Abstract
Background:
Sexual minorities (SMs) experience elevated rates of substance use behaviors and disorders relative to heterosexuals; minority stress is theorized to contribute to these disparities. As SMs are not a homogenous group, analyses that aggregate SMs across sexual identity, age, or gender obscure important variation among this population. To date, age- and gender-specific disparities have not been rigorously examined using a large national sample.
Methods:
Using data on 67,354 adults (ages 18–49) from the 2015 and 2016 National Survey of Drug Use and Health we examined age- and gender-specific disparities in smoking, heavy episodic drinking, marijuana use, illicit drug use, and alcohol/substance use disorder. Age groups were ages 18–25, 26–34, and 35–49. Using logistic regression, we estimated age- and gender-specific odds ratios for gay/lesbian and bisexual individuals, relative to heterosexuals; analyses adjusted for demographic characteristics.
Results:
Bisexual women had significantly elevated odds of all outcomes at all ages, relative to heterosexual women. Gay/lesbian individuals had significantly elevated odds for nearly all outcomes compared to same-gender heterosexuals at ages 18–25, but not consistently at older ages. For bisexual men, significant disparities compared to heterosexual men were only observed at ages 35–49 for marijuana use and alcohol/substance use disorder.
Conclusions:
We find notable within-group differences regarding SM disparities. While disparities were most pronounced in young adulthood for gay/lesbian individuals and mid-adulthood for bisexual men, bisexual women uniquely experienced disparities across all ages. Minority stress experiences may vary with respect to gender, age/cohort, and sexual identity, resulting in differential risk for substance use.
Keywords: substance use, substance use disorders, disparities, LGB, sexual minorities
1. Introduction
Individuals who identify as gay, lesbian, or bisexual experience significantly elevated rates of substance use and substance use disorders (SUD) relative to heterosexuals. Disparities are present at initiation, as sexual minority (SM) youth report younger ages of first use than heterosexual youth (Institute of Medicine, 2011). A meta-analysis of 18 school-based surveys reported that US SM youth had nearly three times the odds of any substance use relative to heterosexual youth, smoking rates 2–3 times higher those of heterosexuals and approximately 1.5 times the odds of marijuana use (Marshal et al., 2008). These disparities persist in adulthood: in national surveys in the US and Canada, SM adults report more alcohol use and heavy episodic drinking (HED) than heterosexual adults (Allen and Mowbray, 2016; McCabe et al., 2009; Pakula et al., 2016), and national surveys in the US and Australia have found SM adults to have significantly elevated marijuana use (Demant et al., 2017; McCabe et al., 2009). Similarly, national surveys find SM youth and adults have elevated cigarette smoking rates and higher odds of moderate or heavy smoking, especially women (Cochran et al., 2013; Corliss et al., 2014; Gonzales et al., 2016). Disparities also have been consistently observed with regard to SUDs: a recent study of the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) found that SM adults have nearly twice the odds of any past-year SUD relative to heterosexuals (Kerridge et al., 2017). SMs are more likely to have an alcohol use disorder (AUD) and experience greater AUD severity (Allen and Mowbray, 2016; Amadio, 2006; McCabe et al., 2009). Notably, while heterosexual women have significantly lower rates of substance use than heterosexual men, SM women have similar or higher rates of substance use behaviors and disorders compared to SM men (Demant et al., 2017; Kerridge et al., 2017; McCabe et al., 2013; Operario et al., 2015).
Evidence suggests that bisexuals have particularly elevated rates of substance use relative to both heterosexuals and gay/lesbian individuals. Rates of heavy drinking among bisexual adults are nearly double those among heterosexuals as well as significantly higher than among gays/lesbians (Gonzales et al., 2016), and bisexual adults are more likely to have an AUD compared to gay, lesbian, or heterosexual adults (Kerridge et al., 2017; McCabe et al., 2013). National surveys find the highest smoking rates among bisexuals (Cochran et al., 2013; Demant et al., 2017). Furthermore, many studies have found gender effects, with pronounced disparities among bisexual females. A study of Youth Risk Behavior Study respondents found that female bisexual young adults had higher rates of lifetime drinking than bisexual males and both heterosexual males and females (Talley et al., 2014). Using national data, McCabe et al. (2009) found that bisexual women had higher rates of heavy drinking, alcohol dependence, marijuana use, and illicit drug use than both heterosexual and gay/lesbian women. While bisexual men had higher rates of illicit drug use and alcohol/substance use dependence than heterosexual men, rates were similar between bisexual and gay men (McCabe et al., 2009).
A predominant theory for the observed disparities among SMs is minority stress, namely the excess chronic stress experienced due to membership in a marginalized social group (Meyer, 2003). Experiences of objective prejudice and discrimination may contribute to internal stressors, such as low self-esteem, shame and guilt, internalized stigma, which may elevate risk of substance use, mental health problems, or social isolation (Meyer, 2003). Additionally, structural stigma, defined as “societal-level conditions, cultural norms, and institutional policies that constrain opportunities, resources, and well-being,” has been identified as a significant factor that may lead to or magnify individual-level discrimination (Hatzenbuehler, 2014; Hatzenbuehler and Link, 2014). Salient structural stigma contributors include lack of legal recognition for same-sex marriages, prohibitions on same-sex couple adoption, lack of non-discrimination policies that protect LBGT individuals, and lack of health insurance parity for mental health and physical conditions (Hatzenbuehler, 2014). Prior work has demonstrated a link between living in a state with same-sex marriage prohibition and increased AUD and mood disorders among SM adults (Hatzenbuehler et al., 2010), while a recent study offered compelling evidence that legalization of same-sex marriage significantly reduced suicide attempts among SM adolescents (Raifman et al., 2017).
The extent to which substance use disparities may vary by age has not been rigorously examined in national samples, yet substance use risk factors and minority stress experiences are likely to differ both across life stage and birth cohort. Contextual factors associated with substance use (e.g., education, employment, family structure, social support) may vary in both frequency and timing across the lifecourse for SMs compared to heterosexuals, and may differentially influence substance use among SMs (Fredriksen-Goldsen et al., 2017a; Gonzales, 2014). Different generations of SMs had distinct experiences of societal acceptance/discrimination, as well as different generational perceptions of substance use (Hammack et al., 2018). A limited number of studies have examined age trends in substance use disparities to date. One longitudinal study found that the disparity in heavy drinking among SMs adolescents increased into young adulthood (Dermody et al., 2014); another found that SM reported higher initial rates of substance use and more rapid escalation of use compared to their heterosexual peers (Marshal et al., 2009). Similarly, a study of college students found that young men who have sex with men had alcohol use trajectories that escalated more rapidly than heterosexual young men (Hatzenbuehler et al., 2008). Relatedly, physical health disparities among SMs have been found to vary by age, with larger disparities among adolescents and young adults than older adults. Gender moderated this relationship, as disparities were present for older ages among women but not men (Branstrom et al., 2016).
