Highlights
-
•
This case is a rare presentation of C. sordellii toxic shock syndrome resulting from a Caesarian section.
-
•
This is the only obstetric case of C. sordellii to have survived.
-
•
Extreme levels of a leukocytosis and hypotension without fevers raises suspiscion for this severe infection.
-
•
Broad spectrum antibiotics, including coverage for anaerobic organisms, and surgical intervention is the standard of care.
-
•
At the moment, no early detection or antitoxins are commercially available.
Keywords: Clostridium sordellii, Toxic shock syndrome, Post-partum, Post-abortion, Leukemoid reaction
Abstract
Introduction
Clostridial toxic shock is a rare syndrome traditionally described in case studies and reviews as a uniformly fatal condition associated with post-partum and post-abortion. Clostridium sordellii was first mentioned in scientific literature as a human pathogen in 1922 when Argentinian microbiologist Alfredo Sordellii identified the organism in gangrenous wounds. Over the past century, there has been infrequent discussion and little awareness surrounding this serious condition. Information about patients who survived C. sordellii toxic shock is essentially nonexistent.
Presentation of case
A 31-year old post-partum female who underwent caesarian section 17 days prior, presented with abdominal pain and septic features. She underwent six operations/procedures over the next 17 days and was hospitalized for 25 days before discharge to her home with a successful outcome.
Discussion
This case provides insight on the process of identifying and managing complications associated with clostridial toxic shock syndrome. Out of now, 16 reported cases of C sordellii gynecologic infections in the world literature, our patient is the second patient to survive infection by this organism. More research is needed to provide clinicians with evidence-based approaches for managing these unique cases.
Conclusion
We present a case report of a rare toxic shock syndrome in a post-partum female caused by Clostridium sordellii. Her survival is notable among 16 patients with whom this infection now has a documented 87.5% mortality rate. Aggressive surgical measures and optimized intensive care management may have contributed to this patient’s survival.
1. Introduction
Clostridium sordellii is a gram positive, anaerobic, spore-forming bacillus found ubiquitously in soil that presents as a rare yet serious pathogenic potential in humans. Case reports have identified C sordellii as the culprit in bacteremia, necrotizing soft tissue infections, orthopedic tissue graft infections, and female upper reproductive tract infections since its 1922 debut in medical literature on gangrenous wounds [1]. Case reviews have demonstrated that postpartum and post-abortion women are a group susceptible to C sordellii infections [[2], [3], [4], [5], [6], [7], [8]]. As many as 18% of healthy women are colonized with a clostridia species but only about 3% are C. Sordellii, as a component of their normal vaginal flora, believed to be introduced by way of recto-vaginal transmission [8,9]. The organism gained attention in 2005 when the US Food and Drug Administration investigated its association with mifepristone-induced abortions after five California women died, but authorities were unable to demonstrate an epidemiologic linkage [10]. A recent 2016 case report commented that up to 10% of healthy women harbor C. sordellii in their vagina, and while most strains are nonpathogenic, those that are virulent can cause fatal infections through toxin-induced septic shock rapidly followed by end-organ failure; identification of C. sordellii has occurred by cultures, mass spectrometry, and other molecular methods. Due to the danger of this syndrome, they argue for the necessity of rapid C sordellii testing for women [11]. A large multicenter trial by Chong et al., on over 4000 women revealed only about 3% colonized with C. sordellii and in this group of 238 patients, only 2 had the lethal toxin. This group concluded that it would be inadvisable and ineffective to use any screening or prophylactic approach to try to prevent [18].
Basic science research has revealed two highly virulent C. sordellii toxins that mediate a systemic inflammatory response: lethal toxin (TcsL) and hemorrhagic toxin (TcsH). The lethal toxin triggers apoptotic mechanisms by exerting its effects on GTPases involved in mitochondrial function, cytoskeletal integrity, and cell cycle checkpoints [12]. Sequelae from these molecular alterations are devastating to endothelial cells, contribute to vascular compromise, and ultimately lead to systemic hemodynamic instability. The host response by uterine macrophage involves secretion of interleukin-10 (IL-10), an anti-inflammatory cytokine that may mask the development of infection and account for the fact that many patients are afebrile [13].
