Abstract
Sleep disturbance is common among young people, with consequences for academic, emotional and behavioural development. Cognitive-behavioural therapy for insomnia (CBT-I) is efficacious, yet it is costly and not available to many who need it. Digitally-delivered CBT-I (eCBT-I) has the potential to overcome these barriers. The purpose of this systematic review was to identify studies which report on the efficacy or effectiveness of eCBT-I for young people with sleep disturbance. Electronic databases were systematically searched and three studies met inclusion criteria. Two studies used the same online intervention for adolescents with insomnia symptoms, while the other was conducted in a college sample of individuals who opted into a stress-management study. Results showed that eCBT-I improved sleep efficiency, sleep quality, sleep-onset latency and total sleep time with effect sizes ranging from 0.17–1.30 (Cohen's d). This suggests that eCBT-I is a promising intervention for young people, but more studies are needed to verify the conditions under which it is most effective.
Abbreviations: BDI-II, Beck Depression Inventory-II; CBT-I, Cognitive-behavioural therapy for insomnia; eCBT-I, digitally-delivered CBT-I; PSQI, Pittsburgh Sleep Quality Index; SE, sleep efficiency; SOL, sleep onset latency; SQ, sleep quality; STAI-S, State-Trait Anxiety Inventory State Version; TIB, time in bed; TST, total sleep time; WASO, wake after sleep onset
Keywords: Insomnia, Sleep disturbance, Adolescence, Cognitive-behavioural therapy
Highlights
-
•
Digitally-delivered youth-focused interventions for sleep disturbance were reviewed.
-
•
There were moderate to large effect sizes for most sleep outcomes (d = 0.17–1.30).
-
•
Digital interventions for youth sleep disturbance are a promising treatment option.
-
•
The available research was limited and more studies in the area are needed.
1. Introduction
Adolescence is a time of major developmental and social change. As children transition into adolescence, many develop sleep problems, with approximately 30% of adolescents reporting at least some level of sleep difficulty (Ohayon et al., 2000). At the clinical end of the spectrum, insomnia is the most common sleep disorder among adolescents, with prevalence rates of approximately 4% (Ohayon et al., 2000). Both subclinical levels of sleep disturbance and insomnia are associated with a range of negative outcomes that are particularly problematic during adolescence, including poorer academic performance (Dewald et al., 2010), problems with interpersonal relationships (Roberts et al., 2001), increased risky behaviour (Shochat et al., 2014), depression (Baglioni et al., 2011; Ford and Kamerow, 1989; Franzen and Buysse, 2008; Harvey, 2001; Riemann and Voderholzer, 2003; Taylor et al., 2003) and suicide (Roane and Taylor, 2008). These educational, behavioural and emotional disturbances caused by sleep problems and insomnia during adolescence can seriously derail psychological, social and vocational pathways into adulthood.
The most common treatment for insomnia is medication. Typically, hypnotics such as benzodiazepine receptor agonists are prescribed, with efficacy supporting their use in both adults and young people (Holbrook et al., 2000; Reed & Findling, 2002). However, as with many pharmacological approaches, benzodiazepines are associated with side effects, dependence and tolerance over time. Moreover, these drugs are not curative which means once treatment is discontinued, the problems re-emerge. An alternative is cognitive-behavioural therapy for insomnia (CBT-I), which is a psychological approach that has comparable efficacy to hypnotics in the short-term, but has longer lasting effects such that benefits are maintained even after the active phase of this brief treatment is discontinued (Mitchell et al., 2012; Riemann and Perlis, 2009; Smith et al., 2002). Clinical guidelines now recommend CBT-I as first line treatment for insomnia (Qaseem et al., 2016). CBT-I involves a combination of strategies that include psychoeducation, sleep restriction, stimulus control, cognitive therapy, and sleep hygiene, and is typically delivered over the course of approximately eight weeks (Sharma and Andrade, 2012). A major challenge in delivering CBT-I at scale are limits to the availability of trained sleep therapists and the high cost of receiving face-to-face treatment (Gulliver et al., 2010; Manber et al., 2012). To this end, there has been great interest in the possibility of delivering CBT-I digitally (via the internet, tablets or smartphones) as a way to overcome the barriers of reach and cost (Griffiths et al., 2006).
