Abstract
Introduction
Latina women have a high burden of depression and other mental health issues particularly in the perinatal period. Suboptimal maternal mental health can have adverse developmental and physiological impacts on child growth. The present study examines the impact of unplanned pregnancy and pregnancy relationship status on prenatal maternal depression in a sample of low-income Latina women. We hypothesized that the association between these prenatal stressors and newborn health would be mediated through prenatal depression.
Method
The present study included a sample 201 Latina mothers and their children recruited from prenatal clinics during their second or third trimesters. Depression symptomology, relationship status were collected prenatally. At birth, several indices of newborn health were examined, including head circumference percentile and birthweight. Finally, planned pregnancy status was retrospectively collected when the child was between 1 and 2 years old.
Results
Structural equation modeling revealed that single women, compared to partnered women, had higher levels of depression. Higher levels of depression, in turn, predicted poorer newborn health. Unplanned pregnancy was not significantly associated with newborn health.
Discussion
These results suggest that relationship status may be an important screening question for medical examiners to ask to pregnant Latina women during prenatal visits. These results are consistent with past research investigating the effects of maternal mental health on adverse birth outcomes that propose that stressful early environments shape developmental trajectories.
Keywords: Depression, Infant Health, Latinos, life history theory, planned pregnancy, relationship status
INTRODUCTION
Pregnancy can engender intense physical and emotional upheavals in women. Psychosocial and cultural factors may not only exacerbate or diminish pregnancy-related stressors (Dunkel Schetter, 2011), but may buffer their effects on pregnancy outcome. Evolutionary perspectives (Ellis, 2004; Hrdy, 2000) suggest that instrumental and social support from one’s partner and family are of importance and can impact child health and development (Ellis, 2004; Flinn, 2006). The intense physiological and temporal burden of pregnancy orients women to be selective of when and with whom they have a child (Ellison, 2003; Trivers, 1972). Medical anthropological frameworks similarly emphasize the role men play as mates and fathers in matters of maternal and infant health (Dudgeon and Inhorn, 2004). Succinctly put, the men as partners framework posits that men, directly and indirectly, help shape the health of women and infants during pregnancy (Dudgeon and Inhorn, 2004).
The impact of father presence (i.e., maternal relationship status) and maternal relationship health on physical development, interpreted through an evolutionary perspective, has been mainly focused on physical health and development in adolescence (Ellis et al., 1999; Ellis and Garber, 2000). For instance, both maternal mental health and father absence was implicated in early pubertal development in girls. As such, we argue that the effects of father presence (i.e., maternal relationship status), may have a similar effect on physical health in newborns, through maternal mental health.
Maternal mental health and the presence of prenatal stressors are critical in shaping newborn health (Diego et al., 2006; Dole, 2003; Grote et al., 2010). Depression may play an especially important role for Latina women given findings that the prevalence of depression among pregnant Latinas is at 32.4% (Lara et al., 2009). Additionally, current theoretical conceptualizations propose that maternal mental health during pregnancy may communicate or convey contextual information to the developing child regarding the quality of the psychosocial environment (Del Giudice, 2012; Dunkel Schetter and Tanner, 2012). The quality or supportiveness of the psychosocial context (conveyed through maternal mental health) should impact infant well-being.
For this reason, we investigate in a sample of Latina women two prenatal stressors that capture the condition of the mother’s environment and indicate whether her social support and material resources are sufficient. The current study investigates the effects of two common stressors on prenatal depression – maternal relationship status and planned pregnancy status – and the impact of depression on newborn health in a sample of low-income Latina women. Both single motherhood and an unwanted or unplanned pregnancy have been linked to neonatal mortality and poorer maternal and child health (Angel and Worobey, 1988; Berkman et al., 2015; Gaudino et al., 1999). Infants without a reported father on their birth certificate were at increased risk for infant mortality, when controlling for other risk factors (Gaudino et al., 1999). We hypothesized that:
Single women and women reporting an unplanned pregnancy will report greater depression than women in relationships or women reporting planned pregnancies,
Greater maternal depression will predict poorer newborn health,
Maternal depression will mediate the relationship between maternal relationship status and unplanned pregnancies with newborn health.
