Abstract
Introduction
This rapid review identifies and summarizes the effectiveness of preventative telemental health interventions. It investigates studies conducted between 2010 and 2016 that improve mood and anxiety with long-term follow-up.
Methods
A literature search of three major databases was performed by four reviewers. After citation tracing, 3604 studies were discovered, and twenty of these met the inclusion criteria. Data from the papers were abstracted, assessed for quality, and effect sizes were calculated.
Results
Salient information was discussed using the Behavioural Vaccine Model of mental illness prevention. This included key concepts such as efficacy, duration of benefits, sociocultural relevance, professional guidance, peer-to-peer support, adherence, delivery and safety.
Conclusion
This review suggests there are clear prolonged benefits to using technology in youth mental illness prevention. Although this is a rapidly growing area of investigation in countries around the globe, there is still a dearth of research with long-term follow-up. Future studies should aim to boost engagement by increasing motivational guidance in order to recruit at-risk youth of all demographics into these promising intervention programs.
Keywords: Youth, Mood, Technology, Mental health, Depression, Anxiety, Rapid review
Highlights
-
•
There are few technology-based interventions for adolescent mood and anxiety disorders with at least 6 months of follow-up.
-
•
A rapid review methodology was used, and 20 articles were discovered.
-
•
Many studies focus on effect sizes, but disregard engagement and motivation —key factors in real-world implementation.
-
•
Many interventions demonstrate efficacy at improving youth mental health. Public scale implementation studies are warranted.
1. Introduction
Psychiatric disorders are a major health concern worldwide, leading to billions of dollars in economic burden (Waddell et al., 2007). A significant proportion of these disorders begin in the pediatric population (Kessler et al., 2005). Estimated prevalence rates for youth mental health disorders range from 8% in the Netherlands to 23% in Switzerland (Patel et al., 2007, Waddell et al., 2005). In the United Sates, the lifetime prevalence of severe mental disorders in 13 to 18 year olds has been estimated to be 21.4% (Merikangas et al., 2010). Mental health disorders among youth can lead to disability, impaired relationships, academic struggles, substance abuse, chronic illness and suicide (Fombonne et al., 2001). Since as much as 75% of adult mental disorders begin between the ages of 12 and 24, prevention at an early age would allow for a long-term decrease of noncommunicable disease in the adult population (Kessler et al., 2005, Kim-Cohen et al., 2003, Rao and Chen, 2009).
There is a general lack of availability and access to mental health professionals and resources, especially in rural areas and underdeveloped countries (Latha et al., 2007, Verhulst et al., 2003). A large treatment gap exists for mental health issues, as there are many barriers in place. These barriers include the cost of care, stigma of mental illness and shortages of professionals (Patel et al., 2007). One study found that 75% of Australian youth did not receive the psychiatric care that they needed (Sawyer et al., 2001). Technology-based interventions could offer a solution to bridge this treatment gap and provide youth with the assistance that they require.
Increasing numbers of Internet and telephone mental health interventions have been developed over the past decade. Youth often respond favorably to these untraditional mental health interventions (Wilkinson et al., 2008), which, when used properly, allow for the private, cost-effective and accessible care of mental illness. Self-help through evidence- and technology-based programs has been found to be especially useful in building resiliency in underserved populations (Kirsch and Lewis, 2004).
The use of technology for the treatment and prevention of mental health disorders is a relatively new field, with a growing field of literature for adults. However, only a few reviews of technology-based mental health interventions for youth exist currently (Calear and Christensen, 2010, Richardson et al., 2010). Calear and colleagues identified 4 programs, all focused on Cognitive Behavioral Therapy (CBT), with preliminary results that showed mild to moderate effect size (Calear and Christensen, 2010). Richardson et al. identified 10 studies and noted that youth reported high satisfaction with computerized CBT, but also high dropout rates (Richardson et al., 2010). Both reviews noted that the study of prevention was particularly difficult in children, and that limited follow-up data were available. CATCH-IT, Competent Adulthood Transition with Cognitive Behavioral Humanistic and Interpersonal Training, was developed by Van Voorhees et al. (2005), with subsequent phase 2 (2009) and Richards et al. phase 3 (2016) clinical trials, to prevent the onset of depressive disorders in adolescents after detection in primary care settings (Van Voorhees et al., 2005, Van Voorhees et al., 2009, Richards et al., 2016).
This paper functions as an update to two reviews that were performed in 2011 (Siemer et al., 2011, Van Voorhees et al., 2011). The pediatric telemental health intervention review by Siemer et al. (2011) identified twenty studies covering a range of mental health disorders, study designs, treatment settings and countries. Quantitative methods were used to investigate these studies, which showed effect sizes ranging from small to moderate. Topics such as safety, peer-to-peer interaction, parent involvement, socioeconomic status and ecological settings were also analysed in the twenty papers.
The second review was based on the novel Behavioural Vaccine Model (BVM) of depression prevention (Van Voorhees et al., 2011). This paper identified 19 Internet-based studies with at least a 6-month follow-up, but was not limited to the pediatric population. Effect sizes showed that online CBT was as effective as face-to-face interventions. The BVM allowed for analysis based on four major categories: Life Course Schedule, Effective Components, Framework for Motivation, and Implementation Structure. In the current review, the Life Course Schedule category will be omitted, as only interventions featuring adolescents and emerging adults are included.
The focus of this review is to describe the structure of potentially effective and “implementable” interventions. This review is unique in that it identifies, summarizes and investigates the effectiveness of technology-based studies, preventative studies and studies with long-term follow-up. Using rapid review methodology allows for a scan of new work and ideas between 2010 and 2016. We focused on interventions that prevented mood and anxiety disorders, including social anxiety, post-traumatic stress disorder (PTSD) and obsessive compulsive disorder (OCD).
2. Methods
A rapid evidence assessment review of Internet and computer-assisted programs to prevent mood and anxiety disorders in pre-teen and adolescent populations was performed (Grant and Booth, 2009). The review addressed the question: What technology-based, educational, preventive measures were associated with the positive prevention of mood and anxiety symptoms in specified youth?
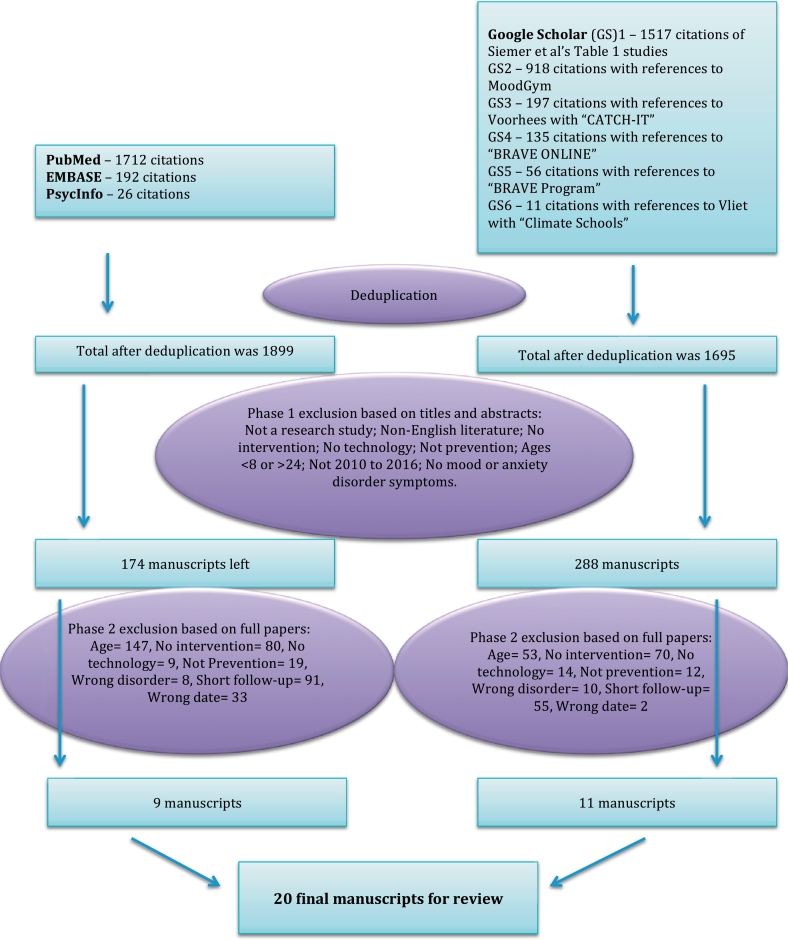
Since several systematic and systematized reviews had summarized evidence prior to 2011, this rapid review methodology and a time-limited approach were deemed efficient for comprehensive evidence discovery. We searched 3 electronic databases (PubMed and EMBASE from 2000 to 11/30/16, PsycInfo from 2000 to 4/1/17), querying the intersection of 1) mood and anxiety conditions or disorders concepts with 2) content delivery via online technologies concepts (Fig. 1). Medline indexed citations were excluded from EMBASE and PsycInfo results. We performed citation tracing of studies from Table 1 of Siemer et al.'s (2011) benchmark review using Google Scholar (GS). Additionally, we implemented 5 targeted GS searches for references related to leading programs in the field (MoodGym, CATCH-IT, Climate Schools). No grey literature searches were conducted, and only English language publications from 2010 to 2016 were included from GS. Reasons for exclusion can be seen in Fig. 1.