Research into the effectiveness of digitally delivered CBT-I (eCBT-I) has established it is effective for the treatment of adult insomnia, with improvements across a range of sleep indices including sleep efficiency (SE), sleep quality (SQ), wake after sleep onset (WASO), sleep onset latency (SOL), total sleep time (TST) and number of night-time awakenings (NWAK; Zachariae et al., 2016). Several studies have compared internet-delivered CBT-I to face-to-face treatments, with some reporting superiority for face-to-face formats (Lancee et al., 2012), while others report no difference (Blom et al., 2016). A recent meta-analysis that drew from eight studies established that effect sizes for eCBT-I are in the small to large range (g = 0.21–1.09), and comparable to face-to-face delivered CBT-I (Zachariae et al., 2016). This approach therefore shows great promise in overcoming some of the barriers associated with the accessibility and use of CBT-I for the treatment of insomnia. Encouragingly, there are now a number of eCBT-I programs commercially available for use by adults (e.g., Sleepio, SHUTi; Christensen et al., 2016; Espie et al., 2012).
While considerable work has been done examining eCBT-I for adults, there is less research into the use of eCBT-I for adolescents. As suggested by the adult literature, there is a great opportunity to potentially prevent a lifelong trajectory of chronic insomnia and associated issues if interventions are made accessible early in the course of illness, before chronic sleep problems emerge. Moreover, young people may be particularly well suited to digital programs because they are generally reluctant to seek professional help (Gulliver et al., 2010), are more comfortable with technology than any previous generation (Younes et al., 2015) and may therefore be more likely to engage with digitally-delivered programs. The data supports this suggestion, with 97% of adolescent individuals with insomnia, when given the choice between internet-delivered and face-to-face group CBT-I, opting for the internet version (de Bruin et al., 2015).
1.1. Aims of study
The state of the literature and evidence supporting the use of eCBT-I to treat sleep problems among young people is unclear. Therefore, the aim of this systematic review was to identify and evaluate studies testing the efficacy and effectiveness of eCBT-I delivered to young people. A description of the available interventions will be provided and a summary of intervention effects will be reported. Given that this is a relatively new area of enquiry, we were interested in studies that reported on both pilot data using pre-post designs, as well as non-randomised controlled trials and randomised controlled trials (RCTs).
Conducting a review of this type will both determine the effectiveness of these interventions in reducing sleep problems and insomnia, and will identify gaps where further research is warranted and required.
2. Methods
The study was conducted in accordance with PRISMA recommendations (Moher et al., 2010) and was registered with PROSPERO [CRD42017054972].
2.1. Search strategy
A search was conducted in Embase, Medline and PsycINFO databases for articles published between 1st January 1991 and 31st December 2016. The start date was selected to coincide with the year the World Wide Web was introduced. The following search terms were used to represent the constructs of (i) technology; ii) intervention; iii) youth; iv) sleep; v) trial methodolgy: app OR computer* OR cyber OR cyberspace OR electronic OR electronic mail OR email OR e-mail OR internet* OR net OR online OR virtual OR web OR e-health OR ehealth OR web OR m-health OR mhealth OR mobile* OR smartphone OR text message OR SMS OR social media OR blog OR forum OR Twitter OR Facebook OR Instagram AND screen* OR assess* OR interven* OR * prevent* or treat* OR track* OR *support OR therapy OR CBT OR self-help AND adolescen* OR child* OR youth OR young person OR young adult OR young people OR emerging adult OR teen* OR school-aged OR student AND Sleep OR insomnia AND Trial OR RCT OR randomised control trial OR randomized controlled trial or randomized control trial OR randomised controlled trial. Two reviewers (AWS, LJ) independently searched all databases. A separate electronic search (using the same terms) was also conducted for the journal Internet Interventions, as it is not currently listed in these databases. In addition, reference lists from included studies and previous literature reviews in this field were hand-searched.
