Abstract
Background
Skin ageing especially senile lentigo directly affects self‐esteem. For decades, senile lentigo has been associated with chronic exposure to solar radiation. However, a study conducted recently in Caucasian subjects suggested that exposure to air pollution was significantly correlated with extrinsic skin ageing, in particular senile lentigines.
Objective
To investigate the association between fine particulate matter (PM 2.5) and skin ageing, particularly senile lentigo and seborrheic keratosis.
Methods
The study enrolled 400 Chinese women aged 40–90 years including 210 from the Yanqing county in Beijing (low PM 2.5 exposure group) and 190 from the Xuanwumen in Beijing (high PM 2.5 exposure group). Skin ageing symptoms, particularly senile lentigines and seborrheic keratoses, were clinically assessed using scores of intrinsic and extrinsic skin ageing. An ordinal logistic regression model was used to analyse the effect of PM 2.5 on skin ageing adjusted for factors underlying skin ageing.
Results
In the study population of Xuanwumen, we found that senile lentigo on cheeks and back of hands was 1.48 times and 2.8 times higher, respectively, compared with those from Yanqing county. However, no association was found between PM 2.5 and seborrheic keratosis. We found that other variables such as smoking, second‐hand smoking, contact with fossil fuels and skin types were significantly associated with skin ageing.
Conclusion
These results indicate that PM 2.5 was another extrinsic factor promoting skin ageing.
Introduction
Ageing of population is one of the most dynamic changes currently affecting our society. This phenomenon has led to a marked shift in the perception of people and an increased desire to improve their appearance, which directly impacts self‐esteem.1 Skin ageing includes extrinsic and intrinsic ageing. Currently, middle‐aged people and elderly increasingly seek treatment for signs of skin ageing, such as senile lentigines and seborrheic keratoses.
Senile lentigo, also called solar lentigo, lentigo senilis or age spot, is a pigmented macule on the face and back of hands. It is present in 90% of Caucasians older than 60 years, and is more prevalent among individuals with dark‐coloured skin. It is believed that solar radiation is an important pathogenic factor underlying the development of senile lentigo. Seborrheic keratosis (SK) is also a common problem in Asians, which is observed in 80% to 100% of population aged over 50 years.2 Among Chinese, most SKs are brown to dark brown. However, SK is not a pigment disorder, but rather a benign neoplasm.
Millions of people worldwide are exposed to fine particulate matter (PM2.5), which is associated with adverse effects on health including a high risk for cancer, pulmonary and cardiovascular diseases.3 Most recently, a study conducted in Germany suggested that exposure to air pollution was significantly correlated with extrinsic skin ageing, in particular, senile lentigines in Caucasian subjects. Until now, no study reported the association between airborne particles and skin ageing in Asian populations, predominantly characterized by the development of senile lentigines.3 Chinese skin is believed to be more sensitive to chemical stimuli. Therefore, we hypothesized that age‐related changes in skin pigmentation correlated with air pollution were predominantly seen in Chinese than in Caucasians.
In this study, we investigated the association between PM2.5 exposure and different signs of ageing including senile lentigo and seborrheic keratosis in a cross‐sectional study using a cohort of Chinese women in two independent study populations aged 40~90 years in Beijing.
Materials and methods
Study design and study populations
We selected the study areas of Xuanwumen and Yanqing county based on the pollution data collected by the Beijing Environmental Protection Monitoring Center. Xuanwumen is located in a highly polluted downtown area. Conversely, Yanqing county is one of the Ecological Development Zones of Beijing, which is scarcely exposed to urban pollution. Over the last decades, the average level of PM2.5 in Xuanwumen was 168.13 μg/m3, representing a high PM2.5 exposure area. By contrast, the level in Yanqing county was 63.56 μg/m3, representing the low PM2.5 exposure area. The average PM2.5 value over the last decades in areas of Beijing is shown in Fig. 1.
Figure 1.
