Abstract
The study investigated the over-time changes and racial/ethnic disparities in the quality of health care services for cigarette smoking cessation in the U.S. from 2007 to 2015. The primary measures included receiving a doctor's advice to quit smoking in the year before smoking cessation and using behavioral interventions for smoking cessation (telephone helplines and web-based interventions) while trying to quit smoking. The study was conducted from January to July 2018. We used merged data from the 2010–11 and 2014–15 Tobacco Use Supplement to the Current Population Survey. The sample sizes were 7011 and 12,025, respectively, for the analyses corresponding to two primary measures. The rate of receiving a doctor's advice to quit increased significantly from 66% (SE = 2%) in 2007 to 73% (SE = 4%) in 2015. The rate of usage of telephone helplines or web-based interventions for smoking cessation increased only from 3% (SE = 1%) in 2007 to 5% (SE = 1%) in 2015. These positive trends remained even after adjusting for several important factors. For both measures, the rates were consistently lower among Hispanic smokers than Non-Hispanic Black/African American and White smokers. Despite the availability of states' behavioral interventions for cessation of tobacco use, utilization of these interventions remains very low, indicating that smokers may not be aware of these free resources, may have misconceptions about these interventions being evidence-based, or there are barriers for using these interventions.
Keywords: Quality of healthcare services, Quit attempts, Racial/ethnic health disparities, Smoking cessation
Highlights
-
•
Receiving doctor's advice to quit smoking increased from 66% to 73% in 2007–15.
-
•
Using telephone helplines/web-based programs increased from 3% to 5% in 2007–15.
-
•
Hispanics were less likely to receive doctor's advice to quit than Non-Hispanic Whites.
1. Introduction
A doctor's advice to quit smoking is an important part of the Five A's strategic support for smoking cessation that utilizes the following five steps: Ask—Advise—Assess—Assist—Arrange (Fiore et al., 2008). A doctor's advice to quit smoking is essential to motivate smokers to quit smoking and to also facilitate successful smoking cessation (Aveyard et al., 2012; Bailey et al., 2018; Cahill et al., 2010; Fiore et al., 2008; Kottke et al., 1988; Lancaster and Stead, 2004; Russell et al., 1979; Stead et al., 2013, Stead et al., 2008; Tomar et al., 1996; Williams et al., 2014; Zhang et al., 2016; Zwar et al., 2014). However, based on smokers' reports, the success rate of receiving a doctor's advice to quit smoking has been relatively low. Specifically, it was 53.3% in 2000, 58.9% in 2005, and 50.7% in 2010 (Kruger et al., 2012).
The rate of receiving a doctor's advice to quit smoking differed across populations of smokers with diverse sociodemographic characteristics. For example, the rate was lower among Hispanic smokers and Non-Hispanic (NH) Black/African American (BAA) smokers relative to NH White smokers (Cokkinides et al., 2008; Houston et al., 2005; Kruger et al., 2012; Lopez-Quintero et al., 2006; Tomar et al., 1996). Specifically, in the U.S. in the period from 2001 to 2010, among current smokers and former smokers (who quit smoking in the past 12 months) who reported seeing a healthcare professional in the past 12 months, the rate of receiving advice to quit was 34.7% for Hispanic, 46.3% for NH BAA, 50.2% for NH White and 47.8% for other NH adults (Centers for Disease Control and Prevention, 2011). In addition, the rate was higher for older than younger smokers (Anda et al., 1987; Browning et al., 2008; Denny et al., 2003; Kruger et al., 2012; Tomar et al., 1996), higher for women than men (Denny et al., 2003; Kruger et al., 2012), and higher- than lower-educated smokers (Houston et al., 2005). However, another study (Kruger et al., 2012) indicated that the prevalence was greater for smokers without a high school diploma rather than higher-educated smokers (but not all pairwise differences were significant).
If a patient is willing to make a quit attempt, a doctor will also recommend using an intervention or pharmacological treatment for smoking cessation, i.e., the “Assist” step in the Five A's framework (Fiore et al., 2008). Nonetheless, prevalence of use of behavioral and pharmacological aids during quit attempts is relatively low. Among recent quitters, i.e., those who quit smoking within a year prior to the assessment, the prevalence of use of behavioral interventions is about 8.0% and the prevalence of use of pharmacological aids is 27.5% (Soulakova and Crockett, 2017). Among long-term quitters, i.e., former smokers who quit smoking one year before the assessment or longer, the prevalence estimates are even lower (Soulakova and Crockett, 2017). Telephone helplines (also termed “quit lines”) and web-based programs and tools are among the most common behavioral interventions for smoking cessation (Soulakova and Crockett, 2017; U.S. Department of Health and Human Services, 2014). These methods are evidence-based and cost-effective (Danielsson et al., 2014; Fiore et al., 2008; Graham et al., 2007; Hopkins et al., 2001; Lustria et al., 2013; Nash et al., 2015; Owen, 2000; Smit et al., 2012; Stead et al., 2007; U.S. Department of Health and Human Services, 2014; Whittaker et al., 2009; Zbikowski et al., 2011; Zhu et al., 2002, Zhu et al., 1996).