Patients generally present with signs of clinical sepsis and rapidly deteriorate to an almost invariably fatal toxic shock syndrome. The C. sordellii toxic shock syndrome inconsistently manifests as a triad of tachycardia, hypotension, and lack of fever [2]. The afebrile nature of this syndrome can be used in some cases to suggest clostridium as the etiology for toxic shock classically associated with severe staphylococcal and group A streptococcal infections. Laboratory results in clostridial shock typically show a remarkably high leukemoid reaction with white blood cell counts as high as 200,000 cells/μl in some cases.
Workup with aerobic and anaerobic cultures and gram stain of gynecological tissue may narrow the differential diagnoses and allow for targeted treatment. As obligate anaerobes, clostridia are fastidious organisms and often difficult to grow and isolate in culture. Definitive diagnosis of C. sordellii is dependent on immune-histochemical (IHC) staining and molecular methods such as polymerase chain reaction (PCR) because other species of clostridia like C. perfringens can inhabit the upper female reproductive tract and mount a concurrent infection. This case has been reported in line with the SCARE criteria [14].
2. Presentation of case
We present a case of a 31-year-old healthy female with no significant past medical history and a past surgical history of a previous cesarean section at term, two years prior. She had an uneventful second cesarean section at term and presented 17 days delivery. Her presenting complaints were; three days of suprapubic abdominal and bilateral flank pain accompanied by dysuria, nausea, vomiting, and diarrhea. She was afebrile but noted subjective rigors and chills. Her caesarian surgical incision was well healed and without evidence of cellulitis or infection. Her presenting vital signs were significant for hypotension. Initial laboratory results revealed a leukocytosis of 23,000 white blood cells/μl with a left shift. She had an elevated serum lactate of 4.1 mmol/liter. She was given intravenous fluid volume resuscitation and empiric broad spectrum intravenous antibiotic therapy in the emergency department and admitted to the Intensive Care Unit (ICU).
The admitting diagnosis was sepsis without an established source. The obstetrics & gynecology and general surgery team provided consultation. Unremarkable urologic and radiologic examinations as well as a clean urinalysis made urosepsis unlikely. Gynecologic and intra-abdominal origin were considered in the etiology.
Postpartum sepsis was entertained and she was taken to the operating room. A gynecologic surgeon performed a suction dilation & curettage (D&C) while a general surgeon laparoscopically examined the intra-abdominal viscera for a potential source, with no clear etiologic findings.
Despite the D&C, a procedure that should have identified and alleviated most uterine infectious sources, her white blood cell count rose to 42,000 cells/μl overnight and her septic shock worsened. Her white blood cell count tripled that day to become a leukemoid reaction of 112,000 cells/μl. She also developed disseminated intravascular coagulation (DIC). Potential infection with Clostridium species including sordellii was considered in the differential.
With rapid clinical deterioration, obstetrics & gynecology and general surgery took the patient back to the operating room on admission day two for another visual inspection and performed a supra-cervical hysterectomy with bilateral salpingectomy. Her abdomen was left open because of development of abdominal compartment syndrome. Clinically the specimen revealed a grossly enlarged, engorged and discolored uterus while the initial pathologic review showed acute and chronic endo-myometritis with necrotic features along with acute salpingitis. The omental fat that was adherent to the uterus and was resected with it en-bloc showed gross necrosis and hemorrhage. Necrotic gynecologic tissue established the puerperal septic source and raised the index of suspicion for C. sordellii infection. Pathology performed microscopic examination of the tissue but did not reveal microorganisms. Specimens from this operation as well as from the previous D&C were sent to the United States Centers for Disease Control and Prevention (CDC) for further investigation. She was given intravenous immunoglobulin (IVIg) was given for a course of three days. A small European study suggested that patients that receive IVIg as adjunctive therapy in toxic shock syndromes have a decrease in the sepsis-related organ failure, although there was no statistical difference in mortality compared to patients that received placebo [15].