Fig. 1.
Rapid review search methodology.
The studies were summarized and analysed using the BVM (Van Voorhees et al., 2011). An effect size calculator (http://www.cem.org/effect-size-calculator) was used when effect sizes were not provided in a study.
The methodological quality of the randomized clinical trials were also assessed using a modified quality index tool developed by Downs and Black (1998). This well validated tool scores the quality of reporting, external validity, and internal validity. Because most studies did not report their power, the power score was omitted in the rating scale. The resultant maximum score was 27. Two assessors independently rated the randomized studies; average scores are shown in Table 1.
Table 1.
Content of youth Internet interventions selected for review.
| Citation | Quality index | Age | N; gender | Study type | Control | Setting/goal | Content | Outcomes between-groups effect size (95% CI) | Outcomes pre/post effect size (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Depression studies | |||||||||
| Hoek et al. (2011); CATCH-IT 6 month | 25 | 17.4 | 83; 56.6% female | RCT | Motivational interviewing vs. Brief advice | Primary care, prevention | CBT, BA, IPT, community resiliency, videos, stories | CESD-10: ES = 0.12 (− 0.31–0.55); PHQ-A: ES = − 0.2 (− 0.63–0.23) | BA: CESD-10: ES = 1.13 (0.72–1.52); PHQ-A: ES = 0.57 (0.19–0.95); MI: CESD-10: ES = 0.93 (0.54–1.31); PHQ-A: ES = 0.77 (0.38–1.15) |
| Saulsberry et al. (2013a); CATCH-IT 1 year | 25 | 17.2 | 58, 57% female | RCT | Motivational interviewing vs. Brief advice | Primary care, prevention | CBT, BA, IPT, community resiliency, videos, stories | CESD-10: ES = 0.08 (− 0.35–0.51); PHQ-A: ES = − 0.05 (− 0.48–0.38) | CESD-10: ES = 0.96 (0.63–1.17); PHQ-A: ES = 0.81 (0.49–1.12) |
| Richards et al. (2016); CATCH-IT 2.5 year | 24.5 | 19.6 | 44; 59.09% female | RCT | Motivational interviewing vs. Brief advice | Primary care, prevention | CBT, BA, IPT, community resiliency, videos, stories | CESD-10: ES = 0.37 (− 0.24–0.96); PHQ-A: ES = 0.28 (− 0.35–0.90) | CESD-10: ES = 0.84 (0.4–1.27); PHQ-A: ES = 0.79 (0.35–1.22) |
| Ip et al. (2016); Grasp the Opportunity | 21 | 14.6 | 257; 68.1% female | RCT | Website vs. Attention control | School, prevention | CBT, BA, community resiliency, videos, stories; IPT excluded | 12 months: CESD-R: ES = − 0.36 (− 0.61 to − 0.11) | 8 months: CESD-R: ES = 0.09 (− 0.12–0.30) |
| Poppelaars et al. (2016); SPARX game vs. Op Volle Kracht lessons | 22.5 | 13.3 | 208; 100% female | RCT | OVK vs. SPARX vs. combined vs. monitoring control | Game, prevention | CBT, education | 12 months vs. control RADS-2: ES = 0.28 (− 0.11–0.67); vs. OVK RADS-2: ES = 0.40 (0.00–0.79) | 12 months: RADS-2: ES = 1.05 (0.63–1.46) |
| van der Zanden et al. (2012); Online Master Your Mood (MYM) | 24 | 20.9 | 244; 84.4% female | RCT | MYM vs. waitlist control | Chat room, prevention | CBT, BA, future planning | ITT 3 months: CESD-D: ES = 0.94 (0.64–1.23); anxiety HADS: ES = 0.49 (0.24–0.75) | 6 months: CESD-D: ES = 1.48 (1.19–1.76); anxiety HADS: ES = 0.92 (0.65–1.18) |
| Kramer et al. (2014); PratenOnline | 23 | 19.5 | 263; 78.7% female | RCT | Website vs. Wait list control | Home, prevention | Solution-Focused Brief Therapy (SFBT) chat with online therapist | 4.5 month Chat vs. WL CESD: ES = 0.79 (0.45–1.08) | 7.5 months vs. baseline CESD: ES = 2.05 (1.75–2.34) |
| Deady et al. (2016); DEAL Project | 24.5 | 21.7 | 104; 59.6% female | RCT | DEAL Project vs. Health Watch control | Home, early intervention | CBT, MI, education, behavioral activation, relaxation & coping, mindfulness | 6 month PHQ-9: ES = 0.39 | 6 month PHQ-9: ES = 1.42 |
| Stallman et al. (2016) | 24.5 | 23 | 107; 92% female | RCT | LI-CBT vs. self-help info only | Telephone, prevention | LI-CBT: Behavioral activation, exposure therapy, problem solving, sleep hygiene, relapse prevention. | 2 month DASS-Depression: ES = − 0.55; DASS-Anxiety: ES = − 0.496 | 2 month DASS-Depression: ES = − 0.755; DASS-Anxiety: ES = − 0.498 |
| Taylor et al. (2016); Image and Mood (IaM) | 23.5 | 20 | 206, 100% female | RCT | iCBT vs. wait-list control | Home, prevention | CBT, IPT, BA, stress management (relaxation training), problem solving, college transition, Discussion board. | Post-test: EDE-Q Global: ES = 0.31; EDI-Drive for Thinness: ES = 0.24; In subgroup of 27 depressed individuals at baseline, BDI-II: ES = 0.96 | Post-test: EDE-Q Global: ES = 1.23 (0.93–1.52); BDI-II: ES = 0.19 (− 0.09–0.46) |
| Anxiety studies | |||||||||
| Christensen et al. (2014); iChill | 23 | 25.6 | 558; 80.6% female | RCT | 5-Arm: iChill with and without email and phone vs. Health Watch Control with and without phone | Home, prevention | CBT, education, physical activity promotion, relaxation, mindfulness meditation | 12 month GAD-7: ES = 0.31 (− 0.05–0.67); Post-test CES-D: ES = 0.66 (0.29–1.01) | 12 month GAD-7: ES = 0.79 (0.45–1.13); Post-test CES-D: ES = 0.67 (0.34–0.99) |
| Calear et al. (2016); Y-Worri/E-couch Anxiety and Worry program | 24.5 | 14.8 | 1767; 62.8% female | RCT | Externally-supported vs. Teacher-supported vs. Wait-list control | School, prevention | CBT, education, relaxation, physical activity | 6 month e-GAD HS vs. control: GAD-7: ES = − 0.14 (− 0.28–0.00); SAS-A: ES = 0.23 (0.09–0.37); WEMWBS: ES = − 0.24 (− 0.38 −− 0.10) | None significant |
| Day et al. (2013) | 25 | 23.5 | 66; 89.3% female | RCT | Immediate vs. Delayed-access | Self-help, prevention | CBT, coaching, relaxation, education. Featured stimulation through videos, audio files, pictures and activities. | 6 week post-test DASS-21 Depression: ES = 0.25 (0.06–1.05), Anxiety: ES = 0.67 (0.16–1.15), Stress: ES = 1.27 (0.73–1.78) maintained at 6 month f/u, w/o a sig. difference | 6 week post-test DASS-21 Depression: ES = 1.13 (0.60–1.63), Anxiety: ES = 1.17 (0.63–1.68), Stress: ES = 0.15 (− 0.33–0.64) |
| De Voogd et al. (2016) | 23.5 | 14.4 | 340; 57.6% female | RCT | Dot probe vs. visual search-based attentional training vs. 2 placebo controls | Home, early intervention | Visual search & dot-probe attention training | 6-month vs. SCARED: ES = 0.14 (− 0.23–0.5); 6-months vs. training CDI: ES = 0.01 (− 0.36–0.37); 12-month vs. RSES: ES = 0.14 (− 0.23–0.5) | 6-month vs. SCARED: ES = 0.33 (0.08–0.58); 6-month vs. CDI: ES = 0.43 (0.18–0.68); 12-month vs. RSES: ES = 0.48 (0.13–0.23) |
| Tillfors et al. (2011) | 24.5 | 16.5 | 19; 89% female | RCT | iCBT vs. wait-list control | Self-help, early intervention | Education, cognitive restructuring, exposure. | Posttest: Social anxiety LSAS-SR Fear: ES = 1.48; LSAS-SR Avoidance: ES = 1.13; Social phobia SPSQ-C: ES = 1.28; Depression MADRS-S: ES = 1.39; Anxiety BAI: ES = 1.47 | Posttest: Social anxiety LSAS-SR Fear: ES = 0.91; LSAS-SR Avoidance: ES = 0.55; Social phobia SPSQ-C: ES = 1.06; Depression MADRS-S: ES = 1.12; Anxiety BAI: ES = 0.97 |