As of 2006, the U.S. network of telephone helplines for smoking cessation provided free services to smokers in all 50 states, the District of Columbia and Puerto Rico via a single toll-free number (1-800-QUIT-NOW) (Keller et al., 2010; Lichtenstein et al., 2010). Despite potential benefits of this network, helplines are not widely used in practice: the prevalence of use was about 1% or less until 2005–06 (Cummins et al., 2007; Keller et al., 2010). Even among smokers who were aware of the telephone helpline, the rate was relatively low – about 8% in 2008–10 (Schauer et al., 2014). Telephone helplines are more commonly used among NH BAA smokers (Zhu et al., 2011) and less commonly used among Hispanic smokers (Zhu et al., 2000) in comparison to NH White smokers. Helplines were also more commonly used among younger than older smokers (Prout et al., 2002; Schauer et al., 2014), women than men (Prout et al., 2002; Zhu et al., 2000), and higher- than lower-educated smokers (Zhu et al., 2011, Zhu et al., 2000).
Currently, the majority of U.S. states offer free web-based interventions for smoking cessation (Neri et al., 2016). Nonetheless, the rate of use of web-based interventions for smoking cessation is very low and is even lower than the rate of use of telephone helplines (Soulakova and Crockett, 2017; Zbikowski et al., 2011). Moreover, the populations of smokers who used either a state-sponsored telephone helpline or a state-sponsored web-based intervention were recently described (Nash et al., 2015; Neri et al., 2016). For example, analysis of data from four states (Alabama, Arizona, Florida, and Vermont) indicated that users of telephone helplines are older (on average) than users of web-based interventions. They also differ in terms of several other sociodemographic characteristics, such as race/ethnicity and education (Neri et al., 2016).
The goal of our study was to assess the progress made in U.S. healthcare for smoking cessation in the period from 2007 to 2015. We assessed this goal through identifying (1) changes in prevalence of receiving a doctor's advice to quit smoking in the past 12 months before smoking cessation, (2) changes in prevalence of using behavioral interventions for smoking cessation (such as telephone helplines and web-based programs) while trying to quit smoking, and (3) whether these changes were similar across diverse racial/ethnic groups. The population of interest were adult former smokers who quit smoking in the period from 2007 to 2015.
2. Methods
2.1. Data
To examine the over-time trends, we analyzed the 2010–11 and 2014–15 Tobacco Use Supplement to the Current Population Survey (TUS-CPS) data (U.S. Department of Commerce and U.S. Census Bureau, 2016). When merging data from two survey periods, we rescaled the weights accordingly to the TUS-CPS methodological guideline (U.S. Department of Commerce and U.S. Census Bureau, 2016). The respondents were 18+ year-old adults who reported being a former smoker at the time of the survey and indicated that they had quit at least seven days ago and no longer than three years ago. Only former smokers who had quit within the past three years prior to the assessment reported detailed information regarding their last quit attempts. For convenience of wording, we term these subjects “smokers” when referring to the time prior to smoking cessation and “former smokers” when referring to the time of the survey.
To assess the changes in prevalence of receiving a doctor's advice to quit smoking we analyzed the cohort (n = 7011) of all former smokers who indicated visiting a doctor or a dentist in the past 12 months prior to quitting. To assess the changes in prevalence of using behavioral interventions (telephone helplines and web-based interventions) we analyzed the cohort (n = 12,025) of all former smokers who reported whether they used or did not use telephone helplines and/or web-based programs for smoking cessation while trying to quit smoking. While these two cohorts were analyzed separately, they overlap: 6996 (34%) former smokers reported both, whether they received a doctor's advice to quit and whether they used behavioral interventions for smoking cessation. Table 1 depicts the sociodemographic characteristics for each cohort. In addition, in each cohort, about 19% resided in the Northeast, 27% resided in the Midwest, 34% resided in the South and 20% resided in the West; 84% resided in metropolitan areas and 16% in non-metropolitan; and about 65% of former smokers were interviewed by phone and 35% of former smokers were interviewed in-person.
Table 1.
Characteristics of former smokers; 2010–11 and 2014–15 TUS-CPS.