To further the literature regarding heterogeneity among SMs, this study examines how substance use behavior and disorder disparities among SMs differ by age and gender, using a national sample of adults ages 18 to 49 from the 2015 and 2016 National Survey of Drug Use and Health (NSDUH). As substance use risk factors and minority stress experiences are likely to vary both with respect to life stage and birth cohort, we estimate age- and gender-specific disparities in substance use behaviors (smoking, heavy episodic drinking, marijuana use, and illicit drug use) and disorders (AUD or SUD) among individuals who identify as gay/lesbian or bisexual, relative to heterosexuals. While substance use disparities among SM adults are well-established, this study is novel in that it examines how the magnitudes of these disparities differ across age and gender for multiple substance use behaviors and disorders. Strengthening our understanding of how disparities in substance use behaviors and disorders among SMs varies by age among adults can help us to better understand and address the factors that contribute to these differences and inform screening and treatment initiatives for this population with elevated and underserved need.
2. Methods
2.1. Study population
Starting in 2015, the NSDUH assessed sexual identity among respondents 18 and older. Data were from the 2015 and 2016 NSDUH, a nationally representative study of drug use among the civilian, non-institutionalized US population ages 12 and older. Data were collected using both computer-assisted personal interviewing and audio computer-assisted self-interviewing to facilitate accurate reporting of sensitive behaviors. The public use NSDUH sample comprised 57,146 individuals (70% interview response rate) in 2015 and 56,897 individuals (68% response rate) in 2016. The NSDUH survey is sponsored by Substance Abuse and Mental Health Services Administration (SAMHSA) and fielded by the Research Triangle Institute; all survey respondents gave informed consent and were compensated $30. Our analytic sample was restricted to individuals ages 18 to 49 who self-identified as either heterosexual, lesbian or gay, or bisexual; individuals ages 12 to 17 were not asked the sexual identity question, and SM sample sizes were too small for accurate estimates among those 50 or older so these groups were excluded, as were those who either did not respond to the sexual identity item or responded “don’t know,” resulting in a total sample of 67,354 individuals, including 4,868 SMs.
2.2. Measures
SM status can be defined with respect to identity, behavior, or attraction; identity has been shown to generally have the strongest association with substance use (Corliss et al., 2014; McCabe et al., 2013) and hence is our focus. Sexual identity was assessed by an item that asked, “Which one of the following do you consider yourself to be?” with response choices of “Heterosexual, that is, straight,” “Lesbian or gay,” “Bisexual,” and “Don’t know.”
The substance use outcomes of interest were: past month cigarette use, past month heavy episodic drinking (HED), past year marijuana use, past year other illicit drug use (not including marijuana), and past year alcohol or other substance use disorder (AUD/SUD). Individuals who smoked cigarettes at least once in the past 30 days were defined as having past month cigarette use. Past month HED was defined as at least one occurrence of HED, namely 4+ drinks in a day for women and 5+ drinks in a day for men, in the past 30 days. Past year marijuana use was defined as at least one episode of marijuana use in the past 12 months. Past year other illicit drug use was defined as at least one episode of using hallucinogens, inhalants, methamphetamine, tranquilizers, cocaine, heroin, stimulants, sedatives, or nonmedical use of prescription pain relievers in the past 12 months. The AUD and SUD questions were based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). An individual was classified as having a past year AUD/SUD if they met DSM-IV abuse or dependence criteria for alcohol, marijuana, or any illicit drug in the past 12 months. AUD and other SUD were combined due to low prevalences among adults ages 35–49, increasing the precision of our estimates among SMs.
NSDUH public use data reports age as a categorical variable; our sample spanned three age categories: 18–25, 26–34, and 35–49 years old. Demographic covariates of interest include the following: race/ethnicity (White, Black, Hispanic, Asian, or Other), education level (less than high school, high school, some college / 2 year college degree, or 4 year college degree), urbanicity (large metro area, small metro area, or non-metro area), employment status (full time employment, part time employment, unemployed, or other), household income (below federal poverty level, up to 2 times federal poverty level, or more than 2 times federal poverty level), indicator for any health insurance, overall self-reported health (excellent, very good, good, or fair/poor), marital status (married, widowed, divorced/separated, or never married), household size (1 to 6+ people), number of respondent’s children under 18 years old living in household (0, 1, 2, or 3+).
2.3. Analysis
Weighted prevalence estimates of sexual identity, stratified by both age and gender were calculated, as well as weighted prevalence estimates for all five substance use outcomes, stratified by age, gender, and sexual identity. To quantify disparities experienced by SMs, we implemented logistic regression models with age, gender, and sexual identity indicators and their interactions in order to estimate age-, gender-, and sexual identity-specific odds ratios (ORs) of a given substance use outcome for SM adults relative to heterosexual adults. We report ORs and corresponding 95% confidence intervals (CI) comparing gay/lesbian individuals and bisexual individuals, respectively, to their same-age and same-gender heterosexual peers. Separate regression models were implemented for each of the five outcomes. We implemented both unadjusted regression models as well as models adjusting for the aforementioned ten demographic covariates. All analyses accounted for NSDUH survey design; per NSDUH guidelines, original sampling weights were divided by two to account for pooling across 2015 and 2016. Analyses were conducted in Stata version 15.
3. Results
3.1. Age, gender, and demographic differences among sexual minorities
Our sample included 4,868 SM individuals; notable age and gender differences were observed among heterosexual, gay/lesbian, and bisexual individuals (Table 1). Women were more likely to identify as SM than men, and the proportion of SMs was highest in the youngest age range and decreased in older age ranges. SM women were significantly more likely to identify as bisexual than gay/lesbian at all ages, although this difference was most pronounced at ages 18–25. SM individuals significantly differed from their same-gender heterosexual peers on a variety of other demographic factors (Table 2). While gay men had higher education levels than heterosexual men, SM women were less likely to have a college degree than heterosexual women. Heterosexual men were more likely to be employed full time than gay or bisexual men; gay/lesbian women were more likely to be employed full time than heterosexual women, while bisexual women were less likely. Gay men and gay/lesbian women were markedly less likely to have ever been married and were more likely to be living alone than their heterosexual peers.
Table 1.
