Abstract
Study Objectives:
The relationship between sleeping and smoking during adolescence remains unclear and is likely complex. We aim to evaluate the longitudinal reciprocal associations between sleep problems, sleep duration, and smoking among non-Hispanic white (NHW) and non-Hispanic black (NHB) youth.
Design:
Prospective cohort study
Setting:
NEXT Generation Health Study
Participants:
A national sample (N = 1394) of NHB and NHW 10th graders were surveyed annually between 2009 (Wave 1) and 2012 (Wave 3).
Interventions:
N/A
Measurements and Results:
Past 30-day smoking, chronic difficulty falling asleep, recent difficulty falling asleep, difficulty staying asleep, and weekday and weekend sleep duration were measured at each wave. Using structural equation models, we observed significant autocorrelations over time for sleep problems and sleep duration. We found significant reciprocal, prospective relationships between smoking and sleep problems. The strengths of the relationships differed by race, with a stronger association between sleep problems and subsequent smoking for NHB than NHW youth. Conversely, a stronger association between smoking and subsequent sleep problems for NHW than NHB youth was observed. These association were independent of demographics, snoring or sleep apnea, body mass index, depressive symptoms, alcohol use, and soda consumption.
Conclusions:
Reciprocal and prospective relationships exist for youth smoking and sleep problems and duration in both NHW and NHB youth. Further research is needed to unravel the complex relationship between the direct effects of nicotine, lifestyle choices that may link smoking and sleep problems, and racial differences.
Keywords: adolescent, smoking, sleep problem, sleep duration, longitudinal.
Statement of Significance
We found reciprocal, prospective associations between smoking and sleep problems in a US longitudinal sample of youth; associations were different between non-Hispanic Black and non-Hispanic White youth. Future research needs to confirm these associations and explore the mechanisms by which smoking and sleep problems among youth may influence each other (eg, lifestyle choices, environmental influence). Smoking cessation intervention studies should include sleep problems as secondary outcomes, and sleep problems intervention studies should also include smoking as a secondary outcome to better understand how intervening on one behavior could result in changes in the other behavior.
INTRODUCTION
Reducing tobacco use and addressing sleep health among adolescents are both national objectives listed in Healthy People 2020.1 Smoking is the top preventable cause of death in the United States. Since the publication of the 1964 Surgeon General’s Report on smoking and health,2 smoking caused 18 million premature deaths in the United States: 6.5 million deaths by smoking-related cancers, 7.8 million deaths by cardiovascular and metabolic diseases, 3.8 million deaths by pulmonary diseases, and 0.2 million deaths by pregnancy- and birth-related conditions and residential fires.3 The 2014 Surgeon General’s Report concluded that smoking causes at least 13 types of cancers, 5 types of cardiovascular diseases, and many other chronic conditions in adults. Although the health effects of smoking in adolescents are less understood,3 studies have found associations between adolescent smoking and health impact,4 depression,5 alcohol use, illicit drug use, and school problems.6
Sleep health in adolescents is defined as optimal sleep duration (8.5–9.5 hr) and timing (10:30 pm–8:00 am) and the absence of sleep disorders.7,8 Based on health surveillance studies, just under 70% of high school students report insufficient sleep (<7 hours on school nights) and approximately 15% report grossly insufficient sleep (<5 hours on school nights).7–10 Sleep debt among adolescents has been linked to increased risk of health problems including poor cardiometabolic health,10–13 risk-taking behavior,14–17 automobile accidents,18–20 and mood disturbances.16,21 Deficient sleep is also associated with decrements in quality of life and neurocognitive function.22,23 Insomnia (ie, difficulty initiating and/or maintaining sleep and general decrements in sleep quality) and delayed sleep phase syndrome (ie, a circadian rhythm disorder is defined as a delay in the sleep phase that conflicts with usual daily activities) are particularly common among adolescents.24,25 As is the case with smoking, sleeping problems may also be associated with psychopathology, alcohol and substance use, school problems, decrements in quality of life, and daytime impairment.