| Characteristics | Cohort: doctor's advice to quit smoking |
Cohort: behavioral interventions for smoking cessation |
||
|---|---|---|---|---|
| Sample count | Percent based on population counts | Sample count | Percent based on population counts | |
| Age | ||||
| 18–24 | 479 | 11.1 | 1084 | 14.3 |
| 25–44 | 2740 | 39.8 | 5365 | 45.0 |
| 45–64 | 2728 | 36.3 | 4158 | 31.4 |
| 65+ | 1064 | 12.8 | 1418 | 9.3 |
| Sex | ||||
| Male | 3185 | 48.6 | 6057 | 54.2 |
| Female | 3826 | 51.4 | 5968 | 45.8 |
| Race/ethnicity | ||||
| Non-Hispanic (NH) White | 5897 | 80.6 | 9620 | 75.2 |
| NH Black/African American | 445 | 7.5 | 872 | 8.5 |
| NH American Indian/Alaska Native | 85 | 0.8 | 152 | 0.9 |
| NH Asian | 99 | 1.7 | 242 | 2.5 |
| NH Hawaiian/Pacific Islander | 14 | 0.1 | 38 | 0.3 |
| NH Multiracial | 127 | 2.0 | 206 | 1.7 |
| Hispanic | 344 | 7.2 | 895 | 10.8 |
| Marital status | ||||
| Married (living with a spouse) | 3411 | 47.0 | 5605 | 44.4 |
| Widowed, divorced or separated | 1960 | 25.7 | 3045 | 22.8 |
| Never married | 1640 | 27.2 | 3375 | 32.8 |
| Education level | ||||
| Below high school | 648 | 9.2 | 1242 | 11.0 |
| High school or equivalent | 2198 | 30.5 | 3935 | 31.9 |
| Some college, bachelor's degree or equivalent | 3692 | 53.8 | 6122 | 51.4 |
| Graduate degree | 473 | 6.5 | 726 | 5.7 |
| Employment status | ||||
| Employed (at work or absent) | 4135 | 59.8 | 7550 | 63.8 |
| Unemployed | 392 | 6.3 | 761 | 7.2 |
| Not in labor force | 2484 | 33.8 | 3714 | 29.0 |
| Sample size (population count) | 7011 (4,606,481) | 12,025 (8,357,950) | ||
2.2. Measures
The first primary measure “receiving a doctor's advice to quit smoking” was defined using responses to two 2010–11 survey items (“During the 12 months before you completely quit smoking, did any medical doctor advise you to stop smoking?” and “During the 12 months before you completely quit smoking, did any dentist advise you to stop smoking?”) and one 2014–15 survey item (“During the 12 months before you completely quit smoking, did any medical doctor advise you to stop smoking?”); the item referring to a dentist was removed from the 2014–15 survey. This measure was defined only for former smokers who reported that they saw a medical doctor (or dentist) in the past 12 months. Thus, our investigation does not include smokers who did not see a doctor in the past 12 months and does not address accessibility to healthcare services.
The second primary measure, “using behavioral interventions for smoking cessation”, was based on two survey items: “When you quit smoking completely, did you use a telephone helpline or quit line?” and “When you quit smoking completely, did you use the internet or a web-based program or tool?”. We note that the respondents to 2014–15 TUS-CPS were not asked about the use of other types of behavioral interventions (such as one-on-one counseling and stop smoking clinic classes or support groups) which were surveyed in 2010–11 TUS-CPS (Soulakova and Crockett, 2017).
The “year of smoking cessation” measure was defined using reported time since smoking cessation and date of the survey as follows. First, the time since smoking cessation (days) was defined using responses to the survey item “About how long has it been since you completely quit smoking cigarettes?” Second, we used the date (month and year) when the survey was administered – that is May 2010, August 2010, January 2011, July 2014, January 2015 and May 2015 – to project the reported time from smoking cessation to a specific year in the period. Because the maximum time since smoking cessation was three years (the minimum was seven days) and the earliest survey was in May 2010 (the latest was in May 2015), the resulting years of smoking cessation covered 2007 to 2015. The annual sample sizes varied from 226 (2015) to 1195 (2010) for the first primary measure (receiving doctor's advice to quit) and from 380 (2015) to 1898 (2014) for the second primary measure (using behavioral interventions for smoking cessation).
2.3. Statistical analysis
First, we derived the annual prevalence estimates for each primary measure in the period from 2007 to 2015. These estimates and corresponding standard errors were based on the main survey weight and 160 replicate weights and thus, are expected to accurately estimate the population prevalence (and standard errors of the estimates). We did not adjust for any specific characteristics of former smokers when deriving the annual prevalence estimates; estimation was done using SAS®9.4 (SAS Institute Inc., 2014).
Then we performed the main statistical analyses that incorporated building and fitting two multiple logistic regression models (for complex survey sampling), one for the logit of the probability of receiving a doctor's advice to quit smoking and the second for the logit of the probability of using behavioral interventions for smoking cessation while trying to quit smoking. Each model included former smokers' race/ethnicity and the year of smoking cessation while controlling for former smokers' sociodemographic characteristics (age, sex, marital status, highest education level, employment status, metro/non-metro area of residency, and U.S. region of residency), and survey mode (phone, in-person). We also explored the significance of the survey period (2010–11, 2014–15), but because this factor was not significant in any model (p > 0.050), it was not included in the final models.
The final models for receiving a doctor's advice to quit smoking (Likelihood Ratio χ2 = 266,816, df = 18, p < 0.001) and using behavioral interventions for smoking cessation (Likelihood Ratio χ2 = 68,258, df = 18, p < 0.001) were used to assess the odds for each primary measure associated with the year of smoking cessation and also to perform multiple comparisons for diverse racial/ethnic groups relative to NH Whites. Bonferroni correction for multiplicity was used when computing the adjusted p-values. The overall significance level was 5% for each model. Because the sample size for NH Hawaiian/Pacific Islanders (HPI) was insufficient, this group was not included in the models. Specifically, only 4 out of 14 HPI former smokers reported receiving a doctor's advice to quit and none out of 38 HPI former smokers reported using a behavioral intervention for smoking cessation. In addition, other racial/ethnic groups had insufficient sample sizes when limiting to a certain year of smoking cessation. Thus, we performed an additional exploration of the overall patterns for NH White, NH BAA, and Hispanic smokers over the three time periods, 2007–09, 2010–12 and 2013–15.