Distribution of 2015–2016 NSDUH participants ages 18–49 by age, gender, and sexual identity (n=67,354).
| Male | Female | |||||
|---|---|---|---|---|---|---|
| Heterosexual (n=29,798) | Gay (n=776) |
Bisexual (n=675) | Heterosexual(n=32,688) | Gay/Lesbian (n=743) | Bisexual (n=2,674) | |
| Ages 18–25 | 12,367 | 368 | 387 | 12,606 | 365 | 1,678 |
| 92.9% | 2.8% | 2.9% | 84.6% | 2.5% | 11.3% | |
| Ages 26–34 | 7,703 | 216 | 153 | 8,600 | 189 | 635 |
| 94.0% | 2.6% | 1.9% | 89.2% | 2.0% | 6.6% | |
| Ages 35–49 | 9,728 | 192 | 135 | 11,482 | 189 | 361 |
| 95.4% | 1.9% | 1.3% | 93.1% | 1.5% | 2.9% | |
Note: Proportions represent within gender, within age group distribution of sexual identity and are weighted to account for NSDUH survey design
Table 2.
Demographic characteristics of 2015–2016 NSDUH participants ages 18–49 by gender and sexual identity (n=67,354).
| Male | Female | |||||
|---|---|---|---|---|---|---|
| Heterosexual (n=29,798) | Gay (n=776) | Bisexual (n=675) | Heterosexual (n=32,688) | Gay/Lesbian (n=743) | Bisexual (n=2,674) | |
| Age | ||||||
| 18–25 | 26.0% | 30.1% | 42.9% | 24.2% | 33.1% | 47.3% |
| 26–34 | 28.7% | 34.7% | 27.5% | 28.4% | 32.6% | 31.4% |
| 35–49 | 45.3% | 35.1% | 29.6% | 47.4% | 34.3% | 21.3% |
| Race/ethnicity | ||||||
| White | 58.5% | 57.6% | 56.2% | 57.4% | 55.0% | 61.6% |
| Black | 12.2% | 12.1% | 9.8% | 13.7% | 20.0% | 14.9% |
| Hispanic | 20.5% | 20.4% | 24.6% | 19.4% | 18.3% | 14.8% |
| Asian | 6.1% | 5.5% | 5.2% | 6.8% | 3.0% | 3.5% |
| Other | 2.7% | 4.4% | 4.2% | 2.7% | 3.7% | 5.3% |
| Education | ||||||
| < High school | 14.1% | 7.5% | 15.2% | 10.2% | 9.4% | 14.1% |
| High school | 26.9% | 20.1% | 28.2% | 20.3% | 24.9% | 27.6% |
| Some college / 2 yr degree | 31.5% | 31.9% | 33.8% | 36.3% | 37.0% | 39.5% |
| 4 yr college degree | 27.5% | 40.5% | 22.8% | 33.3% | 28.8% | 18.9% |
| Urbanicity | ||||||
| Large metro | 56.6% | 67.7% | 60.9% | 57.3% | 55.7% | 59.0% |
| Small metro | 29.4% | 24.3% | 27.4% | 29.3% | 31.3% | 28.3% |
| Non-metro | 14.0% | 8.0% | 11.7% | 13.4% | 13.1% | 12.7% |
| Employment | ||||||
| Full time | 69.1% | 62.2% | 54.6% | 52.2% | 58.9% | 42.1% |
| Part time | 10.8% | 15.3% | 18.0% | 18.7% | 12.7% | 21.4% |
| Unemployed | 7.1% | 7.5% | 8.3% | 5.2% | 7.7% | 9.6% |
| Other | 13.0% | 15.0% | 19.2% | 23.9% | 20.6% | 26.9% |
| Household Income | ||||||
| Below federal poverty | 15.7% | 17.0% | 21.3% | 20.3% | 22.1% | 29.7% |
| Up to 2× federal poverty | 20.3% | 16.5% | 23.1% | 21.1% | 21.7% | 25.7% |
| More than 2× federal poverty | 64.0% | 66.5% | 55.6% | 58.7% | 56.2% | 44.6% |
| Has health insurance | 83.2% | 85.4% | 79.2% | 88.4% | 85.0% | 85.8% |
| Overall self-reported health | ||||||
| Excellent | 24.7% | 26.7% | 17.1% | 25.7% | 17.3% | 16.9% |
| Very good | 39.0% | 37.3% | 40.1% | 38.5% | 40.0% | 35.3% |
| Good | 27.9% | 28.7% | 30.0% | 26.6% | 29.2% | 30.5% |
| Fair/poor | 8.4% | 7.2% | 12.9% | 9.2% | 13.5% | 17.4% |
| Marital status | ||||||
| Married | 44.8% | 9.4% | 22.5% | 47.9% | 16.2% | 25.9% |
| Widowed | 1.1% | 2.2% | 3.2% | 1.3% | 2.1% | 2.1% |
| Divorced/separated | 9.2% | 5.3% | 5.7% | 12.3% | 10.7% | 11.9% |
| Never married | 45.0% | 83.1% | 68.6% | 38.5% | 71.0% | 60.2% |
| Household Size | ||||||
| 1 | 7.8% | 17.6% | 7.6% | 5.4% | 10.5% | 5.7% |
| 2 | 19.9% | 39.0% | 26.6% | 19.9% | 34.2% | 24.0% |
| 3 | 23.1% | 19.5% | 23.7% | 22.6% | 25.3% | 23.4% |
| 4 | 25.4% | 12.5% | 16.6% | 26.5% | 16.2% | 24.0% |
| 5 | 14.1% | 5.1% | 14.0% | 14.7% | 6.5% | 11.7% |
| 6+ | 9.6% | 6.2% | 11.4% | 10.9% | 7.3% | 11.1% |
| Respondent’s children <18 in household | ||||||
| 0 | 59.4% | 94.7% | 79.3% | 45.1% | 74.5% | 59.9% |
| 1 | 15.0% | 2.9% | 9.1% | 21.2% | 14.6% | 19.0% |
| 2 | 15.9% | 1.2% | 8.5% | 21.3% | 8.1% | 13.3% |
| 3+ | 9.7% | 1.2% | 3.1% | 12.5% | 2.8% | 7.9% |
Note: Demographic differences were compared across subgroups using Pearson chi-square tests based on weighted frequencies, corrected for survey design. When comparing across all six subgroups, chi-square tests were significant at the 0.05 level for all variables. Additionally, we conducted chi-square tests to compare sexual identity groups within gender. For men, differences were statistically significant for all variables except race/ethnicity and health insurance. For women, differences were statistically significant for all variables except urbanicity.
