Abstract
Lung cancer is generally diagnosed through traditional bronchoscopy by pulmonologists, whereas data on the application of transesophageal endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for lung cancer diagnosis in China are very rarely reported. We herein describe a case of a 62-year-old woman who presented with non-productive cough and was found to have a pulmonary mass in the upper lobe of the right lung. The results of positron emission tomography revealed an elevated level of 18F-fluorodeoxyglucose accumulation (maximum standardized uptake value of 13.6) in the left adrenal gland. Thus, EUS-FNA was performed to identify the suspected metastasis to the left adrenal gland, and the histopathological examination of the bioptic specimen demonstrated an adenocarcinoma, confirming the value of EUS-FNA as a first-line minimally invasive approach for diagnosis and staging in patients with lung cancer.
Keywords: lung cancer, left adrenal gland, metastasis, ultrasound-guided fine-needle aspiration
Introduction
Endobronchial ultrasound (EBUS) bronchoscopy has been well described in the diagnosis of pulmonary diseases, particularly lung cancer, due to its usefulness in the evaluation of hilar and mediastinal lymph nodes as a diagnostic and staging method (1). Recently, EUS-FNA qualified as a surgical mediastinal staging procedure due to its safety and minimal invasiveness, and is recommended by international guidelines (2). To date, numerous publications have established the value of EUS-FNA in the assessment of mediastinal nodes, as well as the adrenal glands (3–6). Although accumulating evidence has confirmed the efficacy of EUS in the staging of mediastinal nodes, the application of EUS-FNA is not yet widely applied in the diagnosis of patients with lung cancer (7,8). We herein report a case of stage IV lung adenocarcinoma metastatic to the left adrenal gland, which was finally diagnosed by EUS-FNA biopsy. To the best of our knowledge, the present case may be the first to affirm the validity of the use of EUS-FNA as a first-line minimally invasive staging procedure for non-small-cell lung cancer (NSCLC) in China.
Case report
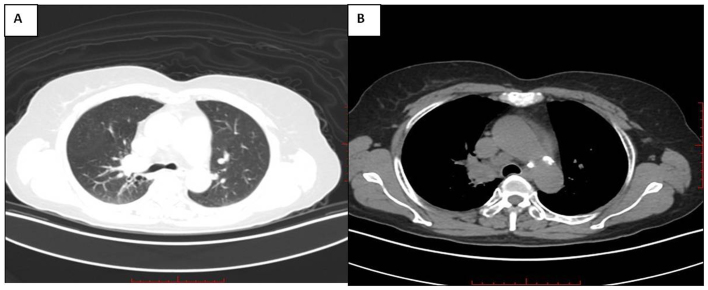
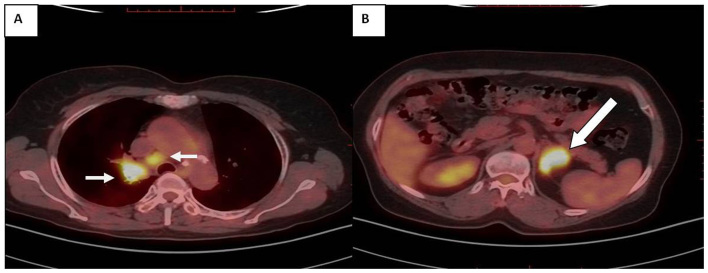
A 62-year-old Han Chinese woman was admitted to the Department of Respiratory Medicine, Shanghai East Hospital, Tongji University School of Medicine (Shanghai, China) in May 2017, with complaints of a non-productive cough persisting for 3 months and a history of passive smoking. No abnormalities were found on routine physical examination. The laboratory tests demonstrated that the serum carcinoembryonic antigen and carbohydrate antigen-125 levels were elevated to 156.7 ng/ml (normal range, 0–5.2 ng/ml) and 85.23 ng/ml (normal range, 0–35 ng/ml), respectively. A computed tomography (CT) scan of the chest revealed a hypodense soft mass (size, 2.3×2.2 cm) with