Abstract
Background
The treatment options for pseudogynecomastia have been limited. Cold‐induced lipolysis provides a noninvasive, localized subcutaneous adipocyte destruction by inducing adipocyte apoptosis.
Objective
This study has been designed to evaluate the efficacy of cold‐induced lipolysis as a treatment modality for pseudogynecomastia.
Methods
In this 28‐week prospective trial, a total of 12 male pseudogynecomastia patients (Korean) were treated twice with cold‐induced lipolysis. Efficacy was determined by chest circumference, ultrasonographic measurement of fat thickness, Simon's Gynecomastia class (SGC), photographic assessment, and the patient's satisfaction (baseline, weeks 4, 8, 16, and 28). Using a questionnaire, safety was evaluated at each visit.
Results
For 10 subjects that completed the trial, chest circumference and fat thickness significantly improved by week 8. This same improvement was gradually noticed through week 28. The patients SGC scores continuously decreased after two sessions. Photographic assessment showed an improvement until week 28. The result of the patient's satisfaction score was also meaningful. While there were no adverse events observed, transient pain and bruising at the treatment site were noticed.
Limitations
We recruited a limited number of participants. Also, we could not exclude there might be other individual factors in association with the patients pseudogynecomastia.
Conclusion
Cold‐induced lipolysis is a safe, effective therapeutic option in the treatment of pseudogynecomastia. Lasers Surg. Med. 48:584–589, 2016. © 2016 The Authors. Lasers in Surgery and Medicine Published by Wiley Periodicals Inc.
Keywords: pseudogynecomastia, lipolysis, cold‐induced lipolysis, fat destruction
ABBREVIATIONS
- SGC
Simon's Gynecomastia class
- PAH
Paradoxical adipose hyperplasia
INTRODUCTION
Gynecomastia is defined as benign proliferation of the mammary gland tissue or adipose tissue in male breasts 1, 2. While this is typically an idiopathic condition, it can also be caused by the following: hormonal imbalance, endocrinologic disease, tumorous conditions, prescription drugs, and medications (such as spironolactone) 3. The prevalence rate of gynecomastia is unknown, as there is no standard diagnostic criteria. However, it has become a matter of common interest in South Korea's cosmetic field. Adolescent gynecomastia is known as a physiologic condition and has a natural progression. Since adult gynecomastia (pseudogynecomastia) cannot be improved spontaneously, invasive techniques such as surgical excision or liposuction are commonly used. However, the demand for noninvasive treatment options is increasing; and this may be due to the many factors that invasive surgeries pose (risk from general anesthesia, prolonged recovery period, high cost, and etc.).
Many noninvasive treatment options, such as high‐intensity focused ultrasound (HIFU), radiofrequency ablation, low‐level external laser therapy, injection lipolysis, low‐intensity nonthermal ultrasound, and cold‐induced lipolysis 4 are being discussed as potential modes of treatment. Among them, regardless of its effectiveness, cold‐induced lipolysis technique has been approved by the Food and Drug Administration of the Unites States (for treating excessive fat in the abdomen, flanks, thighs, and submental space) and is just as safe as the other aforementioned treatments. Until now this method was mainly used for abdominal or thigh fat pad treatment 5. Yet, during this study we used the cold‐induced lipolysis method for male gynecomastia to evaluate its efficacy and safety. When previous studies evaluated the effectiveness of a treatment method, only subjective evaluations, such as photographic assessment, were utilized. However, in this study, we tried to be more objective when proving the effectiveness of cold‐induced lipolysis by measuring both the chest circumference and thickness of fat tissue. Through this study we suggest a transition from the traditional invasive treatment modality to a brand new, noninvasive treatment option with the ability to selectively destruct the adipose tissue.