| Räsänen et al. (2016); The Student Compass/Opiskelijan Kompassi | 24 | 24.29 | 68; 85.3% female | RCT | Online Acceptance and Commitment Therapy (iACT) vs. Waitlist control | Home, coach-guided, early intervention | Education, wellbeing tasks, metaphors, coaching, relaxation, case studies. Engagement through downloadable audio MP3s, educational videos and exercises. Coaches tailored program to students' individual needs. | Post-test: Depression BDI-II: ES = 0.69; Stress PSS: ES = 0.54; Wellbeing MHC-SF: ES = 0.46; Mindfulness skills FFMQ: ES = 0.49; Coherence OLQ-13: ES = 0.53 | Post-test: Depression BDI-II: ES = 1.12; Stress PSS: ES = 0.76; Wellbeing MHC-SF: ES = 0.61; Mindfulness skills FFMQ: ES = 0.62; Coherence OLQ-13: ES = 0.52 |
| Cox et al. (2009); So You've Been In an Accident | 23 | 7–16 | 85; 26 females, 59 males | RCT | Website and booklet vs. Assessment only | Home, early intervention | CBT, resiliency, relaxation, coping, problem solving, reflection | TSCC-A anxiety subscale: ES = − 0.33 (− 0.86–1.9) | None significant |
| Ruggiero et al. (2015); Bounce Back Now (BBN) | 23 | 14.5 | 2000; 51% female | RCT | BBN vs. BBN + ASH (Adult Self Help) vs. Assessment only | Home, Prevention | Education, PTSD (exposure, coping, anxiety management), Depression (BA), Substance abuse (CBT, motivational enhancement). Used text, graphics, videos, quizzes and animations to engage users. | 12 month PTSD: ES = 0.19 (− 0.03–0.41); Depression: ES = 0.19 (− 0.03–0.41) | 12 month PTSD: ES = 0.52 (0.34–0.70); Depression: ES = 0.47 (0.29–0.65) |
| Lenhard et al. (2014); BiP OCD (BarnInternetProjektet) | Not a control study; index not assessed | 14.4 | 21; 61.9% female | Clinical trial | None | Home, Treatment | CBT and education delivered through film, exercises, animations and interactive scripts. | N/A (only one group) | Post-test CY-BOCS: ES = 2.29 (1.5–3.07); 6 month CY-BOCS: ES = 2.35 (1.5–3.18); No changes between 3 and 6 months. Pre/6-month ES = 2.35. |
| Turner et al. (2014) | 24.5 | 14.35 | 72; 52.8% male | RCT | Telephone-CBT vs. CBT (non-inferiority) | Telephone, treatment | CBT, exposure with response prevention (E/RP), relapse prevention, psychoeducation | 6 month CY-BOCS: ES = − 0.13 (− 0.59–0.34) | 6 month CY-BOCS: ES = 1.97 (1.38–2.51); 6 month CDI-Y: ES = 1.13 (0.62–1.61) |
3. Results
3.1. Manuscripts presented by mental disorder category
3.1.1. Depression
Our review identified ten articles matching our inclusion criteria that investigated depression symptoms as the primary outcome (Table 1).
Three of these were from different time-points of the CATCH-IT (Competent Adulthood Transition with Cognitive-behavioral and Interpersonal Training) intervention in the Midwestern and Southern United States. The CATCH-IT intervention is a primary care-centered website designed to prevent depression in at-risk adolescents. It consists of 14 online modules focused on behavioral activation, CBT, interpersonal psychotherapy (IPT) and community resiliency. Eighty-four participants were initially enrolled in either the motivational interviewing (MI) group (10–15 min with therapist) or the brief advice (BA) group (1–2 min with therapist). In the most recent manuscript from Project CATCH-IT, 44 adolescents (52%) were followed-up at 2.5 years post-enrollment (Richards et al., 2016). They had a mean age of 19.64 years (SD = 2.18). When looking at depression with the Center for Epidemological Studies Depression (CESD-10) and Patient Health Questionnaire Adolescent (PHQ-A) at 2.5 years follow-up, the cohort's effect sizes showed improvement. Loneliness scores, hopelessness scores and the percentage of the group with significant depression symptoms (CESD-10 > 9) also decreased. There were no significant differences noted between the MI and BA groups. The effects of the intervention persisted from the 6-months to 2.5-years follow-up, seen in the continued reductions in depression symptoms and percentage of subsyndromal depression (Hoek et al., 2011, Saulsberry et al., 2013a). The between-group differences in number of depressive episodes and hopelessness that were noted at 6-months follow-up were not seen in the 2.5-years follow-up, where there were no significant differences noted between the MI and BA groups. The largest limitation of CATCH-IT involves its high dropout rate. Moreover, because no data were collected on those who dropped out, there is a potential for attrition bias.
Grasp the Opportunity took place in Hong Kong and included the CBT, behavioral activation and resiliency themes from the original CATCH-IT website (Ip et al., 2016). IPT and MI/BA were excluded as they were found to be culturally inappropriate (Sobowale et al., 2013). In this study, 257 Chinese youth with a mean age of 14.63 years (SD = 0.81) were asked to work through 10 online depression prevention modules. The difference between the intervention and control groups showed benefit at 12-months follow-up. Overall, the study was well conducted, but was not blinded. The possibility of a Hawthorne effect increasing reported efficacy of the intervention arm was noted by the authors as well.
SPARX is a fantasy videogame from the Netherlands that uses CBT principles to help adolescents with depressive symptoms over 7 weeks. The randomized controlled trial by Poppelaars et al. compares SPARX to a control group, and to a face-to-face, psychologist-run depression intervention, Op Volle Kracht (OVK) (Poppelaars et al., 2016). The 208 girls were aged 13.35 (SD = 0.71) years on average. At the 12 month follow-up there was a large decrease in the girls' Reynolds Adolescent Depression Scale (RADS-2) scores. The study was robust in its head-to-head design and screening for suicidal ideation deserves special praise. Unfortunately, the study was limited in its ability to truly blind subjects to which arm they received, which raises internal validity concerns.
Grip op Je Dip (Dutch for Master your Mood/MYM) Online is a Dutch prevention intervention for adolescents with subclinical depression (van der Zanden et al., 2012). It consists of six 90-minute online chat room sessions focused on CBT, behavioral activation, and future planning. In this RCT, 244 participants with a mean age of 20.9 (SD = 2.2) years were randomized to either MYM or a waitlist control condition. At the 3 months, ITT analysis, the between-group analysis showed benefit for CESD-D scores and Hospital Anxiety and Depression Scale (HADS) scores. These significant reductions in depression and anxiety continued into the 6-month follow-up. The greatest limitation in this study is its wait-list control design, which raises concerns on the validity of 6 month results. Additionally, participants were largely female and educated, limiting generalizability.