In all analyses we incorporated Balanced Repeated Replications for variance estimation (Wolter, 2007) with the main weight and 160 replicate weights (U.S. Department of Commerce and U.S. Census Bureau, 2016). Models were built and fitted using SAS®9.4 (SAS Institute Inc., 2014).
3. Results
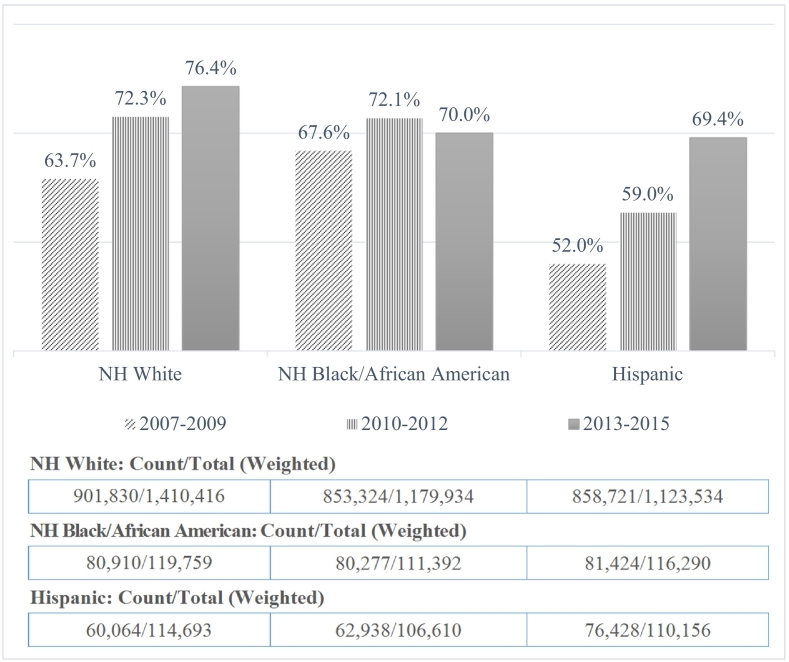
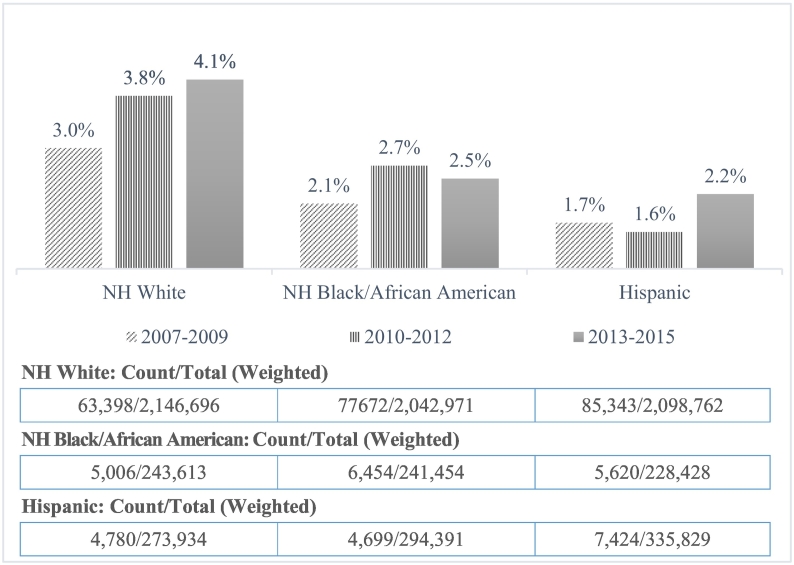
Fig. 1, Fig. 2 illustrate the annual prevalence (these estimates are not adjusted for other factors) of receiving a doctor's advice to quit smoking when visiting a doctor in the past 12 months prior to smoking cessation and using behavioral interventions for smoking cessation while trying to quit smoking, respectively. Overall, there was a significant difference across the annual rates of receiving a doctor's advice to quit (p < 0.001) but there was not a significant difference across the annual rates of using behavioral interventions. Fig. 3, Fig. 4 depict over-time differences in the prevalence for the three largest racial/ethnic groups.
Fig. 1.
Prevalence (SE's ≤ 3.8%) of receiving doctor's advice to quit smoking (unadjusted for other factors) and weighted count (top) and total (bottom); 2010–11 and 2014–15 TUS-CPS.
Fig. 2.
Prevalence (SE's ≤ 1.2%) of using behavioral interventions (unadjusted for other factors), weighted count (top) and total (bottom); 2010–11 and 2014–15 TUS-CPS.
Fig. 3.