2.2. Eligibility criteria
Peer-reviewed journal articles published in English were eligible for the current study. Eligibility was assessed using the PICOS guidelines found in the PRISMA statement (Moher et al., 2010). Participants: To capture the full spectrum of youth, participants with a mean age of between 12 years, 0 months and 24 years, 0 months were included. Interventions: Interventions were required to: i) directly target insomnia or symptoms of insomnia (interventions were permitted to target additional concerns such as anxiety as long as the insomnia-focused component constituted at least 75% of the intervention); ii) incorporate at least two core elements of CBT-I (i.e. sleep restriction, stimulus-control, cognitive therapy, sleep hygiene education and relaxation); iii) be delivered via a web-based or mobile phone application. For multi-modal interventions that delivered component(s) non-digitally (e.g. face-to-face or paper-based), the digital component was required to constitute at least 75% of the program's delivery method. Comparisons: No restriction was imposed on the type or use of control groups. However, for trials that compared an eCBT-I group to a non-intervention control group, between-group effect sizes are reported. Outcomes: Studies were required to report baseline and post-intervention means and SD/SE data for the intervention group. This data was required on at least one primary sleep-related outcome, which could be insomnia severity, SE, WASO, SOL, TST, NA, time in bed (TIB) or subjective sleep quality. Sleep outcomes could be reported using subjective or objective (e.g., polysomnography) approaches. Assessment measures needed to be standardised, validated and reliable instruments or scales suitable for adolescents. Secondary outcomes were related to mental health and general functioning, and measured depressive symptoms, anxiety symptoms, psychological distress, level of functioning and quality of life; however these were not required for study inclusion. Reporting on follow up data was not required for inclusion in the current review. However all available follow-up data was extracted. Study design: Eligible studies included pre-post designs, non-randomised controlled trials and RCTs, including clustered RCTs. Studies were excluded if: participants did not meet the age criterion; the intervention did not target insomnia, incorporate CBT-I components or was not delivered digitally; or; the study did not report sleep-related outcomes.
2.3. Effect size estimates
To evaluate the effect of eCBT-I, effect size estimates (Cohen's d; Cohen, 1992) were extracted from controlled studies that included a non-intervention control group.
2.4. Study selection and data extraction
Two reviewers (AWS, LJ) independently conducted the searches and removed duplicates. Titles and abstracts were then screened by both reviewers and irrelevant articles were removed. These lists were compared and discrepancies were resolved through discussion. Full-texts were then obtained for remaining studies and both reviewers independently assessed whether they met inclusion criteria. Discrepancies were resolved through discussion in consultation with the final author (HC). One reviewer (AWS) extracted all relevant data for included studies into an Excel spreadsheet. Data outlining study design, aims, sample, intervention, outcome measures, outcomes including means and standard deviations on relevant measures, key findings, limitations and conclusions were deemed relevant. A second reviewer (LJ) checked the data extraction was correct.
2.5. Risk of bias in individual studies
Risk of bias was assessed in RCT studies using the Cochrane Collaboration's tool (Higgins et al., 2011). The following seven domains were assessed: i) random sequence generation; ii) allocation concealment; iii) blinding of participants and researchers; iv) blinding of outcome assessments; v) completeness of outcome data; vi) selective reporting; and vii) any other potential sources of bias identified by reviewers. Any disagreements were resolved through discussion. Each study was reported as having low, high or unclear risk of bias for each criterion, rather than a summed total score, which complies with Cochrane recommendations for the use of this tool (Higgins et al., 2011). For non-RCT studies, the Integrated Quality Criteria for the Review of Mulitple Study Designs (ICROMS; Zingg et al., 2016) tool was used, which is better suited to a range of study designs including pre-post and non-randomised and controlled studies (Zingg et al., 2016). This tool requires reports fulfilling, not fulfilling or unknown on each of the domains relevant to each study. A total ICROMS score and overall rating of low, medium or high quality was reported.