The association between smoking and deficient sleep is complex and multifactorial. The direct stimulant effects of nicotine may intensify sleep problems26 and counteract some effect of sleep problems on cognitive function.27 Smoking may be associated with use of other substances such as caffeine and amphetamines that act as stimulants, and there is some evidence of increased use among teens who have short sleep duration.28,29 Smoking and deficient sleep may also be common results of propensity for sensation seeking or underlying psychopathology, for example, both smoking and sleep problems have been found to be associated with depression and anxiety.30,31 Few studies have examined the associations between smoking and deficient sleep among adolescents. Cross-sectional studies found that smoking was positively associated with problems going to sleep, problems staying asleep, and daytime sleepiness;32 higher frequencies of having trouble sleeping;33 delaying bedtime and wake-up time;16 and shorter sleep duration.17 However, unlike longitudinal studies, these cross-sectional studies were unable to provide insight on whether smoking predicts deficient sleep or vice versa.
We identified two longitudinal studies that provided information on this topic. In one longitudinal study, adolescents participated in the Teenage Attitudes and Practices Survey 1989 and 1993 (aged 12–18 at baseline; n = 7960). The study found that smoking status at baseline was associated with development of sleep problems at follow-up.34 In a second study among a longitudinal cohort of 386 children aged 3–8 years at baseline, sleep problems at baseline were associated with onset of smoking during adolescence.35 Collectively, previous studies suggest a possible reciprocal relationship between smoking and sleep problems, but no studies to date have examined this reciprocal relationship in detail.
In light of the limitations of the current literature on smoking, sleep problems, and duration, we analyzed data from the NEXT Generation Health Study to examine the prospective effect of smoking on deficient sleep, and the prospective effect of deficient sleep on smoking behaviors simultaneously. We hypothesized that smoking behavior predicts subsequent sleep problems, and sleep problems also predict subsequent smoking behavior. Additionally, surveillance data showed that prevalence of youth smoking differs by race (10.2% among non-Hispanic White and 5.7% among non-Hispanic Black youth).36 Previous studies also documented that sleep problems are more prevalent in non-Hispanic Blacks than non-Hispanic Whites.37 Therefore, we hypothesize that the associations between smoking and sleep problems differ between these two racial groups.
METHODS
We use data from Waves 1–3 of the NEXT Generation Health Study. The NEXT Generation Health Study is a longitudinal study of a nationally representative cohort of 10th-grade U.S. students. Further details about school and student recruitment have been reported previously.38 Students completed questionnaires annually from 10th through 12th grades, with 2785 participants contributing to the imputed data sets, representing 73% of eligible students. Retention of the baseline sample was 88% and 86% at Wave 2 and Wave 3, respectively. The Wave 2 response rate was adjusted because an additional school (n = 261) was added to the study at that time. The Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development approved the study protocol.
Measures
Dependent Variables
Information on smoking and sleep were collected at each wave. Participants were asked to indicate the number of days they smoked cigarettes in the past 30 days (1 = never, 2 = once or twice, 3 = 3–5 times, 4 = 6–9 times, 5 = 10–19 times, 6 = 20–39 times, 7 = 40 times or more). Sleep duration on weekdays and weekends and sleep problems were assessed. Self-report sleep measures evaluated insufficient sleep and variability in weekday and weekend sleep duration (a marker of circadian phase delay) and sleep problems that are symptoms of insomnia and circadian phase delay. Sleep duration was measured as a continuous variable in hours between the self-reported usual bedtime and wake-up time, separately for weekdays or weekends. Sleep problems, symptoms of insomnia circadian phase delay, were assessed by three measures: (a) difficulties in getting to sleep in the last 6 months, (response options 1 = rarely or never, 2 = about every month, 3 = about every week, 4 = more than once a week, 5 = about every day), (b) trouble falling asleep in the last 4 weeks, and (c) recent trouble staying asleep over the past 4 weeks (response options were 1= never, 2 = less than once a week, 3 = 1–2 times/week, 4 = 3 or 4 times/week, or 5 = 5 or more times/week).
Race/Ethnicity
Respondent race/ethnicity was assessed using two questions asking, “What do you consider your race to be? (Black or African American, White, Asian, American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander)” and “What do you consider your ethnicity to be? (Hispanic or Latino, not Hispanic or Latino)” Participants who reported “Black or African American” for race and “not Hispanic or Latino” for ethnicity were classified as non-Hispanic Black. Participants who reported “White” for race and “not Hispanic or Latino” for ethnicity were classified as non-Hispanic White. We limited our analyses to these two racial/ethnic groups due to low number of respondents in other racial/ethnic groups.
