Introduction
Chronic hematoceles are rare scrotal masses. Clinically and sonographically, a hematocele may simulate a testicular neoplasm. We describe a case of an idiopathic hematocele, which was mistaken for malignant mesothelioma of the tunica vaginalis testis (see Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Scrotal sac filled with a large, heterogeneous and mixed collection with internal non pure cystic areas and thick septations.
Fig. 2.
Gross photograph of the cut surface of the specimen showing a cavity that was filled with old clotted blood (hematocele).
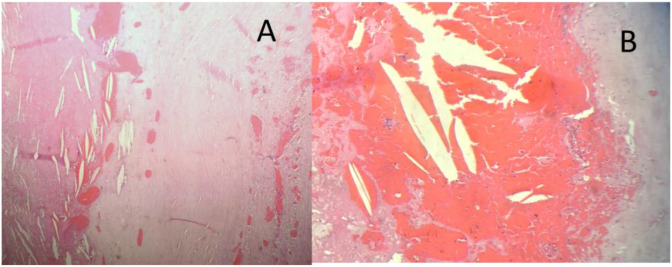
Fig. 3.
The tunica vaginalis was thickened and composed of hypocellular fibrous tissue (A) and cholesterol granuloma(B).
Case report
A 57 -year-old man presented with painless scrotal swelling for 2 years. The patient had no history of asbestos exposure or any surgical procedures. On physical examination, a hard and painless mass was evident in the right scrotum and was suggestive of a hydrocele on palpation. No right inguinal hernia was evident. The levels of αFP, HCG, and LDH were not elevated, and chest radiography was normal. Scrotal ultrasonography revealed a large right hydrocele and extra testicular mass with solid hyperechoic areas separated by irregular septations along the walls of the scrotum. The parenchyma and size of the right testis were normal. Although the levels of tumor markers were normal, the presence of multiloculated paratesticular mass encouraged us to perform right radical inguinal orchidectomy. The postoperative course was uneventful, and the patient was discharged on postoperative day 2. Grossly, the resected mass measured 22 × 16 × 8 cm in diameter, the tunica vaginalis was thickened and entirely filled with brown hemorrhagic material and fibrin. Microscopic examination revealed a thickened tunica vaginalis that contained Cholesterol granuloma composed of fibrogranulomatous with numerous cholesterol crystals and foreign body giant cells. No epithelial type proliferation, cellular atypia or malignant characteristics were identified. The final diagnosis was hematocele.
Discussion
A hematocele is the accumulation of blood in between the layers of the tunica vaginalis and can reach large volumes.
Chronic scrotal hematocele is a rare condition with only 35 cases reported so far in the known literature.5According to etiology, hematoceles can be classified into idiopathic and secondary ones. Idiopathic or spontaneous hematoceles give a history of neither trauma to the testis, nor pain in the organ and seems to be more common in elderly patients.1 Secondary hematoceles are usually associated with trauma, surgery or neoplasm, but sometimes can be caused by hematological alterations or vasculitis.2 The etiology of the hematocele formation in our patient is unknown.
Clinically, hematocele present as slowly progressing, usually non tender scrotal mass which is difficult to transilluminate, the duration of the swelling varies from few months to several decades.5 Hematocele is difficult to diagnose preoperatively because its symptoms may mimic cysts or neoplasms.4At ultrasonography (U/S) hematoceles appear as complex cystic lesions with internal septations and loculations.3 When U/S diagnosis is equivocal it is useful to perform magnetic resonance imaging (MRI), which has a higher sensibility reveal encapsulated mass with high signal intensity in both T1 and T2 images.5 However, it cannot reliably differentiate benign from malignant pathology.
In our case, there was high suspicion of malignant mesothelioma of the tunica vaginalis testis which prompted the execution of inguinal orchidectomy and we found a capsule filled by a friable, soft brown hemorrhagic material and fibrin without evidence of neoplasia.
Conclusion
Idiopathic hematocele should be considered in the differential diagnosis of scrotal masses. The correct management of hematoceles includes early recognition and complete evacuation of the hematoma. This managements avoids testicular compression and prevents epididymo-orchitis abscess formation and necrosis.
Conflicts of interest
None for all authors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Leibovitch I., Ramon J., Ben Chaim J., Nass D., Goldwasser B. Chronic hematocele complicating renal failure and hemodialysis. J Urol. 1991;146:162–164. doi: 10.1016/s0022-5347(17)37742-x. [DOI] [PubMed] [Google Scholar]
- 2.Klimis T., Alexandris I., Kyriakidis A., Athanassiou K., Pyrgioti M., Kyriazis G. A case of chronic huge scrotal hematocele. Internet J Surg. 2013;30(Number 4) [Google Scholar]
- 3.Vikram S Dogra, Ronald H., Oka Mayumi, Deborah J. Sonography of the scrotum. Radiology. 2003;227:18–36. doi: 10.1148/radiol.2271001744. [DOI] [PubMed] [Google Scholar]
- 4.Barale M., Oderda M., Faletti R., Falcone M., Pisano F. The strange case of a hematocele mistaken for a neoplastic scrotal mass. J. Can. Urol. Assoc. 2015;9(3–4):217–219. doi: 10.5489/cuaj.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babakri M.M. Chronic scrotal hematocele: a rare entity and diagnostic dilemma. Urol Nephrol Open Access J. 2017;4(5) 00142. [Google Scholar]