the spicule sign in the right upper lobe; an enlarged paratracheal lymph node in the superior mediastinum (4R) was also identified (Fig. 1A and B). The patient was then scheduled to undergo a 18F-fluorodeoxyglucose positron emission tomography (18FDG-PET) scan and the results demonstrated abnormal 18FDG uptake by the pulmonary mass of the right upper lobe [maximum standardized uptake value (SUVmax) 13.5], the right paratracheal lymph node (4R) (SUVmax, 13.0) (Fig. 2A), as well as the left adrenal gland (SUVmax, 13.6) (Fig. 2B). Furthermore, irregular shape of the left adrenal gland, with dimensions 3.8×2.7 cm, was also observed (Fig. 2B). These findings strongly indicated that the pulmonary lesion was a malignant tumor. Moreover, the enlarged and 18FDG-PET-positive left adrenal gland was also highly likely to be a metastatic site. Routine bronchoscopy was initially performed to assess the airways, and it revealed an obstruction of the bronchus opening at the apical segment of the right upper lobe, without detection of any neoplasm (Fig. 3). Subsequently, EUS-FNA was suggested as a minimally invasive test for the confirmation of suspected metastasis to the left adrenal gland. EUS was conducted in a standardized manner at an endoscopy room under conscious sedation using propofol (9). The vessels surrounding the left adrenal were evaluated with color flow Doppler; then, the optimal lesion site (hypoechoic involvement in the left adrenal gland) was punctured using a 22-gauge needle, guided by real-time ultrasound imaging (Fig. 4). FNA was repeated until sufficient tissue samples were obtained. Subsequently, the samples were processed and stained for cytological analysis. Histopathological examination of the EUS-FNA samples demonstrated an adenocarcinoma. The results of immunohistochemical examination indicated metastatic adenocarcinoma from the primary lung cancer (Fig. 5). Consequently, our patient was treated with gefitinib due to the presence of epidermal growth factor receptor gene mutation. The physical status of the patient has currently been under control since the treatment with gefitinib for ~10 months.
Figure 1.
A chest computed tomography image showing (A) a 2.3×2.2-cm hypodense mass in the upper lobe of the right lung and (B) an enlarged paratracheal lymph node.
Figure 2.
An integrated PET-CT image showing accumulated 18FDG uptake (A) in a lung mass localizing in the right upper lobe and (B) an enlarged mediastinal lymph node (arrows). PET, positron emission tomography; CT, computed tomography; FDG, fluorodeoxyglucose.
Figure 3.

Bronchoscopic image showing an obstruction of the bronchus opening at the apical segment of the right upper lobe.
Figure 4.
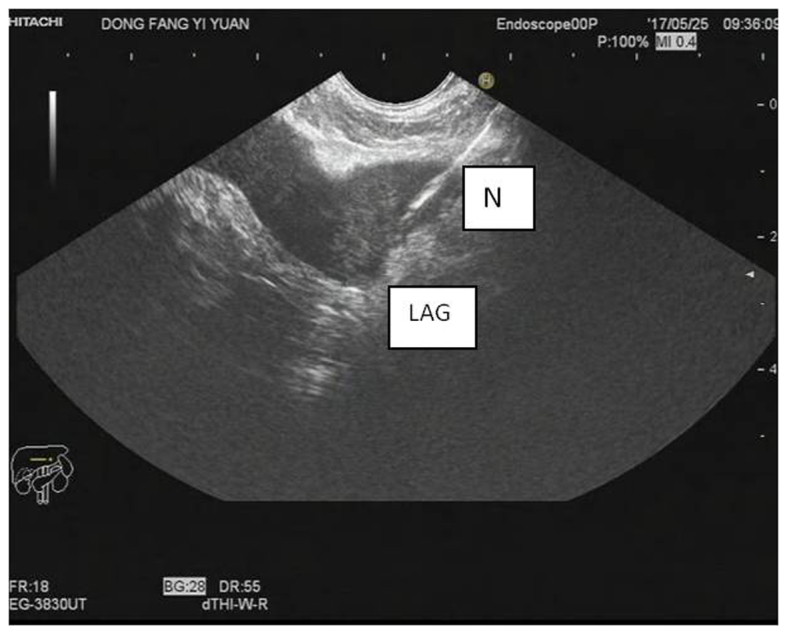
Application of EUS-FNA for the evaluation of an enlarged left adrenal. EUS, endoscopic ultrasound; FNA, fine-needle aspiration; LAG, left adrenal gland; N, needle.
Figure 5.