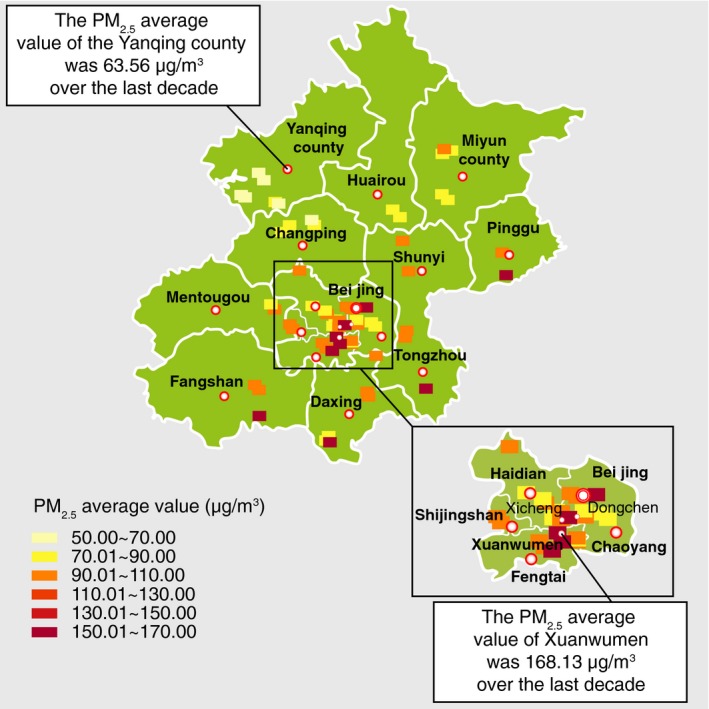
The average PM 2.5 values over the past decades in a few areas of Beijing monitored by the Beijing Environmental Protection Monitoring Center.
All the women volunteers were recruited from the two local communities. The inclusion criteria were as follows: (i) Han Chinese women; (ii) age 40–90 years; and (iii) individuals with at least 10 years of residence at their current address, which was less than 10 km away from the air pollution monitoring station. The volunteers filled the questionnaire under the guidance of dermatologist, and the skin ageing score was completed by a well‐trained dermatologist. A total of 400 women were recruited between March and June 2015. They included 210 from Yanqing county and 190 from Xuanwumen. The Medical Ethics Committee of the Peking University People's Hospital, China approved the study. The study was conducted in accordance with the Declaration of Helsinki and all the study participants provided written informed consent.
Assessment of skin ageing and co‐variables
Skin ageing including the combined influence of intrinsic and extrinsic factors, is reflected by various clinical signs. Skin ageing signs were evaluated on the basis of a validated skin ageing score called Score of Intrinsic and Extrinsic Skin Ageing (SCINEXA), with slight modification (Fig. 2).
Figure 2.
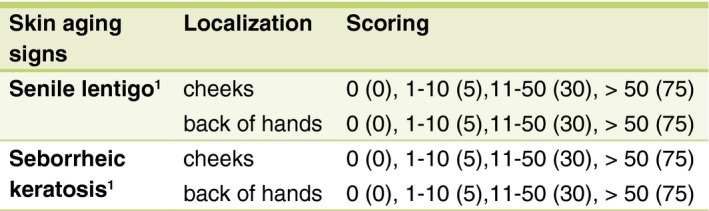
Skin ageing analysis based on SCINEXA scores.
The senile lentigo is a sharply but irregularly pigmented macule varying in colour from yellow‐brown to dark brown. Its size may range from a few millimetres to several centimetres. The typical SK is a well demarcated and elevated papule ranging from flesh to brownish or blackish colour. Most senile lentigines and SKs were diagnosed clinically. Atypical senile lentigines and SKs were diagnosed with a dermatoscope or histopathologically. A value of 0 was assigned if there were no signs, 5 indicated 1–10 spots, 30 represented 11–50 spots and 75 indicated more than 50 spots or seborrheic keratoses.
Demographic data and environmental exposure influenced skin ageing. Factors include age, work environment (indoor/outdoor), education (less than 10 years or more than 10 years), spouse (married or unmarried), history of hormone replacement therapy (yes/no), UV exposure (average hours of outdoor activities per day), sunburn history, sunbed and sunscreen use, smoking history including second‐hand smoking, daily fossil fuel contact in the past decade (yes/no), occupational exposure to toxic and harmful substances (yes/no) and skin type according to Fitzpatrick (1988). These data were collected using questionnaires, which were completed by a well‐trained dermatologist.
Statistical analysis
Qualitative variables were expressed in N (%), quantitative variables in mean (standard deviation SD) or median (25th to 75th percentiles as appropriate). Pearson chi‐squared tests or Fisher's exact tests were used for comparison of categorical variables. Variables not normally distributed were analysed using t‐test and Mann–Whitney U‐test.
