Highlights
-
•
This case report reviews complicated appendicitis that failed non-operative management, underwent appendectomy, and did well post-operatively.
-
•
In the present case, the patient’s clinical picture was substantially worse on presentation four weeks post-diagnosis when compared to his prior hospitalizations, indicating failed non-operative treatment.
-
•
This case report provides an opportunity to review the management of complicated perforated appendicitis.
-
•
This case report could help to increase the awareness of medical professionals who manage similar cases and outline best treatment options such as early surgical intervention.
Abbreviations: RLQ, right lower quadrant; CT, computed tomography
Keywords: Acute appendicitis, Perforated complicated appendicitis, Conservative management, Acute appendectomy, Appendiceal abscess, Fistula
Abstract
Introduction
There is no clear standardized approach to complicated appendicitis associated with abscess or phlegmon, with treatment varying from immediate appendectomy versus non-operative management with antibiotics and possible interval appendectomy. This case report reviews a presentation of complicated appendicitis failing non-operative therapy and reviews the literature on complicated appendicitis.
Presentation of Case
: A 19 year-old male presented with right lower quadrant pain, leukocytosis, and fever. He had been seen at an outside hospital, diagnosed with complicated appendicitis, treated non-operatively, and discharged on antibiotics. CT confirmed persistent complicated appendicitis; he was again treated non-operatively with resolution of symptoms. He was discharged but returned with recurrent pain/leukocytosis. The patient was determined to have failed non-operative management, underwent laparoscopic appendectomy. Post-operatively he improved was doing well in follow up.
Discussion
Historically, the therapy for acute appendicitis has been surgical. However, immediate surgical management of complicated appendicitis is often associated with increased complications. Non-operative management with antibiotics and interval appendectomy in cases of complicated appendicitis is an option. Literature shows that non-operative management of complicated appendicitis is not entirely innocuous. Non-operative management carries a significant failure rate. Patients that undergo immediate appendectomy may have a better health-related quality of life. Non-operative management of complicated appendicitis may lead to worse outcomes and higher healthcare costs.
Conclusion
Non-operative management of complicated appendicitis has significant failure rates, increased healthcare costs, and perhaps increased morbidity when compared to immediate surgical management. Immediate surgical management of complicated appendicitis remains the gold standard and should be used in most patients.
1. Introduction
Appendicitis is one of the most common surgical diagnoses for young patients presenting to the emergency department (ED) with acute abdominal pain, with an overall prevalence of approximately 7% [1]. The lifetime risk is slightly higher in males than in females, although the risk of surgical intervention in males is approximately half that of female patients [1]. The classical presentation begins with periumbilical pain followed by anorexia, nausea, vomiting, right lower quadrant (RLQ) pain with or without fever, and usually leukocytosis; however, these findings are not specific to the diagnosis, and occur in patients with other etiologies for their abdominal pain.
Appendicitis may be complicated by perforation, appendiceal phlegmon or abscess formation. While the traditional treatment for acute appendicitis has been emergent appendectomy, non-operative management in complicated appendicitis with antibiotics and interval appendectomy is an alternative to immediate surgical management [[2], [3], [4], [5]]. The timing of interval surgical removal of the appendix in cases of complicated appendicitis has not been standardized, and there is still debate over the need of interval appendectomy if the initial non-operative approach is chosen. We present a case of complicated appendicitis that failed non-operative therapy. In addition, we review the literature on treatment of complicated appendicitis. This case has been reported in line with the SCARE criteria [6].