On hospital day five with her condition improving, general surgery took her to the operating room for exploratory laparotomy with abdominal washout and application of a vacuum-assisted closure (VAC) device to the wound. She was returned to the operating room on admission day seven for another abdominal washout, application of a Wittmann temporary abdominal fascia Velcro prosthetic patch (Starsurgical, Burlington, WI) and wound VAC. Five days later on admission day 12, she underwent another exploratory laparotomy with abdominal washout and tightening of the Wittmann abdominal fascia patch and placement of a wound VAC. On admission day 14, she underwent her fifth abdominal washout, this time with closure of the abdominal fascia.
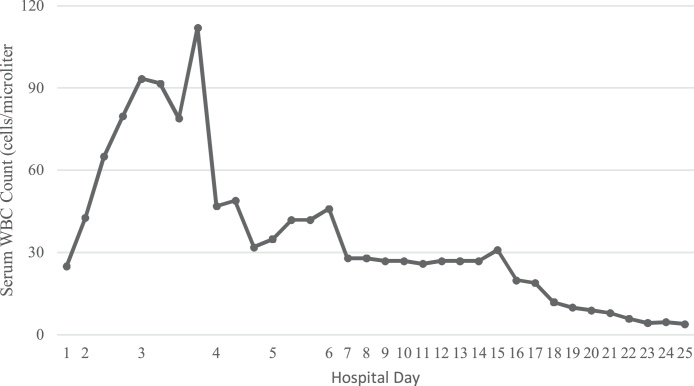
White blood cell counts remained above 40,000 until admission day six. Over the next thirteen days in the ICU, her white blood cell count slowly normalized with a prolonged intravenous antibiotics course (Fig. 1). After 17 days of treatment in the ICU, she was transitioned to the surgical floor; she stayed in the hospital for another week until her discharge on admission day 25. She was successfully discharged with a walker for ambulation and arrangements for physical therapy home visits because she was de-conditioned. Follow up in the clinic; she was doing well a month out.
Fig. 1.
Graph showing patient’s white blood cell count from admission to discharge.
3. Discussion
With numerous interventions, this remarkable case had a positive outcome. Our patient is the second person to survive a C. sordellii gynecological infection out of 30 reported cases in the world medical literature. She underwent a supra-cervical hysterectomy with bilateral salpingectomy, laparoscopic abdominal washout, three exploratory laparotomies with abdominal washout, and a fascial closure procedure for a total of six operations. Massive fluid resuscitation was utilized to treat severe septic shock. The surgical critical care team managed her critical condition for 17 days in the ICU and infectious disease orchestrated a course of broad-spectrum intravenous antibiotic and immunoglobulin therapy.
Our case is the only case where C. sordellii infection happened post-partum via Caesarean section. Most commonly, they occur after childbirth, or more recently, with medically induced abortions due to the theory that this bacterium colonizes the vagina, and the opening of the cervix during labor or abortion permits the retrograde transmigration of vaginal pathogens into the uterine cavity. Nearly all case reports of patients infected with C. sordellii were not as fortunate in their outcomes as ours. There are case reports of C. sordellii infections associated with childbirth (9 including ours), medically induced abortion (5), and spontaneous abortion (2) and non-gynecologic (14). The case-mortality rate in the gynecologic groups is a devastating 87.5% and our report is the first survivor after childbirth. Aldape et al. reported two cases where the patients received prompt broad-spectrum anti-biotic therapy and surgical intervention by means of debridement of necrotic tissue; despite this, in both cases, the patient died [16].
A grave issue and difficult challenge facing clinicians fighting against C. sordellii toxic shock syndrome is that the decline from the moment of diagnosis (if it is even identified early) to the time of death of the patient is astonishingly fast. Another case report by Sinave et al. illustrates just how deadly this infection can be. They describe their experience of a young woman who developed C. sordellii toxic shock syndrome, and despite aggressive antibiotic and critical supportive therapies, the patient expired in under three days after admission [17]. In this case, no surgical interventions were undertaken and the management was purely medical.