3. Results
3.1. Search results
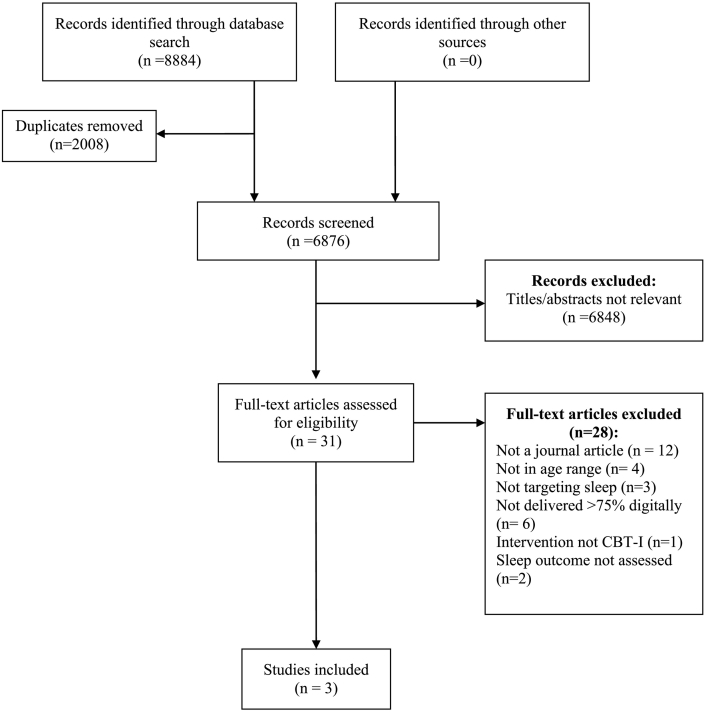
Search results are presented in the PRISMA Flow Diagram (Fig. 1). The database search returned 8884 records. No additional articles were obtained through hand searching recent reviews, or via the search in the Internet Interventions journal. Duplicate records (n = 2008) were removed and the remaining titles and abstracts (n = 6876) were screened. After removing completely irrelevant articles (n = 6848), 31 studies were retained and their full-texts were retrieved and assessed. There were two discrepancies between reviewers, which were resolved through discussion. Three studies met inclusion criteria for this review and were retained for data extraction (see Table 1).
Fig. 1.
PRISMA Flow Diagram.
Table 1.
Characteristics of included studies.
| Authors | Year | N | Allocation (N) |
Age | Control group | Sessions | Sleep outcomes | Follow-up | |
|---|---|---|---|---|---|---|---|---|---|
| eCBT-I | Ctrl | ||||||||
| de Bruin, Oort, Bogles, & Meijer | 2014 | 26 | 13 | N/A | 13–19 years | N/A | 6 | SE, SOL, WASO, TST, TIB, insomnia symptoms, chronic sleep reduction | 2 months |
| de Bruin, Bogels, Oort, & Meijer | 2015 | 78 | 39 | 39 | 12–19 years | WLC | 6 | SE, SOL, WASO, TST, TIB, SQ | 2 months |
| Morris et al. | 2015 | 95 | 48 | 47 | 18–34 years | WLC | 7 | SQ | None |
Note. Randomised controlled trials of digitally-delivered cognitive-behavioural therapy for insomnia. eCBT-I = digitally-delivered cognitive-behavioural therapy for insomnia, Ctrl = control, WLC = waitlist control, SE = sleep efficiency, SOL = sleep onset latency, WASO = wake after sleep onset, TST = total sleep time, TIB = total time in bed, SQ = sleep quality.
