Précis:
We studied 68Ga-DOTATATE PET/CT imaging in patients with insulinoma and found it identifies most tumors and should be considered as an adjunct imaging study.
Abstract
Context:
Reliable localization of insulinoma is critical for successful treatment.
Objective:
This study compared the accuracy of 68Gallium DOTA-(Tyr3)-octreotate (Ga-DOTATATE) positron emission tomography (PET)/computed tomography (CT) to anatomic imaging modalities, selective arterial secretagogue injection (SASI), and intraoperative ultrasound (IO ultrasound) and palpation for localizing insulinoma in patients who were biochemically cured.
Design, Setting, and Patients:
We conducted a retrospective analysis of 31 patients who had an insulinoma. The results of CT, magnetic resonance imaging (MRI), ultrasound, IO ultrasound, 68Ga-DOTATATE PET/CT, SASI, and operative findings were analyzed.
Intervention, Main Outcome Measures, and Results:
The insulinomas were correctly localized in 17 out of 31 (55%) patients by CT, in 17 out of 28 (61%) by MRI, in 6 out of 28 (21%) by ultrasound, and in 9 out of 10 (90%) by 68Ga-DOTATATE. In 29 of 31 patients (93.5%) who had IO ultrasound, an insulinoma was successfully localized. Thirty patients underwent SASI, and the insulinoma was regionalized in 28 out of 30 patients (93%). In 19 out of 23 patients (83%), manual palpation identified insulinoma. In patients who had all 4 noninvasive imaging studies, CT was concordant with 68Ga-DOTATATE in 6 out of 9 patients (67%), MRI in 8 out of 9 (78%), ultrasound in 0 out of 9; the lesion was only seen by 68Ga-DOTATATE in 1 out of 9 (11%).
Conclusions
68Ga-DOTATATE PET/CT identifies most insulinomas and may be considered as an adjunct imaging study when all imaging studies are negative and when a minimally invasive surgical approach is planned.
Insulinoma is the most common functional pancreatic neuroendocrine tumor, with an incidence of 0.1 to 0.3 cases per 100,000 persons per year (1). In over 90% of cases, they are solitary and benign. Patients present with symptoms of hypoglycemia, with blood glucose in the range of 40 to 50 mg/dL, and show resolution of symptoms with glucose administration, otherwise known as the Whipple triad (2). The diagnosis is confirmed by the demonstration of inappropriately elevated insulin and proinsulin levels associated with serum glucose values of <50 mg/dL during the 48-hour fast period (3, 4). Insulinoma may be associated with a hereditary syndrome in nearly 10% of patients, the most common being multiple endocrine neoplasia type 1 (MEN1) (5).
Insulinomas are evenly distributed throughout the pancreas and are usually less than 2 cm in size in approximately 90% of cases (1). This makes them challenging to localize by traditional imaging techniques such as transabdominal ultrasound, contrast-enhanced computed tomography (CT), and magnetic resonance imaging (MRI). Preoperative invasive localizing studies for insulinoma include endoscopic ultrasound with sensitivity of 75% (6), or selective arterial secretagogue injection (SASI) of the major pancreatic arteries with hepatic venous sampling for insulin to regionalize the insulinoma within the pancreas, which has a sensitivity of up to 88% (7). Exploratory laparotomy with intraoperative ultrasound (IO ultrasound) and bimanual palpation of the pancreas is the most sensitive way to detect insulinoma(s) (7, 8). In cases when intraoperative evaluation fails to localize an insulinoma, blind pancreatic resection is not recommended (9). Detection of insulinoma using 68Gallium (Ga)-DOTA peptide has been previously reported. Different radioligands targeting somatostatin receptors, including 68Ga-DOTA-(Tyr3)-octreotate (DOTATATE), 68Ga-DOTA0-D-Phe1-Tyr3-octreotide (DOTATOC), and 68Ga-DOTA-1-NaI3-octreotide (DOTANOC), have been evaluated for detection of neuroendocrine tumors with promising results (10, 11). 68Ga-DOTATATE/DOTATOC positron emission tomography (PET)/computed tomography (CT) has been described in the detection of insulinomas (12). The aim of this study was to evaluate the accuracy of 68Ga-DOTATATE PET/CT as compared with other anatomic imaging modalities, SASI, and IO ultrasound and palpation for localizing insulinoma in patients who were biochemically cured of their insulinomas.