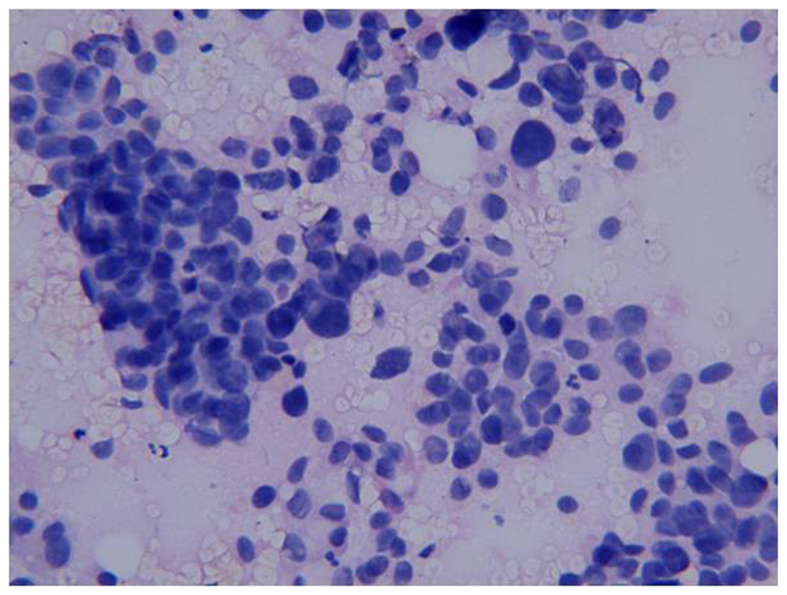
Cytological diagnosis of the adrenal tissue biopsied by EUS-FNA revealing adenocarcinoma cells (stained using the Giemsa method; magnification, ×40). EUS, endoscopic ultrasound; FNA, fine-needle aspiration.
Discussion
Lung cancer is the leading cause of cancer-related mortality worldwide (10). The majority of new cases of lung cancer (≤80%) are NSCLCs (11). Chest CT and integrated PET scans are widely available non-invasive methods for the assessment of suspected NSCLC; however, their efficacy is limited by their relatively low sensitivity (58 and 74%, respectively) and specificity (85% for both) (12). Bronchoscopy is usually required to diagnose or evaluate pulmonary lesions. In terms of minimally invasive techniques, EBUS has the best yield regarding hilar, intrapulmonary, anterior and superior mediastinal lymph nodes. Hence, EBUS is suitable for lymph nodes located in the anterosuperior mediastinum, as well as paratracheal regions (13). On the contrary, patients with enlarged posteroinferior mediastinal or subcarinal lymph nodes may benefit from EUS as a primary staging procedure. The selection of EUS or EBUS is mainly determined by the location of the lymph nodes (14). For mediastinal staging, these two invasive methods may complement each other. Furthermore, compared with EBUS, EUS may detect distant metastatic lesions to subdiaphragmatic organs, including the left adrenal gland and the liver, which adds another advantage with respect to metastatic lung cancer (15).
In the present case, routine bronchoscopy was initially performed, but no mass was detected in the trachea. Accordingly, transbronchial lung biopsy could not be performed. Thus, it was crucial to verify the suspected malignant involvement for the definitive diagnosis. The paratracheal lymph node (4R) and the left adrenal gland were both found to harbor metastatic lesions on CT and 18FDG-PET imaging. In theory, EBUS-guided transbronchial needle aspirate (EBUS-TBNA) and EUS-FNA may be applied to perform a biopsy of the target lesion. However, the mediastinal nodes are surrounded by elements of the cardiopulmonary system, vasculature and skeletal components, which makes tissue sampling challenging (16). It was reported that EBUS-TBNA may be associated with occasional serious complications, such as pneumothorax and respiratory failure requiring ventilation (17). In addition, unlike the trachea, the esophagus is flexible. Using magnified real-time imaging, the operator may approach the adrenal gland, easily avoiding the pancreas and local great vessels and reducing the risk of injuring the pleural space under EUS examination. In this manner, biopsy of the adrenal lesion is safer and simpler. A meta-analysis of 18 studies including a total of 1,201 patients reported that the rate of complications caused by EUS-FNA was as low as 0.8% (only 10 cases) (18). In conclusion, EUS-FNA was considered as a superior technique for the assessment of the metastatic lesions, and a definitive diagnosis of the metastasis to the left adrenal from the primary lung adenocarcinoma was finally confirmed.