2. Case presentation
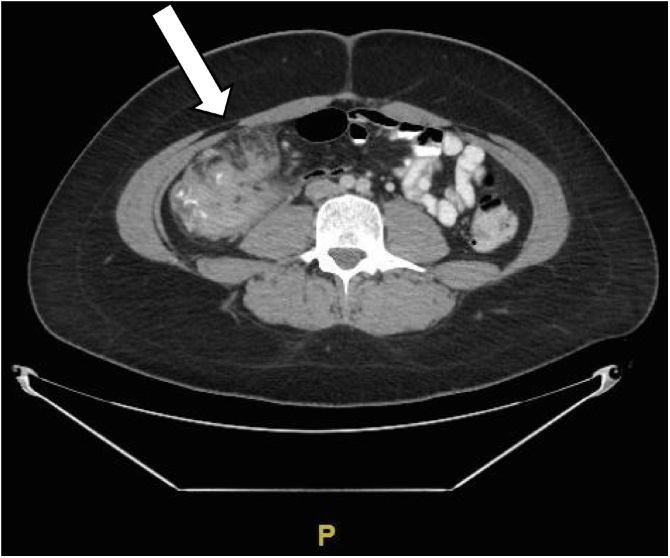
A 19-year-old male presented to the emergency department with a one-day history of worsening RLQ pain. It was associated with fever, chills, nausea and anorexia. He had been seen 10 days prior at an outside hospital with similar presenting symptoms, and a computed tomography (CT) scan at that time showed an acute perforated appendicitis. The patient was treated with intravenous metronidazole and levofloxacin for three days and discharged home with oral antibiotics. His pain returned and then progressed following discharge and was no longer controllable with home pain medications. His second ED visit was to our hospital. Physical examination demonstrated tenderness to light palpation in the RLQ with positive Rovsing’s sign but no generalized peritonitis. White blood cell count was elevated. The patient underwent a CT scan, which revealed a dilated appendix with severe inflammatory stranding centered around the ileocecal valve, inflammatory changes involving the terminal ileum and intraluminal narrowing (Fig. 1). He was also found to have inflammation consistent with phlegmon (abscess in evolution) formation with no drainable discrete collection or abscess.
Fig. 1.
CT abdomen and pelvis with IV and PO contrast. The patient was found to have a large amount of inflammation in the right lower quadrant with phlegmon, as well as marked inflammatory changes including the colon, appendix and terminal ileum.
Given the patient’s delayed presentation, non-septic clinical picture as well as radiographic findings showing significant phlegmon formation and inflammation not easily amenable to surgery, non-operative management was recommended and intravenous piperacillin/tazobactam was initiated. The patient had resolution of fever and leukocytosis during his admission. Repeat CT scan of the abdomen and pelvis with intravenous and oral contrast was ordered prior to discharge, and showed improvement in inflammation with no drainable fluid collection. The patient was discharged home with oral antibiotics after a four-day hospital stay.
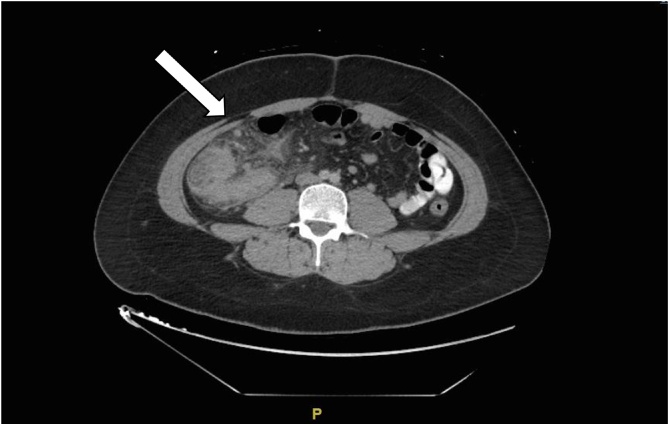
At 20 days post-discharge the patient again returned to the emergency department with worsening peri-umbilical abdominal pain with radiation to the RLQ, associated with nausea and diarrhea. CT scan of the abdomen and pelvis with intravenous and oral contrast was again performed, showing diffuse inflammation and an abnormal cecal region with worsening peri-appendiceal phlegmon, significant RLQ mesenteric lymphadenopathy and adjacent free fluid (Fig. 2, Fig. 3). There was also small foci of free air. The patient was determined to have failed non-operative treatment at that time.
Fig. 2.
CT Scan on readmission 20 days after second encounter, repeat imaging demonstrated mass-like phlegmon and appendiceal thickening with surrounding inflammatory change and prominent adjacent lymph nodes.
Fig. 3.
