Abstract
A case of a young Saudi patient with a previous diagnosis of bronchial asthma, nasal polyps, and chronic smoker, presented with atypical chest pain, elevated serum troponin and borderline ischemic electrocardiogram (ECG) changes, with no significant regional wall motion abnormalities at bedside echocardiography is reported. The patient was admitted to the coronary care unit for continuous monitoring as possible acute coronary syndrome, non-ST elevation myocardial infarction (STEMI). One hour after admission, the patient had ventricular fibrillation (VF) cardiac arrest that required three DC shocks and amiodarone bolus before returning of spontaneous circulation, which followed the fourth shock. The resuscitation took 15 minutes of cardiopulmonary resuscitation (CPR). An immediate 12-leads ECG showed significant ST elevation in precordial leads that mandate an urgent coronary angiogram that revealed patent coronary arteries, therefore spasm of normal coronary arteries was postulated as the operative factor. The cardiac magnetic resonance image (MRI) showed a picture of transmural anterior myocardial infarction, which correlates with the follow up echocardiogram reporting hypokinetic anterior wall. A complete history was taken and no use of illicit drugs or alcohol was found. The unusual presentation in such a patient with evidence of extensive anterior STEMI and normal coronary arteries raise the thought of considering uncommon causes. In view of previous medical history and laboratory evidence of eosinophilia, Kounis syndrome was considered dominant in the differential diagnosis.
Keywords: Coronary, Myocardial, infarction, Kounis
1. Introduction
Myocardial infarction with normal coronary arteries angiography (MINCA) is a life-threatening event with many open questions for physicians and patients [1]. MINCA is common with a prevalence of 1–12% of all myocardial infarctions. The pathogenic mechanisms of MINCA are still unknown, but endothelial dysfunction has been suggested as a possible cause [2].
A history of inflammatory disease was more common in patients with MINCA than in healthy controls. Hypercoagulability due to inflammation has been also reported as a possible reason for MINCA. There are some case reports with patients presenting with MINCA during exacerbation of systemic inflammatory disease without evidence of coronary vasculitis, whereas others have identified a secondary myocarditis. The condition of inflammation and hypercoagulability needs to be elaborated in future studies of MINCA [2].
Our case of a 32-year-old Saudi male soldier presented with a history of 10 days atypical chest pain with increased intensity over the past 7 hours. The patient’s medical history included nasal polyps, bronchial asthma for 10 years on bronchodilators and cigarette smoker (smoking 10 cigarettes/d for 14 years). There was no other significant medical history with irrelevant family history and no history of sudden cardiac death. The patient was hemodynamically stable with normal first and second heart sounds on clinical examination. An electrocardiogram (ECG) on presentation showed borderline ST segment elevation of <1 mm in the inferior leads (Fig. 1). Initial transthoracic echocardiography in the emergency room showed no significant regional wall motion abnormalities (RWMA) with normal left ventricular size and ejection fraction of >55%. The first set of serum troponin was elevated (746 pg/mL, normal troponin <34.2 pg/mL). Normal lipid profile, toxicology screen was sent and chest radiograph showed no abnormality (Fig. 2).
Figure 1.
ECG: normal sinus rhythm with <1 mm ST elevation in the inferior leads. ECG = electrocardiogram.
Figure 2.
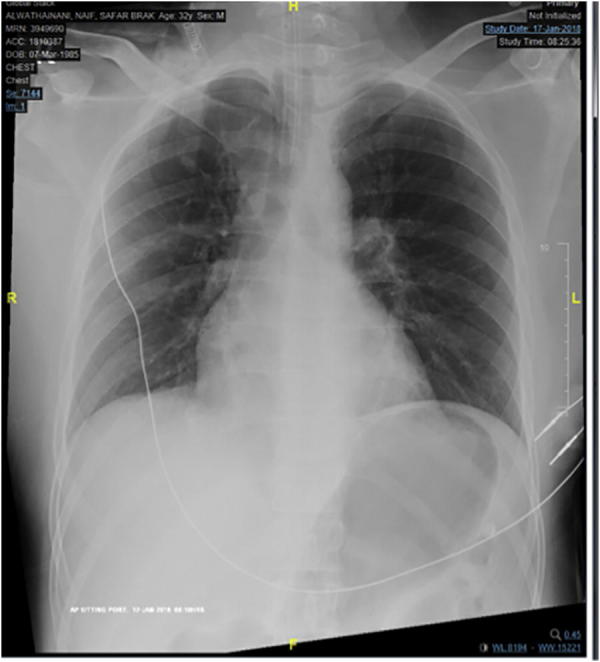
Chest X ray: reported normal.