PratenOnline is a one-on-one chat intervention with trained professionals running Solution-Focused Brief Therapy (SFBT) (Kramer et al., 2014). This study from Urecht, Netherlands randomized 263 adolescents with a mean age of 19.5 (SD = 1.7) to PratenOnline or a wait-list control. This study found significant between group decreases in CESD scores at 9 weeks (ES = 0.18, CI: − 0.10–0.47) and 4.5 months. The depressive symptom scores for the intervention continued to decrease steadily from post-intervention to the 7.5-month follow-up. A large effect size was found when comparing the CESD scores between baseline and 7.5 months. These large effect sizes must be interpreted with skepticism due to the large attrition and low participation rate (58% of participants attended zero sessions).
An Australian intervention for youth called the DEAL Project targets co-occurring depression and alcohol misuse (Deady et al., 2016). This 4-week online intervention includes four 1-hour modules in the areas of CBT, MI, psychoeducation, behavioral activation, mindfulness, relaxation and coping. One hundred and four young adults were randomized to the DEAL Project or an online attention control group. Participants' PHQ-9 scores continued to decrease from post-treatment follow-up (ES = 1.09) to 6-month follow-up. Although there was a significantly larger reduction in depressive scores for the treatment group than the control group post-treatment, there were no differences between groups at 3- and 6-month follow-ups. TOT-AL scores were used to measure alcohol use quantity (drinks per week) and frequency (drinking days per week). There were large within-group effect sizes for quantity (ES = 0.76) and frequency (ES = 0.89) of alcohol use in the treatment group at the 3-month follow-up. However, there were no statistically significant changes from 3- to 6-month follow-ups. As participants were opportunistically collected, this sample may represent a group more amendable to treatment. Additional concerns of this study are its low completion rate (one third did not complete the program).
Low-Intensity Cognitive Behavioral Therapy (LI-CBT) was tested on 107 students with subclinical depression from University of Queensland, Australia, to improve mental health (Stallman et al., 2016). The mean participant age was 23 (SD = 6.4), and 92% were female. They were randomized to either an LI-CBT arm or a self-help control arm. Trained well-being coaches ran initial assessment sessions to personalize the intervention content for each participant. There were up to 7 sessions over telephone or Skype, with LI-CBT content including behavioral activation, exposure therapy, problem solving, sleep hygiene and relapse prevention. Students were encouraged to seek outside support and online mental health interventions. There were significant within-group effects for depression and anxiety at 2 months. Improvements were seen between baseline and the 12-month follow-up on the DASS-Stress, 5-item World Health Organization Well-Being Index (WHO5), and Coping Self-Efficacy scale (CSE). However, the LI-CBT arm had a significant decrease in connectedness (University Connectedness Scale, UCS), while the self-help control had a significant increase in UCS scores. As stated previously, generalizability is limited by the overwhelmingly college-educated, female population. Few participants attended any sessions (58%), which is concerning for internal validity.
Taylor et al. (2016) tested the effects of an online intervention, Image and Mood (IaM), on 206 female students at very high risk of developing an eating disorder (ED) with comorbid depression. The students were 20 years old on average (SD = 1.8), and were randomized to either an iCBT or wait-list control group. The 10-week active intervention consisted of CBT, IPT, behavioral activation, stress management (relaxation training), problem solving, college transition and a discussion board. In a subgroup of 27 participants with baseline depression, there was a significantly larger decrease in depression on the BDI-II. In the iCBT group, there was a 27% lower rate of ED onset, although this was nonsignificant. There were significant within-group effects for the intervention at 1-year follow-up on the EDE-Q Global and BDI-II. While this study had great ethnic diversity, external validity is a concern due to its college based enrollment.
3.1.2. Anxiety
Our review identified 5 articles primarily targeting youth anxiety that matched our inclusion criteria (Table 1). iChill is a 10-week Australian Internet intervention consisting of five trial arms based on the presence of email or telephone reminders: Active, active with telephone, active with email, control and control with telephone (Christensen et al., 2014). The 10 modules integrated CBT, psychoeducation, physical activity promotion, relaxation and mindfulness meditation techniques. There were 558 participants with a mean age of 25.64 years (SD = 3.22). There was a significantly higher improvement in Generalized Anxiety Disorder (GAD-7) scores at 12 months for the active with telephone condition when compared to the control with telephone condition. Unlike the other groups, which demonstrated increases in GAD-7 scores between 6 and 12 months, the active with telephone arm continued to show large reductions in anxiety at 12 months when compared to baseline. The Anxiety Sensitivity Index (ASI) and Penn State Worry Questionnaire (PSWQ) scores were also significantly lower in the active with email arm than the control arm at post-test. They found a significant reduction in Days out of Role due to anxiety for the active with email arm at the 12-month follow-up. While there was moderate loss to follow up (47%) and a predominantly female study population, the major limit to generalizability was excluding participants with comorbid conditions (e.g. social phobia or PTSD).
The Y-Worri/E-couch Anxiety and Worry program is an RCT from Australia (Calear et al., 2016). 1767 students (mean age 14.83 years, SD = 0.97) from 30 schools were enrolled in either an externally supported arm (e-GAD health service/HS, with the presence of a helpful headspace officer), a teacher-supported arm (e-GAD school) or a wait-list control arm. The students spent 30–40 min per week for 6 weeks on the Internet intervention at school. The material consisted of CBT, psychoeducation, relaxation and physical activity. A significant condition-by-time interaction for mental well-being [Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS)] was found that favored the wait-list control arm. At 6-months follow-up, when comparing the e-GAD HS to the control group, there were significant reductions in anxiety, reductions in social anxiety [Social Anxiety Scale for Adolescents (SAS-A)], and increases in well-being (WEMWBS). There were also significant reductions in anxiety at post-test, well-being at post-test and well-being at 6 months (ES = − 0.30, CI = − 0.45 to − 0.14) when comparing e-GAD school to the control condition. Some study strengths included using a wait-list control and randomized schools. Two methodological difficulties were N = 2 schools withdrawing themselves from the study and significant between-group differences at baseline (particularly “language other than English”). The authors noted “language other than English” was associated with attrition.
A RCT by Day et al. (2013) was performed with 66 Canadian university students to test the effects of a self-help intervention to improve scores on the Depression, Anxiety and Stress Scale-21 (DASS-21). They were assigned to either a delayed-access or an immediate-access group, where they completed 5 modules over 6 weeks. The content containing CBT, coaching, relaxation and psychoeducation also included videos, audio files, pictures and activities. At post-test, the students had significant decreases in depression, anxiety, and stress on the DASS-21 when compared to the delayed-access control group. When comparing post-test DASS-21 scores for the immediate-access group to their baseline scores, there were large effect sizes for depression and anxiety, and a small effect size for stress. These improvements in the students' depression, anxiety and stress levels were maintained at the 6-month follow-up. While encouraging, generalizability is limited. The enrollees did not represent the general population (89% of enrollees are female). Also, these findings may be weakened by low 6 month assessment completion rates; 51.5% (N = 17) of the immediate intervention arm and 21.2% (N = 7) wait-list control participants completed.
De Voogd et al. (2016) performed an RCT using online attentional bias modification training to improve the mental health of 340 high school students in the Netherlands. The participants were randomized to either dot-probe attentional training, visual search-based attentional training, visual search placebo or dot-probe placebo groups. The first training session was supervised at school, and the 7 remaining online sessions were done at home. Based on the Emotional Visual Search Task (ESVT), there was a significant reduction in negative attentional bias for the visual search group. No significant differences between active and control conditions were found for depressive symptoms, anxiety symptoms or emotional resilience when measured by using the Children's Depression Inventory (CDI), Screen for Child Anxiety Related Emotional Disorders (SCARED) and a number of other scales. However, at 6 months there were improvements in depression, anxiety, and resilience across all groups in the study compared to baseline. Generating a placebo adds great methodological rigor to these results, despite the somewhat reduced completion rate (only 24% of participants completed all modules).