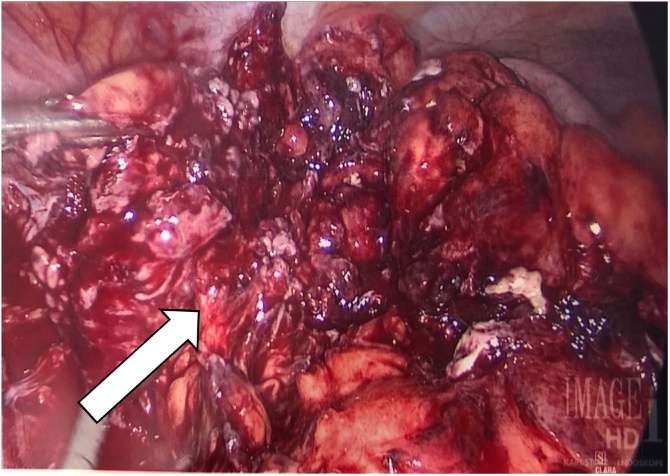
CT scan 20 days after second encounter. A large amount of inflammation of the appendix, colon and cecum is seen with phlegmon (arrow) and foci of free intraperitoneal air.
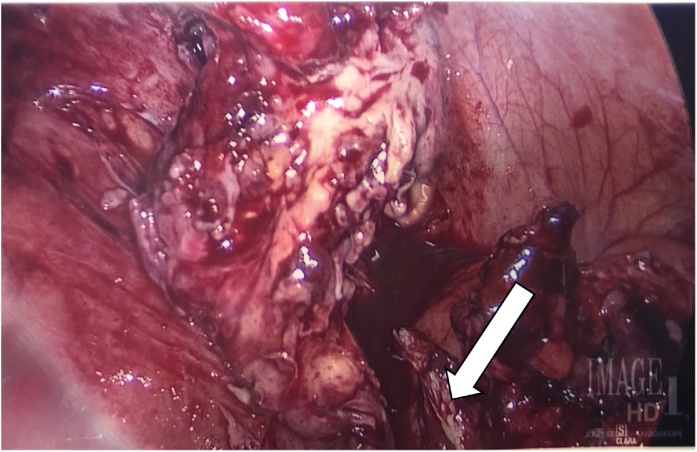
At surgery, a perforated, necrotic appendix was encountered with a large phlegmon and extensive adhesions involving the colon, the small bowel, and the abdominal wall (Fig. 4). Extensive lysis of adhesions was undertaken, and the appendix was found to be perforated near the base. The remnant appendiceal tissue and surrounding phlegmon were highly friable, and the specimen was effectively morcellated and removed piecemeal. A perforation of the cecum near the site of appendiceal perforation was also found, and primary closure was achieved (Fig. 5). A closed drain was placed. The patient had an unremarkable post-operative course, and on post-operative day two, he was discharged home. The drain was removed on post-operative day 14 in the office, and no post-operative complications were noted.
Fig. 4.
Large amount of inflammatory changes in the right lower quadrant centered around the terminal ileum, cecum (colon) and the appendix. Prominent mass-like phlegmon noted in this area with diffusely abnormal cecal region.
Fig. 5.
Mass-like thickening of the appendix and piecemeal removal of the inflamed mass/appendix laparoscopically. The inflamed mass-like appendix is seen to be a part of a larger phlegmon in this area. On the bottom right lower side of the photo the remaining inflamed colon is seen where perforation of the colon was found and repaired with the stapler laparoscopically.
3. Discussion
Appendicitis is one of the most common surgical emergencies in the world, and one of the most frequent causes for acute abdominal pain leading to presentation to the ED [1]. Obstruction of the appendiceal lumen leads to increasing intraluminal pressures and can be caused by fecalith, foreign body, lymphoid hyperplasia or malignancy. As intraluminal pressure rises it eventually surpasses that of the appendiceal veins, leading to outflow obstruction, venous congestion, loss of epithelial integrity and bacterial invasion of the appendiceal wall. With continued obstruction, intraluminal pressures may eventually surpass that of its arterial supply, leading to appendiceal ischemia and necrosis with possible perforation and gangrene of the appendix. Diagnosis of appendicitis requires a combination of consistent history, physical examination and laboratory studies, with increasing use of focused imaging for diagnostic confirmation.