3.2. Age-, gender-, and sexual identity-specific substance use disparities among sexual minorities
The unadjusted prevalences of substance use and disorder were consistently higher among SMs relative to their same-age and same-gender heterosexual peers (Table 3). Among women, both gay/lesbian and bisexual women had higher prevalences of every outcome relative to heterosexual women at each age group; among men, prevalence was higher for 27 of 30 comparisons. Table 4 and Figure 1 present odd ratio estimates quantifying the disparities between SMs and their same-age and same-gender heterosexual peers. Demographically-adjusted analyses indicate that gay men ages 18–25 were significantly more likely to have smoked cigarettes in the past month (aOR=1.5, 9% CI=[1.1, 2.1]) or used marijuana in the past year (aOR=1.4, 95% CI=[1.1, 1.9]) than their heterosexual male peers. At all ages, gay men were significantly more likely to report past year other illicit drug use, with adjusted ORs ranging from 2.0 to 2.3. There were no differences in HED between gay and heterosexual men at any age. Unadjusted estimates were similar, although of greater magnitude at some ages; additionally, after accounting for demographic differences, rates of marijuana use for gay men 26–34 and ages 35–49 were not significantly higher than their heterosexual peers.
Table 3.
Prevalence of substance use outcomes by age, gender, and sexual identity among 2015–2016 NSDUH participants ages 18–49 (n=67,354).
| Male | Female | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heterosexual (n=29,798) | Gay (n=776) |
Bisexual (n=675) |
Heterosexual (n=32,688) |
Gay/Lesbian (n=743) |
Bisexual (n=2,674) |
||||||||
| Past Month Cigarette Smoking | |||||||||||||
| 18–25 | 3,621 | 28.9% | 128 | 36.4% | 117 | 28.4% | 2,472 | 18.5% | 147 | 38.3% | 658 | 36.8% | |
| 26–34 | 2,559 | 32.8% | 66 | 32.7% | 67 | 40.4% | 2,126 | 22.8% | 73 | 35.8% | 289 | 44.0% | |
| 35–49 | 2,498 | 24.7% | 59 | 28.0% | 37 | 25.7% | 2,550 | 20.6% | 62 | 30.3% | 150 | 41.7% | |
| Past Month Heavy Episodic Drinking | |||||||||||||
| 18–25 | 5,019 | 40.9% | 165 | 46.2% | 118 | 30.9% | 4,495 | 36.3% | 181 | 50.9% | 719 | 42.3% | |
| 26–34 | 3,410 | 45.3% | 105 | 49.3% | 60 | 41.6% | 2,624 | 29.9% | 77 | 38.3% | 285 | 45.1% | |
| 35–49 | 3,511 | 35.1% | 83 | 41.5% | 53 | 38.5% | 2,832 | 23.8% | 67 | 34.0% | 127 | 36.0% | |
| Past Year Marijuana Use | |||||||||||||
| 18–25 | 4,365 | 36.1% | 160 | 46.3% | 153 | 37.2% | 3,316 | 26.4% | 173 | 51.6% | 831 | 49.3% | |
| 26–34 | 1,968 | 26.3% | 77 | 37.1% | 66 | 38.4% | 1,388 | 15.9% | 50 | 26.8% | 226 | 35.9% | |
| 35–49 | 1,465 | 14.0% | 53 | 27.1% | 36 | 23.6% | 1,070 | 8.7% | 35 | 17.7% | 118 | 33.4% | |
| Past Year Illicit Drug Use | |||||||||||||
| 18–25 | 2,557 | 21.1% | 126 | 37.3% | 107 | 27.7% | 1,948 | 16.2% | 103 | 29.3% | 525 | 30.9% | |
| 26–34 | 1,211 | 16.7% | 63 | 32.0% | 43 | 23.0% | 914 | 10.9% | 27 | 16.6% | 181 | 29.1% | |
| 35–49 | 861 | 8.5% | 55 | 25.1% | 22 | 14.1% | 770 | 6.7% | 25 | 11.8% | 74 | 20.5% | |
| Past Year AUD or SUD | |||||||||||||
| 18–25 | 2,117 | 17.1% | 96 | 26.1% | 74 | 21.6% | 1,452 | 11.8% | 81 | 22.2% | 373 | 21.2% | |
| 26–34 | 1,189 | 15.9% | 41 | 20.1% | 37 | 22.9% | 673 | 7.7% | 20 | 11.6% | 133 | 19.5% | |
| 35–49 | 1,086 | 10.4% | 54 | 33.1% | 26 | 19.7% | 639 | 5.4% | 22 | 13.7% | 57 | 14.1% | |
Note: Proportions represent within gender, within sexual identity and within age group prevalence of each substance use behavior. Neither rows nor columns are intended to sum to 100%. All proportions are weighted to account for NSDUH survey design but are not adjusted for covariates.
Table 4.
Unadjusted and adjusted odds ratio (OR) estimates of sexual minority disparities in substance use outcomes among 2015–2016 NSDUH participants ages 18–49, relative to same-age and same-gender heterosexual peers (n=67,354).
| Male | Female | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gay (n=776) | Bisexual (n=675) | Gay/Lesbian (n=743) | Bisexual (n=2,674) | ||||||||||||||
| OR | 95% CI | aOR | 95% CI | OR | 95% CI | aOR | 95% CI | OR | 95% CI | aOR | 95% CI | OR | 95% CI | aOR | 95% CI | ||
| Past Month Cigarette Smoking | |||||||||||||||||