METHOD
Participants
Two-hundred and one mothers and their newborns (50% female) participated in the current study. The mothers were all Latina (37.32% South/Central American; 61.19% Mexican; 1.00% Puerto Rican, and 0.50% other) with a mean age of 34.6 (SD = 5.10; range = 25–55). Maternal marital status prior to the birth of their child was as follows: cohabiting, 52.79%; married, 31.47%, divorced, 1.02%; single, 14.72%; 4 cases were missing). The majority of the mothers reported speaking primarily Spanish (93.5%; English, 6.5%), not having formal employment (71.64%; employed, 28.36%), being enrolled in the Women Infants and Children’s program (WIC, 92.04%; no WIC, 7.96%) and having a high school education (77.55%; some college, 17.35%; College, 3.05%; Post-college, 2.04%). Most women in the sample were first time mothers (47.26; 1 child, 30.85%; 2 children, 15.42%; 3 children, 4.98%; 4 children, 1.0% 5 children, 0.50%). The majority of the women who answered whether the pregnancy was planned reported it as not being planned (57.06%; the pregnancy was planned, 42.94; 38 cases did not report this). The sample used in the present secondary data analysis has been previously described (Wojcicki et al., 2011a, 2011b).
Procedures
The study and its procedures were approved by the Committee on Human Research and the Institutional Review Board at University of California, San Francisco and San Francisco General Hospital (SFGH). Pregnant women who were in their second or third trimesters were recruited from prenatal clinics at UCSF and San Francisco General Hospital, California between May 2006 and May 2007. Written consent was obtained from all women in either Spanish or English. Women were ineligible to participate in the study if they: were abusing drugs/alcohol, had a history of diabetes or presently were experiencing gestational diabetes, suffered from polycystic ovarian syndrome, had an eating disorder or another health issue that could impact breast-feeding. If infants of the mother had special care needs or had an Apgar score below 7 at five minutes after delivery, the family was excluded from the study. Women were interviewed by trained research assistants. The research assistants were all fluent in Spanish, had university degrees and had received training from the committee on Human Research on human subjects protection training. See Wojcicki, et al.(2011a, 2011b), for more information about the sample or procedure.
Missing Data Analysis
Missing data on the variables of interest ranged from 4 to 38 cases. Individuals with missing data did not significantly differ from those not missing data on total Center for Epidemiologic Studies Depression Scale score (p = .4174), and total Edinburgh Postnatal Depression Scale score (p = .6275). Individuals with more education (r = .16, p <.03) and English speakers (r = .16, p <.02) were more likely to have missing data. Planned pregnancy question was individually examined for missingness because it had the most missing data. Women with higher levels of education were more likely to not answer the planned pregnancy question (r = .18, p < .01). Missing cases were handled with Robust Maximum likelihood estimation.
Screening for Covariates
Prior to computing Structural Equation Models, we examined possible maternal and sociodemographic confounders that may impact infant health. We ran multiple regression models of covariates predicting components of newborn health and included relationship status and planned pregnancy status (see Supplemental Table S1). The models predicting birth weight, F (11, 127) = 0.92, p = .52, and head circumference, F (11, 120) = 1.50, p = .14, were both non-significant. The covariate model predicting gestational age was significant, F (11, 124) = 1.86, p = .05. The only covariate that significantly predicted head circumference was maternal employment status at pregnancy. Women who reported being employed (yes = 1) had babies with younger gestational age (β = −.31, p < .001). Based on these results, we included employment status (yes, employed/no, not employed) as a covariate in a sub-analysis of our model.
Measures
Maternal Relationship Status
Maternal prenatal relationship status was dichotomously coded to represent whether the mother was single (i.e., single or divorced) or in a relationship (i.e., married or cohabiting). Women who reported being single or divorced were coded as being single (0); women who reported being married or in a cohabiting relationship were coded as being in a relationship (1).
Planned Pregnancy
Planned pregnancy was a dichotomous one-item question (“Had you planned beforehand to become pregnant at that time?”) asking mothers to report whether the pregnancy was planned (“Yes, I had planned to become pregnant” = 1) or not planned (“No, I didn’t plan to become pregnant” = 0). The question was collected retrospectively, when the children were 12 months to 2 years.