Prevalence (SE's ≤ 5.3%) of receiving doctor's advice to quit smoking (unadjusted for other factors); 2010–11 and 2014–15 TUS-CPS.
Fig. 4.
Prevalence (SE's ≤ 0.5%) of using behavioral interventions for smoking cessation (unadjusted for other factors); 2010–11 and 2014–15 TUS-CPS.
Table 2 depicts the results based on the models for all significant main effects. The effect of year of smoking cessation was significant in both models: β = 0.097, p < 0.001 in the model for receiving a doctor's advice to quit smoking and β = 0.060, p = 0.011 in the model for using behavioral interventions for smoking cessation. The odds of receiving a doctor's advice to quit as well as the odds of using behavioral interventions grew from year to year.
Table 2.
Comparisons for all significant factors in the models; 2010–11 and 2014–15 TUS-CPS.
| Characteristic | Odds ratio | Simultaneous confidence intervals | Adjusted p-value |
|---|---|---|---|
| Receiving doctor's advice to quit smoking | |||
| Age (overall p < 0.001) | |||
| 18–24 | 1.00 | Reference | NA |
| 25–44 | 1.78 | (1.33: 2.38) | <0.001 |
| 45–64 | 3.04 | (2.21: 4.19) | <0.001 |
| 65+ | 4.22 | (3.03: 5.89) | <0.001 |
| Race/ethnicity (overall p = 0.009) | |||
| NH White | 1.00 | Reference | NA |
| NH Black/African American | 0.87 | (0.59: 1.28) | NS |
| NH American Indian/Alaska Native | 0.60 | (0.25: 1.43) | NS |
| NH Asian | 0.90 | (0.46: 1.77) | NS |
| NH Multiracial | 1.59 | (0.76: 3.34) | NS |
| Hispanic | 0.66 | (0.47: 0.92) | 0.006 |
| Education (overall p < 0.001) | |||
| Below high school | 1.00 | Reference | NA |
| High school or equivalent | 0.84 | (0.60: 1.17) | NS |
| Some college, bachelor's degree or equivalent | 0.70 | (0.51: 0.95) | 0.018 |
| Graduate degree or equivalent | 0.54 | (0.35: 0.82) | 0.001 |
| Year of smoking cessation (p < 0.001) | |||
| Previous year | 1.00 | Reference | NA |
| Current year | 1.10 | (1.07: 1.13) | NA |
| Using behavioral interventions for smoking cessation | |||
| Age (overall p < 0.001) | |||
| 18–24 | 1.00 | Reference | NA |
| 25–44 | 2.93 | (1.32: 6.49) | 0.004 |
| 45–64 | 3.70 | (1.69: 8.10) | <0.001 |
| 65+ | 2.81 | (1.17: 6.75) | 0.014 |
| Sex (p = 0.003) | |||
| Female | 1.00 | Reference | NA |
| Male | 0.71 | (0.56: 0.89) | NA |
| Year of smoking cessation (p = 0.011) | |||
| Previous year | 1.00 | Reference | NA |
| Current year | 1.06 | (1.01: 1.11) | NA |
Note. Each model included race/ethnicity and year of smoking cessation, and controlled for age, sex, education, U.S. region of residency, metropolitan area of residency, and survey mode as the main effects; NS stands for not significant; NA stands for not applicable.
The odds of receiving a doctor's advice to quit were significantly associated with the former smoker's race/ethnicity (overall p = 0.009). The prevalence of receiving doctor's advice to quit smoking (adjusted for other factors) was 69.7% for NH White, 66.7% for NH BAA, 57.8% for NH American Indian/Alaska Native, 67.5% for NH Asian, 78.6% for NH Multiracial, and 60.3% for Hispanic smokers. However, there was only one significant difference relative to NH White smokers: the prevalence was smaller for Hispanic smokers relative to NH White smokers (adjusted p = 0.006). The odds of using behavioral interventions for smoking cessation were not significantly associated with a smoker's race/ethnicity.
Table 2 illustrates additional results. The odds of receiving a doctor's advice to quit as well as using behavioral interventions were significantly higher for all age groups (i.e., 18–24, 25–44 and 45–64 years old) relative to the 65+ year-old group (all adjusted p′s < 0.050). In addition, the odds of receiving a doctor's advice to quit varied across smokers' education level: the odds were higher for smokers without a complete high school education relative to smokers with other levels of education, but the relative difference was significant only for those who had at least some college education or equivalent. The odds of using behavioral interventions were significantly lower for male smokers than female smokers.
4. Discussion
4.1. Conclusion
The study indicates the overall positive trends in annual prevalence of receiving a doctor's advice to quit smoking as well as using behavioral interventions for smoking cessation among former smokers who quit smoking in the period from 2007 to 2015. The prevalence of receiving a doctor's advice to quit smoking increased from 66% in 2007 to 73% in 2015. The prevalence of using a behavioral intervention for smoking cessation such as a telephone helpline or a web-based program increased from 3% in 2007 to 5% in 2015. These trends suggest certain improvements in health care for smoking cessation but they also point to under-use of behavioral interventions in the U.S. Low prevalence of use of behavioral interventions could be due to unawareness of free resources offered by the state (Schauer et al., 2014). Because visiting a healthcare professional or receiving cessation-related information from media is positively associated with improved awareness of telephone helplines (Schauer et al., 2014), promoting interventions for smoking cessation in healthcare settings and media could be highly beneficial for educating smokers and encouraging them to use these interventions.