| 18–25 | 1.41 | [1.05, 1.88] | 1.48 | [1.07, 2.05] | 0.98 | [0.71, 1.34] | 0.77 | [0.54, 1.09] | 2.73 | [2.09, 3.56] | 2.45 | [1.86, 3.24] | 2.56 | [2.23, 2.95] | 2.06 | [1.77, 2.40] | |
| 26–34 | 1.00 | [0.68, 1.46] | 1.12 | [0.73, 1.70] | 1.39 | [0.90, 2.15] | 1.25 | [0.78, 2.02] | 1.89 | [1.28, 2.79] | 1.40 | [0.92, 2.12] | 2.66 | [2.17, 3.28] | 1.81 | [1.44, 2.28] | |
| 35–49 | 1.18 | [0.78, 1.79] | 1.03 | [0.65, 1.63] | 1.05 | [0.64, 1.74] | 1.01 | [0.56, 1.80] | 1.68 | [1.15, 2.46] | 1.34 | [0.87, 2.06] | 2.77 | [2.10, 3.65] | 2.07 | [1.54, 2.79] | |
| Past Month HED | |||||||||||||||||
| 18–25 | 1.24 | [0.94, 1.64] | 1.20 | [0.89, 1.61] | 0.64 | [0.47, 0.88] | 0.60 | [0.44, 0.82] | 1.82 | [1.40, 2.36] | 1.80 | [1.38, 2.36] | 1.29 | [1.12, 1.47] | 1.27 | [1.11, 1.46] | |
| 26–34 | 1.17 | [0.82, 1.68] | 0.97 | [0.67, 1.41] | 0.86 | [0.56, 1.33] | 0.85 | [0.55, 1.31] | 1.45 | [0.99, 2.14] | 1.11 | [0.74, 1.67] | 1.92 | [1.56, 2.36] | 1.89 | [1.52, 2.34] | |
| 35–49 | 1.31 | [0.89, 1.93] | 0.94 | [0.63, 1.40] | 1.16 | [0.72, 1.85] | 1.12 | [0.70, 1.78] | 1.66 | [1.15, 2.40] | 1.33 | [0.92, 1.93] | 1.81 | [1.36, 2.39] | 1.68 | [1.25, 2.27] | |
| Past Year Marijuana Use | |||||||||||||||||
| 18–25 | 1.53 | [1.15, 2.03] | 1.43 | [1.08, 1.90] | 1.05 | [0.79, 1.40] | 0.91 | [0.68, 1.21] | 2.97 | [2.29, 3.85] | 2.65 | [2.02, 3.47] | 2.71 | [2.37, 3.10] | 2.48 | [2.14, 2.87] | |
| 26–34 | 1.65 | [1.15, 2.38] | 1.21 | [0.84, 1.73] | 1.75 | [1.14, 2.68] | 1.41 | [0.91, 2.19] | 1.95 | [1.24, 3.04] | 1.32 | [0.83, 2.11] | 2.97 | [2.38, 3.70] | 2.36 | [1.87, 2.97] | |
| 35–49 | 2.29 | [1.47, 3.57] | 1.25 | [0.79, 1.97] | 1.90 | [1.15, 3.16] | 1.70 | [1.00, 2.88] | 2.25 | [1.44, 3.53] | 1.50 | [0.94, 2.39] | 5.27 | [3.93, 7.08] | 4.26 | [3.18, 5.69] | |
| Past Year Illicit Drug Use | |||||||||||||||||
| 18–25 | 2.22 | [1.64, 3.00] | 2.09 | [1.53, 2.86] | 1.43 | [1.04, 1.97] | 1.19 | [0.87, 1.65] | 2.15 | [1.61, 2.88] | 2.13 | [1.59, 2.87] | 2.32 | [2.00, 2.69] | 2.06 | [1.76, 2.41] | |
| 26–34 | 2.35 | [1.61, 3.43] | 1.96 | [1.34, 2.86] | 1.49 | [0.95, 2.34] | 1.26 | [0.79, 2.00] | 1.63 | [0.92, 2.88] | 1.22 | [0.68, 2.17] | 3.36 | [2.66, 4.25] | 2.72 | [2.13, 3.48] | |
| 35–49 | 3.60 | [2.35, 5.52] | 2.26 | [1.47, 3.50] | 1.77 | [0.95, 3.31] | 1.61 | [0.85, 3.05] | 1.87 | [1.14, 3.07] | 1.33 | [0.79, 2.23] | 3.59 | [2.54, 5.07] | 2.76 | [1.93, 3.97] | |
| Past Year AUD or SUD | |||||||||||||||||
| 18–25 | 1.71 | [1.24, 2.37] | 1.55 | [1.10, 2.17] | 1.33 | [0.93, 1.90] | 1.13 | [0.79, 1.61] | 2.13 | [1.55, 2.93] | 1.85 | [1.34, 2.56] | 2.01 | [1.69, 2.39] | 1.75 | [1.46, 2.08] | |
| 26–34 | 1.34 | [0.86, 2.07] | 1.07 | [0.68, 1.68] | 1.57 | [0.98, 2.53] | 1.33 | [0.82, 2.18] | 1.57 | [0.88, 2.80] | 1.14 | [0.63, 2.04] | 2.92 | [2.25, 3.78] | 2.34 | [1.79, 3.06] | |
| 35–49 | 4.25 | [2.80, 6.46] | 2.74 | [1.78, 4.22] | 2.10 | [1.23, 3.60] | 1.87 | [1.06, 3.28] | 2.77 | [1.65, 4.66] | 1.99 | [1.18, 3.35] | 2.85 | [1.96, 4.14] | 2.20 | [1.49, 3.24] | |
Note: Reference group is same-age and same-gender heterosexuals (ref OR=1.0). Bold indicates estimates that are significant at 0.05 level. Adjusted regression models included: race/ethnicity, education level, urbanicity, employment status, household income, health insurance status, overall self-reported health, marital status, household size, and number of respondent’s children under 18 years old living in household. Odds ratio estimates are weighted to account for NSDUH survey design.
Figure 1. Adjusted odds ratios estimates of sexual minority disparities in substance use outcomes among 2015–2016 NSDUH participants ages 18–49, relative to same-age and same-gender heterosexual peers (n=67,354).
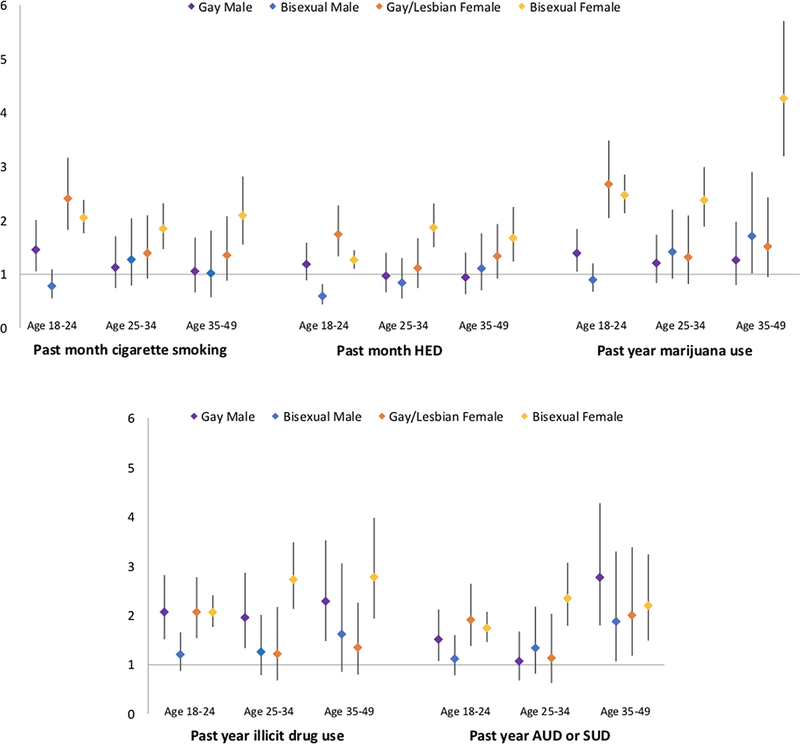
Note: Reference group is same-age and same-gender heterosexuals (ref OR=1.0, denoted by horizontal axis). Adjusted regression models included: race/ethnicity, education level, urbanicity, employment status, household income, health insurance status, overall self-reported health, marital status, household size, and number of respondent’s children under 18 years old living in household. Odds ratio estimates are weighted to account for NSDUH survey design.