Materials and Methods
Patients were evaluated for insulinoma at the National Institutes of Health (NIH) Clinical Center and underwent a resection of their insulinoma. We included patients who had insulinoma confirmed by histopathology in our cohort. Patients with insulinoma were enrolled in a clinical protocol evaluating the accuracy of 68Ga-DOTATATE PET/CT (NCT01967537) after written informed consent was obtained. This prospective study was performed under an investigational new drug protocol approved by the US Food and Drug Administration. The study was reviewed and approved by the National Cancer Institute review board and the NIH Radiation Safety Committee.
We performed a retrospective analysis of 31 patients who underwent surgery for insulinoma at the NIH Clinical Center between 4 November 2009 and 24 August 2016 and had insulinoma confirmed by histology and were biochemically cured. Patients’ laboratory evaluations included measurements of fasting glucose, insulin, proinsulin, and C-peptide, as well as the duration of the fast until hypoglycemia was documented. The imaging results for CT, MRI, and ultrasound and 68Ga-DOTATATE, SASI, and intraoperative findings were correlated to the histopathology finding.
68Ga-DOTATATE scans were performed in 10 patients as previously described (13, 14). Five mCi of 68Ga-DOTATATE was administered through a peripheral vein. After approximately 60 minutes, the patient was placed in a supine position in a PET/CT scanner (Siemens Medical Solutions USA, Inc., Malvern, PA), and images from the upper thighs to skull (including pituitary gland) were obtained. A low-dose, noncontrast CT was used for attenuation correction and anatomic localization. Maximum standardized uptake values were measured based on patient total body weight.
Data analyses
We analyzed the 68Ga-DOTATATE PET/CT uptake status by patient demographic, clinical characteristics, familial vs sporadic insulinoma, and laboratory data. Spearman’s correlation coefficient, Student t test, and χ2 tests were used to test for associations between clinical, pathology, and operative variables in patients who did and did not have 68Ga-DOTATATE PET/CT imaging to evaluate 68Ga-DOTATATE PET/CT imaging’s impact on patient care. P < 0.05 was considered statistically significant. IBM SPSS Statistics Data Editor (New York, NY) and Microsoft Excel (Redmond, WA) were used for statistical analyses.
Results
Clinical characteristics
All patients (N = 31) had a supervised fast with a median duration of 12.5 hours (range: 3 to 41 hours) and the median fasting end glucose was 38 mg/dL (range: 27 to 49). Twenty-seven patients had sporadic insulinoma, and 4 patients had MEN1-associated insulinoma. The demographic and clinical characteristics of the study cohort are summarized in Table 1. Thirteen patients (42%) underwent an open resection of the insulinoma, 10 patients (32%) had a hand-assisted laparoscopic resection, and 8 patients (26%) had a laparoscopic resection. All patients, at the last follow-up, were biochemically cured of their insulinoma. A comparison of patients who had 68Ga-DOTATATE imaging to those who did not revealed no significant difference in age, body mass index, glucose, C-peptide, insulin, and proinsulin before and after supervised fasting between those patients (Table 1). There was also no significant difference in the type of operation and duration of the operation and perioperative outcomes based on having a positive 68Ga-DOTATATE PET/CT scan as compared with patients who did not have the imaging study (Fig. 1 and Table 1).
Table 1.
