Abstract
Objective
This study analyzed suicide data in the general population from the U.S. National Violent Death Reporting System (NVDRS) to investigate suicide burden among those with epilepsy and risk factors associated with suicide and to suggest measures to prevent suicide among people with epilepsy.
Methods
The NVDRS is a multiple-state, population-based, active surveillance system that collects information on violent deaths including suicide. Among people 10 years old and older, we identified 972 suicide cases with epilepsy and 81,529 suicide cases without epilepsy in 17 states from 2003 through 2011. We estimated their suicide rates, evaluated suicide risk among people with epilepsy, and investigated suicide risk factors specific to epilepsy by comparing those with and without epilepsy. In 16 of the 17 states providing continual data from 2005 through 2011, we also compared suicide trends in people with epilepsy (n = 833) and without epilepsy (n = 68,662).
Results
From 2003 through 2011, the estimated annual suicide mortality rate among people with epilepsy was 16.89/100,000 per persons, 22% higher than that in the general population. Compared with those without epilepsy, those with epilepsy were more likely to have died from suicide in houses, apartments, or residential institutions (81% vs. 76%, respectively) and were twice as likely to poison themselves (38% vs. 17%) (P < 0.01). More of those with epilepsy aged 40–49 died from suicide than comparably aged persons without epilepsy (29% vs. 22%) (P < 0.01). The proportion of suicides among those with epilepsy increased steadily from 2005 through 2010, peaking significantly in 2010 before falling.
Significance
For the first time, the suicide rate among people with epilepsy in a large U.S. general population was estimated, and the suicide risk exceeded that in the general population. Suicide prevention efforts should target people with epilepsy 40–49 years old. Additional preventive efforts include reducing the availability or exposure to poisons, especially at home, and supporting other evidence-based programs to reduce mental illness comorbidity associated with suicide.
Keywords: Epilepsy, Suicide, Epidemiology, Rate, Population
1. Introduction
In 2014, 59,097 persons died in the United States as a result of violence. Of the 58,348 violence-related deaths in those ten years old or older, 73% of these deaths were from suicide making it one of the leading causes of death and a major public health problem [1].
A recent study indicated that epilepsy, psychiatric disorder, and suicide may be pathophysiologically linked [2]. Two studies have estimated a suicide risk about 3 times higher in people with epilepsy than in the general population [3,4]. Therefore, suicide among people with epilepsy, especially among those with a co-occurring psychiatric disorder, has caused a great public health concern.
Although many studies have reported the suicide burden in people with epilepsy [5,6], most reported the percentage of suicides among all causes of death in people with epilepsy. Differences in the underlying populations, patient selection criteria, sample sizes, study designs, and methods of analyses in these studies yielded percentages of suicides varying from zero to 70% [5,6]. These differences make it difficult to estimate the overall suicide burden in people with epilepsy, and these estimates are more than ten years old. Even though suicide rates among people with epilepsy can be calculated indirectly from a few population-based studies targeting cause-specific mortality [7,8], the suicide rate among people with epilepsy in the large general population is still unknown because general population-based surveillance systems including both epilepsy and suicide have not been routinely available.
The U.S. National Violent Death Reporting System (NVDRS) is a multiple-state, population-based, active surveillance system that is monitored by the U.S. Centers for Disease Control and Prevention (CDC) [9]. Currently, NVDRS collects data from 32 US states [10]. The NVDRS collects detailed information on the circumstances of violent deaths including suicides in defined populations. Its purpose is to obtain accurate, timely, and comprehensive data to better understand and ultimately to prevent the occurrence of violent deaths in the U.S. [9,10].
Using the NVDRS, we searched for decedents who died from suicide and had mentions in their records of epilepsy or seizures to identify cases of suicide with epilepsy. We also estimated the numbers of people with epilepsy in the participating states based on recent population-based estimates of U.S. epilepsy prevalence [11,12]. This study was designed to answer the following questions among people with epilepsy in the general population who died from suicide: What is the burden of suicide? Does suicide occur more often in people with epilepsy than in the general population? When, where, and how does suicide occur among people with epilepsy? Do the study results provide clues to develop an effective preventive strategy to reduce suicide rates in people with epilepsy? We tried to answer these questions by 1) estimating suicide rates among people with epilepsy; 2) comparing these suicide rates with such rates in the general population; 3) describing selected demographic characteristics and the annual trend of suicide occurrence in people with epilepsy; and 4) comparing these characteristics and this trend between people with epilepsy who died from suicide and people without epilepsy who died from suicide.
2. Materials and methods
2.1. Data source
Currently, NVDRS collects data from 32 states; however, because some states have been a part of the system for a short period of time, we decided to study suicide data from the NVDRS collected from 2003 through 2011 in 17 states, including examining data from 16 states that collected data continuously from 2005–2011. The NVDRS is a U.S. population-based, active surveillance system that collects data on all violent deaths (including suicides) occurring in participating states [9]. The NVDRS is the only state-based surveillance system in the U.S. that pools data on violence-related deaths from multiple sources into a usable, deidentified database. Data come from three primary sources: death certificates, medical examiner/coroner reports, and law enforcement records [10]. The NVDRS collects about 250 unique variables for each death from these information sources. The NVDRS also includes data abstraction by abstractors who compose text narratives that describe further details about the death, taking into account information from all source documents. The NVDRS provides states and communities with comprehensive, accurate, and timely information about violent deaths to aid in the development, implementation, and evaluation of violence prevention strategies, allowing them to track the progress of these strategies over time.
The NVDRS defines suicide as a death resulting from the use of force against oneself when a preponderance of the evidence indicates that the use of force was intentional. This category also includes deaths of persons who intended only to injure rather than to kill themselves, deaths associated with risk-taking behavior without clear intent to inflict fatal injury but associated with high risk for death (e.g., “Russian roulette”), and deaths involving only others' passive assistance to the decedent (e.g., supplying the means or information needed to complete the act). This definition excludes deaths caused by chronic or acute substance abuse without the intent to die and deaths attributed to autoerotic behavior (i.e., self-strangulation during sexual activity). The NVDRS uses the following International Classification of Diseases, 10th edition (ICD-10) codes for suicides: X60–X84 and Y87.0 [9].
2.2. Study design and population
This cross-sectional study was based on NVDRS data from 2003 through 2011 in 17 states (Table 1). By using the method of ICD code and text search (described below), among people 10 years old and older, we identified the total number of suicide deaths, the subset of these deaths who had co-occurring epilepsy, and the remainder who did not have epilepsy. We estimated the suicide rate among people with epilepsy, compared this rate with that in the general population, and contrasted the sociodemographic characteristics by comparing those who died from suicide in those with and without epilepsy. In a subgroup of 16 of these 17 states that provided continual data, we determined annual trends of suicide rates from 2005 through 2011 in people with and without epilepsy (Table 4).