3.2. Studies meeting inclusion criteria
The first study that met inclusion criteria was a trial for adolescents with insomnia comparing the effects of an online CBT-I program with a face-to-face group CBT-I program (de Bruin et al., 2014). The second study was conducted by the same research group and was a larger, randomised trial which included both the online and face-to-face groups, as well as a waitlist control group (de Bruin et al., 2015). The final study was a universal program made available to university students which compared the effects of a commercially available online CBT-I program ‘Insomnia Relief’ to a waitlist control group (Morris et al., 2016). In this third study, an additional online anxiety program condition was included. However, this three-arm study compared the two active interventions to the waitlist control and so only the insomnia and control conditions were of relevance to this review.
3.2.1. Population and sample
The first two studies were treatment trials conducted in Amsterdam, The Netherlands. For the first smaller study, participants were aged between 13 and19 with (MCBT-I = 14.3 years; MFace-to-face = 14.9 years) and reported experiencing insomnia symptoms for at least three days a week for at least four weeks (de Bruin et al., 2014). Twenty-one participants were recruited through local advertisements and healthcare professionals. Participants in the second, larger study were aged between 12 and19 (M = 15.6 years) and were diagnosed as having insomnia according to Diagnostic and Statistical Manual of Mental Disorders-IV criteria, as verified by the research team (de Bruin et al., 2015). One hundred and sixteen participants were recruited through local area advertisements in the community and via health care professionals. The third included study was a universal program offered to a sample of 138 students aged 18–34 years (M = 20.5 years) who self-selected into the study by responding to advertisements for a stress management study placed around the University of Bristol campus and disseminated via the university channels (Morris et al., 2016). No clinical assessment was conducted prior to study entry.
3.2.2. Intervention content and sessions
The two studies conducted by the de Bruin group delivered the same eCBT-I intervention. Both this intervention, and the eCBT-I intervention delivered in the Morris study included psychoeducation, sleep hygiene, sleep restriction, stimulus control, and relaxation. The de Bruin studies also included a cognitive therapy component, while the Morris study included an imagery and progressive muscle relaxation component. The interventions tested in all three studies were delivered using an online system over six weeks. The de Bruin studies used an intervention that was adapted for these trials from an adult intervention, whereby participants had to login to their online portal at a specific time each week in order to complete each of their six weekly ‘consultations’ which included treatment information, exercises, and other personalised feedback from a therapist (e.g., bedtime advice). Conversely, the Morris intervention was fully automated and included seven modules, with participants able to login and use the program flexibly, with weekly text message reminders and emails to complete the relevant module. The intervention used in the Morris study is a commercially available program - “Insomnia Relief”, which is retailed in the UK.
3.2.3. Level of support
In the two de Bruin studies, participants were allocated a sleep therapist with whom they had a 15-minute discussion following their second session, as well as receiving continued feedback from their therapist during the online weekly consult. In the 2015 study, parents of participants were also provided a booklet about the program and encouraged to support their child as they completed the eCBT-I program. The level of support was lower in the Morris study, with participants receiving standardised text messages and emails that were manually sent each week to provide encouragement and to remind participants to complete the modules.
3.2.4. Program completion rates
All three studies reported on program completion rates. In the de Bruin 2014 study, 11 of the 13 CBT-I group participants completed all modules, while the remaining two participants completed four of the six modules. In the de Bruin 2015 study, all but one participant accessed all six sessions, with the final participant accessing four of the six. In the Morris study, completion data was not reported as a function of group but instead was presented collapsed across groups. Therefore, it is not possible to identify the rates of attrition in the CBT-I group. However, collapsed across both the insomnia and other active condition (anxiety), 5.1% of participants withdrew from the study, and 5.8% did not meet the study criteria of engaging with the online material for at least 20 min each week.