Covariates
Demographic covariates included gender (female = 1; male = 0) and parent reported education (highest of mother and father, ascertained during the consent process, dichotomized as high school or less = 1; else = 0). Other covariates included Wave 1 measures of self-reported history of snoring or sleep apnea (yes = 1; no = 0), measured body mass index (kg/m2), depressive symptoms score, alcohol use in the past 30 days (yes = 1; no = 0), and soda drinking (4+ per week = 1; else = 0) at Wave 1. The depressive symptoms score is the sum of six items from the Bosworth Modified Depression Scale39 included in Wave 1 of the survey which asks about feeling sad, irritable, hopeless, eating more or less than usual, sleeping more or less than usual, and difficulty concentrating in the last 30 days (response options 1–5, never to always). The scale was previously evaluated to have good internal consistency (α = 0.79) and to be associated with health risk behavior in a racial/ethnically diverse 9th–12th graders.40 Although these measures were also assessed in Waves 2 and 3, including time-varying covariates did not significantly change the associations of interest. For model parsimony, we only included Wave 1 covariate measures.
Statistical Approach
Descriptive statistics between non-Hispanic White and non-Hispanic Black youth were compared using chi-square tests or t-tests. We used two-group structural equation modeling to evaluate the longitudinal effects of sleep problems and duration and smoking for non-Hispanic White and non-Hispanic Black youth. Specifically, we employed autoregressive cross-lagged models. The autoregressive component allowed us to model the effects of past smoking predicting future smoking and past sleep problems predicting future sleep problems. Cross-sectional correlations between smoking and sleep variables were included in the model to capture their contemporaneous relationships. The cross-lagged component allowed us to model the prospective relationships between past smoking predicting future sleep problem measures and past sleep problem measures predicting future smoking simultaneously in the model. We constrained our model such that the effects in the cross-lagged component would be the same over time within each race/ethnic group but could vary between race/ethnic groups. We report fully standardized results so they are directly comparable by race/ethnicity controlling for known covariates. These models account for clustering by sampling design. Analyses were performed using Mplus version 7.3.
RESULTS
Table 1 reports the descriptive statistics for our sample (n = 1394; non-Hispanic Black = 399; non-Hispanic White = 995). Compared to non-Hispanic White participants, non-Hispanic Black participants were more likely to be female and to have consumed soda in the past 30 days at Wave 1; to report a later weekend mid-sleep time; and to have a higher body mass index at Wave 1 (p < .05). In contrast, compared to non-Hispanic White participants, non-Hispanic Black participants were less likely to have educated parents, to have consumed alcohol in the past 30 days at Wave 1, to report fewer occasions of cigarette smoking, fewer occasions of having troubles falling asleep, and shorter sleep duration on weekdays (p < .05).