Depression
Mother’s level of prenatal depression was assessed utilizing two measures of depression: (1) Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), and (2) Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987). The CES-D (α = .88) consisted of twenty items scored on a 4-point scale from “Rarely or none of the time, <1 day” (0) to “Most of the time, 5–7 days” (3). The EPDS (α = .80) consisted of ten items scored on a 4-point scale, with appropriate items reversed-coded. Higher scores on each of the scales denoted higher levels of depression symptomology.
Newborn Health
Previous health research provided the justification for the aggregation of sets of variables. For instance, aggregated constructs that capture mental and physical health-enhancing factors, such as slow life history in adulthood (Figueredo et al., 2005), ideal cardiovascular health (Lloyd-Jones et al., 2010), and multi-system resiliency (Puterman and Epel, 2012), have been used as outcomes and predictors in prior models of health. Likewise, the creation of health-risking indices has also been used. The most notable example is the allostatic load, which captures concerted dysregulation across various physiological systems (Seeman et al., 2009). As such, the creation of our latent factor for newborn health is informed by past research in pediatrics that find that birth weight and head circumference are early markers of chronic disease risk, such as cardiovascular disease (Barker et al., 1993). Tenets from life history theory (e.g., Flinn et al., 2011) also guided the selection of our items. Two items were selected: (1) birth weight and (2) head circumference, both standardized using guidelines prescribed by the Center for Disease Control (Grummer-Strawn et al., 2010). Greater birth weight and larger head circumference were indicative of better newborn health. Gestational age was used as a covariate of newborn health.
Statistical Analyses
Structural Equation Modeling was performed in Mplus 6. Model fit was assessed by χ2, Comparative Fit Index (CFI), and Root Squared Error of Approximation. Values >0.95 signifies appropriate goodness-of-fit in CFI; values at ≤0.05 appropriate in RMSEA.
RESULTS
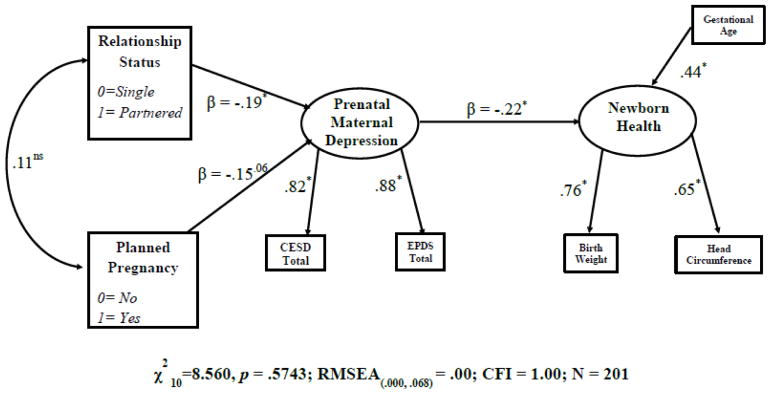
Table 1 displays bivariate correlations for the indicator variables and Figure 1 reports the findings of the structural equation model, including fit indices and standardized parameter estimates for the final model, all which were acceptable. As predicted, relationship status significantly predicted prenatal depression; partnered women reported lower levels of depression (β = −.19, p =.02). Women whose pregnancies had been planned reported less depression prenatally, although the difference was of borderline significance (β = −.15, p = .06). Also as predicted, increased depression predicted poorer newborn health (β = −.22, p = .01). Neither relationship status nor planned pregnancy directly correlated with newborn health.
Table 1.
Descriptive Statistics and Bivariate Correlation of Manifest Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Relationship Status | -- | ||||||
| 2. Planned Pregnancy | .12 | -- | |||||
| 3. CESD | −.17* | −.18* | -- | ||||
| 4. EPDS | −.15* | −.12 | .76** | -- | |||
| 5. Gestational Age | .03 | −.10 | −.03 | −.08 | -- | ||
| 6. Birth Weight1 | .08 | −.04 | −.08 | −.15* | .41** | -- | |
| 7. Head Circumference | .07 | .03 | −.11 | −.17* | .27** | .49** | -- |
|
| |||||||
| Mean or % | 84.26% | 42.94% | 11.65 | 5.63 | 39.30 | −0.17 | 34.20 |
| Standard Deviation | - | - | 9.73 | 4.82 | 1.52 | 1.01 | 2.24 |
p < .05;
p < .01.