3.2.5. Group allocation
All three studies compared an eCBT-I intervention to a comparison condition. The first study used a non-random allocation schedule where the first seven participants were allocated to the eCBT-I condition, and the remaining 20 participants were randomly allocated to either the eCBT-I condition or to the comparison condition (de Bruin et al., 2014). The two other studies used a fully randomised allocation schedule (de Bruin et al., 2015; Morris et al., 2016).
3.2.6. Evaluation control group
The de Bruin 2014 study did not include a non-intervention control group, but instead compared the eCBT-I condition to a CBT-I program delivered face-to-face in small groups. As this did not serve as a control condition, this study was treated as an uncontrolled pre-post study and the results from the eCBT-I group only are considered. The remaining two studies both included a non-active, waitlist control group with which to compare eCBT-I. The de Bruin 2015 study included an additional group face-to-face CBT-I condition, which although did not serve as a control group, nonetheless provided a comparison upon which to compare the relative effect of eCBT-I against the same intervention delivered via a different format.
3.2.7. Outcome measures
The de Bruin studies employed an objective measure of sleep outcomes (actigraphy), as well as self-reported sleep logs. The outcome measures were recorded via both objective and subjective methods were common sleep indices: SE, SOL, WASO, TST and TIB. SQ was also ascertained using the self-report sleep log. All outcomes in these studies related to sleep. In the Morris study, a standardised questionnaire was used to assess the primary outcome: sleep quality as measured by the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). Anxiety and depression provided secondary outcomes as measured using the State-Trait Anxiety Inventory State Version (STAI-S; Spielberger et al., 1983) and the Beck Depression Inventory-II (BDI-II; Beck et al., 1996).
3.2.8. Follow-up
In both de Bruin studies, participants completed a two-month follow-up assessment to indicate whether the effects of the intervention were maintained over time. The Morris study did not include a follow-up beyond the end of the intervention period.
3.2.9. Intervention effects
Results from the de Bruin 2014 study showed significant improvements from baseline to post-intervention on both objective and subjective measures. For actigraphy outcomes, improvements were detected for SE, WASO and SOL. For self-reported outcomes, SE and WASO improved, while there was a reduction in SOL and TIB. Results from the de Bruin 2015 and Morris studies demonstrated significant effects of the eCBT-I program compared to the waitlist control condition on primary sleep outcomes at post-intervention. Effects ranged from small to large and included both objective and subjective measures on sleep outcomes (d = 0.17–1.30). In the de Bruin study, SE, SOL, and TST as measured by actigraphy revealed significant small to large effect sizes (d = 0.30–1.09), with the strongest effect size detected for SE (d = 1.09). Effects of improved SE and reduced SOL were maintained at the two-month follow-up (d = 1.10–1.30). Although results were in the expected direction, neither WASO nor TIB reached statistical significance as measured by actigraphy at either time point (d = 0.11–0.29). The pattern of results was largely replicated for self-reported sleep diary data. SE and SOL demonstrated significant effects of the intervention at post-intervention relative to the control group (d = 0.56–0.82), which were maintained at follow-up (d = 0.52–0.77). Again, the strongest effect was for SE (d = 0.56). SQ, which was measured only using self-report methods demonstrated a significant effect at both post and follow-up (d = 0.41–0.56). Although effects were in the direction of improvement, WASO, TIB and TST did not reach statistical significance at either of the time points (d = 0.17–0.61). Although beyond the scope of this review, there were no statistical differences between the effects of the eCBT-I program relative to the group-based CBT-I program at post-test or follow-up (de Bruin et al., 2015).
Results from the Morris study demonstrated a medium effect size for self-reported SQ as measured on the PSQI (d = 0.51). Secondary outcomes of depression and anxiety did not show significant post-treatment effects (d = 0.49–0.51).