PATIENTS AND METHODS
Study Design
A total of 12 male patients (Korean), who were over 25 years of age and diagnosed with adult pseudogynecomastia, were enrolled in this prospective and nonrandomized clinical trial. This study was approved by the Institutional Review Board (IRB) at our institution, and a consent form was obtained from each participating patient. The following patients were excluded: patients who did not want to be included in this study, those who did not provide consent, those who received surgical excision or liposuction of the breast within the last 6 months, those who were considered to be in the high‐risk group for cold‐induced lipolysis method (such as cryoglobulinemia, cold urticaria, and paroxysmal cold hemoglobulinemia), those who have gynecomastia by endocrinologic disease (such as hypogonadism, hyperthyroidism, pituitary gland disease, male breast cancer, testicular cancer, adrenal gland cancer), those who had inflammatory dermatoses (open wound, or active herpes simplex at the treatment site), and those who were judged to be inappropriate for this study by the researchers.
Patient Characteristics
Twelve patients with pseudogynecomastia were recruited for this study. Ten patients successfully completed this study, while two were excluded for personal reasons. All participants were Korean males with Fitzpatrick's skin types of III and IV, and the average age was 36.4 years (ranging from 25 to 40).
Procedure
In this study, we used a cold‐induced treatment device named MiCool™ by Hironic Co., Ltd. (Seongnam, Korea). For each patient we applied this machine on both sub‐areolar areas for a duration of 1 hour (on “massage mode”). (We attached a schematic picture to help understand this device, Fig. 1). This “1‐hour massage mode” included a cryo‐energy treatment for 45 minutes, which used a cooling intensity factor (CIF) of 33 (−64 mW/cm2), and a massage for 15 minutes. After 4 weeks another treatment was done with the same conditions. Overall a total of two treatment sessions were conducted for each patient (with a follow‐up at 8, 16, and 28 weeks). At the final follow‐up (28th week), we performed an optional treatment to the breast or other area upon patient's request.
Figure 1.
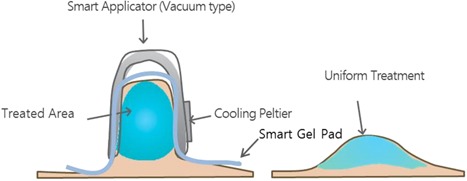
Scheme of smart applicator and targeted area by MiCool. Vacuum type smart applicator pinch sub‐areolar area and transmit cryo‐energy by defined parameter. (Scheme provided by Hironic Co., Ltd., Seongnam, Korea.)
Evaluations
Efficacies were evaluated at baseline, 4, 8, 16, and 28 weeks based on the following fixed criteria: chest circumference, ultrasonographic subcutaneous fat thickness, Simon's Gynecomastia class (SGC), physician's global photographic assessment, and patient's satisfaction. Safety profiles were also evaluated by a questionnaire. The primary endpoint of this study was chest circumference. On each visit we measured the circumference of the entire chest wall (just below the areolar area) with a tapeline. We took three measurements to calculate the average and perform a statistical analysis. Additionally, in the same area we measured the thickness of subcutaneous fat tissue by an ultrasonography (SONOACE X8, Samsung Medison Co., Ltd., Seoul, Korea) and carried out a statistical analysis. We performed a paired t‐test by comparing the averages from each visit.
On every visit, one independent dermatologist performed the grading by SGC (Table 1), and analyzed the tendency of the grade change by a generalized linear model.
Table 1.
Simon's Gynecomastia Class
| Grade 1: Small enlargement, no skin excess |
| Grade 2a: Moderate enlargement, no skin excess |
| Grade 2b: Moderate enlargement with extra skin |
| Grade 3: Marked enlargement with extra skin |
We took pictures of the three axes (front, left, right) each time under the same conditions, which were standardized brightness and distance by a digital camera. These pictures were then used for photographic assessments by two independent dermatologists. The evaluation criteria was divided into five grades: 0 (no interval change, 0%), 1 (minimal improvement, 1–24%), 2 (mild improvement, 25–49%), 3 (moderate improvement, 50–74%), and 4 (marked improvement, 75–100%). The patient's satisfaction score was evaluated at each visit via questionnaire using the following five scores: aggravated (1), not improved (2), a little bit improved (3), somewhat improved (4), and much improved (5).