Significant correlations are bolded.
Birth weight was standardized based on CDC guidelines
Figure 1.
Structural Equation Model investigating the pathway from Maternal Stressors, Prenatal Depression, and Newborn Health, after Robust Maximum Likelihood Estimation, Standardized Estimates.
Sub-analysis Models
Based on the results of the multiple regression models previously described, maternal employment status was included to predict newborn health. Fit indices were good and factor loadings were appropriate, χ221 = 26.3084, p = .1949; RMSEA =.0355; CFI = .9827; NFI = .9232. The pathway of planned pregnancy to depression was the same magnitude as before but missed significance (β = −.14, p = .07). Relationship status to depression was also the same magnitude and significant (β = −.16, p < .03). Both pathways leading to newborn health were non-significant with the inclusion of employment status (depression; β = −.14, p = .10 and employment status; β = −.15, p = .07).
A model was computed including direct pathways from planned pregnancy and relationship status to newborn health (with and without prenatal depression in the model). The pathways were non-significant. Finally, an SEM model that included an interactive term between relationship status and planned pregnancy yielded a non-significant pathway to maternal depression (β = .31, p = .16).
DISCUSSION
A process model was tested whereby prenatal stressors influenced newborn health via maternal prenatal depression in Latina mothers and their newborns (N = 201). Because previous research indicated that father presence and access to resources may affect physical health and development in childhood and adolescence (Del Giudice et al., 2011; Ellis, 2004; Flinn, 2006), we tested a similar model on newborn physical health. We hypothesized that unplanned pregnancy status and the absence of a romantic partner would lead to higher levels of maternal depression in the mothers. Higher levels of prenatal maternal depression would predict poorer newborn health.
The structural equation model revealed that relationship status – the presence or absence of the mother’s partner – significantly predicted maternal depression. In households where no partner was present, women reported higher levels of depression. However, relationship status was not independently associated with newborn health. The model additionally revealed a non-significant negative association between planned pregnancy and maternal depression (e.g., if the pregnancy was unplanned, the mothers reported higher levels of depression). Covariates were screened and maternal prenatal employment status included as a covariate. The model including a pathway between employment status to newborn health was non-significant. Inclusion of employment status in the model also produced a non-significant pathway between depression to newborn health. This suggests that women who are working may be experiencing additional stressors that are directly impacting the health of their children.
These results are of particular interest to midwives and doulas because it underscores the importance of social support on maternal mental health during the process and experience of pregnancy. Previous scholars have asserted that midwives play a significant role in identifying the quality of social support available to the pregnant women and also providing social support to mothers before and after pregnancy (Bogossian, 2007).
Quality of the Psychosocial Environment
Based on extant frameworks, indicators reflecting quality of the maternal psychosocial environment (Dudgeon and Inhorn, 2004; Dunkel Schetter and Tanner, 2012; Ellis, 2004) were highlighted as areas to consider when examining maternal stress during pregnancy: (1) presence of a partner during pregnancy and (2) planned pregnancy status. Both stressors may signify a deficit of psychosocial and/or instrumental support. Culture and family interactions also modulate how Latinas approach parenting and child care (Garcia Coll, 1990). A deficit of social support from partners and family members and an increase in maternal depression and anxiety have been associated with adverse birth outcomes (Dunkel Schetter, 2011). In addition to psychosocial support, men may be providing indirect aid to the mother and the infant during pregnancy through financial means or by performing extra household tasks that allow the mother to seek prenatal care (Casper and Hogan, 1990).