Table 1.
Estimated Annual Suicide Mortality Rates among People with Epilepsy in the General Population (10 years old and older) — U.S. National Violent Death Reporting System, 17 States, 2003–2011.
| Years | Estimated numbers of people with epilepsy by participating states with vary data entering years1 | Estimated No. of people with epilepsy | Total Suicide cases with epilepsy | Annual2 Suicide mortality rate (/100,000) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||||||
| AK | CO | GA | KY | MD | MA | NJ | NM | NC | OH | Ok | OR | RI | SC | UT | VA | WI | ||||
| 2003 | 5349 | x | x | x | 46435 | 54973 | 72833 | x | x | x | x | 30189 | 35145 | x | 62520 | x | 307444 | 40 | 13.01 | |
| 2004 | 5459 | 38486 | 73049 | x | 46940 | 55000 | 73040 | x | 72348 | x | 29709 | 30432 | 9233 | 35717 | x | 63482 | 46838 | 579733 | 82 | 14.14 |
| 2005 | 5537 | 38972 | 66584 | 35515 | 47418 | 55048 | 73323 | 16203 | 73638 | x | 29896 | 30848 | 92001 | 36251 | 19510 | 64409 | 47171 | 732324 | 93 | 12.70 |
| 2006 | 5611 | 39725 | 76271 | 35828 | 47793 | 55210 | 73564 | 16471 | 75438 | x | 30262 | 31364 | 9183 | 37020 | 20016 | 65288 | 47458 | 666502 | 94 | 14.10 |
| 2007 | 5657 | 40410 | 77834 | 36143 | 48069 | 55475 | 73818 | 16700 | 77051 | x | 30567 | 31824 | 9146 | 37741 | 20545 | 65966 | 47739 | 674685 | 105 | 15.56 |
| 2008 | 5722 | 41136 | 79178 | 36409 | 48385 | 55872 | 74200 | 16863 | 78689 | x | 30846 | 32231 | 9141 | 38469 | 21033 | 66705 | 48001 | 682880 | 114 | 16.69 |
| 2009 | 5799 | 41848 | 80298 | 36668 | 48833 | 56370 | 74661 | 17073 | 79936 | x | 31230 | 32604 | 9147 | 39012 | 21500 | 67545 | 48258 | 690782 | 118 | 17.08 |
| 2010 | 5929 | 42542 | 81219 | 36954 | 49378 | 56857 | 75163 | 17327 | 80997 | x | 31574 | 32891 | 9151 | 39469 | 21924 | 68435 | 48480 | 698290 | 162 | 23.20 |
| 2011 | 6014 | 43240 | 82229 | 37161 | 49898 | 57325 | 75560 | 17464 | 81941 | 98669 | 31811 | 33216 | 9144 | 39864 | 22301 | 69213 | 48739 | 803789 | 164 | 20.40 |
| Total | 5836429 | 972 | 16.70 | |||||||||||||||||
Abbreviations: AK, Alaska; CO, Colorado; GA, Georgia; KY, Kentucky; MD, Maryland; MA, Massachusetts; NJ, New Jersey; NM, New Mexico; NC, North Carolina; OH, Ohio; OK, Oklahoma; OR, Oregon; RI, Rhode Island; SC, South Carolina; UT, Utah; VA, Virginia; WI, Wisconsin; X, unavailable.
The estimated number of people with epilepsy in each state in each year is the sum of people with epilepsy from 10–17 years old and from 18 years old older. These numbers were calculated by multiplying the estimated prevalence of epilepsy in U.S. children 10–17 years old (8.1/1,000) and the prevalence of epilepsy in the U.S. adults ≥18 years old (10.0/1,000) by the corresponding age-specific populations in each specific state and year (see Methods section).
The annual suicide mortality rate is the ratio of total number of people with epilepsy who committed suicide to the total estimated number of people with epilepsy each year.
Table 4.
Number And Percentage of Suicides in Those With and Without Epilepsy (10 years old and older) by Year— U.S. National Violent Death Reporting System, 2005–2011, 16 of 17 States (Excluding Ohio).
| Suicides With Epilepsy
|
Suicides Without Epilepsy
|
Total Suicides
|
||||
|---|---|---|---|---|---|---|
| Year | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) |
|
|
|
|||||
| 2005 | 93 | 11.2 (9.1–13.5) | 8,892 | 13.0 (12.7–13.2) | 8,985 | 12.9 (12.7–13.2) |
| 2006 | 94 | 11.3 (9.2–13.6) | 9,194 | 13.4 (13.1–13.6) | 9,288 | 13.4 (13.1–13.6) |
| 2007 | 105 | 12.6 (10.4–15.1) | 9,541 | 13.9 (13.6–14.2) | 9,646 | 13.9 (13.6–14.1) |
| 2008 | 114 | 13.7 (11.4–16.2) | 9,737 | 14.2 (13.9–14.4) | 9,851 | 14.2 (13.9–14.4) |
| 2009 | 118 | 14.2 (11.9–16.7) | 10,172 | 14.8 (14.5–15.1) | 10,290 | 14.8 (14.5–15.1) |
| 2010 | 162 | 19.4 (16.8–22.3)* | 10,445 | 15.2 (14.9–15.5) | 10,607 | 15.3 (15.0–15.5) |
| 2011 | 147 | 17.6 (15.1–20.4) | 10,681 | 15.6 (15.3–15.8) | 10,828 | 15.6 (15.3–15.9) |
| Total | 833 | 68,662 | 69,495 | |||
Abbreviation: 95% CI, 95% exact confidence interval for a percentage (based on the modified Clopper-Pearson CI for a proportion).
p<0.01 when comparing to previous years within the same group, or comparing to suicides without epilepsy in 2010.
2.3. Identification of suicide deaths in people with epilepsy/seizure in NVDRS
To identify cases of suicide among people with epilepsy/seizure, we searched text from death certificates, medical examiner/coroner records, law enforcement reports, and abstractors' narratives/descriptors using the following key words and phrases: “epilepsy”, “seizure”, “convulsion”, “drop attack”, “falling out spell”, and “staring spell”. These key words and phrases have been validated as ways to identify those with possible epilepsy in different kinds of population-based surveys [12,13–15]. We also identified suicide cases with epilepsy by searching for the following epilepsy/seizure-related ICD-10 codes: G40, G41, P90, and R56 in both the underlying cause of death and the first ten multiple conditions recoded on the death certificate. Finally, we read abstractors' narratives/descriptors among those identified as having epilepsy and dying by the method of poisoning from this search and were able to exclude 43 suicide cases whose seizures were not associated with epilepsy but with drugs or other poisons that cause seizures (i.e., drug-induced seizures).
