:e1000707. doi: 10.1080/21688370.2014.1000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mshvildadze M, Neu J. The infant intestinal microbiome: friend or foe? Early Hum Dev. 2010;86(Suppl 1):67–71. doi: 10.1016/j.earlhumdev.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenwood C, Morrow AL, Lagomarcino AJ, et al. Early empiric antibiotic use in preterm infants is associated with lower bacterial diversity and higher relative abundance of Enterobacter. J Pediatr [Internet] 2014;165:23–9. doi: 10.1016/j.jpeds.2014.01.010. [cited 2014 Nov 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24529620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madan JC, Salari RC, Saxena D, et al. Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch Dis Child Fetal Neonatal Ed [Internet] 2012;97:F456–62. doi: 10.1136/fetalneonatal-2011-301373. [cited 2014 Jan 28]; Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3724360&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arboleya S, Sánchez B, Solís G, et al. Impact of Prematurity and Perinatal Antibiotics on the Developing Intestinal Microbiota: A Functional Inference Study. Int J Mol Sci [Internet] 2016;17:649. doi: 10.3390/ijms17050649. Available from: http://www.mdpi.com/1422-0067/17/5/649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibson MK, Wang B, Ahmadi S, et al. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat Microbiol [Internet] 2016;1:16024. doi: 10.1038/nmicrobiol.2016.24. Available from: http://www.nature.com/articles/nmicrobiol201624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacquot A, Neveu D, Aujoulat F, et al. Dynamics and clinical evolution of bacterial gut microflora in extremely premature patients. J Pediatr [Internet] 2011;158:390–6. doi: 10.1016/j.jpeds.2010.09.007. [cited 2014 Feb 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20961563. [DOI] [PubMed] [Google Scholar]
- 12.Mai V, Torrazza RM, Ukhanova M, et al. Distortions in development of intestinal microbiota associated with late onset sepsis in preterm infants. PLoS One [Internet] 2013;8:e52876. doi: 10.1371/journal.pone.0052876. [cited 2014 May 29] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3544792&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Y, Shan G, Sodergren E, Weinstock G, Walker WA, Gregory KE. Longitudinal analysis of the premature infant intestinal microbiome prior to necrotizing enterocolitis: A case-control study. PLoS One. 2015;10:1–16. doi: 10.1371/journal.pone.0118632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arboleya S, Binetti A, Salazar N, et al. Establishment and development of intestinal microbiota in preterm neonates. FEMS Microbiol Ecol. 2012;79:763–72. doi: 10.1111/j.1574-6941.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- 15.Butel M-J, Suau A, Campeotto F, et al. Conditions of bifidobacterial colonization in preterm infants: a prospective analysis. J Pediatr Gastroenterol Nutr. 2007;44:577–82. doi: 10.1097/MPG.0b013e3180406b20. [DOI] [PubMed] [Google Scholar]
- 16.Westerbeek EA, van den Berg A, Lafeber HN, Knol J, Fetter WP, van Elburg RM. The intestinal bacterial colonisation in preterm infants: a review of the literature. Clin Nutr. 2006;25:361–8. doi: 10.1016/j.clnu.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Madan JC, Salari RC, Saxena D, et al. Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch Dis Child Fetal Neonatal Ed [Internet] 2012;97:F456–62. doi: 10.1136/fetalneonatal-2011-301373. [cited 2014 Nov 18] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3724360&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chernikova DA, Koestler DC, Hoen AG, et al. Fetal exposures and perinatal influences on the stool microbiota of premature infants. J Matern Fetal Neonatal Med [Internet] 2016;29:99–105. doi: 10.3109/14767058.2014.987748. [cited 2014 Dec 17] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25394613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbert-Diamond D, Cottingham KL, Gruber JF, et al. Rice consumption contributes to arsenic exposure in US women. Proc Natl Acad Sci U S A [Internet] 2011;108:20656–60. doi: 10.1073/pnas.1109127108. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3251121&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farzan SF, Korrick S, Li Z, et al. In utero arsenic exposure and infant infection in a United States cohort: A prospective study. Environ Res. 2013;126:24–30. doi: 10.1016/j.envres.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Madan JC, Hoen AG, Lundgren SN, et al. Association of Cesarean Delivery and Formula Supplementation With the Intestinal Microbiome of 6-week -Old Infants. JAMA Pediatr [Internet] 2016;170:1–8. doi: 10.1001/jamapediatrics.2015.3732. Available from: http://archpedi.jamanetwork.com/article.aspx?articleid=2479466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butel MJ, Roland N, Hibert A, et al. Clostridial pathogenicity in experimental necrotising enterocolitis in gnotobiotic quails and protective role of bifidobacteria. J Med Microbiol. 1998;47:391–9. doi: 10.1099/00222615-47-5-391. [DOI] [PubMed] [Google Scholar]
- 23.Backhed F, Roswall J, Peng Y, et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe. 2015;17:690–703. doi: 10.1016/j.chom.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Round JL, Mazmanian SK. Inducible Foxp3+ regulatory T-cell development by a commensal bacterium of the intestinal microbiota. Proc Natl Acad Sci U S A. 2010;107:12204–9. doi: 10.1073/pnas.0909122107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazmanian SK, Liu CH, Tzianabos AO, Kasper DL. An immunomodulatory molecule of symbiotic bacteria directs maturation of the host immune system. Cell. 2005;122:107–18. doi: 10.1016/j.cell.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 26.Telesford KM, Yan W, Ochoa-Reparaz J, et al. A commensal symbiotic factor derived from Bacteroides fragilis promotes human CD39(+)Foxp3(+) T cells and Treg function. Gut Microbes [Internet] 2015;6:234–42. doi: 10.1080/19490976.2015.1056973. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsiao EY, McBride SW, Hsien S, et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell [Internet] 2013;155:1451–63. doi: 10.1016/j.cell.2013.11.024. [cited 2014 Mar 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24315484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stark PL, Lee A. The microbial ecology of the large bowel of breast-fed and formula-fed infants during the first year of life. J Med Microbiol. 1982;15:189–203. doi: 10.1099/00222615-15-2-189. [DOI] [PubMed] [Google Scholar]
- 29.Songjinda P, Nakayama J, Kuroki Y, et al. Molecular monitoring of the developmental bacterial community in the gastrointestinal tract of Japanese infants. Biosci Biotechnol Biochem [Internet] 2005;69:638–41. doi: 10.1271/bbb.69.638. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15784997. [DOI] [PubMed] [Google Scholar]
- 30.Dominguez-Bello MG, Costello EK, Contreras M, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107:11971–5. doi: 10.1073/pnas.1002601107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vesty A, Biswas K, Taylor MW, Gear K, Douglas RG. Evaluating the impact of DNA extraction method on the representation of human oral bacterial and fungal communities. PLoS One. 2017;12:1–13. doi: 10.1371/journal.pone.0169877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olsen K, Chaston J. Effects of Host Microbiota on Intestinal Fiber Content [Internet] 2016 Available from: http://jur.byu.edu/?p=20043.
- 33.Jost T, Lacroix C, Braegger C, Chassard C. Assessment of bacterial diversity in breast milk using culture-dependent and culture-independent approaches. Br J Nutr. 2013;110:1253–62. doi: 10.1017/S0007114513000597. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.