An ordinal logistic regression model was used to determine whether the skin ageing symptoms were related to exposure to PM2.5. Coefficients of the variables were determined using adjusted odds ratios (OR) with 95% confidence intervals (CI).
The mutually adjusted association was defined as significant if P < 0.05. Statistical analysis was carried out using spss 22.0 (IBM SPSS, Armonk, NY, USA).
Results
Baseline population demographics
Table 1 provides a description of all the relevant data of the study subjects separately for the Yanqing county and Xuanwumen. All the data derived from the two groups were completely analysed. A total of 210 persons in the Yanqing group and 190 in the Xuanwu group were analysed. All the women were aged between 40 and 90 years. The women from Yanqing were slightly younger (median age = 54.5 years) than the women from Xuanwu (median age = 62 years). Approximately half of the women from Yanqing worked outdoors, and nearly all the women from Xuanwu worked indoors. About 51.4% of the women from Yanqing and 33.7% of the women from Xuanwu had less than 10 years of education, indicating a worse social status in the Yanqing group. Nearly all the women lived with their spouses. Hormone replacement therapy (HRT) was used by 18.6% of the women from Yanqing and by 3.7% from Xuanwu. Based on the average number of hours spent in outdoor activities daily, we considered that all the women received moderate sun exposure. Only a few individuals had a sunburn history or used sunbeds. About 32.5% of the women used sunscreen in their daily life, indicating that they were less likely to engage in protection against UV exposure. Nearly all the women were non‐smokers. A higher number of women had a passive smoking history in the Yanqing group than in the Xuanwu group. A majority of the women in Yanqing (95.7%) and Xuanwu (84.2%) used fossil fuels for cooking. Most individuals were not exposed to toxic or harmful substances at work. All the women had skin types III and IV according to the Fitzpatrick scale. There were significant differences in age distribution, work environment, educational levels, marital status, HRT, sunbed use, second‐hand smoking, fossil fuel exposure and skin types.
Table 1.
Characteristics of study population
| Sample size | N | Low PM2.5 district (63.56 μg/m3) 210 | High PM2.5 district (168.13 μg/m3) 190 | P |
|---|---|---|---|---|
| Age | Mean ± SD (range) | 62.5 ± 22.5 | 63.5 ± 23.5 | *0.000 |
|
Work environment Indoor Outdoor Neither |
Yes% (n) |
56.2 (118) 35.2 (74) 8.6 (18) |
90.0 (171) 8.9 (17) 1.1 (2) |
*0.000 |
| Education (<10 years) | Yes% (n) | 51.4 (108) | 33.7 (64) | *0.001 |
| Spouse | Yes% (n) | 88.1 (185) | 78.4 (149) | *0.009 |
| HRT | Yes% (n) | 18.6 (39) | 3.7 (7) | *0.000 |
| Outdoor activities (hours) |
Mean ± SD (range) |
6 ± 6 | 4.5 ± 4.5 | 0.686 |
| Sunburn history | Yes% (n) | 13.8(29) | 20.0(38) | 0.098 |
| Sunscreen use | Yes% (n) | 34.3 (72) | 30.5 (58) | 0.423 |
| Sunbed use | Yes% (n) | 18.1 (38) | 41.6 (79) | *0.000 |
| Smoking | Yes% (n) | 1.9 (4) | 4.7 (9) | 0.111 |
| Second‐hand smoking | Yes% (n) | 46.2 (97) | 31.1 (59) | *0.002 |
| Fossil fuels contact times (hours per day) |
Yes% (n) mean ± SD (range) |
95.7 (201) 3 ± 2 |
84.2 (160) 3.5 ± 2.5 |
*0.000 |
| OETHS | Yes% (n) | 5.2 (11) | 7.4 (14) | 0.379 |
|
Fitzpatrick skin type III IV |
Yes% (n) Yes% (n) |
54.3 (114) 45.7 (96) |
30.0 (57) 70.7 (133) |
*0.000 |
HRT, hormone replacement therapy; FFC, fossil fuels contact; OETHS, occupations exposed to toxic and harmful substances; M, median.*Values significant if P < 0.05.
Skin ageing
Skin ageing was assessed by a slight modification of SCINEXA. Ageing scores in the Yanqing county and the Xuanwumen study populations are shown separately in Table 2.