An alternative interpretation of the results could be that women who work during pregnancy may be experiencing stressors associated with their job. A meta-analysis of 29 studies found links between physically challenging work environments – “heavy and/or repetitive lifting or load carrying, manual labor, or significant physical exertion” – preterm birth, and small-for-gestational age outcomes in newborns (Mozurkewich et al., 2000, p. 624). Further, when controlling for maternal characteristics and sociodemographic covariates, women who reported having high job strain (high job demand and low/moderate job control) or worked greater than 32 hours a week had a decrease in infant birth weight (Vrijkotte et al., 2009). Independent of psychosocial forces in the household, work stressors may uniquely, and directly, impact newborn health. While the present study only focused on a few environmental stressors, we suggest that future research continue widen the scope to include more environmental and pregnancy-related stressors, and more nuanced measurement of those constructs.
Transmission of Ecological Stressors to Children
A larger question remains about the findings: Why would nature create infants susceptible to transmitted prenatal stressors from the mother? Biosocial theories suggest that maternal mental condition transmits salient information to infants pertaining to the quality of the maternal psychosocial environment (Del Giudice, 2012; Kuzawa, 2007). The information received by the infant provides relevant cues that shape developmental and lifetime trajectories. For instance, predictable, low stress environments foster households whereby mothers can invest her time, energy and physiology in a smaller amount of children, increasing health and competitiveness of the children (Ellis et al., 2009). Findings regarding prenatal stress support this hypothesis. When women report having higher levels of psychological resources (mastery, optimism, and self-esteem), those resources directly decrease stress and directly increase infant birth weight(Rini et al., 1999). Similarly, positive attitudes toward the pregnancy predicts higher infant birthweight(Zambrana et al., 1999).
Life history models of development assert that early exposure to unpredictable environments and extrinsic stress alter developmental trajectories that orients physical and social development to “fit” the environment the child resides in (Belsky et al., 1991; Ellis et al., 2009; see Cabeza de Baca et al., 2016 for a discussion). Fetal programming is one possible mechanism that transmits stressors, impacting development and health trajectories in adulthood (Del Giudice, 2012; Kuzawa, 2007; Shonkoff et al., 2012). Using an evolutionary or another ecobiodevelopmental framework (Shonkoff et al., 2012, 2009) suggests that these findings be considered when investigating the developmental origins of health and disease (DOHaD), which have found associations between adverse birth outcomes, such as low birth weight, and chronic diseases such as metabolic(Norris et al., 2012) and cardiovascular disorders (Risnes et al., 2011) (See Kuzawa(2007) for a review).
Future Directions and Clinical Implications
Data were longitudinal, emphasizing the developmental processes involved in the ontogeny of minority children(Garcia Coll et al., 1996) and demonstrating the temporal effects of depression on newborn health in Latina mothers. Further, the use of latent measures of depression and newborn health in structural equation modeling are also strengths of the study.
While the results of the present study have implications regarding maternal mental health and adverse birth outcomes, there are limitations. One limitation was that there were no measures of socioeconomic status. Chronic stressors such as discrimination, disproportionate access to resources and institutions, and employment are important concepts in pregnancy-related anxiety research (Dunkel Schetter, 2011; Dunkel Schetter and Tanner, 2012) and in minority process models of development (Garcia Coll et al., 1996). For that reason, future research should continue to include them. Another limitation involves the conceptualization of social support among Latina mothers. The present study utilized a dichotomous measure of relationship status (single vs. partnered) as a proxy for father support. Future research should include better, nuanced measures of social support (e.g., Campos et al., 2008) and include extended kin, who may provide supplementary assistance to the mother in Latinas (e.g., Barnett et al., 2015).
Further, research on extended kin support should disentangle the social support received from maternal (mother’s family) and paternal (father’s family) kin and whether partner conflict predicts contributions from both families. Because not all partners may be supportive, it may be possible that depressive symptoms are dampened by the presence of strong familial and friend bonds. Further research may also want to incorporate a continuous measure of planned/unplanned pregnancy (e.g., the London measure of unplanned pregnancy; Barrett et al., 2004) to investigate whether the degree or magnitude of the unplanned pregnancy has an effect on newborn health outcomes. Future research should also examine other measures of psychosocial functioning and distress, such as perceived stress and anxiety, in addition to depression.
Based on the results of our study, we suggest that maternity care providers, physicians, or midwives caring for pregnant women assess access to social support and depressive symptoms – especially among immigrant and/or single women. This could include early pregnancy mental health screening and referring high-risk women to counselors and/or other organizations that may provide care, support and resources to mitigate the effects of maternal depression on newborns.