Study Cohort Clinical and Biochemical Characteristics and Treatment
| Variables | DOTATATE | No DOTATATE | P Value (Fisher's Exact Test)a |
|---|---|---|---|
| Gender | 0.68 | ||
| Male | 4 | 7 | |
| Female | 6 | 14 | |
| Type of operation | 1.0 | ||
| Open | 5 | 8 | |
| Laparoscopic (± hand assist) | 5 | 13 | |
| Complicationsb | 0.42 | ||
| Pancreatic leak | 2 | 10 | |
| No pancreatic leak | 8 | 11 | |
| Sporadic | 7 | 19 | |
| MEN1 | 1 | 3 | |
| Intraoperative findings | |||
| Palpation | 5/8 | 14/15 | |
| Ultrasound | 9/10 | 20/21 | |
| SASI correlated with pathology | 9/10 | 19/20 | |
| Median | Range | P Value (t Test)c | |
| Age (y) | 57.5 | 21–75 | 0.65 |
| Body mass index (kg/m2) | 31 | 20–49 | 0.86 |
| Case duration (min) | 241 | 116–508 | 0.16 |
| Size of insulinoma (cm) | 1.5 | 0.7–2.5 | 0.08 |
| Fasting end glucose (mg/dL) | 38 | 27–49 | 0.15 |
| Fasting end insulin (μU/mL) | 23.2 | 2.7–154 | 0.24 |
| Fasting end proinsulin (pmol/L) | 120 | 11–890 | 0.23 |
| Fasting end C-peptide (ng/mL) | 3.1 | 1.4–10.3 | 0.48 |
| Duration of fasting (h) | 13 | 3–41 | 0.62 |
a Comparison between patients with positive 68Ga-DOTATATE scans and those who did not have a 68Ga DOTATATE scan.
b All Grade A, self-limited requiring no intervention.
c Mann–Whitney U test was used for the fasting end C-peptide, as these values were not normally distributed.
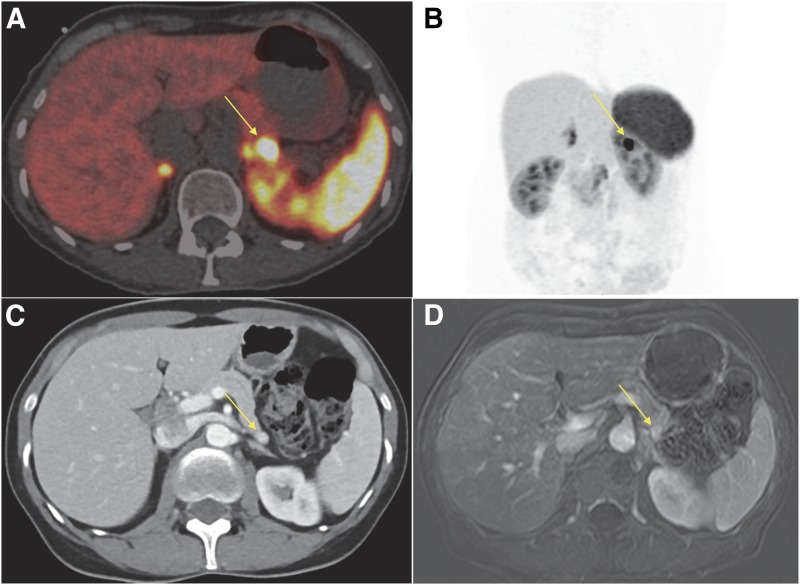
Figure 1.
Representative images of an insulinoma. (A) Axial 68Ga-DOTATATE fused PET/CT arrow pointing to the uptake in the pancreas. (B) 68Ga-DOTATATE anterior 3-dimensional maximum intensity projection; arrow pointing to the uptake in the pancreas. (C) Axial arterial phase CT; arrow pointing to the arterially enhancing lesion in the tail of the pancreas. (D) MRI axial 3-dimensional with arterial contrast imaging; arrow localizing an arterially enhancing lesion in the tail of the pancreas.