2.4. Calculation of suicide rates among people with epilepsy in the general population
We estimated the total number of people with epilepsy in each NVDRS state for each study year in the following way. Using findings from an analysis of data from the 2007 National Survey of Children's Health [11], we estimated that the current (or active) epilepsy prevalence in U.S. children aged 10–17 years is 8.1/1000 persons. The corresponding estimated current epilepsy prevalence in U.S. adults 18 years old or older from an analysis of 2010 U.S. National Health Interview Survey data [12] is 10.0/1000 persons (this prevalence did not change in 2013 NHIS). Using these estimates and the age-specific populations of those 10 years of age or older in each participating state for each study year [16], we estimated the total expected number of people with epilepsy in each state for each study year. The annual state-specific suicide rate in people with epilepsy is the proportion of the total number of suicide cases in people with epilepsy in each state for each study year from the NVDRS to the total expected number of people with epilepsy in each state for each study year.
2.5. Comparing suicide trends between people with and without epilepsy
We estimated trends of annual suicide rates for persons with epilepsy from 17 states participating in NVDRS from 2003 through 2011. We also estimated trends of annual proportions of suicides with and without epilepsy in the 16 states (all but Ohio) with continual data from 2005 through 2011. The annual proportion of suicides is the proportion of the number of suicides each year to the total number of suicides for all years from 2005 through 2011.
2.6. Selected sociodemographic characteristics
To study sociodemographic characteristics associated with violent deaths, NVDRS collects information about characteristics such as age, gender, race/ethnicity, education, and marital status. It also collects information about the location of injury (e.g., victim's home, recreation area, street), the month of injury, and the method of injury (e.g., poisoning, hanging/suffocation, firearm).
2.7. Statistical analysis
In those who died from suicide with and without epilepsy, we compared the proportions of suicide deaths by the month, the location of death, and the method of injury. We also compared the sex-specific proportions of suicide deaths in these two groups by age, race/ethnicity, education, and marital status. We defined as statistically significant differences in proportions of deaths whose two-sided 95% binomial confidence intervals did NOT overlap (the statistical significance level = 0.01). We used the Cochran–Armitage trend test to test for trends (also the statistical significance level = 0.01). All analyses used SAS version 9.3 (SAS Institute). Following NVDRS guidance, we suppressed table cells with fewer than five deaths but did show table cells with no deaths.
3. Results
From 2003 through 2011 in 17 states, NVDRS identified 82,501 suicide deaths, 972 (1.2%) of whom had co-occurring epilepsy. The estimated annual suicide rate among people with epilepsy steadily increased to a peak in 2010 before falling (Table 1). The overall average suicide rate in people with epilepsy was 16.89/100,000 persons per year.
The percentages of suicide deaths by month of death did not differ between people with epilepsy and without epilepsy (Table 2). Most suicide deaths occurred in a house or apartment in those with epilepsy (78%) and those without epilepsy (75%), although significantly more deaths occurred in houses, apartments, or residential institutions in people with epilepsy (81%) than in those without epilepsy (76%; P < 0.01). Poisoning, use of firearms, and hanging/strangulation/suffocation were the top three methods of committing suicide in both those with and without epilepsy. However, compared with suicide cases in those without epilepsy, suicide cases in those with epilepsy were more likely to poison themselves (38% vs. 17%; P < 0.01) but less likely to use hanging, strangulation, suffocation, or firearms (54% vs. 76%; P < 0.01).
Table 2.
Number and Percentage of Suicides with and without Epilepsy (10 years old and older), By Method , Location, and Month—U.S. National Violent Death Reporting System, 17 States, 2003–2011
| With Epilepsy
|
Without Epilepsy
|
Total
|
||||
|---|---|---|---|---|---|---|
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |
| Month | ||||||
| January | 93 | 9.6 (7.8–11.6) | 6,540 | 8.0 (7.8–8.2) | 6,633 | 8.0 (7.9–8.2) |