Supplementary Material
Highlights.
Maternal mental health conveys the quality of the psychosocial environment.
Theory suggests the child will develop based on the information conveyed.
Impact of relationship status and planned pregnancy on depression were examined.
Being single indirectly affected child health through prenatal depression.
Pregnancy-related stressors may be important to probe by physicians.
Acknowledgments
Funding Sources
This work was supported by the National Institute of Health grant T32MH019391 to the first author. This work was also supported in part by grants from the Hellman Family Foundation, the Children’s Digestive Health and Nutrition Foundation (CDHF), NIH grant DK060617, DK080825 and by NIH/NCRR UCSF-CTSI Grant Number UL1 RR024131.
Biographies
Tomás Cabeza de Baca, PhD, is currently a postdoctoral fellow in the Division of Cardiology at the University of California, San Francisco.
Janet Wojcicki, PhD MPH, is an Associate Professor in the Department of Pediatrics at the University of California, San Francisco.
Elissa Epel, PhD, is a Professor in the Department of Psychiatry and Director of the Aging, Metabolism, and Emotions Lab at the University of California, San Francisco.
Nancy E. Adler, PhD, is the director of both the Center for Health and Community (CHC) and the “Psychology and Medicine: Translational Research on Stress, Behavior and Disease” at the University of California, San Francisco.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Ethical Approval: The study and its procedures were approved by the Committee on Human Research and the Institutional Review Board at University of California, San Francisco and San Francisco General Hospital (SFGH).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tomás Cabeza de Baca, CeNter for StUdy of AdveRsiTy and CardiovascUlaR DiseasE (NURTURE Center), Division of Cardiology, University of California, San Francisco CA.
Janet M. Wojcicki, Division of Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, University of California, San Francisco.
Elissa S. Epel, UCSF Center for Obesity Assessment, Study, & Treatment, Department of Psychiatry, University of California San Francisco.
Nancy E. Adler, Center for Health and Community, Department of Psychiatry, University of California, San Francisco.
References
- Angel R, Worobey JL. Single motherhood and children’s health. J Health Soc Behav. 1988;29:38. doi: 10.2307/2137179. [DOI] [PubMed] [Google Scholar]
- Barker DJ, Osmond C, Simmonds SJ, Wield GA. The relation of small head circumference and thinness at birth to death from cardiovascular disease in adult life. BMJ. 1993;306:422–426. doi: 10.1136/bmj.306.6875.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett MA, Cabeza de Baca T, Jordan A, Tilley E, Ellis BJ. Associations among child perceptions of parenting support, maternal parenting efficacy and maternal depressive symptoms. Child Youth Care Forum. 2015;44:17–32. doi: 10.1007/s10566-014-9267-9. [DOI] [Google Scholar]
- Barrett G, Smith SC, Wellings K. Conceptualisation, development, and evaluation of a measure of unplanned pregnancy. J Epidemiol Community Health. 2004;58:426–433. doi: 10.1136/jech.2003.014787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Steinberg L, Draper P. Childhood Experience, Interpersonal Development, and Reproductive Strategy: An Evolutionary Theory of Socialization. Child Dev. 1991;62:647–670. doi: 10.1111/j.1467-8624.1991.tb01558.x. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Zheng Y, Glymour MM, Avendano M, Börsch-Supan A, Sabbath EL. Mothering alone: cross-national comparisons of later-life disability and health among women who were single mothers. J Epidemiol Community Health. 2015;69:865–872. doi: 10.1136/jech-2014-205149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogossian FE. Social support: Proposing a conceptual model for application to midwifery practice. Women Birth. 2007;20:169–173. doi: 10.1016/j.wombi.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Cabeza de Baca T, Wahl RA, Barnett MA, Figueredo AJ, Ellis BJ. Adversity, adaptive calibration, and health: The case of disadvantaged families. Adapt Hum Behav Physiol. 