The increase in prevalence of receiving doctor's advice to quit smoking and using behavioral interventions was not uniform among diverse racial/ethnic groups of smokers. Unadjusted analyses indicated that the highest increase in prevalence of receiving a doctor's advice to quit was observed for Hispanic smokers but the highest increase in prevalence of using behavioral interventions was observed for NH White smokers.
After adjusting for other factors, the overall prevalence of receiving a doctor's advice to quit was significantly lower for Hispanic than NH White smokers. This result is consistent with previous findings (Cokkinides et al., 2008; Kruger et al., 2012; Lopez-Quintero et al., 2006; Tomar et al., 1996). The underlying reason for the relatively low prevalence of being advised to quit among Hispanic smokers is not clear; it could be that Hispanic smokers are less likely to receive screening for smoking when visiting a healthcare professional (Jamal et al., 2012). In addition, among low-language-acculturated Hispanic smokers, the language barrier can be an obstacle for these screenings and discussions when visiting a doctor (Juckett, 2013; Zinser et al., 2011). The overall prevalence of using behavioral interventions did not differ significantly across racial/ethnic groups.
4.2. Limitations and future directions
The study has several limitations. First, the primary measures were based on former smokers' retrospective reports of their quitting behaviors and events preceding their smoking cessation in the past three years. Recalling and reporting behaviors and events that occurred in the past may introduce some response bias in the TUS-CPS reports (Soulakova et al., 2015, Soulakova et al., 2013). Second, because current and former smokers responded to two different sets of questions, we considered only former smokers in this study. Thus, results should not be generalized to current smokers who had (unsuccessful) quit attempts. In addition, while we attempted to perform comparisons for diverse racial/ethnic groups, due to small group sample sizes for specific years, the insignificant results could be due to lack of statistical power. Another limitation is that we did not address accessibility to healthcare services and availability of medical insurance among smokers. Prior research indicated discrepancies in the rate of receiving a doctor's advice to quit smoking across insurance types: the lowest rate of receiving advice corresponded to uninsured patients (35.3%) and the highest rate corresponded to patients enrolled in Medicare plan (59.0%) (Centers for Disease Control and Prevention, 2011).
Future studies could explore whether the patients' reports agree with the medical records, e.g., it could be that the healthcare providers recommend smokers to use behavioral interventions though the patients do not recall/report these recommendations. In addition, it would be of interest to estimate the rate of receiving a doctor's advice to quit smoking and the rate of using interventions for smoking cessation among smokers who tried to quit smoking but relapsed. In these studies, electronic health records could offer a valuable data source, especially for estimating the longitudinal trends (Stevens et al., 2016).
Funding
This work was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health [R01MD009718]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interests
There is no conflict of interests.
Acknowledgements
We would like to thank the editor and reviewers for providing us with their suggestions. These suggestions were incorporate in the revised draft. We would also like to thank James Holland and Richard Pack for editing the draft and helping us improve the manuscript.
References
- Anda R.F., Remington P.L., Sienko D.G., Davis R.M. Are physicians advising smokers to quit. J. Am. Med. Assoc. 1987;257:1916–1919. [PubMed] [Google Scholar]
- Aveyard P., Begh R., Parsons A., West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012;107:1066–1073. doi: 10.1111/j.1360-0443.2011.03770.x. [DOI] [PubMed] [Google Scholar]
- Bailey S.R., Stevens V.J., Fortmann S.P. Long-term outcomes from repeated smoking cessation assistance in routine primary care. Am. J. Health Promot. 2018 doi: 10.1177/0890117118761886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning K.K., Ferketich A.K., Salsberry P.J., Wewers M.E. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob. Res. 2008;10:55–61. doi: 10.1080/14622200701704905. [DOI] [PubMed] [Google Scholar]
- Cahill K., Lancaster T., Green N. Stage-based interventions for smoking cessation. In: Cahill K., editor. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; Chichester, UK: 2010. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control & Prevention Quitting smoking among adults — United States, 2001–2010. Morb. Mortal. Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- Cokkinides V.E., Halpern M.T., Barbeau E.M., Ward E., Thun M.J. Racial and ethnic disparities in smoking-cessation interventions. Am. J. Prev. Med. 2008;34:404–412. doi: 10.1016/j.amepre.2008.02.003. [DOI] [PubMed] [Google Scholar]