The patient was admitted to the coronary care unit for clinical management as possible non-ST elevation myocardial infarction, started on guidelines directed anti-ischemic measures.
One hour later the patient suddenly had ventricular fibrillation cardiac arrest (Fig. 3) with immediate cardiopulmonary resuscitation (CPR) (according to American resuscitation guidelines) was commenced, three DC shocks and epinephrine, which did not give any response. Following the fourth shock and amiodarone bolus (150 mg IV), he returned to spontaneous circulation within a total of 15 minutes CPR. The patient was intubated and mechanically ventilated with use of inotropic support. Repeated 12 lead ECG showed significant precordial ST elevation >20 mm in V2 and >10 mm in V3, with 2–5 mm elevation in the remaining precordial leads (Fig. 4). Urgent coronary angiogram (∼1 hour post returned to spontaneous circulation) revealed patent coronary arteries (Fig. 5); spasm of normal coronary arteries was postulated as the operative factor. Post arrest transthoracic echocardiogram showed mild to moderately reduced left ventricular systolic function and ejection fraction 40% with severe anteroseptal hypokinesis at the mid and apical segments (Fig. 6).
Figure 3.
VF arrest. VF = ventricular fibrillation.
Figure 4.
Repeated ECG showed significant precordial ST elevation >20 mm in V2 and >10 mm in V3, with 2–5 mm elevation in remaining precordial leads. ECG = electrocardiogram.
Figure 5.
Coronary angiogram revealed patent coronary arteries.
Figure 6.
Transthoracic echocardiogram apical four chamber view that showed grossly normal left ventricle size. Left ventricular systolic function is mild to moderately reduced and ejection fraction = 40–45%. There is severe anteroseptal hypokinesis at the mid and apical segments.
Laboratory results showed an increased level of serum troponin from 746 pg/mL to peaked level of 36498 pg/mL (2 days from initial set). Renal profile and HgA1c (haemoglobin A1c or glycated haemoglobin) were normal. Raised eosinophilic count was 8.3%. Urine for toxic screen was negative for cocaine, amphetamine, and opiates.
For the unusual presentation and finding, cardiac MRI was performed the day after and showed the left ventricle normal in size with moderate reduction of left ventricular systolic function and ejection fraction 33%. There was moderate to severe hypokinesia of the mid distal anteroseptum and the apical cap, delayed subendocardial enhancement involving a large area proximal, mid to distal anteroseptum, and a central core of hypointensity suggestive of microvascular obstruction. The rest of the myocardial segments were normal. Large acute myocardial infarction with signs of microvascular obstruction in the left anterior descending (LAD) territory was reported (Fig. 7).
Figure 7.

Cardiac MRI. Large acute myocardial infarction with signs of microvascular obstruction in the LAD territory involving the anteroseptal segments and the apical cap was noted. LAD = left anterior descending; MRI = magnetic resonance imaging.
2. Discussion
MINCA that has been known for >30 years has been reported substantially in the literature [3]. The underlying mechanisms are not known fully and multifactorial etiology makes MINCA patients complex.
A potential diagnosis in this case was allergic vasospasm. This patient has a history of bronchial asthma, nasal polyps, and documented allergy to nonsteroidal anti-inflammatory drugs (NSAIDs) [4].. The presence of extensive anterior ST elevation myocardial infarction based on ECG, transthoracic echocardiography and cardiac MRI, with normal coronary arteries on coronary angiography made the treating team consider Kounis syndrome [5], type 1 variant [6]. Clues that pointed towards this differential diagnosis were the temporal relationship between development of VF requiring resuscitation after receiving loading dose of aspirin; persistence of symptoms of light-headedness and episodes of hypotension on the 3rd day of admission with presyncope while on daily aspirin and receiving beta blockers; eosinophilia (8.3% [normal <6%]), elevated IgE (95.9 IU/mL [normal <100 IU/mL]), cessation of these symptoms after stopping medications that were reported to exacerbate Kounis syndrome and gradual improvement in overall condition after initiating corticosteroids, antihistamines, and leukotriene receptor antagonists.
