Abstract
Culprit lesion identification in ST elevation myocardial infarction (STEMI) is often guided by electrocardiogram (ECG) changes. However, in the setting of multi-vessel coronary artery occlusion, this can be challenging. We describe an interesting case of dual territory STEMI with unanticipated ECG changes that bring forth the concept of ‘balanced ischaemia’. These seemingly bizarre findings are well explained using the fundamentals of electrocardiography reinstating its relevance in modern day cardiology.
INTRODUCTION
Culprit lesion identification in ST elevation myocardial infarction (STEMI) is guided by electrocardiogram (ECG) changes. However, in the setting of a dual territory STEMI ECG changes can by complex and challenging to decipher. We share an interesting case of ‘balanced ischaemia’ on ECG in the setting of a dual territory STEMI.
CASE REPORT
A 45-year-old man with a prior history of stenting to the left anterior descending (LAD) artery presented with chest pain. His cardiac risk factors included hypertension and dyslipidaemia.
ECG done at the emergency department suggested posterior STEMI (Figs 1 and 2). Emergent coronary angiography revealed occluded left circumflex (LCX) (Fig. 3) and LAD arteries (Fig. 4). The LCX was deemed to be the culprit and stented with resolution of chest pain (Fig. 5). Plans were made to functionally evaluate the LAD at a later date.
Figure 1:
ST depression in anterior leads during angina suggestive of posterior STEMI.
Figure 2:
Posterior ECG confirming posterior STEMI with ST elevation in leads V7–9.
Figure 3:
Mid LCX occlusion.
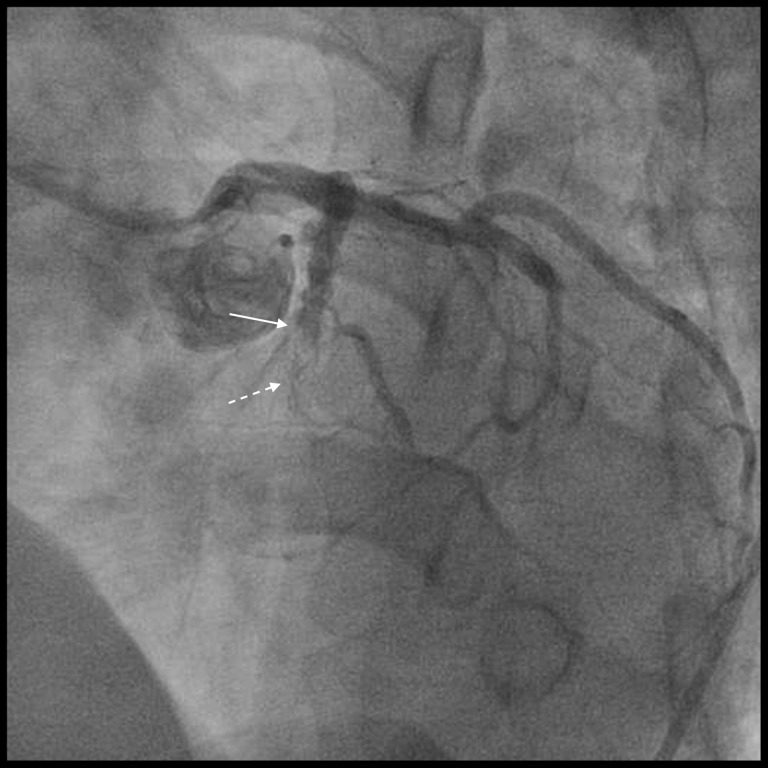
Figure 4:
Mid LAD occlusion (solid arrow) and previous LAD stent (dotted arrow).
Figure 5:
Thrombolysis in myocardial infarction (TIMI) 3 flow post percutaneous coronary intervention (PCI) to mid LCX occlusion.
Post-intervention ECG done after transfer to the coronary care unit unexpectedly showed marked ST elevation in the anterior and inferior leads (Fig. 6) without recurrence of chest pain. An urgent relook angiogram confirmed LCX stent patency and an unchanged LAD occlusion. Intervention to the LAD was performed, with aspiration thrombectomy and evidence of very late stent thrombosis on optical coherence tomography (OCT). Following LAD stenting (Fig. 7) the ST changes on ECG improved (Fig. 8).
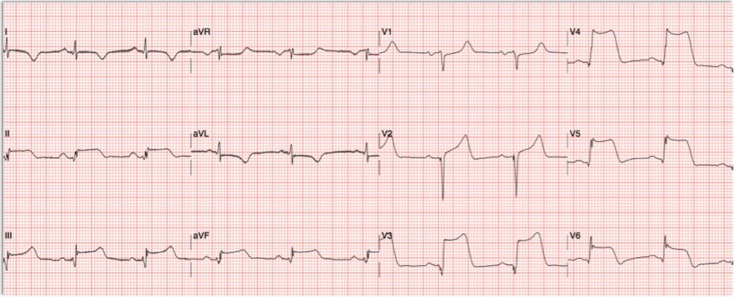
Figure 6:
ECG following PCI to the LCX showing unexpected tombstone ST elevation in leads V3-6 and inferior leads.