Statistical Analysis
A statistical analysis was done using Microsoft Excel and SPSS version 20.0 by IBM, Chicago, Illinois, USA (statistical program). We performed a paired t‐test and used a generalized linear model for the data given at baseline and each subsequent visit. A P‐value of less than 0.05 was considered to be statistically significant.
Adverse Effects
Patients were educated about reporting adverse events anytime during and after the treatment, in addition to filling out a questionnaire about possible adverse effects. Moreover, we examined for adverse effects at each visit. Both kinds of examinations for adverse effects were based on the safety profiles (which includes the manifestation period, degree, and results of the adverse effect(s)).
RESULTS
Chest Circumference
For 10 of the patients, the average chest circumference (cm) at baseline, 4, 8, 16, and 28 weeks was 100.02, 98.13, 96.77, 95.72, and 96.15, respectively. The average chest circumference gradually decreased until week 16 with a statistical significance (P < 0.05), while it slightly increased at week 28 (Fig. 2). However, when each value was compared with the initial baseline value, all showed a statistically significant reduction (P < 0.05).
Figure 2.
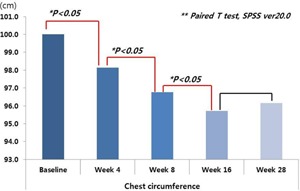
Average chest circumference at each visit. Chest circumference showed gradual decrease until week 16, which slightly increased at week 28.
Ultrasonographic Evaluation of Subcutaneous Fat Thickness
The average thickness (cm) of the left subcutaneous fat at baseline, 4, 8, 16, and 28 weeks was 1.70, 1.51, 1.41, 1.31, and 1.29, respectively (Fig. 3). Furthermore, the average value of the right side was 1.67, 1.53, 1.40, 1.34, and 1.26, respectively. After the first session of cold‐induced lipolysis (at week 4), the average thickness remarkably decreased with statistical significance (P < 0.05). Although some values were not statistically significant, ultrasonographic fat thickness of both sides of the breast continuously decreased throughout the entire period after two cycles of cold‐induced lipolysis (Fig. 4).
Figure 3.
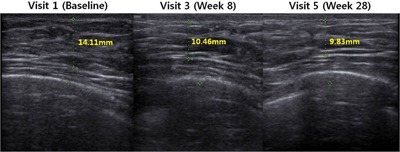
One sample patient's subcutaneous fat thickness measured by ultrasonograph. Dotted line is measured fat thickness, showing a gradual decrease each visit.
Figure 4.
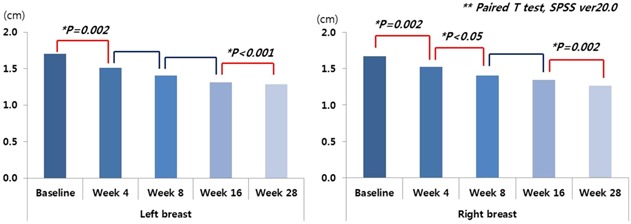
Average of subcutaneous fat thickness. Ultrasonographic fat thickness of both sides of the breast was continuously decreased after two cycles of cold‐induced lipolysis.
SGC
At each visit a physician performed the grading with SGC, and the average of each value was 2.10, 2.00, 1.80, 1.60, and 1.40. We analyzed the average of each visit's SGC by a generalized linear model. SGC scores continuously decreased after two sessions of cold‐induced lipolysis with statistical significance (Fig. 5; P = 0.003).
Figure 5.
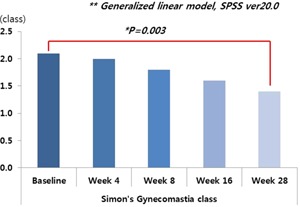
Tendency of Simon's Gynecomastia class (SGC) score. SGC scores were continuously decreased after two sessions of cold‐induced lipolysis.
Global Photographic Assessment and Patient's Satisfaction
Based on the evaluation criteria mentioned above, we scored each grade and calculated the average of the tendency. Although there were conflicting opinions regarding the degree of improvement at week 28, on the average improvement continuously increased throughout the whole period. The average patient satisfaction at weeks 4, 8, 16, and 28 was 3.4, 3.8, 3.2, and 3.4, respectively. All of these values were greater than the score of 3, while peeking at week 8 with a score of 3.8 (Fig. 6).