Historically, the mainstay of therapy for acute appendicitis has been surgical, with a shift from open to laparoscopic appendectomy as the gold standard of treatment since early 1990s. Not surprisingly, surgical management of cases of complicated appendicitis have been associated with significantly increased complication rates compared to uncomplicated cases [[7], [8], [9], [10]]. The initial challenge is distinguishing uncomplicated from complicated appendicitis preoperatively. Studies show that neither clinical findings nor laboratory markers are reliable enough to estimate the severity of the acute appendicitis, therefore the role of CT in identifying complicated and uncomplicated acute appendicitis is of pivotal importance. Temporal progression can be suggestive, as a larger percentage of cases of complicated acute appendicitis had symptoms for more than 24 h when compared to cases of uncomplicated acute appendicitis (81% and 38%, respectively) [12]. Atema et al demonstrated that utilizing a scoring system that combines clinical features (age, temperature, duration of symptoms, white blood cell count, C-reactive protein levels, and presence of extraluminal free air, periappendiceal fluid and appendicolith) and imaging yielded 95% certainty when identifying uncomplicated appendicitis preoperatively. Two separate models and scoring systems were created – one based on CT and clinical features, and one on ultrasound and clinical features. The CT model was based on a maximum score of 22 points; of the 284 patients, 150 had a score of 6 points or less, of whom eight (5.3%) had complicated appendicitis, yielding a negative predictive value (NPV) of 94.7%. The ultrasound model included all the same factors except for extraluminal free air, resulting in a maximum score of 19 instead of 22 points; the ultrasound score was calculated for 312 patients, 105 of which had a score of 5 or less, of whom three (2.9%) had complicated appendicitis, yielding an NPV of 97.1% [16]. The factors for these models are illustrated in Table 1, Table 2 below. Being able to accurately differentiate uncomplicated appendicitis from complicated appendicitis is key in guiding surgical management, and can be accomplished with sensitive clinical findings and imaging.
Table 1.
Model and scoring system combining CT and clinical features amounting to a maximum score of 22 [21].
| Points | |
|---|---|
| Clinical features | |
| Age ≥45 years | 2 |
| Body temperature (°C) ≤37.0 37.1–37.9 ≥38.0 |
1 2 3 |
| Duration of symptoms ≥48 h | 2 |
| WBC count >13 × 109/l | 3 |
| CRP (mg/l) ≤50 51–100 >100 |
1 2 3 |
| CT features | |
| Free extraluminal air | 3 |
| Periappendiceal fluid | 3 |
| Presence of appendicolith | 3 |
Table 2.
Model and scoring system combining ultrasound and clinical features amounting to a maximum score of 19 [21].
| Points | |
|---|---|
| Clinical features | |
| Age ≥45 years | 2 |
| Body temperature (°C) ≤37.0 37.1–37.9 ≥38.0 |
1 2 3 |
| Duration of symptoms ≥48 h | 2 |
| WBC count >13 × 109/l | 3 |
| C-reactive protein (mg/l) ≤50 51–100 >100 |
1 2 3 |
| Ultrasound features | |
| Periappendiceal fluid | 3 |
| Presence of appendicolith | 3 |
Recent efforts to address the risks associated with surgical therapy of complicated appendicitis have included the introduction of non-operative management with intravenous antibiotics and interval appendectomy once inflammation has subsided to perform the operation safely. Cases of appendicitis complicated with phlegmon and abscess account for 2–10% of all appendicitis cases. Evidence suggests a role for non-operative management in cases of appendicitis complicated by phlegmon or abscess [[3], [4], [5],13]. Typically, after successful non-operative management of an appendiceal mass, interval appendectomy is performed either semi-electively or electively. This non-operative approach is common but has been questioned by an increasing amount of evidence. A meta-analysis by Cheng et al reviewed two studies with forty patients each [20]. In one study, 40 adult and pediatric patients with phlegmon were randomized to either early appendectomy as soon as appendiceal mass resolved within the same admission (n = 20) or interval open appendectomy after 6 weeks (n = 20). In the second trial 40 pediatric patients with appendiceal abscess were randomized to either early emergent laparoscopic appendectomy (n = 20) or delayed interval laparoscopic appendectomy after 10 weeks (n = 20). The study concluded that the participants that underwent early appendectomy had better health-related quality of life (measured at 12 weeks after appendectomy via a quality of life questionnaire on a scale of 0–100 [mean difference 12.40 points] when compared to those that underwent delayed i.e. interval appendectomy [20]. A study by Young et al. alludes to early appendectomy being the appropriate management for complicated appendicitis (criteria described in Table 3) due to high failure rates of non-operative management and the morbidity associated with those failures; patients that failed non-operative management ended up requiring open appendectomies with 55.6% needing bowel resection, whereas early appendectomies demonstrated lower incidence of bowel resection when compared to patients who were initially