Table 2.
Skin ageing symptoms
| Sample size |
Low PM2.5 district (63.56 μg/m3)
n = 210 |
High PM2.5 district
(168.13 μg/m3) n = 190 |
P | |
|---|---|---|---|---|
| Senile lentigo | ||||
|
On cheeks
0 (0) 5 (1–10) 30 (11–50) 75 (>50) |
Yes% (n) |
21.4 (45) 55.7 (117) 21.4 (45) 1.4 (3) |
6.3 (12) 93 (48.9) 82 (43.2) 1.6 (3) |
*0.000 |
|
On back of hands
0 (0) 5 (1–10) 30 (11–50) 75 (>50) |
Yes% (n) |
33.8 (71) 53.8 (113) 12.4 (26) 0 |
14.7 (28) 52.6 (100) 31.1 (59) 1.6 (3) |
*0.000 |
| Seborrheic keratosis | ||||
|
On cheeks
0 (0) 5 (1–10) 30 (11–50) |
Yes% (n) |
81.4 (171) 18.1 (38) 0.5 (1) |
60.5 (115) 34.7 (66) 4.7 (9) |
*0.000 |
|
On back of hands
0 (0) 5 (1–10) 30 (11–50) 75 (>50) |
Yes% (n) |
86.2 (181) 13.8 (29) 0 0 |
74.7 (142) 22.6 (43) 2.1 (4) 0.5 (1) |
*0.003 |
Chi‐squared test for binary variables and t‐test for continuous variables. *Values significant if P < 0.05.
Association between PM2.5 exposure and skin ageing
PM2.5 was significantly associated with senile lentigines on cheeks and on the back of hands in the ordinal logistic regression model. However, no association existed between PM2.5 and seborrheic keratoses. All the adjusted odds ratios (OR) are listed in Table 3. The association between skin ageing and multiple variables, including PM2.5, are shown separately for the Yanqing county (low PM2.5 district). Among the study population of Xuanwumen, we found 1.48 and 2.8 times higher number of spots on cheeks and back of hands, respectively, compared with the study population of Yanqing county. PM2.5 was significantly associated with more severe senile lentigo.
Table 3.
Association between PM2.5 and skin ageing signs use ordinal logistical regression. (significant association with P < 0.05)
| Senile lentigo | Seborrheic keratosis | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| On cheeks | On back of hands | On cheeks | On back of hands | |||||||||||||
| B | OR1 | 95% CI | P | B | OR1 | 95% CI | P | B | OR1 | 95% CI | P | B | OR1 | 95% CI | P | |
| Yanqing (low PM2.5) | −0.91 | 0.403 | 0.239, 0.679 | 0.001* | −1.337 | 0.263 | 0.156, 0.441 | 0.000* | −0.469 | 0.626 | 0.334, 1.174 | 0.144 | 0.079 | 1.082 | 0.53, 2.209 | 0.828 |
| Age | 0.064 | 1.006 | 1.038, 1.095 | 0.000* | −0.009 | 0.991 | 0.967, 1.016 | 0.482 | 0.034 | 1.035 | 1.004, 1.067 | 0.025* | 0.021 | 1.021 | 0.986, 1.059 | 0.244 |
| Work environment | 0.012 | 1.013 | 0.584, 1.754 | 0.964 | −0.723 | 0.485 | 0.282, 0.835 | 0.009* | 0.438 | 1.549 | 0.764, 3.144 | 0.225 | 0.02 | 1.02 | 0.463, 2.245 | 0.961 |
| Education level <10 years | 0.06 | 1.061 | 0.584, 1.928 | 0.845 | 0.172 | 1.188 | 0.660, 2.138 | 0.565 | 0.689 | 1.991 | 0.978, 4.055 | 0.058 | 0.226 | 1.253 | 0.571, 2.753 | 0.574 |
| Have spouse | 0.001 | 1.001 | 0.541, 1.853 | 0.997 | 0.033 | 1.033 | 0.566, 1.888 | 0.915 | −0.147 | 0.863 | 0.441, 1.690 | 0.668 | 0.32 | 1.377 | 0.612, 3.097 | 0.44 |
| HRT = yes | 0.082 | 1.086 | 0.554, 2.128 | 0.811 | 0.053 | 1.054 | 0.536, 2.073 | 0.878 | −0.138 | 0.871 | 0.378, 2.006 | 0.745 | −0.109 | 0.897 | 0.352, 2.281 | 0.819 |
| Sunburn history = yes | 0.185 | 1.203 | 0.691, 2.092 | 0.513 | −0.54 | 0.583 | 0.336, 1.009 | 0.054 | −0.661 | 0.516 | 0.240, 1.109 | 0.09 | −0.207 | 0.813 | 0.367, 1.8 | 0.61 |