Tillfors et al. (2011) performed an RCT in Sweden using online CBT (iCBT) to reduce social anxiety, depression and general anxiety in high school students. 19 students were randomized to either an iCBT condition or a wait-list control condition. The 9-week intervention consisted of psychoeducation, cognitive restructuring and exposure therapy. It included interactive components such as essay questions and multiple-choice quizzes. At post-test, when the iCBT group was compared to the control group, there were significant decreases in scores for social anxiety measured by the Liebowitz Social Anxiety Scale (LSAS-SR) for Fear and the LSAS-SR for Avoidance; social phobia measured by the Social Phobia Screening Questionnaire (SPSQ-C); depression measured by the Montgomery-Asberg Depression Rating Scale (MADRS-S); and anxiety measured by the Beck Anxiety Inventory (BAI). These reductions were maintained at the 1-year follow-up, but general anxiety scores reverted to pre-test levels at this time point. These results are promising, but potentially limited in statistical power (small sample size), generalizability (participants were from one geographic area), and internal validity (passive wait list control arm).
3.1.3. Well-being
The Student Compass, Opiskelijan Kompassi in Finnish is an early intervention for university students, which was designed to improve well-being and mental health (Räsänen et al., 2016). 68 students were randomized to the Online Acceptance and Commitment Therapy (iACT) group or the wait-list control group. The Student Compass consisted of 2 coach-guided face-to-face sessions and 5 online sessions done from home. These coaches tailored the program to the students' individual needs. It included content such as psychoeducation, well-being tasks, metaphors, coaching, relaxation and case studies. Engagement was increased through downloadable audio MP3s, educational videos and exercises. Participants' rated their mental health with the Mental Health Continuum-Short Form (MHC-SF) for well-being, BDI-II for depression, Perceived Stress Scale-10 (PSS-10) for stress, Five Facet Mindfulness Questionnaire (FFMQ) for mindfulness and Orientation to Life Questionnaire (OLQ-13) for sense of coherence. When comparing the active intervention to the control group at post-test, significant improvements were found in the students' well-being (MHC-SF), depression (BDI-II), stress (PSS-10), mindfulness skills (FFMQ) and sense of coherence (OLQ-13). They also uncovered significant within-group improvements in all the above categories at post-test, and the effects persisted at 12 months. The Student Compass was highly effective in generating participation — 9.3% dropped out and 79% completed all modules and 12 month follow up. This study's generalizability is limited by its college-age, female sample (85% female).
3.1.4. Post-trauma
So You've Been In An Accident is an Australian website (http://kidsaccident.psy.uq.edu.au) for children following unintentional injury.(Cox et al., 2009) 85 children with a mean age of 10.9 (SD = 2.18) were randomized to a control group or a 5-month self-help Internet intervention consisting of CBT, resiliency, relaxation, coping, problem-solving and reflection concepts. The parents of the affected children were given a 4-page booklet with informational material. The Trauma Symptom Checklist for Children-A (TSCC-A) Anxiety subscale scores for the intervention group was significantly lower than the control group. There were also improvements that did not reach significance in the other subsets of the TSCC-A (posttraumatic stress, depression, anger, dissociative) compared to the control group. At the 6-month follow-up, the intervention group had a large within-group effect size for the TSCC-A Anxiety subscale (ES = 0.47, CI = − 0.06–0.98). No significant differences were found between the parents in the intervention and control groups. Some concerns with this study include low participation with materials and high dropout (34%). While unblinded, this was the first randomized control study of this type.
Bounce Back Now (BBN) is a website used to improve mental health symptoms in youth following disasters. Ruggiero et al. (2015) studied its effects on a sample of 2000 adolescents who experienced tornadoes. The mean age of the children was 14.5 (SD = 1.7) and 51% were female. They were randomized to three study groups: BBN, BBN + ASH (Adult Self Help, which contained an additional 7 modules for parents of the affected youth), and an assessment-only control group. The 4-module BBN website used strategies such as psychoeducation, exposure, coping, anxiety management, behavioral activation, CBT and motivational enhancement. Text, graphics, videos, quizzes and animations were implemented to engage users. At the 12-month follow-up, there were significant decreases in PTSD symptoms and depressive symptoms in the BBN as compared to the control group. There was also a significantly larger decrease in depressive symptoms in the BBN group when compared to the BBN + ASH group at 12 months. No significant differences between groups were found for alcohol and tobacco use. This study's major strength was its large sample with relatively robust diversity. Engagement with the website was self-reported, and thus subject to recall bias.
3.1.5. Obsessive compulsive disorder (OCD)
A Swedish clinical trial called BiP OCD (BarnInternetProjektet) was used to reduce OCD symptoms in adolescents (Lenhard et al., 2014). The 21 participants in the study had a mean age of 14.4 years old (SD = 2.64). The 12-week, 12-chapter Internet-based intervention consisted of CBT and education delivered through film, exercises, animations and interactive scripts. Trained clinical psychologists followed the teens to help with the treatment and offer encouragement. The parents of the participants were also given 5 chapters as an adjunct to the core program for the adolescents to boost effectiveness. At post-test, there was a significantly large improvement in the participants' Children's Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) scores, with an effect size of d = 2.29. The significant improvement in CY-BOCS scores from post-test to 3 months had an effect size of d = 0.67 (CI = 0.04–1.3). These reductions in OCD symptoms were maintained at the 6-month follow-up, but did not improve further. This study represents an encouraging, but preliminary study. As such, its key limitations are small sample size and lack of control arm, reducing its ability to control for nonspecific factors.
Turner et al. (2014) performed a randomized controlled non-inferiority trial to compare face-to-face CBT with Telephone-CBT (TCBT) in 72 adolescents with OCD. The participants had a mean age of 14.35 (SD = 2.13) years old. In the TCBT group, 14 telephone sessions were conducted with trained therapists. The content of the intervention for both groups consisted of CBT, exposure with response prevention (E/RP), relapse prevention and psychoeducation. The teens had improvements in their OCD symptoms on the CY-BOCS at every time-point, with a 6-month effect size of d = 1.97. This improvement was also seen for depression symptoms on the Beck Depression Inventory for Youth (BDI-Y). It was found that for every assessment until the 6-month follow-up, TCBT was non-inferior to face-to-face CBT sessions. While this study was randomized, it lacks a non-intervention control arm. Additionally, an arguably high non-inferiority threshold was chosen. More study with a lower threshold would confirm non-inferiority.
3.2. Behavioral Vaccine Model elements in the manuscripts
3.2.1. Effective components
3.2.1.1. Comparative effectiveness
For the content of an Internet-based intervention to be seen as helpful, it should have a higher comparative effectiveness than traditional interventions. The eight studies in this review that were focused on preventing depression had between-group effect sizes ranging from 0.05 to 0.96. When comparing the active to the control conditions for the papers preventing general anxiety, effect sizes ranged from 0.14 to 0.67. For PTSD, the range of between-group effect sizes was 0.19 to 0.33. The BiP OCD intervention did not have a control condition for comparison. The between-group effect size for the other OCD study was 0.13, which showed non-inferiority of telephone CBT when compared to face-to-face CBT (Turner et al., 2014). For the social anxiety, eating disorders and well-being interventions, the between-group effect sizes were 1.48, 0.31 and 0.46, respectively. The interventions reviewed were as effective or more effective at improving mental health symptoms than their respective controls.
3.2.1.2. Duration of benefits
The improvements made to mental health symptoms should be maintained over a long time to truly be effective. All of the studies in this review conducted at least a 6-month follow-up, and 14 of the studies performed a 12-month follow-up. Image and Mood (IaM) and CATCH-IT performed 2-year and 2.5-year follow-ups, respectively. When comparing depression symptoms at baseline to depression symptoms at long-term follow-up, effect sizes ranged from 0.09 to 2.35, showing the significant prolonged benefits of Internet interventions. Although a number of the interventions had waning effects at later time points, the mental health scores were still improved from the baseline values, and non-inferior to the control conditions.