Patients in similar case reports did not necessarily undergo hysterectomy. The implications of these operations are life altering and it is a very difficult decision but the near uniformity death rate may require this treatment. Studies indicate that clostridial species that cause severe infections in obstetrics and gynecology warrant aggressive medical and surgical intervention, given their aggressive ability to progress into disseminating sepsis, toxic shock syndrome, and necrotizing tissue infections. Given that C. sordellii is the source of one of the most fatal toxic shock syndromes (resulting from its two major virulence factors called lethal toxin and hemorrhagic toxin), early detection, antibiotics, and surgery is the cornerstone of treatment [19]. The intraoperative decision for hysterectomy in our patient brought into consideration her rapidly deteriorating condition with a suspected gynecologic source for severe septic shock. While the consequences of hysterectomy are drastic, this early operative intervention is what allowed her to survive. This approach may limit the progression of clostridial toxic shock and allow for survivors.
Throughout her hospitalization, working diagnoses included toxic shock syndrome, endometritis, and sepsis secondary to C. sordellii. Tissue samples sent to the CDC underwent examination with light microscopy, immunohistochemical staining, and confirmatory PCR testing. Results from the CDC returned but took nearly three weeks after successful discharge of our patient. Microscopic examination of uterine tissue showed extensive endometrial necrosis, hemorrhage, fibrin deposition, neutrophilic infiltration with edematous changes, and focal granulation tissue. Lymphoplasmacytic infiltrate extended into the myometrium and many thrombosed vessels were visualized throughout the sample. Uterine contents were positive for C. sordellii on IHC staining and validated with PCR.
4. Conclusion
We present a case of report of a rare toxic shock syndrome in a postpartum woman caused by Clostridium sordellii. It is the only reported case of a postpartum female to survive a C. sordellii infection. This was achieved via aggressive medical and surgical intervention. Septic shock with leukemoid reaction, and disseminated intravascular coagulation, complicated her critical care course. She received six operations by obstetrics & gynecology and general surgery. Her survival is notable among the now 16 other postpartum and post-abortion women with whom this infection now has a documented 87.5% mortality rate. In our patient, optimized ICU management and surgical measures with early hysterectomy and management of abdominal compartment syndrome with numerous exploratory laparotomies with abdominal washout procedures may have contributed to her survival. In the future fight against this devastating infection, early hysterectomy may be lifesaving.
Conflict of interest
Authors declare no competing interests.
Funding
None.
Ethical approval
This report was conducted in compliance with ethical standards.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Adel Elkbuli, Dessy Boneva, Mark McKenney – Conception of study, acquisition of data, analysis and interpretation of data, drafting and revision of the article.
Dessy Boneva, Mark McKenney, Shaikh Hai – Management of case, revision of article, final approval of the version to be submitted.
Brandon Diaz, Adel Elkbuli, Dessy Boneva, Shaikh Hai, Sean Kuffman, John D. Ehrhardt Jr– Acquisition of data, Analysis of data, drafting and revision of article.
Adel Elkbuli, Dessy Boneva, Sean Kuffman, Shaikh Hai, Brandon Diaz, Mark McKenney – Analysis of data, revision of article.
Registration of research studies
This is a case report study.
Guarantor
Dessy Boneva.
Mark McKenney.
Shaikh Hai.