As previously reported, the adrenal glands are the fourth most common metastatic site in lung cancer (19). Of note, metastases to left adrenal gland are significantly more common compared with those to the right adrenal (20). In the present case, the PET findings were consistent with those of previous reports. Given that the left adrenal is easily accessible through the stomach and may be easily visualized and real-time sampled by EUS, EUS may be considered as the preferred approach to the biopsy of left adrenal lesions (6). The utility of EUS-FNA has been broadened to provide tissue evidence of suspected left adrenal metastases in lung malignancies (21). Schuurbiers et al demonstrated that EUS-FNA has a relatively high sensitivity (86%) and positive predictive value (70%) for malignant lesions in the left adrenal gland (22). Thus, EUS-FNA is a staging tool valuable for identifying metastases to the left adrenal gland in patients with lung cancer.
Although EUS may serve as a replacement for EBUS in assessing mediastinal lymph nodes, the application of EUS-FNA for diagnosing lung malignancies remains limited and controversial. Reddy et al reported that the majority of oncologists in the US did not consider EUS to be helpful for NSCLC staging, with very few (<20%) selecting this procedure as a diagnostic tool (23). Therefore, it is crucial to ameliorate the application of EUS in the staging of lung cancer. In the present case, the diagnostic value of EUS-FNA in lung cancer with suspected left adrenal metastasis was confirmed and, although performing EBUS may be possible, EUS-FNA may also be utilized as the first-line approach to detecting suspected lung malignancy, improving the application of EUS-FNA in the diagnosis of lung cancer with nodal or distant metastases.
From this case study of primary lung adenocarcinoma with mediastinal lymph node and left adrenal metastases described above, left adrenal biopsy via EUS-FNA was found to be an efficient approach to obtaining a final definitive diagnosis. The feasibility and validity of EUS-FNA in the diagnosis and staging of NSCLC was also demonstrated. Even when EBUS is not difficult to perform, EUS-FNA may also be an alternative option for first-line staging in NSCLC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of materials and data
Not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Authors' contributions
ML analyzed the clinical data and drafted the manuscript. YS provided the imaging data. HL performed the bronchoscopy. MX was the gastroenterologist who performed the EUS-FNA. QZ conducted follow-up on the patient in the outpatient clinic. ZG contributed to critical review and supervised the entire work. All the authors have read and approved the final version of this manuscript.
Competing interests
The authors declare that they have no competing interests to disclose.
References
- 1.Yasufuku K, Chiyo M, Koh E, Moriya Y, Iyoda A, Sekine Y, Shibuya K, Iizasa T, Fujisawa T. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer. 2005;50:347–354. doi: 10.1016/j.lungcan.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Detterbeck FC, Jantz MA, Wallace M, Vansteenkiste J, Silvestri GA. American College of Chest Physicians: Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132(3 Suppl):202S–220S. doi: 10.1378/chest.07-1362. [DOI] [PubMed] [Google Scholar]
- 3.ASGE Standards of Practice Committee, corp-author. Jue TL, Sharaf RN, Appalaneni V, Anderson MA, Ben-Menachem T, Decker GA, Fanelli RD, Fukami N, Ikenberry SO, et al. Role of EUS for the evaluation of mediastinal adenopathy. Gastrointest Endosc. 2011;74:239–245. doi: 10.1016/j.gie.2011.03.1255. [DOI] [PubMed] [Google Scholar]
- 4.Hwangbo B, Lee GK, Lee HS, Lim KY, Lee SH, Kim HY, Lee HS, Kim MS, Lee JM, Nam BH, Zo JI. Transbronchial and transesophageal fine-needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest. 2010;138:795–802. doi: 10.1378/chest.09-2100. [DOI] [PubMed] [Google Scholar]
- 5.Ang TL, Chua TS, Fock KM, Tee AK, Teo EK, Mancer K. EUS-FNA of the left adrenal gland is safe and useful. Ann Acad Med Singapore. 2007;36:954–957. [PubMed] [Google Scholar]