3.2.1.3. Socio-cultural relevance
It is important for studies of interventions to be generalizable, and for there to be diversity of the study group. In 18 out of the 20 papers reviewed, there was a female predominance, with the percentage of females ranging from 51% to 100%. The reviewed studies spanned a large geographical area and represented a variety of cultures. Five articles were from the United States (Richards et al., 2016, Hoek et al., 2011, Saulsberry et al., 2013a, Taylor et al., 2016, Ruggiero et al., 2015), and studies were found from Australia (Deady et al., 2016, Stallman et al., 2016, Christensen et al., 2014, Calear et al., 2016, Cox et al., 2009), the Netherlands (Poppelaars et al., 2016, van der Zanden et al., 2012, Kramer et al., 2014), Sweden (De Voogd et al., 2016, Poppelaars et al., 2016, Lenhard et al., 2014), the United Kingdom (Turner et al., 2014), Finland (Räsänen et al., 2016), China (Ip et al., 2016), and Canada (Day et al., 2013).
Nine studies identified in the review mentioned the ethnicities of their participants. The interventions performed in the United States and Australia ranged from 51% to 76.19% white participants. The interventions from Europe and China were almost entirely composed of European and Chinese participants, respectively. Little mention could be found about making the interventions applicable to diverse groups of people. The stories in the CATCH-IT website are from adolescents with varied experiences, with the intent that youth from various cultural backgrounds could find the site appropriate (Van Voorhees et al., 2008). CATCH-IT was designed to be used by diverse groups, and has undergone adaptations for Chinese, African American and Latino American youth (Saulsberry et al., 2013a, Ip et al., 2016).
Seven studies mentioned parental education, which ranged from the parents completing at least middle school, to most of the parents completing at least some college education. Bounce Back Now (BBN) reported that the parents' median annual income ranged from $40,000 to $60,000 (Ruggiero et al., 2015).
3.2.2. Framework for motivation
3.2.2.1. Degree of professional guidance
Thirteen of the reviewed interventions mentioned motivational techniques and some form of guidance from the study operators. Seven studies used email correspondence to encourage completion and provide clarification, while a few used text-message or phone-call reminders. The Student Compass intervention provided personalized feedback and content to participants over email (Räsänen et al., 2016). For some of the studies, guidance and motivation was provided by teachers (Ip et al., 2016, Calear et al., 2016), PCPs (Richards et al., 2016, Hoek et al., 2011, Saulsberry et al., 2013a), and telephone/Skype therapists (Stallman et al., 2016, Turner et al., 2014).
3.2.2.2. Peer-to-peer support
The only intervention in this review that facilitated peer-to-peer conversation was Image and Mood, where moderators posted questions on the Discussion Board to encourage conversations (Taylor et al., 2016). There was an average of 3.2 (SD = 4.5) posts to the Discussion Board per participant.
Parents of affected youth can function as strong supports if recruited into the prevention process. Six of the reviewed studies involved parents significantly in their interventions. In the three studies of the CATCH-IT website, parents were given resiliency training to strengthen family life (Hoek et al., 2011). The So You've Been In An Accident intervention provided parents with a 4-page booklet about parent and child coping and emotional recovery (Cox et al., 2009); however, in this study no significant differences were found between the parents in the intervention and control groups. In the study by Ruggiero et al. (2015), parents in the Bounce Back Now + Adult Self Help group were given access to an additional 7 modules for their own mental health, called Disaster Recovery Web. The BiP OCD Website featured 5 chapters for parents about family accommodation and coping techniques (Lenhard et al., 2014).
3.2.2.3. Adherence
All 20 studies measured their participants' adherence to the interventions. Completion of all provided modules ranged from 24% to 85%. However, a number of the studies deemed that participants did not need to complete every single module to consider that the full intervention was received. PratenOnline noted high attrition rates; their participants only completed an average of 1.36 (SD = 2.08) sessions (Kramer et al., 2014).
3.2.3. Implementation structure
3.2.3.1. Delivery mechanisms
Thirteen interventions in this review mentioned ways in which they increase the user's attention to the material. This included videos/animations, stories, chats with a therapist online or over the phone, audio/downloadable MP3 files, graphics, quizzes, exercises/activities and discussion boards (Richards et al., 2016, Hoek et al., 2011, Saulsberry et al., 2013a, Ip et al., 2016, Kramer et al., 2014, Stallman et al., 2016, Taylor et al., 2016, Day et al., 2013, Tillfors et al., 2011, Räsänen et al., 2016, Ruggiero et al., 2015, Lenhard et al., 2014, Turner et al., 2014).
These mechanisms were also implemented to improve satisfaction, which eight studies investigated. Out of a highest possible satisfaction rating of 10, the intervention ratings ranged from 6.32 to 9.12.
3.2.3.2. Delivery context
The participants accessed eighteen of the interventions from their own homes. This included two interventions where CBT was delivered over the phone or Skype (Stallman et al., 2016, Turner et al., 2014). Two of the studies delivered their programs primarily at school, during free periods or during an allotted time, under supervision (Ip et al., 2016, Calear et al., 2016, Turner et al., 2014). Poppelaars et al. (2016) compared a home-based intervention, SPARX, to a school-based intervention, Op Volle Kracht (OVK), and found no significant difference between depressive symptoms at all time-points (Poppelaars et al., 2016). At 12 months, there was an effect size of 0.4 (CI = 0.00–0.79) in favor of SPARX.
3.2.3.3. Safety
Ten of the studies mentioned safety protocols for high-risk participants, although the two telephone-based and school-based interventions were also likely to be monitored by their proctors. Precautions in place included safety assessment calls and program coach supervision. When emergency cases were discovered, the adolescents were usually referred to their PCPs or given mental health help-seeking contacts.
4. Discussion
This is a rapid review of technology-based mood and anxiety health interventions for youth between 2010 and 2016. This review is unique in that it exclusively investigates preventative interventions with duration of follow-up > 6 months. Twenty studies were identified from across the globe. Nineteen of these were RCTs, and BiP OCD was a clinical trial.
The Behavioral Vaccine Model used in this review allowed for a wholesome analysis of the interventions (Van Voorhees et al., 2011). First, the Effective Components were reviewed. There was a good degree of comparative effectiveness because in all cases, the active interventions were equal or better than their control conditions at improving their primary outcomes. For a study to truly be classified as an efficient and effective prevention intervention, there needs to be a prolonged duration of benefits. This was demonstrated in all of the above interventions, where the improvements in mental health continued past 6 months.
The sociocultural relevance of the studies is important to consider, as well. Eighteen of the studies had a majority of females, which aligns with expectations, as females have been found to have a higher incidence and prevalence of internalizing disorders (Piccinelli and Wilkinson, 2000). Of the papers that mentioned parental characteristics, the studied children generally had parents with more education and higher incomes. For interventions to be applicable to youth of various socioeconomic demographics, the interventions should include underprivileged groups in their trials (Airhihenbuwa, 1990). Study creators should strive to achieve participant populations of all sociocultural demographics in order to truly gauge their interventions' public health benefits. Adapting interventions for other cultural groups is an effective way to enhance their palatability. For example, CATCH-IT has been modified for use with Chinese, Latino and African-American adolescents (Sobowale et al., 2013, Saulsberry et al., 2013b).
The Framework for Motivation was the second category of the Behavioural Vaccine Model that was reviewed. Fifteen of the papers mentioned professional guidance that was used to boost user engagement. One of these interventions found that the group with motivational interviewing had fewer depressive episodes and reported less hopelessness than the brief advice group (Saulsberry et al., 2013a). Interestingly, this difference between groups disappeared at the 2.5-year follow-up (Richards et al., 2016).
Discussion with like-minded peers has been shown to be of use in reducing eating disorder symptoms (Kass et al., 2014) and likely depressive symptoms as well (Griffiths et al., 2009). Although the Image and Mood eating disorder intervention that used a discussion board showed limited activity with an average of 3.2 posts per adolescent, the effect sizes in the study ranged from medium to large. University students with depressive symptoms reported that using an online peer forum helped them with loneliness, and created a space for giving and receiving support (Horgan et al., 2013). However, it has been found that social network services (SNS) have the potential to cause a negative downward spiral, especially when interacting with peers who have a negative view of the SNS, or severely depressed peers (Takahashi et al., 2009).
Parents can also aid in the mental health prevention process (Wickramaratne et al., 2011). However, in the BBN study, there were smaller reductions in depressive symptoms in the Adult Self Help group. While some parent mental health education should be provided, Ruggiero et al. (2015) suggest that the focus in youth interventions should be on improving youth mental health (Ruggiero et al., 2015).