References
- 1.Sordellii A. Un anaerobic agent de gangrene gazeuse. C. R. Soc. Biol. 1922;87:838–840. [Google Scholar]
- 2.Zane S., Guarner J. Gynecologic clostridial toxic shock in women of reproductive age. Curr. Infect. Dis. Rep. 2011;13(December (6)):561–570. doi: 10.1007/s11908-011-0207-7. [DOI] [PubMed] [Google Scholar]
- 3.Sinave C., Le Templier G., Blouin D. Toxic shock syndrome due to Clostridium sordellii: a dramatic postpartum and postabortion disease. Clin. Infect. Dis. 2002;35(11):1441–1443. doi: 10.1086/344464. [DOI] [PubMed] [Google Scholar]
- 4.Cohen A.L., Bhatnagar J., Reagan S. Toxic shock associated with Clostridium sordellii and Clostridium perfringens after medical and spontaneous abortion. Obstet. Gynecol. 2007;110:1027–1033. doi: 10.1097/01.AOG.0000287291.19230.ba. [DOI] [PubMed] [Google Scholar]
- 5.Rørbye C., Petersen I.S., Nilas L. Postpartum Clostridium sordellii infection associated with fatal toxic shock syndrome. Acta Obstet. Gynecol. Scand. 2000;79(12):1134–1135. [PubMed] [Google Scholar]
- 6.McGregor J.A., Soper D.E., Lovell G., Todd J.K. Maternal deaths associated with Clostridium sordellii infection. Am. J. Obstet. Gynecol. 1989;161(4):987–995. doi: 10.1016/0002-9378(89)90768-0. [DOI] [PubMed] [Google Scholar]
- 7.Bitti A., Mastrantonio P., Spigaglia P. A fatal postpartum Clostridium sordellii associated toxic shock syndrome. J. Clin. Pathol. 1997;50(3):259–260. doi: 10.1136/jcp.50.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fischer M., Bhatnagar J., Guarner J. Fatal toxic shock syndrome associated with Clostridium sordellii after medical abortion. N. Engl. J. Med. 2005;353:2352–2360. doi: 10.1056/NEJMoa051620. [DOI] [PubMed] [Google Scholar]
- 9.Gorbach S.L., Menda K.B., Thadepalli H., Keith L. Anaerobic microflora of the cervix in healthy women. Am. J. Obstet. Gynecol. 1973;117(8):1053–1055. doi: 10.1016/0002-9378(73)90753-9. [DOI] [PubMed] [Google Scholar]
- 10.Ho C.S., Bhatnagar J., Cohen A.L. Undiagnosed cases of fatal Clostridium-associated toxic shock in Californian women of childbearing age. Am. J. Obstet. Gynecol. 2009;201(459):e1–7. doi: 10.1016/j.ajog.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Guzzetta M., Williamson A., Doung S. Clostridium sordellii as an uncommon cause of fatal toxic shock syndrome in a postpartum 33-year-old Asian woman, and the need for antepartum screening for this Clostridia species in the general female population. Lab. Med. 2016;47(3):251–255. doi: 10.1093/labmed/lmw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hao Y., Senn T., Opp J. Lethal toxin is a critical determinant of rapid mortality in rodent models of Clostridium sordellii endometritis. Anaerobe. 2010;16(April (6)):155–160. doi: 10.1016/j.anaerobe.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aldape M.J., Bryant A.E., Katahira E.J. Innate immune recognition of, and response to, Clostridium sordellii. Anaerobe. 2010;16:125–130. doi: 10.1016/j.anaerobe.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Darenberg J., Ihendyane N., Sjölin J. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: a European randomized, double-blind, placebo-controlled trial. Clin. Infect. Dis. 2003;37(January (3)):333–340. doi: 10.1086/376630. [DOI] [PubMed] [Google Scholar]
- 16.Aldape M.J., Bryant A.E., Stevens D.L. Clostridium sordellii infection: epidemiology, clinical findings, and current perspectives on diagnosis and treatment. Clin. Infect. Dis. 2006;43(January (11)):1436–1446. doi: 10.1086/508866. [DOI] [PubMed] [Google Scholar]
- 17.Sinave C., Le Templier G., Blouin D. Toxic shock syndrome due to Clostridium sordellii: a dramatic postpartum and postabortion disease. Clin. Infect. Dis. 2002;35(11):1441–1443. doi: 10.1086/344464. [DOI] [PubMed] [Google Scholar]
- 18.Chong E., Winikoff B., Charles D. Vaginal and rectal Clostridium sordellii and Clostridium perfringens presence among women in the United States. Obstet. Gynecol. 2016;127(February (2)):360–368. doi: 10.1097/AOG.0000000000001239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beryl Manning-Geist, Rimawi Bassam H. Severe infections in obstetrics and gynecology: how early surgical intervention saves lives. J. Clin. Gynecol. Obstet. 2016;5(1):1–16. [Google Scholar]