Together, effect size estimates provided by the two studies which employed a control condition suggest that there are small to large effects associated with eCBT-I compared to a waitlist control condition, on a range of objectively and subjectively measured sleep outcomes including SE, SOL, TST, and SQ.
3.2.10. Risk of bias
The methodological quality of the three reported studies varied significantly (see Table 2, Table 3). For the pilot study, which was treated as a non-controlled pre-post-study, risk of bias was low except in the case of the lack of control group. The authors did not provide a rationale for the lack of a control group, although they did note that they were conducting a feasibility and efficacy study which for these purposes did not require a control group. Accordingly, they did not show attempts to mitigate the effect of this lack of control group. All other areas of the study methodology were free from bias. Overall, the study was assessed as medium quality using the ICROMS tool.
Table 2.
Quality assessment of non-RCTs.
| Study design | Clear statement of aims | Rationale for intervention points or adequate baseline measurement | Explanation for lack of control group | Justification for sample choice | Blinded assessment of primary outcome measures | Reliable primary outcome measures | Incomplete outcome data addressed | Intervention unlikely to affect data collection | Attempts to mitigate effects of no control | Analysis sufficiently rigorous | Free of selective outcome reporting | Limitations addressed | Conclusions clear and justified | Free of other bias | Ethics issues addressed | Final ICROMS score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| de Bruin et al. (2014) | NCBA | + | + | − | + | + | + | + | + | − | + | + | + | + | + | + | 13 |
Note. NCBA = non-controlled before-after; quality ratings: + = yes, − = no,? = unknown; final ICROMS score: low quality = 0–12 points, medium quality = 13–17 points, high quality = 18–26 points.
Table 3.
Quality assessment of RCTs.
| Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other forms of bias | |
|---|---|---|---|---|---|---|---|
| de Bruin et al. (2015) | + | + | – | + | + | + | + |
| Morris et al. (2016) | + | + | – | ? | – | ? | + |
Note. + = low risk (included information protecting against bias), − = high risk (did not protect against source of bias), ? = unclear risk of bias.
For the two RCTs, there was no evidence of selection bias in either trial, with both studies reporting the use of a random number table to inform the randomisation sequence. Allocation of participants to condition was appropriately concealed such that allocations could not have been foreseen prior to or during enrolment. As is the case in psychological studies, there is always a high risk of performance bias because participants are informed of the intervention they have been allocated in advance of receiving treatment. Detection bias was not possible in the de Bruin study because all outcome measures were collected automatically via an online portal so no bias could be introduced by non-blind personnel collecting outcome data. However, the risk of detection bias was unclear in the Morris study because insufficient detail was provided to make an assessment about the nature of how the outcome assessments were conducted (e.g., online or face-to-face). There was low risk of attrition bias in the de Bruin study with comparable levels of missing data across conditions. However, in the Morris study, attrition risk was high because the authors failed to provide attrition data for each group and did not provide reasons for drop-out. Moreover, a completer analysis was conducted rather than an intent-to-treat analysis, which introduced possible bias. There was low risk of selective reporting in the de Bruin study, which had registered the trial and published a protocol outlining all outcomes in advance of conducting the trial. The risk of reporting bias was unclear in the Morris study because the authors did not provide enough information to assess whether all outcomes were reported. There was no evidence of additional bias in either study.
4. Discussion
The aim of this study was to review studies testing the effect of eCBT-I interventions delivered to young people for sleep problems which could range from mild levels of disturbance to clinical insomnia. Unlike the adult literature for which a substantial body of work exists (Seyffert et al., 2016; Zachariae et al., 2016), we identified only three studies (one small pilot study and two RCTs) evaluating eCBT-I in young people. The results from these studies were promising, with improvements in sleep outcomes from baseline to post-intervention in all three studies, and with medium to large effect sizes for sleep outcomes in the two controlled studies, relative to a waitlist control group.