Bisexual men exhibited few significant disparities relative to heterosexual men – at ages 35–49, they were significantly more likely to report marijuana use (aOR=1.7, 95% CI = [1.0, 2.9]) or an AUD/SUD (aOR=1.9, 95% CI = [1.1, 3.3]) in the past year. Bisexual men ages 18–25 had significantly lower odds of past month HED (aOR=0.6, 95% CI=[0.4, 0.8]), the only instance of SM individuals having significantly lower substance use than their heterosexual peers.
For gay/lesbian women, substance use disparities were primarily concentrated among young adults 18–25 (adjusting for demographic differences). Indeed, for all five outcomes examined, gay/lesbian women in this age group had significantly elevated odds of use/disorder compared to same-age heterosexual women. OR estimates ranged from 1.8 times the odds of past month HED to 2.5 times the odds of past month cigarette smoking. Additionally, gay/lesbian women ages 35–49 had twice the odds of experiencing a AUD or SUD in the past year compared to heterosexual women (aOR=2.0, 95% CI=[1.2, 3.4]). Notably, in the unadjusted analyses, smoking and marijuana use were significantly elevated among gay/lesbian women ages 26–34 and 35–49, and HED and other illicit drug use were significantly elevated among gay/lesbian women at ages 35–49. These differences were no longer significant after accounting for demographic differences between heterosexual and gay/lesbian women at ages 26–34 and 35–49.
Bisexual women had significantly elevated odds of all substance use outcomes at all ages, relative to same-age heterosexual women. Odds of smoking ranged from 1.8 to 2.1, odds of HED ranged from 1.3 to 1.9, and odds of illicit drug use ranged from 2.1 to 2.8. Marijuana use was particularly elevated, with odds ranging from 2.4 to 4.3 among bisexual women ages 35–49. Additionally, odds of a past year AUD/SUD ranged from 1.8 to 2.3. While there was no consistent pattern in terms of age trends among bisexual women, the highest odds were consistently observed in either the oldest age group (smoking, marijuana use, and illicit drug use) or the middle age group (HED and AUD/SUD). Demographic adjustment somewhat reduced observed disparities, but never eliminated the large differences in substance use and disorder between bisexual and heterosexual women across age groups.
4. Discussion
This study is among the first to comprehensively examine age- and gender-specific disparities among SMs with respect to multiple substance use outcomes using a large national sample of US adults. Our findings demonstrate within-group heterogeneity among SMs, as disparities relative to heterosexuals varied significantly by age, gender, and sexual identity. While SM women had elevated rates of smoking and HED compared to heterosexual women at many ages, SM men generally did not appear to be at elevated risk for smoking and HED compared to heterosexual men. Among bisexuals, there were striking gender differences; bisexual women had profoundly elevated use compared to heterosexual women at all ages 18–49, whereas bisexual men had relatively few disparities relative to their same-age heterosexual male peers. Furthermore, SM subgroups were not uniformly at risk for elevated substance use; rates of HED among bisexual men ages 18–25 were significantly lower than among heterosexual men ages 18–25. Disparities followed distinct age trends across SM subgroups, highlighting that elevated risk for substance use and disorders was not limited to young adulthood, nor did risk decrease linearly across ages groups. SM men and women ages 35–49 reported significantly higher rates of AUD/SUD than same-age and same-gender heterosexuals; the magnitude of this disparity among this age group was largest for gay men, which may be in part associated with experiences and losses during the height of the HIV/AIDS epidemic. Gay men and bisexual women both had significantly elevated rates of illicit drug use (other than marijuana) comared to heterosexuals at ages 18–25, 26–34, and 35–49; among gay men, these disparities may in part reflect club drug usage. While female gender and older age are robust protective factors for most forms of substance use among heterosexuals, these factors appear to have a diminished, and differential, protective effect among SMs (Green and Feinstein, 2012), as age appears to have a stronger protective effect for gay/lesbian women compared to bisexual women. Overall, our results highlight the importance of examining heterogeneity among SMs, a point emphasized by a recent meta-analysis of SM suicide disparities that found risk to vary with respect to the “three-way intersection” of age, gender, and sexual identity (Salway et al., 2018).
We considered both unadjusted and adjusted estimates of disparities across SM subgroups. Conceptually, health disparities are framed as health differences across population groups that are socially determined and thus are unnecessary, avoidable, or unjust (Braveman, 2003). Furthermore, the origins of health disparities are understood to lie in a complex and interrelated set of individual and contextual factors. We note that we are not estimating the “causal effect” of sexual identity, and thus adjusted analyses are not intended to reduce bias in “effect” estimates. Rather, we present adjusted results in order examine whether SM disparities are primarily related to differences in general demographic and contextual factors associated with substance use. We acknowledge that some of the covariates we adjust for may be mediators in the relationship between sexual identity and substance use or have reciprocal associations with substance use. As observed in our sample, both male and female SMs are very distinct from same-gender heterosexuals with respect to all covariates considered. Adjusting for these differences attenuated some of the observed disparities, yet the majority persisted after adjustment, suggesting that other factors or experiences (as discussed below) uniquely experienced by SMs contribute to elevated risk.
SM women and gay men ages 18–25 had significantly elevated rates of almost all substance use outcomes relative to same-age and same-gender heterosexuals. Ages 18–25 is viewed as emerging adulthood, a challenging developmental period associated with peak risk for substance use in the general population (Arnett, 2005). Emerging adulthood involves identity exploration regarding romantic relationships; for SM young adults, the sexual identity formation process may involve confusion, fear, repression, or self-stigma which may elevate risk for substance use during this developmental period (Greene and Britton, 2012). Another contributing factor may be individual-level discrimination and bullying, which is still routinely experienced by SM youth and young adults (Gayles and Garofalo, 2012; Gower et al., 2017; Hatzenbuehler et al., 2015). Lack of family support may also be a salient risk factor, as SM youth report lower levels of parental closeness and higher rates of abuse and homelessness compared to heterosexual youth (Friedman et al., 2011; Pearson and Wilkinson, 2013; Rice et al., 2013). One review found that half of SM youth who come out to their parents experience rejection (Rosario and Schrimshaw, 2013). Bullying, family rejection and identity formation are experiences that are often most acute for SMs in adolescence and young adulthood; during later adulthood, SM individuals may have fully synthesized their identity and established social connections and their own families (Salway et al., 2018), factors which may attenuate risk for substance use. Notably, SM respondents ages 18–25 were born between 1990 and 1998 and are coming of age in the most tolerant social climate to date. They were children and adolescents in 2003 when both Lawrence v. Texas found state sodomy laws to be unconstitutional and Massachusetts became the first state to legalize gay marriage and were young adults in 2015 when Obergefell v. Hodges legalized gay marriage nationwide. While this cohort of individuals ages 18–25 may be facing less structural discrimination relative to older birth cohorts, the profound disparities among this cohort highlight that young SM adults continue to experience extensive, unique lifecourse-related stressors.