| February | 65 | 6.7 (5.2–8.5) | 6,053 | 7.4 (7.3–7.6) | 6,118 | 7.4 (7.2–7.6) |
| March | 95 | 9.8 (8.0–11.8) | 7,012 | 8.6 (8.4–8.8) | 7,107 | 8.6 (8.4–8.8) |
| April | 69 | 7.1 (5.6–8.9) | 6,830 | 8.4 (8.2–8.6) | 6,899 | 8.4 (8.2–8.6) |
| May | 92 | 9.5 (7.7–11.5) | 7,187 | 8.8 (8.6–9.0) | 7,279 | 8.8 (8.6–9.0) |
| June | 79 | 8.1 (6.5–10.0) | 6,945 | 8.5 (8.3–8.7) | 7,024 | 8.5 (8.3–8.7) |
| July | 76 | 7.8 (6.2–9.7) | 7,275 | 8.9 (8.7–9.1) | 7,351 | 8.9 (8.7–9.1) |
| August | 77 | 7.9 (6.3–9.8) | 7,059 | 8.7 (8.5–8.9) | 7,136 | 8.7 (8.5–8.9) |
| September | 93 | 9.6 (7.8–11.6) | 6,874 | 8.4 (8.2–8.6) | 6,967 | 8.5 (8.3–8.6) |
| October | 74 | 7.6 (6.0–9.5) | 6,945 | 8.5 (8.3–8.7) | 7,019 | 8.5 (8.3–8.7) |
| November | 85 | 8.8 (7.1–10.7) | 6,439 | 7.9 (7.7–8.1) | 6,524 | 7.9 (7.7–8.1) |
| December | 72 | 7.4 (5.9–9.3) | 6,296 | 7.7 (7.5–7.9) | 6,368 | 7.7 (7.5–7.9) |
| Total | 970b | 81,455 b | 82,425 b | |||
| Location | ||||||
| House/Apartment | 756 | 77.8 (75.0–80.4)* | 60,748 | 74.5 (74.2–74.8) | 61,504 | 74.5 (74.3–74.8) |
| Commercial Area | 46 | 4.7 (3.5–6.3) | 3,665 | 4.5 (4.4––4.6) | 3,711 | 4.5 (4.4–4.6) |
| Transport area: other | 35 | 3.6 (2.5–5.0) | 3,872 | 4.7 (4.6–4.9) | 3,907 | 4.7 (4.6–4.9) |
| Other Specified Places | 31 | 3.2 (2.2–4.5) | 2,894 | 3.5 (3.4–3.7) | 2,925 | 3.5 (3.4–3.7) |
| Natural Area/Countryside | 28 | 2.9 (1.9–4.1) | 3,561 | 4.4 (4.2–4.5) | 3,589 | 4.4 (4.2–4.5) |
| Residential Institution | 28 | 2.9 (1.9–4.1)* | 1,484 | 1.8 (1.7–1.9) | 1,512 | 1.8 (1.7–1.9) |
| Public Transport area | 24 | 2.5 (1.6–3.7) | 2,718 | 3.3 (3.2–3.5) | 2,742 | 3.3 (3.2–3.4) |
| Unknown | 13 | 1.3 (0.7–2.3) | 1,456 | 1.8 (1.7–1.9) | 1,469 | 1.8 (1.7–1.9) |
| Recreational Area | 11 | 1.1 (0.6–2.0) | 1,131 | 1.4 (1.3–1.5) | 1,142 | 1.4 (1.3–1.5) |
| Total | 972 | 81,529 | 82,501 | |||
| Method | ||||||
| Poisoning | 332 | 38.4 (35.2–41.8)* | 12,566 | 16.9 (16.7–17.2) | 12,898 | 17.2 (16.9–17.4) |
| Firearm | 297 | 34.4 (31.2–37.6)* | 39,334 | 53.0 (52.6–53.3) | 39,631 | 52.8 (52.4–53.1) |
| Hanging/Strangulation/Suffocation | 169 | 19.6 (17.0–22.4)* | 17,380 | 23.4 (23.1–23.7) | 17,549 | 23.4 (23.1–23.7) |
| Fall/Jumping | 26 | 3.0 (2.0–4.4) | 1,662 | 2.2 (2.1–2.3) | 1,688 | 2.2 (2.1–2.4) |
| Sharp Object | 15 | 1.7 (1.0–2.8) | 1,248 | 1.7 (1.6–1.8) | 1,263 | 1.7 (1.6–1.8) |
| Other Specified Means/Unspecified Means | 8 | 0.9 (0.4–1.8) | 620 | 0.8 (0.8–0.9) | 628 | 0.8 (0.8–0.9) |
| Fire and Burns | 6 | 0.7 (0.3–1.5) | 284 | 0.4 (0.3–0.4) | 290 | 0.4 (0.3–0.4) |
| Sequelae of intentional self-harm, assault, and events of | 6 | 0.7 (0.3–1.5) | 150 | 0.2 (0.2–0.2) | 156 | 0.2 (0.2–0.2) |
| Drowning and Submersion | 5 | 0.6 (0.2–1.3) | 776 | 1.0 (1.0–1.1) | 781 | 1.0 (1.0–1.1) |
| Explosive Material | 0 | ------ | 5 | 0.0 (0.0–0.0) | 5 | 0.0 (0.0–0.0) |
| Blunt Object | 0 | ------ | a | a | ||
| Motor Vehicle | 0 | ------ | 223 | 0.3 (0.3–0.3) | 223 | 0.3 (0.3–0.3) |
| Total | 864b | 100.0 | 74,252 b | 100.0 | 75,116b | 100.0 |
Abbreviation: 95% CI: 95% exact confidence interval for a percentage (based on the modified Clopper-Pearson CI for a proportion).
P<0.01when comparing those with epilepsy to those without epilepsy.
Estimates were not reported when number of decedents was 1–4.
Total numbers are fewer than 972 (suicides with epilepsy), 81529 (suicides without epilepsy) or 82501 (total suicides),respectively due to the missing data .
Most suicides in both those with and those without epilepsy occurred among those 18–59 years old (84% vs. 76%) and among non-Hispanic whites (86% vs. 85%) (Table 3). Compared with those without epilepsy, however, those with epilepsy were more likely to commit suicide if they were 30–39 years old (women), 40–49 years old (both sexes), or 50–59 years old (men) and less likely to commit suicide if they were younger than 30 years old or were 70 years old or older (P < 0.01). The percentages of people with epilepsy who committed suicide did not differ from that of people without epilepsy by race/ethnicity or educational level; about one-third of the suicides in both groups occurred among those with the least education. In both those with and without epilepsy, women were more likely than men to commit suicide if they had been separated, divorced, or widowed, and men were more likely than women to commit suicide if they had never been married (all P-values <0.01).
Table 3.
Number And Percentage of Suicides With and Without Epilepsy(10 years old and older), by Decedent’s Sociodemographic Characteristics—U.S. National Violent Death Reporting System, 17 States, 2003–2011.