Accuracy of 68Ga-DOTATATE PET/CT
Ten patients underwent a 68Ga-DOTATATE scan, and 9 out of 10 (90%) had an insulinoma successfully localized. In 9 patients, the tumor was regionalized using SASI, and the median size of insulinoma was 1.5 cm (range: 0.7 to 2.5 cm). The gold standard for defining a positive localization result was histology. In all 10 patients, the tumors stained positive for insulin and were well differentiated. Eight out of 9 tumors had a Ki-67 of less than 2% (World Health Organization grade I); 1 had a Ki-67 of 3% to 5% (World Health Organization grade II; 68Ga-DOTATATE positive). In 4 patients, the tumor was localized to the distal pancreas; in 3 patients, to the head of the pancreas; and in 3 patients, to the body of the pancreas. Other imaging modalities performed in the 10 patients included CT, MRI, and ultrasound. Transabdominal ultrasound did not identify an insulinoma in any of the 10 patients. A CT scan accurately localized the insulinoma in 6 out of the 10 patients, and an MRI localized the insulinoma in 8 of the 10 patients. The patient with negative 68Ga-DOTATATE underwent an enucleation of an uncinate process insulinoma. The tumor measured 1.5 cm in the greatest dimension and stained positive for insulin, chromogranin, and synaptophysin. The Ki-67 (MIB-1) labeling index was 1% to 2% and the mitotic count was 1/10 high-power fields. One patient had negative anatomic imaging studies (CT, MRI, and ultrasound), and no lesion was identified using IO ultrasound. The patient underwent an extended distal pancreatectomy and was biochemically cured. Pathology evaluation demonstrated multiple well-differentiated neuroendocrine tumors, the largest measuring 4 mm. The neuroendocrine tumors present stained positively for chromogranin and insulin and negative for gastrin, glucagon, pancreatic polypeptide, and somatostatin.
Accuracy of imaging modalities in entire study cohort
Out of the 31 patients with pathology-confirmed insulinoma, CT accurately localized the lesion in 17 out of 31 patients (55%, average tumor size of 1.37 cm). MRI localized the insulinoma in 17 out of 28 patients (61%, average tumor size of 1.37 cm). In 12 patients, both CT and MRI were positive. Abdominal ultrasound accurately localized the insulinoma in 6 out of 28 (21%) of the patients. IO ultrasound was performed in 31 patients, in 29 of whom insulinoma was successfully localized (93%). In 23 patients who had an open or hand-assisted laparoscopic exploration, manual palpation identified 19 out of 23 (83%) of the insulinoma. In patients who had all 4 noninvasive imaging studies (CT, MRI, ultrasound, and 68Ga-DOTATATE), CT was concordant with 68Ga-DOTATATE in 6 out of 9 patients (67%) and MRI in 7 out of 9 (78%), and in 1 out of 9 patients (11%), the lesion was only seen by 68Ga-DOTATATE (Table 2). Transabdominal ultrasound was performed in 8 patients and did not localize the tumor in any of them.
Table 2.
Concordance Between 68Ga-DOTATATE Anatomic Imaging Studies
| 68Ga-DOTATATE | Concordance (%) | |
|---|---|---|
| CT (+) | 6/9 | 67 |
| MRI (+) | 7/9 | 78 |
| Ultrasound (+) | 0/9 | 0 |
Discussion
In this study, we compared the results of 68Ga-DOTATATE PET/CT to other preoperative anatomic imaging and SASI to determine the accuracy of 68Ga-DOTATATE. It was positive in 9 out of 10 patients. In 1 of the 10 patients in whom insulinoma was regionalized with SASI, 68Ga-DOTATATE PET/CT was the only positive imaging study, as the other 5 imaging studies were negative. When we compared clinical variables, biochemical variables, treatment, patient outcome, and tumor histology, there was no significant difference between patients who underwent 68Ga-DOTATATE PET/CT imaging vs those patients who did not have this imaging.
Insulinomas are associated with substantial morbidity and mortality when not treated. The only curative treatment of this tumor is surgical resection. However, localization of insulinoma can be challenging, as most tumors are often less than 2 cm and may be present in any part of the pancreas. Multiple preoperative imaging modalities may be used to localize insulinoma in addition to endoscopic ultrasound, but in most studies, SASI is the most accurate test for regionalizing the tumor. Whereas it is neither necessary nor cost effective to perform multiple imaging studies in patients with insulinoma, this was done at our institution under a clinical investigation protocol and allowed for a head-to-head comparison to evaluate the clinical utility, if any, of 68Ga-DOTATATE scanning.