Furthermore, our results highlight that bisexual women uniquely reported significant disparities for all substance use outcomes across all ages, while bisexual men had few disparities relative to their same-age heterosexual male peers. It is not fully clear why bisexual men and women have such distinct outcomes. It has been theorized that bisexuals overall face additional types of stigma and discrimination based on their sexual identity on top of the minority stress experienced by gay and lesbian individuals. In particular, they may face skepticism regarding the very existence of bisexuality, arising from the commonly held binary model of sexual orientation (e.g., homosexuality or heterosexuality), leading to perceptions that bisexuals are confused about whether they are heterosexual or gay/lesbian or temporarily experimenting (Mohr et al., 2017). Additionally, bisexual individuals in a same-gender relationship are frequently perceived as gay or lesbian, while those in an opposite-gender relationship are perceived as heterosexual, an “invisibility” that may be internalized and contribute to mental distress and social isolation. Bisexuals have lower rates of identity disclosure and lower levels of LGBT community connectedness (Fredriksen-Goldsen et al., 2017b; Yarns et al., 2016) and may experience rejection from gay and lesbian individuals who believe that bisexuals have access to heterosexual privilege, particularly when in an opposite-gender relationship (Feinstein and Dyar, 2017; Friedman et al., 2014; Roberts et al., 2015). Regarding gender differences, Weiss (2003) discusses that there are greater tensions between lesbians and bisexual women than gay and bisexual men, due to the historical influences of lesbian feminism and the lesbian separatist movement, which regarded bisexual women’s relationships with men as a betrayal to the advancement of lesbian rights. This legacy of friction may contribute to greater exclusion from the LGBT community by bisexual women (Salway et al., 2018; Weiss, 2003). Overall, bisexual invisibility, societal skepticism or confusion over the meaning of bisexuality, as well as stigma from the gay and lesbian community are factors that may persist across the lifecourse and may be differentially higher among women, contributing to persistent substance use disparities across adulthood. It is imperative that future research on substance use disparities among SMs investigates differential risk factors for bisexual men and women.
There are several limitations of this study that warrant consideration. First, our SM measure may be subject to under-reporting. Measures of substance use behaviors and SUD symptoms are self-reported, and thus may be subject to measurement error due to recall bias or social desirability bias. While our analyses adjusted for multiple demographic covariates, the NSDUH does not include an indicator for cohabitation, an important shortcoming given the recency of legalization of same sex marriage. Many other important risk and protective factors that may differ between heterosexuals and SMs were also not measured by the NSDUH (e.g., experiences of discrimination/victimization, sexual assault, social support, HIV-related loss). As the NSDUH sampling frame did not include sexual identity, the subpopulation of SMs is not designed to reflect a nationally-representative sample of SM adults. Finally, due to the cross-sectional nature of our data, we cannot distinguish between disparities arising due to age and due to birth cohort; thus, our results may not generalize to longitudinal lifecourse age trends.
5. Conclusion
SM adults are a diverse population with elevated substance use rates and treatment need. While there are commonalities in experiences among SMs, our results regarding distinct patterns of disparities suggest that addressing unique experiences of women, bisexuals, and older and younger SMs in a treatment context is important. The needs of older gay men and lesbians differ from those of their younger counterparts, while bisexual women appear to have strong need at all ages.
While our study, comprising over 4,800 SM adults, represents one of the largest national samples in which SM substance use disparities have been examined to date, our knowledge of substance use among SMs pales in comparison to the magnitude of prior studies conducted among predominately heterosexual populations. Ongoing work is needed to further our understanding of the ways in which SMs differentially experience substance use and its consequences relative to heterosexuals. Furthermore, as more national surveys ask sexual orientation, it is increasingly possible to examine heterogeneity among SMs in large national samples. Future work should continue to examine SM disparities with regard to the three-way intersection of age, gender, and sexual identity (with a particular focus among older SMs) in order to better understand the relative importance of lifecourse versus birth cohort differences and to identify risk and protective factors associated with differential substance use risk across SM subgroups.
References
- Allen JL, Mowbray O, 2016. Sexual orientation, treatment utilization, and barriers for alcohol related problems: Findings from a nationally representative sample. Drug Alcohol Depend 161, 323–330. [DOI] [PubMed] [Google Scholar]
- Amadio DM, 2006. Internalized heterosexism, alcohol use, and alcohol-related problems among lesbians and gay men. Addict Behav 31(7), 1153–1162. [DOI] [PubMed] [Google Scholar]
- Arnett JJ, 2005. The developmental context of substance use in emerging adulthood. Journal of Drug Issues 35(2), 235–253. [Google Scholar]
- Branstrom R, Hatzenbuehler ML, Pachankis JE, 2016. Sexual orientation disparities in physical health: age and gender effects in a population-based study. Soc Psychiatry Psychiatr Epidemiol 51(2), 289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, 2003. Monitoring equity in health and healthcare: A conceptual framework. J Health Popul Nutr 21(3), 181–192. [PubMed] [Google Scholar]
- Cochran BN, Peavy KM, Robohm JS, 2007. Do specialized services exist for LGBT individuals seeking treatment for substance misuse? A study of available treatment programs. Subst Use Misuse 42(1), 161–176. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Bandiera FC, Mays VM, 2013. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003–2010 National Health and Nutrition Examination Surveys. Am J Public Health 103(10), 1837–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corliss HL, Rosario M, Birkett MA, Newcomb ME, Buchting FO, Matthews AK, 2014. Sexual orientation disparities in adolescent cigarette smoking: intersections with race/ethnicity, gender, and age. Am J Public Health 104(6), 1137–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demant D, Hides L, Kavanagh DJ, White KM, Winstock AR, Ferris J, 2017. Differences in substance use between sexual orientations in a multi-country sample: findings from the Global Drug Survey 2015. J Public Health (Oxf) 39(3), 532–541. [DOI] [PubMed] [Google Scholar]