treated non-operatively (3.3% vs 17.1%, respectively) [21]. This demonstrates that conservative, non-operative management of complicated appendicitis may actually lead to worse outcomes, higher healthcare costs and less patient satisfaction. Turhan et al reinforced that the mean hospital stay of patients with appendicitis who were treated non-operatively was significantly longer than those treated operatively [22]. Elective interval appendectomies are an option when considering non-operative management on initial presentation, but they also result in higher healthcare costs. Cases where non-operative management with interval appendectomy was used cost over $4000 more per patient than those treated with initial operative management [23]. Furthermore, as depicted in the large pediatric study of Bachur et al. 66% of 99,001 children with appendicitis were diagnosed with non-perforated appendicitis, 4190 (6%) of which underwent non-operative management (NOM) – these cases are part of an increasing number of NOM cases observed over 6 years. However, during the 12-month follow-up period, NOM patients were more likely to have: advanced and additional imaging (+8.9%), ED visits (+11%), and hospitalizations (+43.7%). Interestingly, among the patients that underwent NOM initially, a substantial portion (46%) eventually had an appendectomy [24]. Logically, all of the aforementioned outcomes contribute to increase in healthcare cost. However, the timing of interval appendectomy and the safety of in-hospital delay are still under debate, and there is no clear timeline in the literature as to when to perform interval appendectomy, with recommendations ranging from two to eight weeks following initial non-operative therapy.
Table 3.
Comparing Acute Appendicitis to Complicated Appendicitis [22].
| Acute Appendicitis | Complicated Appendicitis | |
|---|---|---|
| Perforation | No | Yes |
| Abscess | No | Yes |
| Phlegmon | No | Yes |
The use of antibiotics and planning an interval appendectomy in cases of complicated appendicitis seem to be successful in the majority of cases yet up to one-third of patients develop complications such as abscess formation and/or readmission prior to planned interval appendectomy contributed to certain clinical indicator [26]. Approximately, 25% of patients with appendiceal abscess fail non-operative management even with percutaneous drainage. However, mortality rate did not differ between both groups [26].
Another issue in utilizing non-operative management of complicated appendicitis is an increased rate of neoplasms, up to 16% in older patients undergoing delayed interval appendectomy [27]. Another study found an even higher incidence with 33% of older patients undergoing interval appendectomy having a neoplasm [27]. Furthermore, a study by Enblad et al noted an increase in short and long-term incidence of bowel cancer in patients with non-surgical treatment of appendicitis when compared to those with operative management. We recommend that in patients older than 35 years old who do not have an interval appendectomy a colonoscopy or CT colonography should be considered. This would also serve as a cancer-screening tool especially if the patient has a family history of intestinal cancers.
Future studies should further investigate the necessity for surgical interventions in patients with recurrent appendicitis. However good clinical sense dictates that all recurrent appendicitis be treated surgically so that tissue can be obtained for pathology to rule out malignancy or possible recurrent inflammatory bowel disease, which may require subsequent intervention.
In the present case, the patient’s clinical picture was substantially worse on presentation four weeks post-diagnosis when compared to his prior hospitalizations, indicating failed non-operative treatment. While technically challenging given the patient’s extensive intraperitoneal inflammation and significant adhesions, surgical management was successful without the need for conversion to open appendectomy.
4. Conclusions
We report a case of a patient with repeat hospitalizations due to recurrent complicated appendicitis. The patient failed non-operative management of complicated appendicitis and underwent a laparoscopic appendectomy, and did well post-operatively. This case provides an opportunity to review the management of complicated appendicitis. Non-operative management of complicated appendicitis has significant failure rates, increased healthcare costs, and perhaps increased morbidity when compared to immediate surgical management. Immediate surgical management of complicated appendicitis remains the gold standard of care and should be used in most patients.
Conflict of interest
Authors declare no competing interests.
Funding
None.
Ethical approval
This report was conducted in compliance with ethical standards. Patient consent was received.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Adel Elkbuli– Conception of study, acquisition of data, analysis and interpretation of data, drafting and revision of the article. Dessy Boneva – Management of case, revision of article, final approval of the version to be submitted Brandon Diaz– Acquisition of data, Analysis of data, drafting and revision of article.