- Cummins S.E., Bailey L., Campbell S., Koon-Kirby C., Zhu S.-H. Tobacco cessation quitlines in North America: a descriptive study. Tob. Control. 2007;16:i9–i15. doi: 10.1136/tc.2007.020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsson A.-K., Eriksson A.-K., Allebeck P. Technology-based support via telephone or web: a systematic review of the effects on smoking, alcohol use and gambling. Addict. Behav. 2014;39:1846–1868. doi: 10.1016/j.addbeh.2014.06.007. [DOI] [PubMed] [Google Scholar]
- Denny C.H., Serdula M.K., Holtzman D., Nelson D.E. Physician advice about smoking and drinking: are U.S. adults being informed? Am. J. Prev. Med. 2003;24:71–74. doi: 10.1016/s0749-3797(02)00568-8. [DOI] [PubMed] [Google Scholar]
- Fiore M.C., Jaén C.R., Baker T.B. Clinical Practice Guideline. Executive Summary. U.S. Department of Health and Human Services. Public Health Service; Rockville, MD: 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- Graham A.L., Cobb N.K., Raymond L., Sill S., Young J. Effectiveness of an internet-based worksite smoking cessation intervention at 12 months. J. Occup. Environ. Med. 2007;49:821–828. doi: 10.1097/JOM.0b013e3180d09e6f. [DOI] [PubMed] [Google Scholar]
- Hopkins D.P., Briss P.A., Ricard C.J. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am. J. Prev. Med. 2001;20:16–66. doi: 10.1016/s0749-3797(00)00297-x. [DOI] [PubMed] [Google Scholar]
- Houston T.K., Scarinci I.C., Person S.D., Greene P.G. Patient smoking cessation advice by health care providers: the role of ethnicity, socioeconomic status, and health. Am. J. Public Health. 2005;95:1056–1061. doi: 10.2105/AJPH.2004.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A., Dube S.R., Malarcher A.M., Shaw L., Engstrom M.C. Tobacco use screening and counseling during physician office visits among adults—National ambulatory medical care survey and national health interview survey, United States, 2005–2009. Morb. Mortal. Wkly Rep. 2012;61:38–45. [PubMed] [Google Scholar]
- Juckett G. Caring for Latino patients. Am. Fam. Physician. 2013;87:48–56. [PubMed] [Google Scholar]
- Keller P.A., Feltracco A., Bailey L.A. Changes in tobacco quitlines in the United States, 2005–2006. Prev. Chronic Dis. 2010;7:1–6. [PMC free article] [PubMed] [Google Scholar]
- Kottke T.E., Battista R.N., DeFriese G.H., Brekke M.L. Attributes of successful smoking cessation interventions in medical practice: a meta-analysis of 39 controlled trials. J. Am. Med. Assoc. 1988;259:2882–2889. doi: 10.1001/jama.259.19.2883. [DOI] [PubMed] [Google Scholar]
- Kruger J., Shaw L., Kahende J., Frank E. Health care providers' advice to quit smoking, national health interview survey, 2000, 2005, and 2010. Prev. Chronic Dis. 2012;9 doi: 10.5888/pcd9.110340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster T., Stead L. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2004:1–41. doi: 10.1002/14651858.CD000165.pub2. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E., Zhu S.-H., Tedeschi G.J. Smoking cessation quitlines: an underrecognized intervention success story. Am. Psychol. 2010;65:252–261. doi: 10.1037/a0018598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Quintero C., Crum R.M., Neumark Y.D. Racial/ethnic disparities in report of physician-provided smoking cessation advice: analysis of the 2000 National Health Interview Survey. Am. J. Public Health. 2006;96:2235–2239. doi: 10.2105/AJPH.2005.071035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria M.L.A., Noar S.M., Cortese J., Van Stee S.K., Glueckauf R.L., Lee J. A meta-analysis of web-delivered tailored health behavior change interventions. J. Health Commun. 2013;18:1039–1069. doi: 10.1080/10810730.2013.768727. [DOI] [PubMed] [Google Scholar]
- Nash C.M., Vickerman K.A., Kellogg E.S., Zbikowski S.M. Utilization of a Web-based vs integrated phone/Web cessation program among 140,000 tobacco users: an evaluation across 10 free state quitlines. J. Med. Internet Res. 2015;17:1–25. doi: 10.2196/jmir.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neri A.J., Momin B.R., Thompson T.D. Use and effectiveness of quitlines versus Web-based tobacco cessation interventions among 4 state tobacco control programs. Cancer. 2016;122:1126–1133. doi: 10.1002/cncr.29739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen L. Impact of a telephone helpline for smokers who called during a mass media campaign. Tob. Control. 2000;9:148–154. doi: 10.1136/tc.9.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prout M.N., Martinez O., Ballas J. Who uses the smoker's quitline in Massachusetts? Tob. Control. 2002;11:ii74–ii75. doi: 10.1136/tc.11.suppl_2.ii74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell M.A.H., Wilson C., Taylor C., Baker C.D. Effect of general practitioners' advice against smoking. Br. Med. J. 1979;2:231–235. doi: 10.1136/bmj.2.6184.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS Institute Inc.; Cary, NC, USA: 2014. SAS/STAT® 13.1 User's Guide. [Google Scholar]