| Sunscreen use = yes | −0.326 | 0.722 | 0.448, 1.163 | 0.181 | −0.21 | 0.811 | 0.512, 1.283 | 0.37 | −0.007 | 0.993 | 0.547, 1.803 | 0.981 | 0.401 | 1.493 | 0.784, 2.844 | 0.223 |
| Outdoor activities time | 0.025 | 1.025 | 0.919, 1.143 | 0.181 | −0.06 | 0.942 | 0.848, 1.047 | 0.267 | −0.083 | 0.92 | 0.795, 1.064 | 0.261 | 0.011 | 1.011 | 0.87, 1.174 | 0.885 |
| Smoking = yes | 0.202 | 1.224 | 0.762, 1.996 | 0.404 | 0.286 | 1.331 | 0.841, 2.107 | 0.222 | 1.004 | 2.729 | 1.585, 4.7 | 0.000* | 1.015 | 2.758 | 1.528, 4.981 | 0.001* |
| Second‐hand smoking = yes | 0.579 | 1.784 | 1.145, 2.781 | 0.011* | 0.012 | 1.012 | 0.656, 1.560 | 0.958 | 0.016 | 1.016 | 0.598, 1.726 | 0.952 | 0.85 | 2.341 | 1.288, 4.254 | 0.005* |
| FFC = yes | 0.858 | 2.358 | 1.152, 4.825 | 0.019* | 0.658 | 1.932 | 0.983, 3.794 | 0.056 | 0.091 | 1.095 | 0.494, 2.429 | 0.823 | −0.021 | 0.98 | 0.405, 2.367 | 0.963 |
| OETHS = yes | −0.116 | 0.891 | 0.391, 2.029 | 0.783 | 0.678 | 1.969 | 0.888, 4.367 | 0.095 | 0.72 | 2.053 | 0.837, 5.035 | 0.116 | 0.51 | 1.666 | 0.637, 4.353 | 0.298 |
| Skin type III | −0.686 | 0.504 | 0.324, 0.782 | 0.002* | −0.06 | 0.942 | 0.617, 1.439 | 0.783 | −0.3 | 0.741 | 0.435, 1.263 | 0.271 | −0.112 | 0.894 | 0.496, 1.611 | 0.71 |
FFC, fossil fuels contact; HRT, hormone replacement therapy; OETHS, occupations exposed to toxic and harmful substances. *Values significant if P < 0.05.
Among the other variables associated with skin ageing, we found that second‐hand smoking (OR = 1.784) and contact with fossil fuels (OR = 2.357) were associated with a higher number of spots on cheeks. Females with skin type III manifested significantly fewer spots on cheeks (OR = 0.504) compared with skin type IV. Working indoors was associated with less spots on the hands (OR = 0.485). Smoking was strongly associated with seborrheic keratoses on both cheeks (OR = 2.729) and back of hands (OR = 2.758). Second‐hand smoking was associated with seborrheic keratosis on hands (OR = 2.341). Age increased the risk of spots by 0.6% on cheeks, and seborrheic keratoses by 3.5% on cheeks and 2.1% on the back of hands with every additional year.
Discussion
We found a strong association between PM2.5 and senile lentigo. Ultraviolet radiation (UVR) contributes to the formation of acquired senile lentigo in human skin.4 We defined senile lentigo results following chronic exposure to a variety of environmental factors including UVR, particulate and possibly gaseous constituents of ambient air pollution. Asians generally avoid sun exposure. Photodamage due to chronic sun exposure was greatly reduced in Asian skin. However, Asians develop senile lentigo much earlier than age‐matched Caucasians,5 suggesting that sun exposure is not the only causative factor for the development of senile lentigo. Senile lentigo is due to an increase in the melanin content inside keratinocytes, and may or may not be associated with melanocytic hyperplasia. It is a type of pigment spot, but differs from Chloasma and freckles. Vierkötter et al.3 found that a distance of 100 m or less from a busy road was associated with 35% more senile lentigo on forehead and 15% more senile lentigo on cheeks. However, the difference was not significant.