2016;2:93–115. doi: 10.1007/s40750-016-0042-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos B, Schetter CD, Abdou CM, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: Positive implications for pregnant Latinas. Cultur Divers Ethnic Minor Psychol. 2008;14:155–162. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casper LM, Hogan DP. Family networks in prenatal and postnatal health. Biodemography Soc Biol. 1990;37:84–101. doi: 10.1080/19485565.1990.9988749. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Del Giudice M. Fetal programming by maternal stress: Insights from a conflict perspective. Psychoneuroendocrinology. 2012;37:1614–1629. doi: 10.1016/j.psyneuen.2012.05.014. [DOI] [PubMed] [Google Scholar]
- Del Giudice M, Ellis BJ, Shirtcliff EA. The adaptive calibration model of stress responsivity. Neurosci Biobehav Rev. 2011;35:1562–1592. doi: 10.1016/j.neubiorev.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diego MA, Jones NA, Field T, Hernandez-Reif M, Schanberg S, Kuhn C, Gonzalez-Garcia A. Maternal psychological distress, prenatal cortisol, and fetal weight. Psychosom Med. 2006;68:747–753. doi: 10.1097/01.psy.0000238212.21598.7b. [DOI] [PubMed] [Google Scholar]
- Dole N. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- Dudgeon MR, Inhorn MC. Men’s influences on women’s reproductive health: medical anthropological perspectives. Soc Sci Med. 2004;59:1379–1395. doi: 10.1016/j.socscimed.2003.11.035. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25:141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ. Timing of pubertal maturation in girls: an integrated life history approach. Psychol Bull. 2004;130:920. doi: 10.1037/0033-2909.130.6.920. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Figueredo AJ, Brumbach BH, Schlomer GL. Fundamental Dimensions of Environmental Risk: The Impact of Harsh versus Unpredictable Environments on the Evolution and Development of Life History Strategies. Hum Nat. 2009;20:204–268. doi: 10.1007/s12110-009-9063-7. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Garber J. Psychosocial antecedents of variation in girls’ pubertal timing: Maternal depression, stepfather presence, and marital and family stress. Child Dev. 2000;71:485–501. doi: 10.1111/1467-8624.00159. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, McFadyen-Ketchum S, Dodge KA, Pettit GS, Bates JE. Quality of early family relationships and individual differences in the timing of pubertal maturation in girls: A longitudinal test of an evolutionary model. J Pers Soc Psychol. 1999;77:387–401. doi: 10.1037/0022-3514.77.2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison PT. On Fertile Ground. Harvard University Press; Cambridge: 2003. [Google Scholar]
- Figueredo AJ, Vásquez G, Brumbach BH, Sefcek JA, Kirsner BR, Jacobs WJ. The K-factor: Individual differences in life history strategy. Personal Individ Differ. 2005;39:1349–1360. doi: 10.1016/j.paid.2005.06.009. [DOI] [Google Scholar]
- Flinn M. Evolution and ontogeny of stress response to social challenges in the human child. Dev Rev. 2006;26:138–174. doi: 10.1016/j.dr.2006.02.003. [DOI] [Google Scholar]
- Flinn MV, Nepomnaschy PA, Muehlenbein MP, Ponzi D. Evolutionary functions of early social modulation of hypothalamic-pituitary-adrenal axis development in humans. Neurosci Biobehav Rev. 2011;35:1611–1629. doi: 10.1016/j.neubiorev.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Garcia Coll C, Crnic K, Lamberty G, Wasik BH, Jenkins R, Garcia HV, McAdoo HP. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996;67:1891–1914. doi: 10.1111/j.1467-8624.1996.tb01834.x. [DOI] [PubMed] [Google Scholar]
- Garcia Coll CT. Developmental utcome of minority infants: A process-oriented Look into our beginnings. Child Dev. 1990;61:270–289. doi: 10.1111/j.1467-8624.1990.tb02779.x. [DOI] [PubMed] [Google Scholar]