Figure 6.
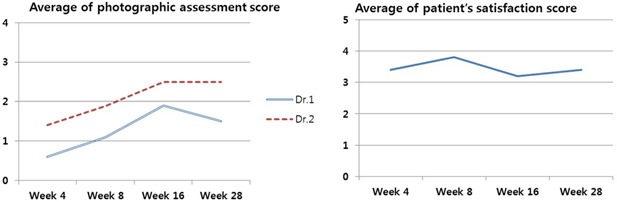
Average of photographic assessment score and average of patient's satisfaction score. The average of improvement tendency was continuously increased during the whole period. Also, patient's satisfaction score is over 3 during the whole period.
Safety Assessment
Except for transient pain and bruising after each session of cold‐induced lipolysis, there were no adverse side effects shown or reported by patients. In addition, none of the patients showed paradoxical adipose hyperplasia (PAH) during the whole period.
DISCUSSION
Gynecomastia is defined as a benign proliferation of the adipose tissue or mammary gland tissue in male breasts. This may occur as a result of an adolescence's physiologic change, but may also arise as a result of a hormonal disturbance, drug side effect or endocrinologic disease. While true gynecomastia is associated with the proliferation of the mammary gland tissue, pseudogynecomastia is associated with the accumulation of the adipose tissue. There is a limitation on the treatment options for patients with pseudogynecomastia. Recently, pseudogynecomastia has increasingly become a cosmetic problem, especially with regard to weight reduction. The mainstream treatment option still remains to be invasive (such as surgical excision and liposuction). However, there are a few reports regarding the associated complications with invasive treatments, such as mortality from fat embolism. Therefore, there is a growing need to introduce a noninvasive technique for treating gynecomastia.
There are various kinds of noninvasive techniques. One is the cold‐induced lipolysis technique, also known as Cryolipolysis™. First approved by the Food and Drug Administration (FDA) of the United States in September 2010, Cryolipolysis™ was administered with a machine named Coolsculpting® by ZELTIQ Aesthetics Inc. (Pleasanton, CA). The Korea Food and Drug Administration (KFDA) also granted ZELTIQ permission to be used for noninvasive subcutaneous fat reduction by maintaining a low temperature in the target area. In a previous study using Coolsculpting® in 518 European patients with excessive and unwanted fat (at the flanks, abdomen, back, inner thighs, knees, and buttocks), there was a significant fat reduction effect after 3–6 months from one to three sessions of cryolipolysis, and every two of three patients were satisfied with the result 6. In our study, we used the machine named MiCool™ by Hironic Co., Ltd., which has also been approved by KFDA for noninvasive subcutaneous fat reduction. Its basic mechanism and effectiveness are similar to Coolsculpting® 7. However, an advantage of MiCool™ is its cost‐effectiveness; it is approximately half the price of Coolsculpting® in Korea. It is performed by applying the tips of the machine to the target area, thereby selectively destroying the adipose tissue by delivering cooling energy. Since adipocyte is sensitive to low temperatures, cold‐induced lipolysis can selectively destruct the adipose tissue while preserving the epidermis and dermis 8. Although there were previous animal studies regarding the mechanism of cold‐induced lipolysis, the exact mechanisms in humans remains unclear. It is thought that the adipose tissue apoptosis pathway is activated by caspase‐3, which is also activated by an intracellular lipid crystallization with cryo‐energy 9, 10. Furthermore, there is a study that shows an increased PPAR delta level in adipose tissue after 30 to 60 days post‐treatment 11.
In the present study, we applied cold‐induced lipolysis technique for pseudogynecomastia and evaluated the treatment effect with objective indexes, such as the measurement of chest circumference and subcutaneous fat thickness. Also, each patient was assessed with SGC and its tendency was then analyzed. Two independent dermatologists' global photograph assessments were also done, and the patient's satisfaction score was collected via questionnaire.