Figure 7:
TIMI 3 flow post PCI to mid LAD occlusion.
Figure 8:
ECG following PCI to the LAD showing expected evolutionary changes.
DISCUSSION
This case highlights the concept of ‘balanced ischaemia’ on ECG in the setting of a dual territory STEMI emphasizing the basics of electrocardiography. An ECG is a representation of myocardial electrical potentials. The QRS complexes, ST segments are vectors that have varying magnitudes and directions, similar to that of mathematical vectors. When there are two electrical vectors in opposing directions, there can be a cancellation of the electrical activity and this would result in an ECG pattern that is non-conventional.
In this case, the anterior and posterior vectors do not completely cancel each other out because they are not exactly 180 degrees apart in terms of direction. But rather the resultant vector from the sum of the anterior and posterior vectors resulted in attenuated ST elevation changes.
Despite acute dual coronary artery occlusion, initial ECG changes were subtle. This could be due to opposing anterior and posterior vectors balancing out each other initially. Once the posterior ischaemia was relieved with revascularisation of the left circumflex artery, the anterior vector became unopposed, revealing the tombstone ST elevations. A wrap around LAD can explain the ST elevation in the inferior leads.
This concept of balanced ischaemia where electrically opposite territories that have comparable ischaemic burden negate each other has been described by Madias et al. previously [1–3].
The alternative explanation we have is that, at presentation the patient had a posterior STEMI. And from the time of the first ECG done in the emergency department to the catheterization lab, he developed another STEMI involving the LAD and this was just not captured on ECG because there was no ECG done during that period.
However, what makes this less likely is that the patient’s chest pain resolved with revascularisation of the left circumflex artery and the OCT performed during the second angiogram showed evidence of very late stent thrombosis in the LAD.
New ST elevation after an apparently successful coronary intervention can be seen be in acute stent thrombosis, coronary artery dissection, suboptimal reperfusion and as in our case after unmasking ‘balanced ischaemia’. From a clinical perspective this case reiterates the need to follow up patients after coronary intervention with an ECG to ensure resolution of ST elevation—an often neglected practice that can be potentially life saving.
Patients with multi-vessel (MV) occlusion in STEMI are very ill and often do not survive until cardiac catheterization because they present with cardiogenic shock, ventricular arrhythmias or sudden death. Several factors have been implicated in concomitant MV thrombosis in STEMI—a pro-inflammatory state begetting more thrombosis, coronary embolism, hypercoagulable states (e.g. due to thrombocytosis, hyperhomocysteinemia, malignancy) and prolonged coronary vasospasm [4, 5]. In our case, the identifiable factors were a heightened inflammatory state, smoking history and non-compliance to anti-platelet therapy.
In summary, this case brings forth the concept of ‘balanced ischaemia’ on ECG in the setting of a dual territory STEMI, highlighting an unusual presentation of a common yet fatal medical condition, hinging on the fundamentals of electrocardiography.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.
ETHICAL APPROVAL
Not applicable.
CONSENT
A written ‘Oxford University Press Patient Consent’ was signed by patient after informed consent.
GUARANTOR
I will accept full responsibility for the work, had access to the data, and controlled the decision to publish.
REFERENCES
- 1. Madias JE, Mahjoub M, Valance J. The paradox of negative exercise stress ECG/positive thallium scintigram. Ischemic ST-segment counterpoise as the underlying mechanism. J Electrocardiol 1996;29:243–8. [DOI] [PubMed] [Google Scholar]
- 2. Madias JE, Sheth K. Ischemic ST-segment counterpoise: one mechanism of false electrocardiographic response to exercise stress testing. Am J Noninvas Cardiol 1994;8:194–9. [Google Scholar]
- 3. Madias JE. Six new considerations in electrocardiography: theoretical considerations, and applications in ECG diagnosis. Int J Bioelectromagn 2002;4:135–6. [Google Scholar]
- 4. Pollak PM, Parikh SV, Kizilgul M, Keeley EC. Multiple culprit arteries in patients with ST segment elevation myocardial infarction referred for primary percutaneous coronary intervention. Am J Cardiol 2009;104:619–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee CW, Lai CH, Lu TM. Double coronary artery thrombosis presenting as acute extensive anterior ST-segment elevation myocardial infarction. J Chin Med Assoc 2013;76:407–10. [DOI] [PubMed] [Google Scholar]