- Schauer G.L., Malarcher A.M., Zhang L., Engstrom M.C., Zhu S.-H. Prevalence and correlates of quitline awareness and utilization in the United States: an update from the 2009–2010 National Adult Tobacco Survey. Nicotine Tob. Res. 2014;16:544–553. doi: 10.1093/ntr/ntt181. [DOI] [PubMed] [Google Scholar]
- Smit E.S., de Vries H., Hoving C. Effectiveness of a Web-based multiple tailored smoking cessation program: a randomized controlled trial among Dutch adult smokers. J. Med. Internet Res. 2012;14:1–12. doi: 10.2196/jmir.1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soulakova J.N., Crockett L.J. Unassisted quitting and smoking cessation methods used in the United States: analyses of 2010–2011 Tobacco Use Supplement to the Current Population Survey Data. Nicotine Tob. Res. 2017;20:30–39. doi: 10.1093/ntr/ntw273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soulakova J.N., Bright B.C., Crockett L.J. On consistency of self-and proxy-reported regular smoking initiation age. J. Subst. Abus. Alcohol. 2013;1:1001–1017. [PMC free article] [PubMed] [Google Scholar]
- Soulakova J.N., Bright B.C., Crockett L.J. Perception of time since smoking cessation: time in memory can elapse faster. J. Addict. Behav. Ther. Rehabil. 2015;4 doi: 10.4172/2324-9005.1000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead L.F., Perera R., Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob. Control. 2007;16:i3–i8. doi: 10.1136/tc.2006.019737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead L.F., Bergson G., Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2008;2:1–56. doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- Stead L.F., Buitrago D., Preciado N., Sanchez G., Hartmann-Boyce J., Lancaster T. Physician advice for smoking cessation. Cochrane Libr. 2013 doi: 10.1002/14651858.CD000165.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens V.J., Solberg L.I., Bailey S.R. Assessing trends in tobacco cessation in diverse patient populations. Nicotine Tob. Res. 2016;18:275–280. doi: 10.1093/ntr/ntv092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar S.L., Husten C.G., Manley M.W. Do dentists and physicians advise tobacco users to quit? J. Am. Dent. Assoc. 1996;127:259–265. doi: 10.14219/jada.archive.1996.0179. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Commerce, U.S. Census Bureau . 2016. National Cancer Institute and Food and Drug Administration Co-sponsored Tobacco Use Supplement to the Current Population Survey. 2014–15. ( https://cancercontrol.cancer.gov/brp/tcrb/tus-cps/ Technical Documentation https://www.census.gov/programs-surveys/cps/technical-documentation/complete.html) [Google Scholar]
- U.S. Department of Health and Human Services Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. The health consequences of smoking—50 years of progress: a report of the Surgeon General. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf
- Whittaker R., Borland R., Bullen C., Lin R.B., McRobbie H., Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2009:4. doi: 10.1002/14651858.CD006611.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R.J., Masica A.L., McBurnie M.A. Documentation of the 5 as for smoking cessation by PCPs across distinct health systems. Am. J. Manag. Care. 2014;20:e35–e42. [PMC free article] [PubMed] [Google Scholar]
- Wolter K.M. Springer Science and Business Media; 2007. Introduction to Variance Estimation. [Google Scholar]
- Zbikowski S.M., Jack L.M., McClure J.B. Utilization of services in a randomized trial testing phone-and web-based interventions for smoking cessation. Nicotine Tob. Res. 2011;13:319–327. doi: 10.1093/ntr/ntq257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Chaiton M.O., Diemert L.M., Bondy S.J., Brown K.S., Ferrence R. Health professional advice, use of medications and smoking cessation: a population-based prospective cohort study. Prev. Med. 2016;91:117–122. doi: 10.1016/j.ypmed.2016.07.027. [DOI] [PubMed] [Google Scholar]
- Zhu S.-H., Tedeschi G.J., Anderson C.M., Pierce J.P. Telephone counseling for smoking cessation: What's in a call? J. Couns. Dev. 1996;75:93–102. [Google Scholar]
- Zhu S.-H., Anderson C.M., Johnson C.E., Tedeschi G., Roeseler A. A centralised telephone service for tobacco cessation: the California experience. Tob. Control. 2000;9:ii48–ii55. doi: 10.1136/tc.9.suppl_2.ii48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S.-H., Anderson C.M., Tedeschi G.J. Evidence of real-world effectiveness of a telephone quitline for smokers. N. Engl. J. Med. 2002;347:1087–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- Zhu S.-H., Gardiner P., Cummins S. Quitline utilization rates of African-American and white smokers: the California experience. Am. J. Health Promot. 2011;25:S51–S58. doi: 10.4278/ajhp.100611-QUAN-185. [DOI] [PubMed] [Google Scholar]
- Zinser M.C., Pampel F.C., Flores E. Distinct beliefs, attitudes, and experiences of Latino smokers: relevance for cessation interventions. Am. J. Health Promot. 2011;25:eS1–eS15. doi: 10.4278/ajhp.100616-QUAN-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwar N.A., Mendelsohn C.P., Richmond R.L. Supporting smoking cessation. Br. Med. J. 2014;348:29–33. doi: 10.1136/bmj.f7535. [DOI] [PubMed] [Google Scholar]