The value of chest circumference and subcutaneous fat thickness measurements improved gradually. Unlike the improvement of subcutaneous fat thickness, the chest circumference value at week 28 was only slightly increased (without statistical significance) when compared with the previous visit. It is suggested that the chest circumference measurement may vary by breathing cycle or daily conditions. Hence the degree of increase may be insignificant and it is not considered as PAH. When we analyzed the SGC score, there was a significant improvement throughout the whole period. This study may be significant since we are presenting meaningful results with objective measurements and analyses, especially since previous studies only used subjective indexes (such as photographic assessment to evaluate the treatment effect).
It is, however, worth noting that pseudogynecomastia is a cosmetic problem, which means that to a certain degree it is inherently subjective. Thus, to avoid subjective bias, we performed a photographic assessment using two independent dermatologists and evaluated the patient's satisfaction score. Although the scores of photographic assessment may differ between the two dermatologists when comparing the average, it did show an increased improvement until week 16. Although the degree of improvement slightly decreased at week 28, the absolute value of the score was increased. When compared with the baseline there was a significant improvement with the photographic assessment and no evidence of recurrence. While the effect is not dramatic, there were visible photographic improvements after two sessions of cold‐induced lipolysis (Fig. 7). Moreover, the average satisfaction score was greater than 3 (a little bit improved). Therefore, we can conclude that there was overall improvement for all patients, despite the variance of improvement from one patient to another.
Figure 7.
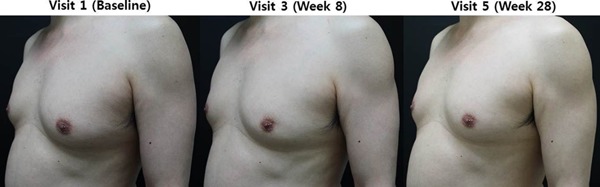
Photographic evaluation of one patient. Compared with the baseline, there were visible improvements after two sessions of cold‐induced lipolysis.
With regard to the safety of this treatment, there was only transient pain, bruising, erythema, and numbness without the alteration of blood lipid levels and liver function 12, furthermore there was no permanent nerve damage. Recently, some case series reported PAH after cryolipolysis 13, 14. Its incidence rate was reported to be within 0.005% to 0.4%. The pathogenesis of this phenomenon is unclear, but it was thought to be preexisting adipocyte hypertrophy. Given the low incidence rate of PAH, there were no cases of PAH during the whole observational period of our study.
There are some limitations in this study. Our study recruited a small number of participants. Pseudogynecomastia is ambiguous to define and difficult to recognize by patients themselves. This difficulty in self‐assessment could be considered as a limitation on the number of volunteers recruited. However, under a well‐controlled study, our results have significant meaning. Moreover, a patient's fat index or gynecomastia status may have varied by daily diet, exercise, etc., as we did not control other individual factors.
Traditional therapeutic options, such as surgical excision or liposuction can show dramatic effect. Since patients can be exposed to unnecessary risks of complications, a noninvasive technique, such as cold‐induced lipolysis, may be a good alternative therapeutic option. Recently, Munavallli et al. reported the effects of cryolipolysis on male enlarged breasts, similar to our study 15. They performed cryolipolysis™ for 21 patients using Coolsculpting® by Zeltiq, and evaluated the effectiveness via ultrasound, clinical photographs, and surveys. They concluded that cryolipolysis™ is a safe, effective, and well‐tolerated noninvasive treatment modality. Although our result is similar to Munavalli et al., our strength is the use of measurements. Our results offer greater objectivity via chest circumference measurements. We also reconfirmed the safety and effectiveness of cold‐induced lipolysis as a treatment option for male pseudogynecomastia. It is important to note the possibility of PAH as a complication, which is thought to be the most important side effect; however, there is no case of PAH in our study. The risk of PAH is very rare, and given the risk and benefit comparison between invasive traditional technique and noninvasive cold‐induced lipolysis, the latter seems logical and should be tried first. This is why we can conclude that cold‐induced lipolysis has strong advantages compared with invasive techniques, even if it shows a less dramatic effect. Furthermore, even if the underlying mechanism is somewhat unclear, adipocyte apoptosis pathway by cryo‐energy is a clue for future research about adipocyte. Also, there is an added benefit as it can be applied to other adipose tissue related diseases, such as lipoma.