- Gaudino JA, Jenkins B, Rochat RW. No fathers’ names: a risk factor for infant mortality in the State of Georgia, USA. Soc Sci Med. 1999;48:253–265. doi: 10.1016/S0277-9536(98)00342-6. [DOI] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67:1012. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grummer-Strawn LM, Reinold CM, Krebs NF Centers for Disease Control. Use of World Health Organization and CDC growth charts for children aged 0-59 months in the United States. Morb Mortal Wkly Rep MMWR. 2010;59:1–15. [PubMed] [Google Scholar]
- Hrdy SB. Mother nature: maternal instincts and how they shape the human species. Ballantine Books; New York: 2000. 1st Ballantine Books ed. ed. [Google Scholar]
- Kuzawa CW. Developmental origins of life history: Growth, productivity, and reproduction. Am J Hum Biol. 2007;19:654–661. doi: 10.1002/ajhb.20659. [DOI] [PubMed] [Google Scholar]
- Lara MA, Le HN, Letechipia G, Hochhausen L. Prenatal depression in Latinas in the U.S. and Mexico. Matern Child Health J. 2009;13:567–576. doi: 10.1007/s10995-008-0379-4. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Mozurkewich E, Luke B, Avani M, Wolf FM. Working conditions and adverse pregnancy outcome: A meta-analysis. Obstet Gynecol. 2000;95:623–635. doi: 10.1016/S0029-7844(99)00598-0. [DOI] [PubMed] [Google Scholar]
- Norris SA, Osmond C, Gigante D, Kuzawa CW, Ramakrishnan L, Lee NR, Ramirez-Zea M, Richter LM, Stein AD, Tandon N, Fall CHD the COHORTS Group. Size at Birth, Weight Gain in Infancy and Childhood, and Adult Diabetes Risk in Five Low- or Middle-Income Country Birth Cohorts. Diabetes Care. 2012;35:72–79. doi: 10.2337/dc11-0456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puterman E, Epel E. An intricate dance: life experience, multisystem resiliency, and rate of telomere decline throughout the lifespan. Soc Personal Psychol Compass. 2012;6:807–825. doi: 10.1111/j.1751-9004.2012.00465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18:333–345. doi: 10.1037/0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- Risnes KR, Vatten LJ, Baker JL, Jameson K, Sovio U, Kajantie E, Osler M, Morley R, Jokela M, Painter RC, Sundh V, Jacobsen GW, Eriksson JG, Sørensen TIA, Bracken MB. Birthweight and mortality in adulthood: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:647–661. doi: 10.1093/ije/dyq267. [DOI] [PubMed] [Google Scholar]
- Seeman T, Gruenewald T, Karlamangla A, Sidney S, Liu K, Mcewen B, Schwartz J. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am J Hum Biol. 2009;22:463–472. doi: 10.1002/ajhb.21018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities: Building a New Framework for Health Promotion and Disease Prevention. JAMA. 2009;301:2252. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, Garner AS, McGuinn L, Pascoe J, Wood DL The Committee on psychosocial aspects of child and family health, Committee on early childhood, adoption, and dependent care, and section on developmental and behavioral pediatrics. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Trivers R. Parental investment and sexual selection. In: Campbell BG, editor. Sexual Selection & the Descent of Man, 1871-19. Aldine de Gruyter; New York: 1972. pp. 136–179. [Google Scholar]
- Vrijkotte TGM, van der Wal MF, van Eijsden M, Bonsel GJ. First-trimester working conditions and birthweight: A prospective cohort study. Am J Public Health. 2009;99:1409–1416. doi: 10.2105/AJPH.2008.138412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojcicki JM, Holbrook K, Lustig RH, Caughey AB, Muñoz RF, Heyman MB. Infant formula, tea, and water supplementation of Latino infants at 4-6 weeks postpartum. J Hum Lact. 2011a;27:122–130. doi: 10.1177/0890334410396510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojcicki JM, Holbrook K, Lustig RH, Epel E, Caughey AB, Muñoz RF, Shiboski SC, Heyman MB. Chronic maternal depression Is associated with reduced weight gain in Latino infants from birth to 2 years of age. PLoS ONE. 2011b;6:e16737. doi: 10.1371/journal.pone.0016737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrana RE, Dunkel-Schetter C, Collins NL, Scrimshaw SC. Mediators of ethnic-associated differences in infant birth weight. J Urban Health. 1999;76:102–116. doi: 10.1007/BF02344465. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.