Table 1.
Sample Characteristics Among Non-Hispanic Black (NHB, n = 399) and Non-Hispanic White (NHW, n = 995) Participants in the NEXT Generation Health Study, Waves 1–3.
| Characteristic | NHB, Mean (SD) | NHW, Mean (SD) | p |
|---|---|---|---|
| Number of occasions smoked in the past 30 days (1–7) | |||
| Wave 1 | 1.15 (0.77) | 1.67 (1.65) | <.01 |
| Wave 2 | 1.09 (0.50) | 1.68 (1.68) | <.01 |
| Wave 3 | 1.12 (0.65) | 1.91 (1.91) | <.01 |
| Troubles falling asleep in the past 4 weeks (1–5) | |||
| Wave 1 | 2.16 (1.19) | 2.50 (1.21) | <.01 |
| Wave 2 | 2.15 (1.16) | 2.47 (1.22) | <.01 |
| Wave 3 | 2.10 (1.14) | 2.33 (1.17) | <.01 |
| Trouble staying asleep in the past 4 weeks (1–5) | |||
| Wave 1 | 2.21 (1.24) | 2.32 (1.25) | .14 |
| Wave 2 | 2.24 (1.27) | 2.21 (1.21) | .71 |
| Wave 3 | 2.18 (1.20) | 2.21 (1.18) | .64 |
| Difficulty getting to sleep in the past 6 months (1–5) | |||
| Wave 1 | 1.91 (1.33) | 2.21 (1.39) | <.01 |
| Wave 2 | 1.82 (1.20) | 2.14 (1.36) | <.01 |
| Wave 3 | 1.82 (1.15) | 2.03 (1.28) | <.01 |
| Weekday sleep duration (hours) | |||
| Wave 1 | 7.31 (1.21) | 7.61 (0.94) | <.01 |
| Wave 2 | 7.35 (1.22) | 7.63 (1.00) | <.01 |
| Wave 3 | 7.15 (1.04) | 7.58 (1.02) | <.01 |
| Weekend sleep duration (hours) | |||
| Wave 1 | 9.23 (1.79) | 9.37 (1.46) | .17 |
| Wave 2 | 9.30 (1.84) | 9.32 (1.52) | .89 |
| Wave 3 | 8.96 (1.74) | 9.06 (1.41) | .33 |
| Weekday mid-sleep time | |||
| Wave 1 | 2:28 am | 2:27 am | .64 |
| Wave 2 | 2:30 am | 2:35 am | .13 |
| Wave 3 | 2:39 am | 2:44 am | .14 |
| Weekend mid-sleep time | |||
| Wave 1 | 5:25 am | 5:02 am | <.01 |
| Wave 2 | 5:19 am | 5:05 am | .01 |
| Wave 3 | 5:19 am | 5:06 am | .01 |
| Gender (female) | 61.9% | 54.2% | <.01 |
| Parent education (>high school) | 62.4% | 77.2% | <.01 |
| Snoring or sleep apnea at W1 | 31.1% | 29.1% | .45 |
| Consumed alcohol in the past 30 days at Wave 1 | 25.3% | 34.4% | <.01 |
| Consumed soda in the past 30 days at Wave 1 | 83.5% | 78.6% | <.01 |
| Body Mass Index at Wave 1 | 25.09 (6.15) | 24.29 (5.45) | .02 |
| Depressive symptom score at Wave 1 | 2.29 (0.86) | 2.28 (0.82) | .82 |
Percentages were presented for categorical variables. T-tests and chi-square tests were used to test the differences between NHB and NHW.
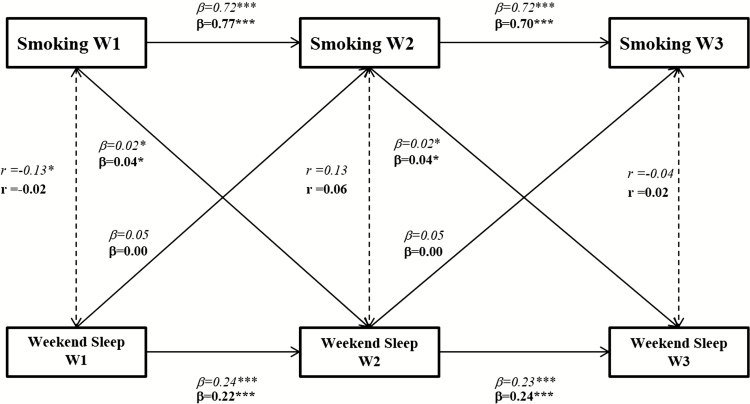
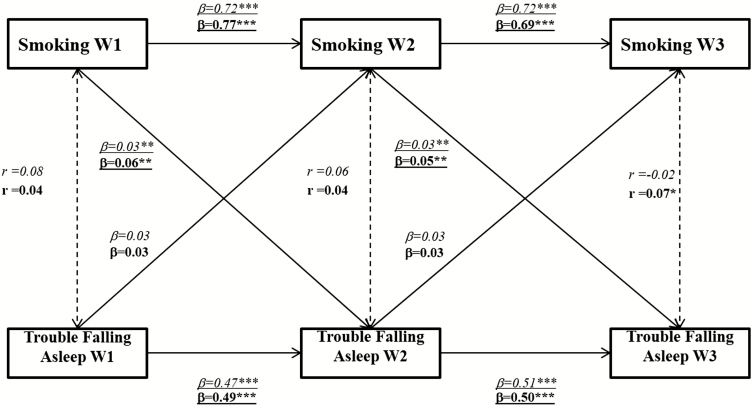
Across all models, we observed strong autoregressive relationships for past 30-day smoking occasions and each of the sleep measures for non-Hispanic White participants but only strong autoregressive relationships for each of the sleep measures for non-Hispanic Black. The autoregressive correlations were stronger among non-Hispanic White than non-Hispanic Black participants for troubling staying asleep in the past 30 days over time (Figure 3; p < .05) and weekday sleep during over time (p < .05; NHW W1→W2 (β) = 0.54, W2→W3 (β) = 0.53; NHB W1→W2 (β) = 0.46, W2→W3 (β) = 0.45). Figure 1 reports the results for our model for chronic difficulty falling asleep (ie, difficulties getting to sleep over the past 6 months). We found number of smoking occasions predicted subsequent chronic difficulty falling asleep for both non-Hispanic Black and non-Hispanic White participants (p < .05), and the effect did not vary significantly between these two groups (p > .05).