IRB protocol approval number: B‐1310/221‐008.
Sources of funding: This article has no funding source.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1. Dan U, Lunenfeld B. Gynecomastia–physiology and pathophysiology. Harefuah 1992; 123(5–6):221–222. [PubMed] [Google Scholar]
- 2. Johnson RE, Murad MH. Gynecomastia: Pathophysiology, evaluation, and management. Mayo Clinic Proc 2009; 84(11):1010–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rose LI, Underwood RH, Newmark SR, Kisch ES, Williams GH. Pathophysiology of spironolactone‐induced gynecomastia. Ann Intern Med 1977; 87(4):398–403. [DOI] [PubMed] [Google Scholar]
- 4. Jewell ML, Solish NJ, Desilets CS. Noninvasive body sculpting technologies with an emphasis on high‐intensity focused ultrasound. Aesthetic Plast Surg 2011; 35(5):901–912. [DOI] [PubMed] [Google Scholar]
- 5. Boey GE, Wasilenchuk JL. Fat reduction in the inner thigh using a prototype cryolipolysis applicator. Dermatol Surg 2014; 40(9):1004–1009. [DOI] [PubMed] [Google Scholar]
- 6. Dierickx CC, Mazer JM, Sand M, Koenig S, Arigon V. Safety, tolerance, and patient satisfaction with noninvasive cryolipolysis. Dermatol Surg 2013; 39(8):1209–1216. [DOI] [PubMed] [Google Scholar]
- 7. Kim J, Kim DH, Ryu HJ. Clinical effectiveness of non‐invasive selective cryolipolysis. J Cosmet Laser Ther 2014; 16(5):209–213. [DOI] [PubMed] [Google Scholar]
- 8. Zelickson B, Egbert BM, Preciado J, Allison J, Springer K, Rhoades RW, Manstein D. Cryolipolysis for noninvasive fat cell destruction: Initial results from a pig model. Dermatol Surg 2009; 35(10):1462–1470. [DOI] [PubMed] [Google Scholar]
- 9. Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR. Selective cryolysis: A novel method of non‐invasive fat removal. Lasers Surg Med 2008; 40(9):595–604. [DOI] [PubMed] [Google Scholar]
- 10. Krueger N, Mai SV, Luebberding S, Sadick NS. Cryolipolysis for noninvasive body contouring: Clinical efficacy and patient satisfaction. Clin Cosmet Investig Dermatol 2014; 7:201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kwon TR, Yoo KH, Oh CT, Shin DH, Choi EJ, Jung SJ, Hong H, Choi YS, Kim BJ. Improved methods for selective cryolipolysis results in subcutaneous fat layer reduction in a porcine model. Skin Res Technol 2015; 21(2):192–200. [DOI] [PubMed] [Google Scholar]
- 12. Klein KB, Zelickson B, Riopelle JG, Okamoto E, Bachelor EP, Harry RS, Preciado JA. Non‐invasive cryolipolysis for subcutaneous fat reduction does not affect serum lipid levels or liver function tests. Lasers Surg Med 2009; 41(10):785–790. [DOI] [PubMed] [Google Scholar]
- 13. Jalian HR, Avram MM, Garibyan L, Mihm MC, Anderson RR. Paradoxical adipose hyperplasia after cryolipolysis. JAMA Dermatol 2014; 150(3):317–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Singh SM, Geddes ER, Boutrous SG, Galiano RD, Friedman PM. Paradoxical adipose hyperplasia secondary to cryolipolysis: An underreported entity? Lasers Surg Med 2015; 47(6):476–478. [DOI] [PubMed] [Google Scholar]
- 15. Munavalli GS, Panchaprateep R. Cryolipolysis for targeted fat reduction and improved appearance of the enlarged male breast. Dermatol Surg 2015; 41(9):1043–1051. [DOI] [PubMed] [Google Scholar]