- Dermody SS, Marshal MP, Cheong J, Burton C, Hughes T, Aranda F, Friedman MS, 2014. Longitudinal disparities of hazardous drinking between sexual minority and heterosexual individuals from adolescence to young adulthood. J Youth Adolesc 43(1), 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein BA, Dyar C, 2017. Bisexuality, minority stress, and health. Curr Sex Health Rep 9(1), 42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Bryan AE, Jen S, Goldsen J, Kim HJ, Muraco A, 2017a. The Unfolding of LGBT Lives: Key Events Associated With Health and Well-being in Later Life. Gerontologist 57(suppl 1), S15–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Shiu C, Bryan AE, Goldsen J, Kim HJ, 2017b. Health Equity and Aging of Bisexual Older Adults: Pathways of Risk and Resilience. J Gerontol B Psychol Sci Soc Sci 72(3), 468–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MR, Dodge B, Schick V, Herbenick D, Hubach R, Bowling J, Goncalves G, Krier S, Reece M, 2014. From Bias to Bisexual Health Disparities: Attitudes toward Bisexual Men and Women in the United States. LGBT Health 1(4), 309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Guadamuz TE, Wei C, Wong CF, Saewyc E, Stall R, 2011. A meta-analysis of disparities in childhood sexual abuse, parental physical abuse, and peer victimization among sexual minority and sexual nonminority individuals. Am J Public Health 101(8), 1481–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayles TA, Garofalo R, 2012. Bullying and School-Based Violence in Lgbt Teenage Populations. Journal of Adolescent Health 50(2), S27–S27. [Google Scholar]
- Gonzales G, 2014. Same-sex marriage--a prescription for better health. N Engl J Med 370(15), 1373–1376. [DOI] [PubMed] [Google Scholar]
- Gonzales G, Przedworski J, Henning-Smith C, 2016. Comparison of Health and Health Risk Factors Between Lesbian, Gay, and Bisexual Adults and Heterosexual Adults in the United States: Results From the National Health Interview Survey. JAMA Intern Med 176(9), 1344–1351. [DOI] [PubMed] [Google Scholar]
- Gower AL, Forster M, Gloppen K, Johnson AZ, Eisenberg ME, Connett JE, Borowsky IW, 2017. School Practices to Foster LGBT-Supportive Climate: Associations with Adolescent Bullying Involvement. Prev Sci. [DOI] [PubMed] [Google Scholar]
- Green KE, Feinstein BA, 2012. Substance Use in Lesbian, Gay, and Bisexual Populations: An Update on Empirical Research and Implications for Treatment. Psychology of Addictive Behaviors 26(2), 265–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene DC, Britton PJ, 2012. Stage of Sexual Minority Identity Formation: The Impact of Shame, Internalized Homophobia, Ambivalence Over Emotional Expression, and Personal Mastery. Journal of Gay & Lesbian Mental Health 16(3), 188–214. [Google Scholar]
- Hammack PL, Frost DM, Meyer IH, Pletta DR, 2018. Gay Men’s Health and Identity: Social Change and the Life Course. Arch Sex Behav 47(1), 59–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, 2014. Structural Stigma and the Health of Lesbian, Gay, and Bisexual Populations. Current Directions in Psychological Science 23(2), 127–132. [Google Scholar]
- Hatzenbuehler ML, Duncan D, Johnson R, 2015. Neighborhood-Level LGBT Hate Crimes and Bullying Among Sexual Minority Youths: A Geospatial Analysis. Violence Vict 30(4), 663–675. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Link BG, 2014. Introduction to the special issue on structural stigma and health. Soc Sci Med 103, 1–6. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS, 2010. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health 100(3), 452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, 2011. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. National Academies Press, Washington DC. [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, Ruan WJ, Chou SP, Zhang H, Jung J, Hasin DS, 2017. Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug Alcohol Depend 170, 82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, Bukstein OG, Morse JQ, 2008. Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction 103(4), 546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, Thompson AL, 2009. Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction 104(6), 974–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ, 2009. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction 104(8), 1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Hughes TL, Boyd CJ, 2013. Sexual orientation and substance abuse treatment utilization in the United States: results from a national survey. J Subst Abuse Treat 44(1), 4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, Jackson SD, Sheets RL, 2017. Sexual Orientation Self-Presentation Among Bisexual-Identified Women and Men: Patterns and Predictors. Arch Sex Behav 46(5), 1465–1479. [DOI] [PubMed] [Google Scholar]
- Operario D, Gamarel KE, Grin BM, Lee JH, Kahler CW, Marshall BD, van den Berg JJ, Zaller ND, 2015. Sexual Minority Health Disparities in Adult Men and Women in the United States: National Health and Nutrition Examination Survey, 2001–2010. Am J Public Health 105(10), e27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakula B, Shoveller J, Ratner PA, Carpiano R, 2016. Prevalence and Co-Occurrence of Heavy Drinking and Anxiety and Mood Disorders Among Gay, Lesbian, Bisexual, and Heterosexual Canadians. Am J Public Health 106(6), 1042–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J, Wilkinson L, 2013. Family relationships and adolescent well-being: are families equally protective for same-sex attracted youth? J Youth Adolesc 42(3), 376–393. [DOI] [PubMed] [Google Scholar]
- Raifman J, Moscoe E, Austin SB, McConnell M, 2017. Difference-in-Differences Analysis of the Association Between State Same-Sex Marriage Policies and Adolescent Suicide Attempts. JAMA Pediatr 171(4), 350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice E, Barman-Adhikari A, Rhoades H, Winetrobe H, Fulginiti A, Astor R, Montoya J, Plant A, Kordic T, 2013. Homelessness experiences, sexual orientation, and sexual risk taking among high school students in Los Angeles. J Adolesc Health 52(6), 773–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts TS, Horne SG, Hoyt WT, 2015. Between a Gay and a Straight Place: Bisexual Individuals’ Experiences with Monosexism. Journal of Bisexuality 15(4), 554–569. [Google Scholar]
- Rosario M, Schrimshaw EW, 2013. The sexual identity development and health of lesbian, gay, and bisexual adolescents: An ecological perspective, in: Patterson CJ, D’Augelli AR (Eds.), Handbook of psychology and sexual orientation Oxford University Press, New York, NY, pp. 87–101. [Google Scholar]
- Salway T, Ross LE, Fehr CP, Burley J, Asadi S, Hawkins B, Tarasoff LA, 2018. A Systematic Review and Meta-Analysis of Disparities in the Prevalence of Suicide Ideation and Attempt Among Bisexual Populations. Arch Sex Behav. [DOI] [PubMed] [Google Scholar]
- Talley AE, Hughes TL, Aranda F, Birkett M, Marshal MP, 2014. Exploring alcohol-use behaviors among heterosexual and sexual minority adolescents: intersections with sex, age, and race/ethnicity. Am J Public Health 104(2), 295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JT, 2003. GL vs BT. Journal of Bisexuality 3(3–4), 25–55. [Google Scholar]
- Yarns BC, Abrams JM, Meeks TW, Sewell DD, 2016. The Mental Health of Older LGBT Adults. Curr Psychiatry Rep 18(6), 60. [DOI] [PubMed] [Google Scholar]