68Ga-DOTATATE has a high affinity to somatostatin receptors 2, which are commonly expressed in neuroendocrine tumors (15). Prasad et al. (12) found that somatostatin receptors 2 expression in insulinomas is present in up to 80% of cases. 68Ga-DOTATATE PET/CT has been reported to detect neuroendocrine tumors as small as 6 mm in size (11). One possible advantage of 68Ga-DOTATATE is to exclude the presence of additional pancreatic neuroendocrine tumors not detected by anatomic imaging in inherited syndromes such as MEN1. Although SASI is more accurate for regionalizing insulinomas, it is a costly and invasive test that requires a skilled interventional radiologist, who may not be readily available, and it may be associated with complications. 68Ga-DOTATATE was shown to be safe with total radiation exposure less than that of 111In-DTPA-octreotide and 18F-FDG (16). To our knowledge, there have been no prospective studies to evaluate the accuracy of 68Ga-DOTATATE PET/CT to localize insulinoma. Prasad et al. (12) analyzed the sensitivity of 68Ga-DOTATATE/DOTANOC in a retrospective study for the localization of insulinoma. Seven patients underwent a 68Ga-DOTANOC, which successfully localized the insulinoma in 6 patients. Six patients underwent 68Ga-DOTATATE, and an insulinoma was localized in 5 of them. Of these 5 patients, 1 had a benign insulinoma, 2 had malignant insulinomas, and 2 had nesidioblastosis (12). 68Ga-DOTA-exendin-4 PET/CT has also been evaluated in patients with insulinoma. Wild et al. detected all insulinomas in 2 prospective studies, consisting of 4 patients (17) and 6 patients (18). Sharma et al. (19) evaluated 68Ga-DOTANOC PET/CT imaging in 35 patients suspected to have insulinoma and reported a sensitivity of 25.8% and a specificity of 25%.
As the incidence of insulinoma is 0.1 to 0.3 cases per 100,000 persons per year (1), 1 of the limitations of our study is the low number of patients. In addition, not all of the patients had all of the imaging modalities performed, and only 10 patients underwent 68Ga-DOTATATE PET/CT.
In summary, 68Ga-DOTATATE PET/CT is a noninvasive imaging modality that identifies most insulinomas. It appears to offer limited additional information when other anatomic imaging studies localize the tumor and should be considered an adjunct when all imaging studies are negative in a patient with an insulinoma, especially if a focused or minimally invasive surgical approach is preferred.
Acknowledgments
This research was supported, in part, by the intramural research program of the Center for Cancer Research, National Cancer Institute.
Disclosure Summary: The authors have nothing to disclose.
Abbreviations:
- CT
computed tomography
- DOTATATE
DOTA-(Tyr3)-octreotate
- Ga
Gallium
- MEN1
multiple endocrine neoplasia type 1
- MRI
magnetic resonance imaging
- NIH
National Institutes of Health
- PET
positron emission tomography
- SASI
selective arterial secretagogue injection
References
- 1. Zhou J, Enewold L, Stojadinovic A, Clifton GT, Potter JF, Peoples GE, Zhu K. Incidence rates of exocrine and endocrine pancreatic cancers in the United States. Cancer Causes Control. 2010;21(6):853–861. [DOI] [PubMed] [Google Scholar]
- 2. Whipple AO, Frantz VK. Adenoma of islet cells with hyperinsulinism: a review. Ann Surg. 1935;101(6):1299–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hirshberg B, Livi A, Bartlett DL, Libutti SK, Alexander HR, Doppman JL, Skarulis MC, Gorden P. Forty-eight-hour fast: the diagnostic test for insulinoma. J Clin Endocrinol Metab. 2000;85(9):3222–3226. [DOI] [PubMed] [Google Scholar]
- 4. Guettier JM, Lungu A, Goodling A, Cochran C, Gorden P. The role of proinsulin and insulin in the diagnosis of insulinoma: a critical evaluation of the Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4752–4758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mansour JC, Chen H. Pancreatic endocrine tumors. J Surg Res. 2004;120(1):139–161. [DOI] [PubMed] [Google Scholar]