Figure 3.
Race-stratified, autoregressive, cross-lagged model for number of smoking occasions and recent difficulty staying asleep (trouble falling asleep in the past 4 weeks) in Waves 1–3. Note: P30D = past 30 days, P4Wk = past 4 weeks, W = wave. *p < .05; # Estimates differ between non-Hispanic Black (NHB) and non-Hispanic White (NHW; p < .05). Controlled for gender, parent education, snoring or sleep apnea, body mass index, depressive symptoms, and alcohol and soda consumption at Wave 1.
Figure 1.
Race-stratified, autoregressive, cross-lagged model for number of smoking occasions and chronic difficulty falling asleep (difficulty getting to sleep in the past 6 months) in Waves 1–3. Note: P30D = past 30 days, P6M = past 6 months, W = wave. *p < .05, # Estimates differ between non-Hispanic Black (NHB) and non-Hispanic White (NHW; p < .05). Controlled for gender, parent education, snoring or sleep apnea, body mass index, depressive symptoms, and alcohol and soda consumption at Wave 1.
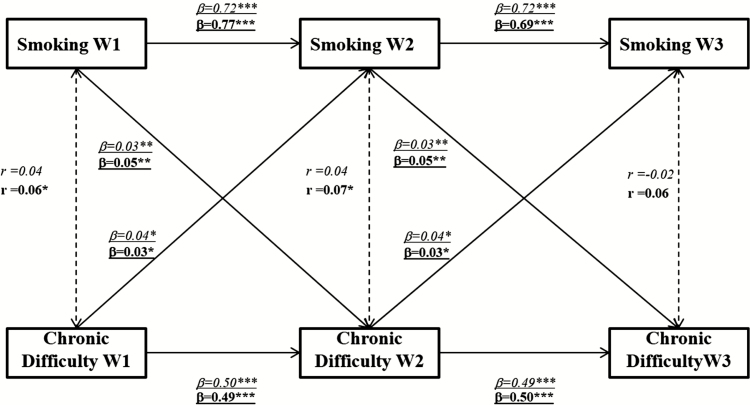
Figure 2 reports the results for our model for recent difficulty falling asleep (ie, trouble falling asleep in the past 4 weeks). We observed a significant prospective effect of number of smoking occasions on subsequent recent difficulty falling asleep as well as a significant prospective effect of recent difficulty falling asleep on subsequent number of smoking occasions (p < .05). These associations also differ by race/ethnicity. Effect of number of smoking occasions on subsequent recent difficulty falling asleep was stronger in non-Hispanic White than non-Hispanic Black participants (0.07–0.08 vs. 0.02–0.04), while effect of recent difficulty falling asleep on subsequent number of smoking occasions was stronger in non-Hispanic Black than non-Hispanic White participants (0.06–0.08 vs. 0.02).
Figure 2.
Race-stratified, autoregressive, cross-lagged model for number of smoking occasions and recent difficulty falling asleep (trouble falling asleep in the past 4 weeks) in Waves 1–3. Note: P30D = past 30 days, P4Wk = past 4 weeks, W = wave.
*p < .05; # Estimates differ between non-Hispanic Black (NHB) and non-Hispanic White (NHW; p < .05). Controlled for gender, parent education, snoring or sleep apnea, body mass index, depressive symptoms, and alcohol and soda consumption at Wave 1.
Figure 3 reports the results for our model for recent difficulty staying asleep (ie, trouble staying asleep in the past 4 weeks). We only observed significant effect of number of smoking occasion on subsequent recent difficulty staying asleep among non-Hispanic White participants (p < .05). No significant cross-lag associations were observed between number of smoking occasions and sleep duration during weekdays and weekends (p > .05).