Organic compounds present on the surface of PM may penetrate the skin and directly affect viable skin cells such as keratinocytes and melanocytes. In barrier‐deficient skin and skin wounds, particles may cause oxidative stress and skin inflammation.6, 7 In the lung, particulate matter (PM) generates reactive oxygen species. Whether this is also true for skin cells is currently unknown. It should be noted, however, that these particles carry organic chemicals such as polyaromatic hydrocarbons (PAH), which are highly lipophilic and easily penetrate the skin.6 We believe that both UVR and PAH‐loaded particles activate Aryl hydrocarbon receptor (AHR) in human skin and thereby contribute to lentigo. Notably, recent studies demonstrate that AHR activation in skin cells induced skin pigmentation.5 UVR exposure of AHR‐deficient mice causes significantly weaker pigmentation compared with that in the wild‐type mice. The difference is probably due to decreased melanocyte proliferation.8 AHR signalling in skin cells is important for skin pigmentation. Further, studies suggested that the effects of air pollutants might be amplified in the presence of other air pollutants in conjunction with UVR.9
Seborrheic keratosis is a benign, hyperplastic pigmentation of the epidermis and represents the most common cutaneous neoplasm.10 Seborrheic keratosis is one of the most common dermatologic lesions. Despite the high prevalence of SK, its aetiology and pathogenesis are poorly understood.11 Individuals with SKs generally have a positive family history for the condition.12 Exposure to sunlight increases the risk for SKs.2 Friction may also play a role in SK development.11 Though SKs appear more frequently on areas exposed to sun, lesions may also occur on any site of the skin except palms or soles, which are not sun‐exposed.2, 9, 10 Viral infection is also considered a possible cause of SKs based on clinical similarities to warts.2
The evidence indicates that SK is probably caused by intrinsic factors. Intrinsic ageing of the skin occurs naturally due to physiological changes over time at variable but genetically pre‐determined rates.13 Hormone replacement substantially reverses some of the intrinsic effects.14 Our study found that women undergoing hormone replacement therapy showed a lower incidence of seborrheic keratosis on cheeks and the back of hands. However, it was not significant, due to the small sample size.
In this study, we found that various factors contribute to skin ageing. All the variables were analysed in a multivariate statistical model. We observed that skin type III was associated with limited senile lentigo, consistent with previous reports suggesting that light skin type showed different features of extrinsic skin ageing than darker skin types. The light skin type was more likely to show wrinkles and elastosis, and the darker skin type was associated with senile lentigo. Second‐hand smoking history was associated with senile lentigo on the cheeks. An earlier study found that rats exposed to second‐hand smoke showed diminished collagen formation and high mobility group box 1 expression resulting in prematurely aged skin.15 In our study, we also found that smoking was associated with seborrheic keratosis. The ‘smoker's face’ refers to a face with lines or wrinkles typically radiating at right angles from the upper and lower lips or corners of the eyes.16 Until now, no data correlating smoking with seborrheic keratosis have been published. A mechanistic study is required to determine the relative contribution of smoking to seborrheic keratosis. A previous epidemiological study of Chinese people showed that cooking with solid fuels was significantly associated with severe coarse wrinkles, pronounced laxity and occurrence of fine wrinkles.17 Our study investigated whether cooking with fossil fuels was associated with senile lentigo on cheeks. Women who worked indoors showed minimal senile lentigo on the back of their hands compared with women working outdoors. It is yet to be established if outdoor work often entails manual labour.
To the best of our knowledge, this is the first study showing an association between PM2.5 exposure and development of senile lentigines in a Han Chinese population. Our investigation into Chinese ancestry enhances our understanding of the impact of environmental pollution on skin ageing, especially on senile lentigo formation. This study provides prospective new data advocating the importance of skin care, particularly the use of deep facial cleansing to remove dust from the skin completely and thoroughly. The use of protective cosmetics that include sunscreen and antioxidants should also be stressed, to combat the oxidative stress induced by PM2.5.
Acknowledgements
We express our sincere gratitude to the following: Prof. Dr. Robert Schwartz from Rutgers New Jersey Medical School who improved the manuscript, and Huixin‐Liu from Peking University People's Hospital for assistance with statistical methods and Shang‐ling Li and Wen‐zheng Liu who assisted with figures and tables.