| Male
|
Female
|
Both Sexes
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| With Epilepsy
|
Without Epilepsy
|
With Epilepsy
|
Without Epilepsy
|
With Epilepsy
|
Without Epilepsy
|
|||||||
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |
| Age Group (Years) | ||||||||||||
| 10–17 | 11 | 1.7 (0.9–3.1) | 1,749 | 2.7 (2.6–2.9) | 10 | 2.9 (1.4–5.3) | 572 | 3.3 (3.0–3.5) | 21 | 2.2 (1.3–3.3) | 2,321 | 2.9 (2.7–3.0) |
| 18–29 | 100 | 15.9 (13.1–19.0) | 12,324 | 19.3 (19.0–19.6) | 44 | 12.8 (9.5–16.8) | 2,552 | 14.6 (14.1–15.1) | 144 | 14.8 (12.6–17.2)* | 14,876 | 18.3 (18.0–18.5) |
| 30–39 | 95 | 15.1 (12.4–18.1) | 10,617 | 16.6 (16.3–16.9) | 78 | 22.7 (18.4–27.5)* | 2,909 | 16.6 (16.1–17.2) | 173 | 17.8 (15.4–20.4) | 13,526 | 16.6 (16.4–16.9) |
| 40–49 | 173 | 27.5 (24.0–31.2)* | 13,472 | 21.1 (20.8–21.4) | 106 | 30.9 (26.1–36.1)* | 4,475 | 25.6 (25.0–26.3) | 279 | 28.7 (25.9–31.7) * | 17,947 | 22.0 (21.8–22.3) |
| 50–59 | 147 | 23.4 (20.1–26.9)* | 11,931 | 18.7 (18.4–19.0) | 71 | 20.7 (16.5–25.4) | 3,938 | 22.5 (21.9–23.2) | 218 | 22.4 (19.8–25.2) | 15,869 | 19.5 (19.2–19.8) |
| 60–69 | 52 | 8.3 (6.2–10.7) | 6,347 | 9.9 (9.7–10.2) | 27 | 7.9 (5.3–11.2) | 1,732 | 9.9 (9.5–10.4) | 79 | 8.1 (6.5–10.0) | 8,079 | 9.9 (9.7–10.1) |
| 70 and Above | 51 | 8.1 (6.1–10.5)* | 7,506 | 11.7 (11.5–12.0) | 7 | 2.0 (0.8–4.2)* | 1,305 | 7.5 (7.1–7.9) | 58 | 6.0 (4.6–7.6) * | 8,811 | 10.8 (10.6–11.0) |
| Total | 629 | 63,946 | 343 | 17483 | 972 | 81,429a | ||||||
| Race/Ethnicity | ||||||||||||
| Non–Hispanic White | 524 | 84.8 (81.7–87.5) | 53,488 | 84.7 (84.4–85.0) | 295 | 86.8 (82.7–90.2) | 14,968 | 86.7 (86.2–87.2) | 819 | 85.5 (83.1–87.7) | 68,456 | 85.1 (84.9–85.4) |
| Non–Hispanic Black | 37 | 6.0 (4.3–8.2) | 4,595 | 7.3 (7.1–7.5) | 15 | 4.4 (2.5–7.2) | 899 | 5.2 (4.9–5.5) | 52 | 5.4 (4.1–7.1) | 5,494 | 6.8 (6.7–7.0) |
| Hispanic | 35 | 5.7 (4.0–7.8) | 3,049 | 4.8 (4.7–5.0) | 18 | 5.3 (3.2–8.2) | 614 | 3.6 (3.3–3.8) | 53 | 5.5 (4.2–7.2) | 3,663 | 4.6 (4.4–4.7) |
| Other | 22 | 3.6 (2.2–5.3) | 1,999 | 3.2 (3.0–3.3) | 12 | 3.5 (1.8–6.1) | 785 | 4.5 (4.2–4.9) | 34 | 3.5 (2.5–4.9) | 2,784 | 3.5 (3.3–3.6) |
| Total | 618 | 63,131 | 340 | 17,266 | 958a | 80,397a | ||||||
| Education | ||||||||||||
| High School or Less | 202 | 32.1 (28.5–35.9) | 20,950 | 32.7 (32.4–33.1) | 97 | 28.3 (23.6–33.4) | 4,750 | 27.1 (26.5–27.8) | 299 | 30.8 (27.9–33.8) | 25,700 | 31.5 (31.2–31.8) |
| Some College | 39 | 6.2 (4.4–8.4) | 4,515 | 7.1 (6.9–7.3) | 34 | 9.9 (7.0–13.6) | 1,430 | 8.2 (7.8–8.6) | 73 | 7.5 (5.9–9.4) | 5,945 | 7.3 (7.1–7.5) |
| Undergraduate | 55 | 8.7 (6.7–11.2) | 4,929 | 7.7 (7.5–7.9) | 39 | 11.4 (8.2–15.2) | 1,858 | 10.6 (10.2–11.1) | 94 | 9.7 (7.9–11.7) | 6,787 | 8.3 (8.1–8.5) |
| Graduate Degree | 11 | 1.7 (0.9–3.1) | 1,576 | 2.5 (2.3–2.6) | 6 | 1.7 (0.6–3.8) | 540 | 3.1 (2.8–3.4) | 17 | 1.7 (1.0–2.8) | 2,116 | 2.6 (2.5–2.7) |
| Unknown | 322 | 51.2 (47.2–55.2) | 32,047 | 50.1 (49.7–50.4) | 167 | 48.7 (43.3–54.1) | 8,920 | 51.0 (50.2–51.7) | 489 | 50.3 (47.1–53.5) | 40,967 | 50.3 (49.9–50.6) |
| Total | 629 | 64,017 | 343 | 17,498 | 972 | 81,515a | ||||||
| Marital Status | ||||||||||||
| Married | 216 | 34.9 (31.1–38.8) | 23,666 | 37.4 (37.0–37.8) | 115 | 33.8 (28.8–39.1) | 6,362 | 36.7 (36.0–37.4) | 331 | 34.5 (31.5–37.6) | 30,028 | 37.2 (36.9–37.6) |
| Widowed/Divorced/ | 169 | 27.3 (23.8–31.0) † | 17,526 | 27.7 (27.3–28.0)‡ | 129 | 37.9 (32.8–43.3) | 2429.7 (29.4– | |||||
| Separated | 6,402 | 37.0 (36.2–37.7) | 298 | 31.1 (28.2–34.1) | 23,928 | 30.0) | ||||||
| Never Married | 234 | 37.8 (34.0–41.8) † | 22,112 | 34.9 (34.6–35.3)‡ | 96 | 28.2 (23.5–33.3) | 4,561 | 26.3 (25.7–27.0) | 330 | 34.4 (31.4–37.5) | 26,673 | 33.1 (32.8–33.4) |
| Total | 619 | 63,304 | 340 | 17,325 | 959a | 80,629a | ||||||
Abbreviation: 95% CI: 95% exact confidence interval for a percentage (based on the modified Clopper-Pearson CI for a proportion).
P<0.01 when comparing those with epilepsy to those without epilepsy in the same gender groups or both sex group.
P< 0.01 when comparing those with epilepsy in the female group.
P< 0.01 when comparing those without epilepsy in the female group.
Total number are fewer than 972 (suicides with epilepsy) or 81529 (suicides without epilepsy), respectively due to the missing data.
When looking only at the 16 states that provided continual data from 2005 through 2011, NVDRS identified 69,495 suicide deaths, 833 (1.2%) of whom had co-occurring epilepsy. The trends of suicide deaths steadily increased over time in those with and without epilepsy (Table 4 and Fig. 1). In 2010, the percentage of suicide deaths in people with epilepsy peaked and significantly exceeded both that of those with epilepsy in previous years and that of those without epilepsy in 2010 (both P < 0.01), though these percentages did not differ significantly in 2011. This phenomenon is consistent with our observation in Table 1 indicating that the annual suicide rate among people with epilepsy steadily increased to a peak in 2010 before falling.
Fig. 1.
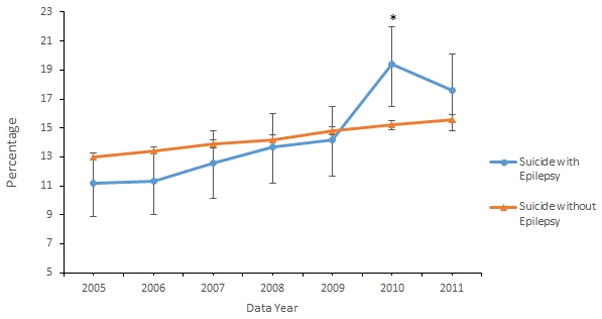
Annual percentage of suicides among all suicides (10 years old and older, 2005 to 2011), by epilepsy status.