The Implementation Structure is the final category we examined, which looked at the interventions' delivery methods. Regarding the types of technology used in the interventions, there were sixteen studies with Internet modules, one study with an online game, one study with online chat-room sessions, and two studies with telephone interventions. Turner et al. (2014) found that telephone CBT (TCBT) was non-inferior to face-to-face CBT at reducing OCD symptoms (Turner et al., 2014). Interestingly, 77.8% of participants in the TCBT condition responded that they were very happy, while only 40.7% felt this way in the face-to-face CBT condition. In telemental health interventions, especially those targeted for the youth population, it is important to use entertainment techniques in order to boost engagement (Sobowale et al., 2013). Informational media alternatives to text were used in thirteen of the interventions in this review, and satisfaction rates were high.
Only eight studies looked at participant satisfaction, which is a useful way to understand reception of an intervention. For example, in the iChill intervention, Christensen et al. (2014) found that 37.8% of youth preferred the active website with email reminders trial condition, while only 5.6% preferred the conditions with telephone reminders (Christensen et al., 2014). This valuable feedback should be used to guide future intervention design.
Mental health interventions intended for public dissemination should include safety protocols for emergency cases. Only seven of the interventions in this review commented on participant safety. One-on-one monitoring might not be practical in a large public health setting, so a useful mechanism might be to program alerts for keywords that might signal high risk for harm or disease exacerbation.
Some limitations of this paper are that papers in languages other than English and grey literature were not included. In addition, rapid reviews are meant to assess the available literature on a particular subject, while making some concessions on the depth of quality appraisal (Grant and Booth, 2009). A full systematic review would offer a deeper analysis of the studies. Future studies should focus on implementation of already efficacious mental health interventions.
5. Conclusion
As we can see in this review, there are a small number of telemental health interventions with long-term follow-up in the pediatric population. The twenty papers identified showcase the potential effectiveness of technology-based interventions at reducing the burden of youth mood and anxiety disorders on a global scale. There is substantial evidence that these interventions are beneficial to youth recruited via mechanisms that likely select motivated participants. However, as can be seen in this review, the elements key to effectiveness and implementation are often not included in many of these studies - such as population based recruiting, implementation in real world settings and systems to enhance motivation for completion. Henceforth, the field should move toward implementation and effectiveness research, with a focus on increasing public health impact through substantial “reach” according to Glasgow's RE-AIM model. In particular, there needs to be a strong focus on motivational and implementation models.
Acknowledgement
During the period in which this review was written, Dr. Gladstone and Dr. Van Voorhees received support from the National Institutes of Mental Health 1 RO1 MH090035-01A1 (Primary Care Internet Based Depression Prevention for Adolescents, CATCH-IT 3).
Footnotes
This paper is being revised for resubmission to Internet Interventions.
As study coordinator for PATH, an internet-based clinical trial (funded by NIMH RO1 MH090035-01A1), I am taking lead editing responsibilities for this review article.
References
- Airhihenbuwa C.O. A conceptual model for culturally appropriate health education programs in developing countries. Int. Q. Community Health Educ. 1990;11(1):53–62. doi: 10.2190/LPKH-PMPJ-DBW9-FP6X. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med. J. Aust. 2010;192(11):S12. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Batterham P.J., Poyser C.T., Mackinnon A.J., Griffiths K.M., Christensen H. Cluster randomised controlled trial of the e-couch Anxiety and Worry program in schools. J. Affect. Disord. 2016;196:210–217. doi: 10.1016/j.jad.2016.02.049. [DOI] [PubMed] [Google Scholar]
- Christensen H., Batterham P., Mackinnon A., Griffiths K.M., Hehir K.K., Kenardy J.…Bennett K. Prevention of generalized anxiety disorder using a web intervention, iChill: randomized controlled trial. J. Med. Internet Res. 2014;16(9) doi: 10.2196/jmir.3507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox C.M., Kenardy J.A., Hendrikz J.K. A randomized controlled trial of a web-based early intervention for children and their parents following unintentional injury. J. Pediatr. Psychol. 2009:jsp095. doi: 10.1093/jpepsy/jsp095. [DOI] [PubMed] [Google Scholar]
- Day V., McGrath P.J., Wojtowicz M. Internet-based guided self-help for university students with anxiety, depression and stress: a randomized controlled clinical trial. Behav. Res. Ther. 2013;51(7):344–351. doi: 10.1016/j.brat.2013.03.003. [DOI] [PubMed] [Google Scholar]
- De Voogd E.L., Wiers R.W., Prins P.J.M., de Jong P.J., Boendermaker W.J., Zwitser R.J., Salemink E. Online attentional bias modification training targeting anxiety and depression in unselected adolescents: short-and long-term effects of a randomized controlled trial. Behav. Res. Ther. 2016;87:11–22. doi: 10.1016/j.brat.2016.08.018. [DOI] [PubMed] [Google Scholar]
- Deady M., Mills K.L., Teesson M., Kay-Lambkin F. An online intervention for co-occurring depression and problematic alcohol use in young people: primary outcomes from a randomized controlled trial. J. Med. Internet Res. 2016;18(3) doi: 10.2196/jmir.5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fombonne E., Wostear G., Cooper V., Harrington R., Rutter M. The Maudsley long-term follow-up of child and adolescent depression. Br. J. Psychiatry. 2001;179(3):210–217. doi: 10.1192/bjp.179.3.210. [DOI] [PubMed] [Google Scholar]
- Grant M.J., Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- Griffiths K.M., Calear A.L., Banfield M. Systematic review on Internet Support Groups (ISGs) and depression (1): do ISGs reduce depressive symptoms? J. Med. Internet Res. 2009;11(3) doi: 10.2196/jmir.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek W., Marko M., Fogel J., Schuurmans J., Gladstone T., Bradford N.…Van Voorhees B.W. Randomized controlled trial of primary care physician motivational interviewing versus brief advice to engage adolescents with an Internet-based depression prevention intervention: 6-month outcomes and predictors of improvement. Transl. Res. 2011;158(6):315–325. doi: 10.1016/j.trsl.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horgan A., McCarthy G., Sweeney J. An evaluation of an online peer support forum for university students with depressive symptoms. Arch. Psychiatr. Nurs. 2013;27(2):84–89. doi: 10.1016/j.apnu.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Ip P., Chim D., Chan K.L., Li T.M., Ho F.K.W., Voorhees B.W.…Tso W. Effectiveness of a culturally attuned Internet-based depression prevention program for Chinese adolescents: a randomized controlled trial. Depress. Anxiety. 2016;33(12):1123–1131. doi: 10.1002/da.22554. [DOI] [PubMed] [Google Scholar]
- Kass A.E., Trockel M., Safer D.L., Sinton M.M., Cunning D., Rizk M.T.…Wilfley D.E. Internet-based preventive intervention for reducing eating disorder risk: a randomized controlled trial comparing guided with unguided self-help. Behav. Res. Ther. 2014;63:90–98. doi: 10.1016/j.brat.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). "Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication": (Erratum). [DOI] [PubMed]
- Kim-Cohen J., Caspi A., Moffitt T.E., Harrington H., Milne B.J., Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch. Gen. Psychiatry. 2003;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. (Jul 1) [DOI] [PubMed] [Google Scholar]
- Kirsch S.E., Lewis F.M. Using the world wide web in health-related intervention research: a review of controlled trials. Comput. Inform. Nurs. 2004;22(1):8–18. doi: 10.1097/00024665-200401000-00005. (Jan 1) [DOI] [PubMed] [Google Scholar]