Conflicts of interest
None declared.
Funding sources
This study was supported by the Chinese Medical Association ‐Vichy Research Project Grant No. 2119000206 and the National Natural Science Foundation of China (Grant No. 81472902).
The copyright line for this article was changed on 27 July 2018 after original online publication.
References
- 1. Vierkötter A, Ranft U, Krämer U et al The SCINEXA: a novel, validated score to simultaneously assess and differentiate between intrinsic and extrinsic skin ageing. J Dermatol Sci 2009; 53: 207–211. [DOI] [PubMed] [Google Scholar]
- 2. Chung JH. Photoaging in Asians. Photodermatol Photoimmunol Photomed 2003; 19: 109–121. [DOI] [PubMed] [Google Scholar]
- 3. Vierkötter A, Schikowski T, Ranft U et al Airborne particle exposure and extrinsic skin aging. J Invest Dermatol 2010; 130: 2719–2726. [DOI] [PubMed] [Google Scholar]
- 4. Flament F, Bazin R, Laquieze S et al Effect of the sun on visible clinical signs of aging in Caucasian skin. Clin Cosmet Investig Dermatol 2013; 6: 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nakamura M, Morita A, Seité S et al Environment‐induced lentigines: formation of solar lentigines beyond ultraviolet radiation. Exp Dermatol 2015; 24: 407–411. [DOI] [PubMed] [Google Scholar]
- 6. Krutmann J, Liu W, Li L et al Pollution and skin: from epidemiological and mechanistic studies to clinical implications. J Dermatol Sci 2014; 76: 163–168. [DOI] [PubMed] [Google Scholar]
- 7. Burke KE, Wei H. Synergistic damage by UVA radiation and pollutants. Toxicol Ind Health 2009; 25: 219–224. [DOI] [PubMed] [Google Scholar]
- 8. Jux B, Kadow S, Luecke S et al The aryl hydrocarbon receptor mediates UVB radiation–induced skin tanning. J Invest Dermatol 2011; 131: 203–210. [DOI] [PubMed] [Google Scholar]
- 9. Drakaki E, Dessinioti C, Antoniou CV. Air pollution and the skin. Front Environ Sci 2014; 2: 11. [Google Scholar]
- 10. Gaballah MA, Ahmed RA. Diagnostic value of CD10 and Bcl2 expression in distinguishing cutaneous basal cell carcinoma from squamous cell carcinoma and seborrheic keratosis. Pathol Res Pract 2015; 211: 931–938. [DOI] [PubMed] [Google Scholar]
- 11. Jackson JM, Alexis A, Berman B et al Current Understanding of Seborrheic Keratosis: Prevalence, Etiology, Clinical Presentation, Diagnosis, and Management. J Drugs Dermatol 2015; 14: 1119–1125. [PubMed] [Google Scholar]
- 12. Wolff K, Goldsmith LA, Katz SI et al Fitzpatrick's dermatology in general medicine, 2 Volumes[J]. Transplantation, 2008, 85(654). [Google Scholar]
- 13. Farage MA, Miller KW, Elsner P et al Intrinsic and extrinsic factors in skin ageing: a review. Int J Cosmet Sci 2008; 30: 87–95. [DOI] [PubMed] [Google Scholar]
- 14. Farage MA, Miller KW, Elsner P et al Functional and physiological characteristics of the aging skin. Aging Clin Exp Res 2008; 20: 195–200. [DOI] [PubMed] [Google Scholar]
- 15. Chaichalotornkul S, Nararatwanchai T, Narkpinit S et al Secondhand smoke exposure‐induced nucleocytoplasmic shuttling of HMGB1 in a rat premature skin aging model. Biochem Biophys Res Commun 2015; 456: 92–97. [DOI] [PubMed] [Google Scholar]
- 16. Morita A. Tobacco smoke causes premature skin aging. J Dermatol Sci 2007; 48: 169–175. [DOI] [PubMed] [Google Scholar]
- 17. Li M, Vierkötter A, Schikowski T et al Epidemiological evidence that indoor air pollution from cooking with solid fuels accelerates skin aging in Chinese women. J Dermatol Sci 2015; 79: 148–154. [DOI] [PubMed] [Google Scholar]