*P < 0.01 when comparing to previous years within the same group or comparing to people without epilepsy in 2010.
4. Discussion
Estimates of the suicide burden among people with epilepsy in the general population vary substantially, but most of them were based on small populations. Suicide rates can be calculated based on the published data from only a few studies with large samples of patients with epilepsy, but these studies neither focused on suicide rates [7] nor were representative of the general population [8]. Our study fills these gaps. By using the population-based NVDRS, this study is the first to estimate suicide rates among people with epilepsy in a large, general population of 17 U.S. states participating in NVDRS in the years studied. The estimated average annual suicide rate among people with epilepsy in this population from 2003 through 2011 was 16.89/100,000 persons. About 1.2% of all suicides occurred among people with epilepsy. A prior meta-analysis estimated that 13.5% of all suicides occurred among people with epilepsy [17]. We think that this meta-analysis overestimated the percentage of suicides among those with epilepsy because many of its included studies comprised small samples, highly selected groups of patients, and studies from different countries.
Both a large, Danish case–control study within a cohort and a different comprehensive meta-analysis reported that people with epilepsy have about 3 times the risk of suicide than those in the general population [3,4]. Our study indicated that the estimated average annual suicide rate across the 17 NVDRS states from 2003 through 2011 among people with epilepsy (16.89/100,000 persons) was only 22% higher than that in the general population of the same states during the same years (13.84/100,000 per persons) [18]. In contrast with the Danish study, our smaller risk estimate is consistent with other findings that suicide risk among people with epilepsy is lower in community than in patient populations [4]. Other possible explanations for this smaller risk include variations among countries [5] or underidentification (or estimation) of suicides co-occurring with epilepsy (see the detailed description below of limitations). However, the strength of the current estimate is that it is based on data from about one-third of the U.S. population from the 17 participating U.S. states [16]. This study also identified epilepsy and seizures in suicide decedents through a broad search in all suicide-related official documents including unique abstractor's narratives/descriptors in the NVDRS.
Except for suicide burden and risk, the basic epidemiology of suicide (its distribution and determinants) among people with epilepsy in the general population also has been unclear [19–21]. In our study, people with epilepsy who died of suicide were more likely to poison themselves than those without epilepsy, a finding consistent with those from studies based on reports from hospitals and emergency rooms [21–23]. This consistent finding in different populations suggests that people with epilepsy who demonstrate a prior risk for suicide (suicidal intentions or attempts) may benefit from having caregivers, relatives, and others in the home supervise the availability of potentially harmful materials to prevent suicide; this is especially important at home [24] since suicide among people with epilepsy in our study more often occurred at home than elsewhere.
Because suicide poisonings are more likely to occur among people with epilepsy, it is important to understand the drugs involved in this special group. One-third to two-thirds of patients with epilepsy who were proven or suspected suicides and reported in previous studies overdosed on antiepileptic drugs [21,25]. In the current study, a search of 36 antiepileptic drugs (see supplemental document 1 online) in the NVDRS data files (including abstractor's narrative and descriptor) found that only 20/332 (6%) of those with epilepsy who poisoned themselves used antiepileptic drugs to commit suicide (detailed results not shown). This difference in estimates between our findings and previous findings may result from different sample sizes, study designs, and especially selected patient populations.
Another important finding from this study is that, compared with people without epilepsy, those with epilepsy aged 40–49 are more likely, and those aged 18–29 or 70 years old or older are less likely, to commit suicide. In the general population, even though epilepsy incidence is higher in children and older adults [26,27], the highest epilepsy prevalence occurs in those 35 through 64 years old [10], which may account for our results. Other factors in these middle-age groups may also contribute to this increased risk. Obviously, further advocacy of awareness of suicide risk in these vulnerable age groups is needed to prevent suicide deaths.
In both those with epilepsy and those without epilepsy, never married men died from suicide more often than never married women, and separated, divorced, or widowed women died from suicide more often than separated, divorced, or widowed men. These findings are consistent with other studies indicating that less social support is a major risk factor for morbidity as well as mortality [28]. Because people with epilepsy are more likely to never have been married than those without epilepsy [29,30], decreased social support [31] may make them more prone to psychological and physical ailments that could cause a higher risk of suicide [32]. However, overall marital status did not differ between those with and without epilepsy when we combined men and women who died from suicide.
Finally, from 2003 to 2011, the estimated annual suicide rate among people with epilepsy steadily increased over time, peaking in 2010, before falling. The proportion of annual suicides among all suicides in those with epilepsy also followed the same pattern, peaking in 2010, significantly higher than that in those with epilepsy in the previous years and also significantly higher than this proportion in those without epilepsy in 2010. The estimated U.S. epilepsy prevalence overall rose from 2007 until 2010 and 2011, where it plateaued [26]. Although consistent with our trend in the proportion of annual suicides among all suicides in those with epilepsy, these changes in prevalence would not account for changes in estimated annual suicide rates using estimated populations with epilepsy as the denominators. Another explanation, the impact of the recent U.S. economic recession, is possible; a trend analysis from 54 countries (including 18 Western Hemisphere countries) has shown that, after the 2008 economic crisis, rates of suicide increased, particularly in men and in countries with higher job losses [33]. The economic crisis and its consequent unemployment, poverty, debt, and diminished public welfare could lead to depression [34], a major risk factor for suicide in people with epilepsy [35]. People with epilepsy have less education, a lower household income, poorer health status, and a higher unemployment rate than those without epilepsy [36], and depression affects 30–50% of individuals with epilepsy [37–39]. This socioeconomically and mentally vulnerable group therefore might be more subject to the negative impact of the 2008 U.S. economic crisis than the general population leading to this unusual peak in the suicide rate. However, further research is needed to confirm or refute this hypothesis.