Valerie Polcz: Analysis and interpretation of data, drafting of article. Mark McKenney – Analysis of data, revision of article.
Registration of research studies
This is a case report study.
Guarantor
Mark McKenney
Dessy Boneva
Adel Elkbuli.
References
- 1.Addiss D.G., Shaffer N., Fowler B.S., Tauxe R.V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 2.Wijayanayaka T., Davidson J., Bütter A. Does size matter? Correlation of ultrasound findings in children without clinical evidence of acute appendicitis. J. Pediatr. Surg. 2018;(February (9)) doi: 10.1016/j.jpedsurg.2018.02.025. pii: S0022-3468(18)30079-4, (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 3.Peter S.D., Aguayo P., Fraser J.D. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J. Pediatr. Surg. 2010;45(1):236–240. doi: 10.1016/j.jpedsurg.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 4.Smith C. Yearbook of Gastroenterology. 2010. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) pp. 200–202. 2010. [DOI] [PubMed] [Google Scholar]
- 5.Oliak D., Yamini D., Udani V.M., Lewis R.J., Vargas H., Arnell T., Stamos M.J. Nonoperative management of perforated appendicitis without periappendiceal mass. Am. J. Surg. 2000;179(3):177–181. doi: 10.1016/s0002-9610(00)00299-3. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Johnson A. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta-analysis. J. Emerg. Med. 2012;42(4):499. [Google Scholar]
- 8.Ricci M.A., Trevisani M.F., Beck W.C. Acute appendicitis: a 5-year review. Am. Surg. 1991;57:301–305. [PubMed] [Google Scholar]
- 9.Velanovich V., Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am. Surg. 1992;58:264–269. [PubMed] [Google Scholar]
- 10.Hale D.A., Molloy M., Pearl R.H. Appendectomy: a contemporary appraisal. Ann. Surg. 1997;225:252–261. doi: 10.1097/00000658-199703000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lietzén E. Is preoperative distinction between complicated and uncomplicated acute appendicitis feasible without imaging? Surgery. 2016;160(3):789–795. doi: 10.1016/j.surg.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Varadhan K.K., Neal K.R., Lobo D.N. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156. doi: 10.1136/bmj.e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atema J.J. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br. J. Surg. 2015;102(December (8)):979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]
- 20.Cheng Y., Xiong X., Lu J., Wu S., Zhou R., Cheng N. Early versus delayed appendicectomy for appendiceal phlegmon or abscess. Cochrane Database of Systematic Reviews. 2017;(6) doi: 10.1002/14651858.CD011670.pub2. Art. No.: CD011670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young K.A. outcomes of complicated appendicitis: is conservative management as smooth as it seems? Am. J. Surg. 2018;215(4):586–592. doi: 10.1016/j.amjsurg.2017.10.032. [DOI] [PubMed] [Google Scholar]
- 22.Turhan A.N. Comparison of operative and non operative management of acute appendicitis. Ulus. Travma Acil Cerrahi Derg. 2009;15(5):459–462. [PubMed] [Google Scholar]
- 23.Wu J.X. Cost effectiveness of nonoperative management versus laparoscopic appendectomy for acute uncomplicated appendicitis. Surgery. 2015;158(3):712–721. doi: 10.1016/j.surg.2015.06.021. [DOI] [PubMed] [Google Scholar]
- 24.Bachur R.G., Lipsett S.C., Monuteaux M.C. Outcomes of nonoperative management of uncomplicated appendicitis. Pediatrics. 2017;140(February (1)) doi: 10.1542/peds.2017-0048. [DOI] [PubMed] [Google Scholar]
- 26.Nazarey P.P., Stylianos S., Velis E. Treatment of suspected acute perforated appendicitis with antibiotics and interval appendectomy. J. Pediatr. Surg. 2014;49(March (3)):447–450. doi: 10.1016/j.jpedsurg.2013.10.001. Epub 2013 Oct 9. [DOI] [PubMed] [Google Scholar]
- 27.Wright G.P., Mater M.E., Carroll J.T. Is there truly an oncologic indication for interval appendectomy? Am. J. Surg. 2015;209(March (3)):442–446. doi: 10.1016/j.amjsurg.2014.09.020. Epub 2014 Dec 11. [DOI] [PubMed] [Google Scholar]