- 6. Morera J, Guillaume A, Courtheoux P, Palazzo L, Rod A, Joubert M, Reznik Y. Preoperative localization of an insulinoma: selective arterial calcium stimulation test performance. J Endocrinol Invest. 2016;39(4):455–463. [DOI] [PubMed] [Google Scholar]
- 7. Guettier JM, Kam A, Chang R, Skarulis MC, Cochran C, Alexander HR, Libutti SK, Pingpank JF, Gorden P. Localization of insulinomas to regions of the pancreas by intraarterial calcium stimulation: the NIH experience. J Clin Endocrinol Metab. 2009;94(4):1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shin JJ, Gorden P, Libutti SK. Insulinoma: pathophysiology, localization and management. Future Oncol. 2010;6(2):229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hirshberg B, Libutti SK, Alexander HR, Bartlett DL, Cochran C, Livi A, Chang R, Shawker T, Skarulis MC, Gorden P. Blind distal pancreatectomy for occult insulinoma, an inadvisable procedure. J Am Coll Surg. 2002;194(6):761–764. [DOI] [PubMed] [Google Scholar]
- 10. Yang J, Kan Y, Ge BH, Yuan L, Li C, Zhao W. Diagnostic role of Gallium-68 DOTATOC and Gallium-68 DOTATATE PET in patients with neuroendocrine tumors: a meta-analysis. Acta Radiol. 2014;55(4):389–398. [DOI] [PubMed] [Google Scholar]
- 11. Srirajaskanthan R, Kayani I, Quigley AM, Soh J, Caplin ME, Bomanji J. The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med. 2010;51(6):875–882. [DOI] [PubMed] [Google Scholar]
- 12. Prasad V, Sainz-Esteban A, Arsenic R, Plöckinger U, Denecke T, Pape UF, Pascher A, Kühnen P, Pavel M, Blankenstein O. Role of (68)Ga somatostatin receptor PET/CT in the detection of endogenous hyperinsulinaemic focus: an explorative study. Eur J Nucl Med Mol Imaging. 2016;43(9):1593–1600. [DOI] [PubMed] [Google Scholar]
- 13. Sadowski SM, Millo C, Cottle-Delisle C, Merkel R, Yang LA, Herscovitch P, Pacak K, Simonds WF, Marx SJ, Kebebew E. Results of (68)gallium-DOTATATE PET/CT scanning in patients with multiple endocrine neoplasia type 1. J Am Coll Surg. 2015;221(2):509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sadowski SM, Neychev V, Millo C, Shih J, Nilubol N, Herscovitch P, Pacak K, Marx SJ, Kebebew E. Prospective study of 68Ga-DOTATATE positron emission tomography/computed tomography for detecting gastro-entero-pancreatic neuroendocrine tumors and unknown primary sites. J Clin Oncol. 2016;34(6):588–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Druckenthaner M, Schwarzer C, Ensinger C, Gabriel M, Prommegger R, Riccabona G, Decristoforo C. Evidence for somatostatin receptor 2 in thyroid tissue. Regul Pept. 2007;138(1):32–39. [DOI] [PubMed] [Google Scholar]
- 16. Walker RC, Smith GT, Liu E, Moore B, Clanton J, Stabin M. Measured human dosimetry of 68Ga-DOTATATE. J Nucl Med. 2013;54(6):855–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Antwi K, Fani M, Nicolas G, Rottenburger C, Heye T, Reubi JC, Gloor B, Christ E, Wild D. Localization of hidden insulinomas with (6)(8)Ga-DOTA-exendin-4 PET/CT: a pilot study. J Nucl Med. 2015;56(7):1075–1078. [DOI] [PubMed] [Google Scholar]
- 18. Christ E, Wild D, Forrer F, Brändle M, Sahli R, Clerici T, Gloor B, Martius F, Maecke H, Reubi JC. Glucagon-like peptide-1 receptor imaging for localization of insulinomas. J Clin Endocrinol Metab. 2009;94(11):4398–4405. [DOI] [PubMed] [Google Scholar]
- 19. Sharma P, Arora S, Karunanithi S, Khadgawat R, Durgapal P, Sharma R, Kandasamy D, Bal C, Kumar R. Somatostatin receptor based PET/CT imaging with 68Ga-DOTA-Nal3-octreotide for localization of clinically and biochemically suspected insulinoma. Q J Nucl Med Mol Imaging. 2016;60(1):69–76. [PubMed] [Google Scholar]