This study has several limitations. First of all, the identification of epilepsy and seizure among suicide cases could have misclassified some suicide cases. In particular, the search for epilepsy/seizure in NVDRS may profoundly undercount the number of persons who died from suicide with epilepsy because suicide data from the NVDRS do not typically include previous medical records for the decedents; therefore, an epilepsy/seizure diagnosis may be missed unless it came up when investigators of violent deaths talked to those who may have known the decedent or may not have been recorded if the diagnosis was not viewed as a potential factor associated with the individual's death. On the other hand, some of the nonspecific words and phrases we searched for to identify those with epilepsy/seizure (e.g., “falling out spell”, “staring spell”, “drop attack”) could have referred to other conditions and thus lead to overestimates of the number of suicide cases attributed to persons with epilepsy. Second, we estimated the expected number of people with epilepsy in each state as denominators for our suicide rates among those with epilepsy based on two, national age-specific prevalence rate estimates, which may not be appropriate because incidence may differ by states. Third, NVDRS included data from only 17 states, not from the whole U.S. population. Fourth, the number of suicides was too few to compare suicide rates by various sociodemographic factors, such as race/ethnicity and socioeconomic status. Fifth, about half of the reports of persons who died from suicide lacked information about education. Finally, most people who die by suicide have comorbid psychiatric disorders [40]. Depression remains an important but underdiagnosed, common comorbidity of epilepsy that contributes to premature mortality seen in this population [41]. Further study is needed to examine associations between epilepsy–suicide and prior history of mental illness.
5. Conclusion
This is the first study to describe the basic epidemiology among people with epilepsy who died from suicide by systematically investigating the suicide burden and the sociodemographic characteristics of people with epilepsy in the general population. This study used large, population-based data from a unique U.S. data system, the NVDRS, which includes most suicides (from 2003 through 2011 in the 17 U.S. states; about one-third of the U.S. population) and comprehensive information that allows the identification of persons with epilepsy who died from suicide. Among those with epilepsy, this study estimated the suicide rate, evaluated the risk of suicide compared with that in the general population, investigated the suicide risk factors by socioeconomic characteristics, and described suicide trends.
To reduce suicide risk, in addition to those prevention measures proposed in the abovementioned discussion, providers should screen for and treat depression in people with epilepsy following appropriate recommendations and guidelines [42,43]. Suicide Safe, the US Substance Abuse and Mental Health Service Administration's suicide prevention app, helps providers integrate suicide prevention strategies into their practice [44]. Epilepsy health and social service providers can consider implementing evidence-based depression treatment interventions for adults with epilepsy and comorbid depression [45,46]. To prevent suicide among people with epilepsy, caregivers and other members of the public can participate in Mental Health First Aid, an evidence-based program that teaches people about mental illness and its symptoms and how to recognize and intervene during a mental health crisis [47]. Mental Health First Aid training is available in communities throughout the United States.
Finally, population-based surveillance targeting both epilepsy and suicide could be enhanced to allow further study of the epidemiology of suicide among different racial groups with epilepsy in the U.S. nationwide.
Supplementary Material
Acknowledgments
We wish to thank all contributors from participating state NVDRS; the International Association of Chiefs of Police; the National Institute for Occupational Safety and Health; and the National Center for Health Statistics, CDC. The authors are grateful to Dr. R. Matthew Gladden from the Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC for his invaluable contribution in abstracting the analytic dataset from the NVDRS and reviewing this manuscript.
Footnotes
Disclosure(s)
The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Disclosure of conflicts of interest
None of the authors have any conflicts of interest to disclose. We confirm that we have read the journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.yebeh.2016.05.028.
References
- 1.Centers for Disease Control and Prevention. Web-based injury query and reporting system (WISQARS) Accessed at: http://www.cdc.gov/injury/wisqars/fatal_injury_reports.html.
- 2.Hesdorffer DC, Ishihara L, Mynepalli L, Webb DJ, Weil J, Hauser WA. Epilepsy, suicidality, and psychiatric disorders: a bidirectional association. Ann Neurol. 2012;72:184–91. doi: 10.1002/ana.23601. [DOI] [PubMed] [Google Scholar]
- 3.Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case–control study. Lancet Neurol. 2007;6:693–8. doi: 10.1016/S1474-4422(07)70175-8. [DOI] [PubMed] [Google Scholar]
- 4.Bell GS, Gaitatzis A, Bell CL, Johnson AL, Sander JW. Suicide in people with epilepsy: how great is the risk? Epilepsia. 2009;50:1933–42. doi: 10.1111/j.1528-1167.2009.02106.x. [DOI] [PubMed] [Google Scholar]
- 5.Robertson M. Suicide, parasuicide, and epilepsy. In: Engel J, Pedley TA, editors. Epilepsy: a comprehensive textbook. Philadelphia: Lippincott-Raven; 1997. pp. 2141–57. [Google Scholar]
- 6.Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003;4(Suppl 3):S31–8. doi: 10.1016/j.yebeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Kwon C, Liu M, Quan H, Thoo V, Wiebe S, Jetté N. Motor vehicle accidents, suicides, and assaults in epilepsy. Neurology. 2011 Mar;76(1) doi: 10.1212/WNL.0b013e31820e7b3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nilsson L, Tomson T, Farahmand BY, Diwan V, Persson PG. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia. 1997;38:1062–8. doi: 10.1111/j.1528-1157.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Surveillance for violent deaths—National Violent Death Reporting System, 16 states, 2010. Morb Mortal Wkly Rep. 2014;63(1):1–33. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. National violent death reporting system. Accessed at http://www.cdc.gov/violenceprevention/nvdrs/index.html.
- 11.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129:256–64. doi: 10.1542/peds.2010-1371. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Epilepsy in adults and access to care—United States, 2010. Morb Mortal Wkly Rep. 2012;61(45):909–13. [PubMed] [Google Scholar]
- 13.Anderson DW, Schoenberg BS, Haerer AF. Prevalence surveys of neurologic disorders: methodologic implications of the Copiah County study. J Clin Epidemiol. 1988;41:339–45. doi: 10.1016/0895-4356(88)90141-2. [DOI] [PubMed] [Google Scholar]
- 14.Brooks DR, Avetisyan R, Jarrett KM, Hanchate A, Shapiro GD, Pugh MJ, et al. Validation of self-reported epilepsy for purposes of community surveillance. Epilepsy Behav. 2012;23:57–63. doi: 10.1016/j.yebeh.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Epilepsy surveillance among adults—19 states, Behavioral Risk Factor Surveillance System, 2005. Morb Mortal Wkly Rep. 2008;57(6):1–20. [PubMed] [Google Scholar]
- 16.United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin. Compiled from 1990–1999 bridged-race intercensal population estimates (released by NCHS on 7/26/2004); revised bridged-race 2000–2009 intercensal population estimates (released by NCHS on 10/26/2012); and bridged-race vintage 2014 (2010–2014) postcensal population estimates (released by NCHS on 6/30/2015) Available on CDC WONDER Online Database. Accessed at http://wonder.cdc.gov/bridged-race-v2014.Html.