- Kramer J., Conijn B., Oijevaar P., Riper H. Effectiveness of a web-based solution-focused brief chat treatment for depressed adolescents and young adults: randomized controlled trial. J. Med. Internet Res. 2014;16(5) doi: 10.2196/jmir.3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latha K.S., Reddy H., Thergaonkar N.R., Wadkar A.J., Saz U.E., Arslan M.T.…Srinath S. Mental health policy for children and adolescents in developing countries. J. Indian Assoc. Child Adolesc. Ment. Health. 2007;3(1) [Google Scholar]
- Lenhard F., Vigerland S., Andersson E., Rück C., Mataix-Cols D., Thulin U.…Serlachius E. Internet-delivered cognitive behavior therapy for adolescents with obsessive-compulsive disorder: an open trial. PLoS One. 2014;9(6) doi: 10.1371/journal.pone.0100773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K.R., He J.P., Burstein M., Swanson S.A., Avenevoli S., Cui L.…Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J. Am. Acad. Child Adolesc. Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Flisher A.J., Hetrick S., McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- Piccinelli M., Wilkinson G. Gender differences in depression. Br. J. Psychiatry. 2000;177(6):486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Poppelaars M., Tak Y.R., Lichtwarck-Aschoff A., Engels R.C., Lobel A., Merry S.N.…Granic I. A randomized controlled trial comparing two cognitive-behavioral programs for adolescent girls with subclinical depression: a school-based program (Op Volle Kracht) and a computerized program (SPARX) Behav. Res. Ther. 2016;80:33–42. doi: 10.1016/j.brat.2016.03.005. [DOI] [PubMed] [Google Scholar]
- Rao U., Chen L. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin. Neurosci. 2009;11:45–62. doi: 10.31887/DCNS.2009.11.1/urao. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Räsänen P., Lappalainen P., Muotka J., Tolvanen A., Lappalainen R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: a randomized controlled clinical trial. Behav. Res. Ther. 2016;78:30–42. doi: 10.1016/j.brat.2016.01.001. [DOI] [PubMed] [Google Scholar]
- Richards K., Marko-Holguin M., Fogel J., Anker L., Ronayne J., Van Voorhees B.W. Randomized clinical trial of an internet-based intervention to prevent adolescent depression in a primary care setting (Catch-It): 2.5-year outcomes. J. Evid. Based Psychot. 2016;16(2):113. [PMC free article] [PubMed] [Google Scholar]
- Richardson T., Stallard P., Velleman S. Computerised cognitive behavioural therapy for the prevention and treatment of depression and anxiety in children and adolescents: a systematic review. Clin. Child. Fam. Psychol. Rev. 2010;13(3):275–290. doi: 10.1007/s10567-010-0069-9. [DOI] [PubMed] [Google Scholar]
- Ruggiero K.J., Price M., Adams Z., Stauffacher K., McCauley J., Danielson C.K.…Carpenter M.J. Web intervention for adolescents affected by disaster: population-based randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54(9):709–717. doi: 10.1016/j.jaac.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulsberry Alexandria, M. H. M., B. K., H. M. C. Randomized clinical trial of a primary care internet-based intervention to prevent adolescent depression: one-year outcomes. J. Can. Acad. Child Adolesc. Psychiatry. 2013;22(2):107. [PMC free article] [PubMed] [Google Scholar]
- Saulsberry A., Corden M.E., Taylor-Crawford K., Crawford T.J., Johnson M., Froemel J.…Van Voorhees B.W. Chicago urban resiliency building (CURB): an internet-based depression-prevention intervention for urban African-American and Latino adolescents. J. Child Fam. Stud. 2013;22(1):150–160. [Google Scholar]
- Sawyer M.G., Arney F.M., Baghurst P.A., Clark J.J., Graetz B.W., Kosky R.J.…Rey J.M. The mental health of young people in Australia: key findings from the child and adolescent component of the national survey of mental health and well-being. Aust. N. Z. J. Psychiatry. 2001;35(6):806–814. doi: 10.1046/j.1440-1614.2001.00964.x. [DOI] [PubMed] [Google Scholar]
- Siemer C.P., Fogel J., Van Voorhees B.W. Telemental health and web-based applications in children and adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2011;20(1):135–153. doi: 10.1016/j.chc.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobowale K., Zhou A.N., Van Voorhees B.W., Stewart S., Tsang A., Ip P.…Chim D. Adaptation of an internet-based depression prevention intervention for Chinese adolescents: from “CATCH-IT” to “grasp the opportunity”. Int. J. Adolesc. Med. Health. 2013;25(2):127–137. doi: 10.1515/ijamh-2013-0020. [DOI] [PubMed] [Google Scholar]
- Stallman H.M., Kavanagh D.J., Arklay A.R., Bennett-Levy J. Randomised control trial of a low-intensity cognitive-behaviour therapy intervention to improve mental health in university students. Aust. Psychol. 2016;51(2):145–153. [Google Scholar]
- Takahashi Y., Uchida C., Miyaki K., Sakai M., Shimbo T., Nakayama T. Potential benefits and harms of a peer support social network service on the internet for people with depressive tendencies: qualitative content analysis and social network analysis. J. Med. Internet Res. 2009;11(3) doi: 10.2196/jmir.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C.B., Kass A.E., Trockel M., Cunning D., Weisman H., Bailey J.…Wilfley D.E. Reducing eating disorder onset in a very high risk sample with significant comorbid depression: a randomized controlled trial. J. Consult. Clin. Psychol. 2016;84(5):402. doi: 10.1037/ccp0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tillfors M., Andersson G., Ekselius L., Furmark T., Lewenhaupt S., Karlsson A., Carlbring P. A randomized trial of internet-delivered treatment for social anxiety disorder in high school students. Cogn. Behav. Ther. 2011;40(2):147–157. doi: 10.1080/16506073.2011.555486. [DOI] [PubMed] [Google Scholar]
- Turner C.M., Mataix-Cols D., Lovell K., Krebs G., Lang K., Byford S., Heyman I. Telephone cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: a randomized controlled non-inferiority trial. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53(12):1298–1307. doi: 10.1016/j.jaac.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees B.W., Ellis J., Ford D.E. Pilot study of a primary care/web-based depression prevention intervention for young adults (project Catch-it) J. Gen. Intern. Med. 2005;20:187. [Google Scholar]
- Van Voorhees B.W., Vanderplough-Booth K., Fogel J., Gladstone T., Bell C., Stuart S.…Ross R. Integrative internet-based depression prevention for adolescents: a randomized clinical trial in primary care for vulnerability and protective factors. J. Can. Acad. Child Adolesc. Psychiatry. 2008;17(4):184. [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees B.W., Fogel J., Reinecke M.A., Gladstone T., Stuart S., Gollan J.…Larson J. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. J. Dev. Behav. Pediatr. 2009;30(1):23–37. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees B.W., Mahoney N., Mazo R., Barrera A.Z., Siemer C.P., Gladstone T.R., Muñoz R.F. Internet-based depression prevention over the life course: a call for behavioral vaccines. Psychiatr. Clin. N. Am. 2011;34(1):167–183. doi: 10.1016/j.psc.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhulst F.C., Achenbach T.M., Van der Ende J., Erol N., Lambert M.C., Leung P.W.…Zubrick S.R. Comparisons of problems reported by youths from seven countries. Am. J. Psychiatr. 2003;160(8):1479–1485. doi: 10.1176/appi.ajp.160.8.1479. [DOI] [PubMed] [Google Scholar]
- Waddell C., McEwan K., Shepherd C.A., Offord D.R., Hua J.M. A public health strategy to improve the mental health of Canadian children. Can. J. Psychiatr. 2005;50:226–233. doi: 10.1177/070674370505000406. [DOI] [PubMed] [Google Scholar]
- Waddell C., Hua J.M., Garland O.M., Peters R., McEwan K. Preventing mental disorders in children: a systematic review to inform policy-making. Can. J. Public Health. 2007:166–173. doi: 10.1007/BF03403706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickramaratne P., Gameroff M.J., Pilowsky D.J., Hughes C.W., Garber J., Malloy E.…Trivedi M.H. Children of depressed mothers 1 year after remission of maternal depression: findings from the STAR* D-Child study. Am. J. Psychiatr. 2011;168(6):593–602. doi: 10.1176/appi.ajp.2010.10010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson N., Ang R.P., Goh D.H. Online video game therapy for mental health concerns: a review. Int. J. Soc. Psychiatry. 2008;54(4):370–382. doi: 10.1177/0020764008091659. [DOI] [PubMed] [Google Scholar]
- van der Zanden R., Kramer J., Gerrits R., Cuijpers P. Effectiveness of an online group course for depression in adolescents and young adults: a randomized trial. J. Med. Internet Res. 2012;14(3) doi: 10.2196/jmir.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]