In Kounis syndrome, one requirement is elevation of serum tryptase during the first few hours after presentation with MINCA, but unfortunately, in our case the blood was tested for serum tryptase >2 days later and the result was 5.0 µg/L (normal level <11.4 µg/L). It is known that serum tryptase returns to normal levels within 6–24 hours [7]. Kounis syndrome is an uncommon cause and will require further workup for accurate treatment.
Other differential diagnoses include microvascular obstruction, coronary vasospasm, spontaneously atherosclerotic plaque rupture, hypercoagulability, Takotsubo cardiomyopathy, and myocarditis. Apart from cardiac MRI that was suggestive of microvascular obstruction, all the cardiac workup did not support any of the other mentioned differential diagnosis. Prognosis of MINCA patients (with or without ST elevation) is better than that with obstructive coronary lesions [8], [9]. The most important factor influencing the prognosis of MINCA patients is left ventricular function [10].
Before discharge home, our patient had implantable cardioverter defibrillator (ICD) implanted for secondary prevention because of no clear underlying cause of his presentation (Fig. 8). We believe that Kounis syndrome causing allergic coronary vasospasm is dominant in the differential diagnosis in our case. In similar cases, early serum testing for tryptase level is recommended. We think that our case will help to raise awareness of Kounis syndrome as a possible cause of MINCA.
Figure 8.

Chest X-ray post ICD implantation. ICD = implantable cardioverter defibrillator.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Ammann P., Kraus M., Angehrn W., Rickli H., Marschall S., Schmid L. Characteristics and prognosis of myocardial infarction in patients with normal coronary arteries. Chest. 2000;117:333–338. doi: 10.1378/chest.117.2.333. [DOI] [PubMed] [Google Scholar]
- 2.Daniel M., Ekenback C., Agewall S., Brolin E.B., Caidahl K., Cederlund K. Risk factors and markers for myocardial infarction with angiographically normal coronary arteries. Am J Cardiol. 2015;116:838–844. doi: 10.1016/j.amjcard.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 3.Iuliano L., Micheletta F., Napoli A., Catalano C. Myocardial infarction with normal coronary arteries: a case report and review of the literature. J Med Case Rep. 2009;3:24. doi: 10.1186/1752-1947-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samter M., Beers Jr. R.F. Concerning the nature of intolerance to aspirin. J Allergy. 1967;40:281–293. doi: 10.1016/0021-8707(67)90076-7. [DOI] [PubMed] [Google Scholar]
- 5.Kounis N., Zavras G. Histamine-induced coronary artery spasm: The concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 6.Kounis N.G., Mazarakis A., Tsigkas G., Giannopoulos S., Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7:805–824. doi: 10.2217/fca.11.63. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz L.B., Yunginger Y.W., Miller J., Bokhari R., Dull D. Time course of appearance and disappearance of human mast cell tryptase in the circulation after anaphylaxis. J Clin Invest. 1989;83:1551–1555. doi: 10.1172/JCI114051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmar W., Lefkovits J. Acute ST elevation myocardial infarction with angiographically normal coronary arteries: causes and outcomes. Int J Cardiol. 2008;128:131–133. doi: 10.1016/j.ijcard.2007.05.053. [DOI] [PubMed] [Google Scholar]
- 9.Cortell A., Sanchis J., Bodí V., Núnez J., Mainar L., Pellicer M. Non-ST-elevation acute myocardial infarction with normal coronary arteries: predictors and prognosis. Rev Esp Cardiol. 2009;62:1260–1266. doi: 10.1016/s1885-5857(09)73353-5. [DOI] [PubMed] [Google Scholar]
- 10.Da Costa A., Isaaz K., Faure E., Mourot S., Cerisier A., Lamaud M. Clinical characteristics, aetiological factors, and long-term prognosis of myocardial infarction with an absolutely normal coronary angiogram; a 3-year follow-up study of 91 patients. Eur Heart J. 2001;22:1459–1465. doi: 10.1053/euhj.2000.2553. [DOI] [PubMed] [Google Scholar]