DISCUSSION
Using longitudinal study data of adolescents, after accounting for the depressive symptoms and alcohol and soda consumption, smoking frequency was significantly associated with future sleep problems. Specifically, we found that number of smoking occasions in the past 30 days was associated with subsequent recent and chronic difficulty falling asleep for both non-Hispanic Black and non-Hispanic White youth, and recent difficulty staying asleep for non-Hispanic White youth. This finding suggests that smoking may influence sleep quality independent of psychopathology (eg, depression) and other substance use such as caffeine or alcohol. It further implies that by achieving the Healthy People 2020 goal of reducing tobacco use among adolescents, sleep health could be improved.
Our finding that recent and chronic difficulty in falling asleep was associated with future smoking is novel to the existing literature. Only one previous longitudinal study reported that sleep problems at ages 3–8 were associated with onset of smoking during adolescence while we found that sleep onset problems predicted subsequent smoking during adolescence. There are several possible explanations for this finding. Sleep onset problems can be caused by stress and subclinical and persistent mental health problems. Perhaps, adolescents who persistently experience problems falling asleep smoke to self-medicate with the mild stimulant effects of nicotine to improve their mood, without knowing smoking could jeopardize their sleep. It is also plausible that unhealthy lifestyle choices could contribute to both sleep onset problems (eg, habitual use of media, poor sleep hygiene, and caffeine use) and smoking. In both cases, educating adolescents with sleep problems about the association between smoking and sleep deficiency could result in decreasing risk of engaging in this unhealthy behavior.
It is noteworthy that a reciprocal relationship exists between smoking and recent difficulty falling asleep, that is, current smoking was associated with subsequent sleep problems, and sleep problems were associated with subsequent smoking, creating feedback loops. This finding provides new insight into the dynamic mechanisms that explain adolescent smoking and sleep problems. This finding has at least two implications. First, future research should capture the complex reciprocal relationship between smoking and sleep problems to better understand how changes in one outcome leads to changes in the other outcome. Second, while intervening on one outcome (either smoking or sleep deficiency) could improve the other outcome, simultaneously intervening on both outcomes may produce synergistic impact beyond what could be achieved by intervening on a single outcome alone. While not measured here, smoking and sleep problems may also have underlying shared causes such as increased propensity for risk-taking behavior, chronic mild mental health problems, and unhealthy lifestyle choices (eg, other drug use). This is supported by our data showing that depressive symptoms were positively associated with smoking, recent and chronic difficulty falling asleep, and recent difficulty staying asleep in both non-Hispanic Black and non-Hispanic White youth, and were negatively associated with weekday sleep duration in non-Hispanic White youth (p < .05). It is possible that depressive symptoms (and other mental health problems) may increase the vulnerability of youth to peer influence on smoking,30 particularly when they are sleep deprived. Early education and intervention to address these problems could reduce risk of smoking and improve sleep health. Future intervention research is needed to test this hypothesis.
We observed that the associations between current smoking and subsequent sleep problems differed between non-Hispanic Black adolescents and non-Hispanic White adolescents in some areas. The effect of smoking on sleep problem was stronger for non-Hispanic White youth than for non-Hispanic Black youth. Perhaps, non-Hispanic Black youth encounter more psychosocial stressors (eg, discrimination, violence, socioeconomically related stress) than non-Hispanic White youth that could negatively influence sleep problems, thereby diluting the association between smoking and subsequent sleep problems.41,42 On the other hand, the association between sleep problems and subsequent cigarette smoking was weaker in non-Hispanic White youth than non-Hispanic Black youth. This could be due to higher concentration of tobacco outlets in neighborhoods with higher concentration of non-Hispanic Black individuals, which provides higher exposure to point-of-sale cigarette advertising and access to cigarettes. Consequently, this environment differentially may facilitate non-Hispanic Black youth to self-medicate their sleeping problems with cigarettes.43 Ethnic, racial, and cultural differences in sleep habits and chronotype have been observed, but the underlying causes have not been studied. Future research is needed to test these hypotheses.
Limitations
Although using two-group structural equation modeling provides insight into non-Hispanic Black–White differences in patterns related to adolescent smoking and sleep problems and duration, our analyses were unable examine additional race/ethnic differences due to small sample sizes of other groups. As such, we are limited in our ability to generalize our results only to non-Hispanic Black–White differences and cannot speak to patterns that may or may not exist in other race/ethnic groups. Another area of concern lies with the snoring or sleep apnea question used as a control measure. Snoring and sleep apnea are different health issues with differing severity, etiology, and prevalence. Unfortunately, because the wording of this question conflated the two constructs, we were unable to run additional analyses to test whether past smoking predicted future sleep apnea or snoring. We elected to keep this measure as a covariate in case the measure reflected the more concerning problem, sleep apnea, in order to approach this issue conservatively. Furthermore, non-Hispanic Black adolescents in our study may have underreported difficulty falling asleep. A previous study showed that White American adults were more than Black American adults to report difficulty falling asleep, but less likely to report sleep latency >30 minutes,44 suggesting potential race-specific underreporting. Lack of a smoking timing measure is also a limitation, since the effect of smoking on sleep could be highly time dependent. Therefore, our current analysis may have underestimated the effect of smoking on sleep.