- 6.Eloubeidi MA, Seewald S, Tamhane A, Brand B, Chen VK, Yasuda I, Cerfolio RJ, Omar S, Topalidis T, Wilcox CM, Soehendra N. EUS-guided FNA of the left adrenal gland in patients with thoracic or GI malignancies. Gastrointest Endosc. 2004;59:627–633. doi: 10.1016/S0016-5107(04)00296-2. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez LV, Geenen JE, Schmalz MJ, Catalano MF. The underutilization of EUS-guided FNA in the lymph-node staging of non-small-cell lung cancer: Perceptions of chest physicians in Wisconsin. Gastrointest Endosc. 2005;62:517–520. doi: 10.1016/j.gie.2005.04.054. [DOI] [PubMed] [Google Scholar]
- 8.Walsh PR, Williams DB. Mediastinal adenopathy: Finding the answer with endoscopic ultrasound-guided fine-needle aspiration biopsy. Intern Med J. 2005;35:392–398. doi: 10.1111/j.1445-5994.2005.00857.x. [DOI] [PubMed] [Google Scholar]
- 9.Peric R, Schuurbiers OC, Veseliç M, Rabe KF, van der Heijden HF, Annema JT. Transesophageal endoscopic ultrasound-guided fine-needle aspiration for the mediastinal staging of extrathoracic tumors: A new perspective. Ann Oncol. 2010;21:1468–1471. doi: 10.1093/annonc/mdp578. [DOI] [PubMed] [Google Scholar]
- 10.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 11.Alberg AJ, Ford JG, Samet JM. American College of Chest Physicians: Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132(3 Suppl):29S–55S. doi: 10.1378/chest.07-1347. [DOI] [PubMed] [Google Scholar]
- 12.Silvestri GA, Gould MK, Margolis ML, Tanoue LT, McCrory D, Toloza E, Detterbeck F. American College of Chest Physicians: Noninvasive staging of non-small cell lung cancer: ACCP evidenced-based clinical practice guidelines (2nd edition) Chest. 2007;132(3 Suppl):178S–201S. doi: 10.1378/chest.07-1360. [DOI] [PubMed] [Google Scholar]
- 13.Herth FJ, Eberhardt R, Vilmann P, Krasnik M, Ernst A. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax. 2006;61:795–798. doi: 10.1136/thx.2005.047829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill KR, Ghabril MS, Jamil LH, Hasan MK, McNeil RB, Woodward TA, Raimondo M, Hoffman BJ, Hawes RH, Romagnuolo J, Wallace MB. Endosonographic features predictive of malignancy in mediastinal lymph nodes in patients with lung cancer. Gastrointest Endosc. 2010;72:265–271. doi: 10.1016/j.gie.2010.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lankarani A, Wallace MB. Endoscopic ultrasonography/fine-needle aspiration and endobronchial ultrasonography/fine-needle aspiration for lung cancer staging. Gastrointest Endosc Clin N Am. 2012;22(207–219):viii. doi: 10.1016/j.giec.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Hasan MK, Gill KR, Wallace MB, Raimondo M. Lung cancer staging by combined endobronchial ultrasound (EBUS) and endoscopic ultrasound (EUS): The gastroenterologist's perspective. Dig Liver Dis. 2010;42:157–162. doi: 10.1016/j.dld.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 17.Varela-Lema L, Fernández-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: A systematic review. Eur Respir J. 2009;33:1156–1164. doi: 10.1183/09031936.00097908. [DOI] [PubMed] [Google Scholar]
- 18.Micames CG, McCrory DC, Pavey DA, Jowell PS, Gress FG. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest. 2007;131:539–548. doi: 10.1378/chest.06-1437. [DOI] [PubMed] [Google Scholar]
- 19.Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; Analysis of 1,000 autopsied cases. Cancer. 1950;3:74–85. doi: 10.1002/1097-0142(1950)3:1<74::AID-CNCR2820030111>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 20.Ettinghausen SE, Burt ME. Prospective evaluation of unilateral adrenal masses in patients with operable non-small-cell lung cancer. J Clin Oncol. 1991;9:1462–1466. doi: 10.1200/JCO.1991.9.8.1462. [DOI] [PubMed] [Google Scholar]
- 21.Bodtger U, Vilmann P, Clementsen P, Galvis E, Bach K, Skov BG. Clinical impact of endoscopic ultrasound-fine needle aspiration of left adrenal masses in established or suspected lung cancer. J Thorac Oncol. 2009;4:1485–1489. doi: 10.1097/JTO.0b013e3181b9e848. [DOI] [PubMed] [Google Scholar]
- 22.Schuurbiers OC, Tournoy KG, Schoppers HJ, Dijkman BG, Timmers HJ, de Geus-Oei LF, Grefte JM, Rabe KF, Dekhuijzen PN, van der Heijden HF, Annema JT. EUS-FNA for the detection of left adrenal metastasis in patients with lung cancer. Lung Cancer. 2011;73:310–315. doi: 10.1016/j.lungcan.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 23.Reddy NK, Markowitz AB, Abbruzzese JL, Bhutani MS. Knowledge of indications and utilization of EUS: A survey of oncologists in the United States. J Clin Gastroenterol. 2008;42:892–896. doi: 10.1097/MCG.0b013e3180cab11a. [DOI] [PubMed] [Google Scholar]