- 17.Pompili M, Girardi P, Tatarelli R. Death from suicide versus mortality from epilepsy in the epilepsies: a meta-analysis. Epilepsy Behav. 2006;9:641–8. doi: 10.1016/j.yebeh.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple cause of death 1999–2013 on CDC WONDER online database, released 2015. [on Aug 12, 2015 11:47:01 am];Data are from the multiple cause of death files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the vital statistics cooperative program. Accessed at http://wonder.cdc.gov/mcd-icd10.Html.
- 19.Moscicki EK. Identification of suicide risk factors using epidemiologic studies. Psychiatr Clin N Am. 1997;20:499–517. doi: 10.1016/s0193-953x(05)70327-0. [DOI] [PubMed] [Google Scholar]
- 20.Christiansen E, Stenager E. Risk for attempted suicide in children and youths after contact with somatic hospitals: a Danish register-based nested case–control study. J Epidemiol Community Health. 2012;66:247–53. doi: 10.1136/jech.2009.103887. [DOI] [PubMed] [Google Scholar]
- 21.Nilsson L, Ahlbom A, Farahmand BY, Asberg M, Tomson T. Risk factors for suicide in epilepsy: a case control study. Epilepsia. 2002;43:644–51. doi: 10.1046/j.1528-1157.2002.40001.x. [DOI] [PubMed] [Google Scholar]
- 22.Seo JG, Lee JJ, Cho YW, Lee SJ, Kim JE, Moon HJ, et al. Suicidality and its risk factors in Korean people with epilepsy: a MEPSY study. J Clin Neurol. 2015;11:32–41. doi: 10.3988/jcn.2015.11.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackay A. Self-poisoning—a complication of epilepsy. Br J Psychiatry. 1979;134:277–82. doi: 10.1192/bjp.134.3.277. [DOI] [PubMed] [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services. A guide for taking care of your family member after treatment in the emergency department. Accessed at http://store.samhsa.gov/shin/content//SMA08-4357/SMA08-4357.pdf.
- 25.Hawton K, Fagg J, Marsack P. Association between epilepsy and attempted suicide. J Neurol Neurosurg Psychiatry. 1980;43:168–70. doi: 10.1136/jnnp.43.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helmers SL, Thurman DJ, Durgin TL, Pai AK, Faught E. Descriptive epidemiology of epilepsy in the U.S. population: a different approach. Epilepsia. 2015;56:942–8. doi: 10.1111/epi.13001. [DOI] [PubMed] [Google Scholar]
- 27.Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the “common” neurologic disorders? Neurology. 2007;68:326–37. doi: 10.1212/01.wnl.0000252807.38124.a3. [DOI] [PubMed] [Google Scholar]
- 28.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–5. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 29.Kobau R, Zahran H, Grant D, Thurman DJ, Price PH, Zack MM. Prevalence of active epilepsy and health-related quality of life among adults with self-reported epilepsy in California: California health interview survey, 2003. Epilepsia. 2007;48:1904–13. doi: 10.1111/j.1528-1167.2007.01161.x. [DOI] [PubMed] [Google Scholar]
- 30.Elliott JO, Lu B, Moore JL, McAuley JW, Long L. Exercise, diet, health behaviors, and risk factors among persons with epilepsy based on the California Health Interview Survey, 2005. Epilepsy Behav. 2008;13:307–15. doi: 10.1016/j.yebeh.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Elliott JO, Charyton C, Sprangers P, Lu B, Moore JL. The impact of marriage and social support on persons with active epilepsy. Epilepsy Behav. 2011;20:533–8. doi: 10.1016/j.yebeh.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 32.Szaflarski M. Social determinants of health in epilepsy. Epilepsy Behav. 2014;41:283–9. doi: 10.1016/j.yebeh.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 33.Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013;347:f5239. doi: 10.1136/bmj.f5239. [1–15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Depression and the global economic crisis: is there hope? Lancet. 2012;380:1203. doi: 10.1016/S0140-6736(12)61694-8. Editorial. [DOI] [PubMed] [Google Scholar]
- 35.Hecimovic H, Santos JM, Carter J, Attarian HP, Fessler AJ, Vahle V, et al. Depression but not seizure factors or quality of life predicts suicidality in epilepsy. Epilepsy Behav. 2012;24:426–9. doi: 10.1016/j.yebeh.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elliott JO, Lu B, Shneker BF, Moore JL, McAuley JW. The impact of ‘social determinants of health’ on epilepsy prevalence and reported medication use. Epilepsy Res. 2009;84:135–45. doi: 10.1016/j.eplepsyres.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Swinkels WA, Kuyk J, van Dyck R, Spinhoven P. Psychiatric comorbidity in epilepsy. Epilepsy Behav. 2005;7:37–50. doi: 10.1016/j.yebeh.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 38.Kanner AM. Depression in epilepsy: a frequently neglected multifaceted disorder. Epilepsy Behav. 2003;4(Suppl 4):11–9. doi: 10.1016/j.yebeh.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 39.Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanisms, and treatment. Biol Psychiatry. 2003;54:388–98. doi: 10.1016/s0006-3223(03)00469-4. [DOI] [PubMed] [Google Scholar]
- 40.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 41.Noe KH, Locke DE, Sirven JI. Treatment of depression in patients with epilepsy. Curr Treat Options Neurol. 2011;13(4):371–9. doi: 10.1007/s11940-011-0127-8. [DOI] [PubMed] [Google Scholar]
- 42.US Preventive Services Task Force. Final Recommendation Statement Depression in Adults: Screening. 2009 Dec; [Available at:] http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/depression-in-adults-screening.
- 43.Kanner AM. The treatment of depressive disorders in epilepsy: what all neurologists should know. Epilepsia. 2013;54(Suppl 1):3–12. doi: 10.1111/epi.12100. [DOI] [PubMed] [Google Scholar]
- 44.SAMHSA. Suicide safe: the suicide prevention app for health care providers. [Internet] Available at http://store.samhsa.gov/apps/suicidesafe/
- 45.Chaytor N, Ciechanowski P, Miller JW, Fraser R, Russo J, Unutzer J, et al. Long-term outcomes from the PEARLS randomized trial for the treatment of depression in patients with epilepsy. Epilepsy Behav. 2010;20(3):545–9. doi: 10.1016/j.yebeh.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 46.Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, DiIorio C, et al. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy Behav. 2010;19:247–54. doi: 10.1016/j.yebeh.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 47.Mental Health First Aid USA. [Internet]. Available at: http://www.mentalhealthfirstaid.org/cs/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