In light of the limitations of the current literature on smoking and sleep problems and duration, we analyzed data from the NEXT Generation Health Study to examine the prospective effect of smoking on sleep problems simultaneously and the prospective effect of sleep problems on smoking behaviors. We also assessed whether these effects differ across non-Hispanic White and non-Hispanic Black youth. We found complex, reciprocal associations between smoking and sleep onset problems among adolescents that appear to operate differently for these two racial/ethnic groups. Future studies should build upon this research exploring in detail the hypothesized complex relationship between smoking and sleep quality in youth and the race/ethnic differences. Intervention studies targeting both sleep health and smoking could improve both and eliminate shared causes.
DISCLOSURE STATEMENT
None declared.
Supplementary Material
ACKNOWLEDGMENT
Bellatorre and Choi’s effort is funded by the Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health. The NEXT Generation Health Study is supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Contract # HHSN275201200001I), and the National Heart, Lung and Blood Institute (NHLBI), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA), and the National Institute on Drug Abuse (NIDA).
REFERENCES
- 1. U.S. Department of Health and Human Services. 2020 Topics and Objectives—Objectives A–Z; 2014https://www.healthypeople.gov/2020/topics-objectives. Accessed October 1, 2015.
- 2. Surgeon General’s Advisory Committee on Smoking and Health. The Reports of the Surgeon General: Smoking and Health. Washington, DC: Office of the Surgeon General; 1964. [Google Scholar]
- 3. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 4. U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 5. Steuber TL, Danner F. Adolescent smoking and depression: which comes first? Addict Behav. 2006; 31(1): 133–136. [DOI] [PubMed] [Google Scholar]
- 6. Hanna EZ, Yi HY, Dufour MC, Whitmore CC. The relationship of early-onset regular smoking to alcohol use, depression, illicit drug use, and other risky behaviors during early adolescence: results from the youth supplement to the third national health and nutrition examination survey. J Subst Abuse. 2001; 13(3): 265–282. [DOI] [PubMed] [Google Scholar]
- 7. Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1980; 2(4): 453–460. [DOI] [PubMed] [Google Scholar]
- 8. Crowley SJ, Van Reen E, LeBourgeois MK, et al. A longitudinal assessment of sleep timing, circadian phase, and phase angle of entrainment across human adolescence. PLoS One. 2014; 9(11): e112199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, Croft JB. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students—United States, 2007. J Adolesc Health. 2010; 46(4): 399–401. [DOI] [PubMed] [Google Scholar]
- 10. Wheaton AG, Perry GS, Chapman DP, Croft JB. Self-reported sleep duration and weight-control strategies among U.S. high school students. Sleep. 2013; 36(8): 1139–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dominguez-Rodriguez A, Abreu-Gonzalez P. The link between sleep duration and inflammation: effects on cardiovascular disease. Int J Cardiol. 2014; 173(3): 600–601. [DOI] [PubMed] [Google Scholar]
- 12. Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One. 2013; 8(11): e82305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grandner MA, Sands-Lincoln MR, Pak VM, Garland SN. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013; 5: 93–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hildenbrand AK, Daly BP, Nicholls E, Brooks-Holliday S, Kloss JD. Increased risk for school violence-related behaviors among adolescents with insufficient sleep. J Sch Health. 2013; 83(6): 408–414. [DOI] [PubMed] [Google Scholar]
- 15. O’Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behav Sleep Med. 2005; 3(3): 113–133. [DOI] [PubMed] [Google Scholar]
- 16. Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav. 2010; 34(2): 237–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stea TH, Knutsen T, Torstveit MK. Association between short time in bed, health-risk behaviors and poor academic achievement among Norwegian adolescents. Sleep Med. 2014; 15(6): 666–671. [DOI] [PubMed] [Google Scholar]
- 18. Danner F, Phillips B. Adolescent sleep, school start times, and teen motor vehicle crashes. J Clin Sleep Med. 2008; 4(2): 533–535. [PMC free article] [PubMed] [Google Scholar]
- 19. Hutchens L, Senserrick TM, Jamieson PE, Romer D, Winston FK. Teen driver crash risk and associations with smoking and drowsy driving. Accid Anal Prev. 2008; 40(3): 869–876. [DOI] [PubMed] [Google Scholar]
- 20. Vorona RD, Szklo-Coxe M, Lamichhane R, Ware JC, McNallen A, Leszczyszyn D. Adolescent crash rates and school start times in two central virginia counties, 2009–2011: a follow-up study to a southeastern virginia study, 2007–2008. J Clin Sleep Med. 2014; 10(11): 1169–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and suicidality: results from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med. 2011; 7(4): 351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011; 58(3): 649–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gruber R, Michaelsen S, Bergmame L, et al Short sleep duration is associated with teacher-reported inattention and cognitive problems in healthy school-aged children. Nat Sci Sleep. 2012; 4(5): 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hysing M, Pallesen S, Stormark KM, Lundervold AJ, Sivertsen B. Sleep patterns and insomnia among adolescents: a population-based study. J Sleep Res. 2013; 22(5): 549–556. [DOI] [PubMed] [Google Scholar]
- 25. Sivertsen B, Pallesen S, Stormark KM, Bøe T, Lundervold AJ, Hysing M. Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study. BMC Public Health. 2013; 13(1): 1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Davila DG, Hurt RD, Offord KP, Harris CD, Shepard JW., Jr Acute effects of transdermal nicotine on sleep architecture, snoring, and sleep-disordered breathing in nonsmokers. Am J Respir Crit Care Med. 1994; 150(2): 469–474. [DOI] [PubMed] [Google Scholar]
- 27. Levin ED, McClernon FJ, Rezvani AH. Nicotinic effects on cognitive function: behavioral characterization, pharmacological specification, and anatomic localization. Psychopharmacology (Berl). 2006; 184(3-4): 523–539. [DOI] [PubMed] [Google Scholar]
- 28. Bryant Ludden A, Wolfson AR. Understanding adolescent caffeine use: connecting use patterns with expectancies, reasons, and sleep. Health Educ Behav. 2010; 37(3): 330–342. [DOI] [PubMed] [Google Scholar]
- 29. Pollak CP, Bright D. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics. 2003; 111(1): 42–46. [DOI] [PubMed] [Google Scholar]
- 30. Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998; 88(10): 1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry Hum Dev. 2010; 41(2): 156–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995; 155(7): 734–737. [PubMed] [Google Scholar]
- 33. Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug Alcohol Depend. 2001; 64(1): 1–7. [DOI] [PubMed] [Google Scholar]
- 34. Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000; 106(2): E23. [DOI] [PubMed] [Google Scholar]
- 35. Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009; 10(7): 787–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Singh T, Arrazola RA, Corey CG, Husten CG, Neff LJ, Homa DM, King BA. Tobacco use among middle and high school students–United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2016; 65(14): 361–367. [DOI] [PubMed] [Google Scholar]
- 37. Grandner MA, Knutson KL, Troxel W, Hale L, Jean-Louis G, Miller KE. Implications of sleep and energy drink use for health disparities. Nutr Rev. 2014; 72(Suppl 1): 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Conway KP, Vullo GC, Nichter B, et al Prevalence and patterns of polysubstance use in a nationally representative sample of 10th graders in the United States. J Adolesc Health. 2013; 52(6): 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bosworth K, Espelage D, DuBay T, Dahlberg LL, Daytner G. Using multimedia to teach conflict-resolution skills to young adolescents. Am J Prev Med. 1996; 12(5 Suppl): 65–74. [PubMed] [Google Scholar]
- 40. Dunn EC, Johnson RM, Green JG. The Modified Depression Scale (MDS): a brief, no-cost assessment tool to estimate the level of depressive symptoms in students and schools. School Ment Health. 2012; 4(1): 34–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013; 5(2): 100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009; 32(1): 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nichter M. Smoking: what does culture have to do with it? Addiction. 2003; 98(Suppl 1): 139–145. [DOI] [PubMed] [Google Scholar]
- 44. Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013; 9(9): 897–905; 905A–905D. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.