The studies included in this review were relatively heterogeneous: the pilot study was a precursor to the treatment trial conducted in an adolescent sample (de Bruin et al., 2014, de Bruin et al., 2015), while the other was a broader intervention that was implemented in a self-selecting college sample that did not require a clinical diagnosis or specified symptom level to receive the program. While the paucity of studies and the heterogeneous nature of the included studies makes it difficult to draw strong conclusions about the overall effectiveness of eCBT-I, this review nonetheless suggests that there are positive outcomes across different kinds of studies (pre-post; RCTs), employing different interventions (study specific, freely available), and using diverse participant samples (adolescent, young adult; non-clinical, clinical). Moreover, while the two de Bruin studies established efficacy for eCBT-I among those who self-report insomnia symptoms or receive a clinical diagnosis, the fact that in the Morris study, participants self-selected into a stress management course and were not required to be experiencing sleep difficulties, indicates there are improvements in sleep among nonclinical and non-treatment seeking samples. The implication that follows is that eCBT-I could be beneficial as a preventive intervention, potentially averting the development of significant sleep problems among young people experiencing stress. This possibility should be tested by conducting randomised controlled trials which monitor participants over time to elucidate any preventive benefit of eCBT-I.
The current review identified programs that varied in level of support available – one was a fully automated program (Morris et al., 2016) and the other was a therapist-supported online program (de Bruin et al., 2014, de Bruin et al., 2015). The positive effects from the study with automated support, in particular, is promising because therapist support and engagement is more costly and may deter some young people from utilising these programs, particularly if they are concerned about remaining anonymous. That said, the broader literature on internet interventions has found that programs with therapist guidance are often associated with better outcomes than fully-automated treatments (Palmqvist et al., 2007; Spek et al., 2007). Therefore, future work will need to systematically address this issue by directly comparing therapist-supported and automated versions of the same intervention.
In the current review, we evaluated the two RCTs in terms of the relative effectiveness of eCBT-I compared to a waitlist control group. Although there were large effect sizes for eCBT-I when compared to an inactive waitlist control group, future studies should include attention-matched control conditions such that they are able to account for non-specific therapeutic factors such as time spent engaged in an online program and therapist contact. Related to this issue is the effect of eCBT-I compared to more traditional face-to-face approaches. Of note was that both the de Bruin studies included a face-to-face group CBT-I condition, and in the larger trial study, no differences between this and the eCBT-I condition were found (de Bruin et al., 2015). However, there was some evidence of superiority for the face-to-face format in the pilot study (de Bruin et al., 2014), and some studies from the adult literature have reported larger effect sizes for individual face-to-face therapy (e.g., Lancee et al., 2016). Given the mixed findings, more research is required to address this issue definitively.
Perhaps a surprising finding from the Morris study was that there was no effect of the intervention on depression or anxiety. This contradicts the general finding in the literature that depression may be improved indirectly by targeting sleep problems (Clarke and Harvey, 2012). Notably though, the participants in the Morris study did not reach clinical criteria for depression or anxiety, falling below the accepted clinical cut-offs on both the depression and anxiety scales at baseline (Beck et al., 1996; Spielberger et al., 1983). Therefore, it might be the case that secondary effects on mental health symptoms are only evident when participants are in the clinical range to begin with. This hypothesis requires further empirical testing, and the inclusion of mental health outcomes in future studies would identify the conditions under which sleep interventions may improve depression and/or anxiety.
The findings from the studies reviewed in this article underscore the potential value of using digital approaches to target sleep problems in young people. Large population-based surveys now show that up to 99.7% of young people access the internet regularly, with the vast majority of those (92%) reporting daily use (Hoare et al., 2017; Lenhart et al., 2015). This pervasive use of technology provides an opportunity to deliver digital interventions to young people who otherwise may not seek help. Young people are generally reluctant to seek help for mental health problems for a range of reasons, but these often include stigma and a preference for self-reliance (Gulliver et al., 2010; Rickwood et al., 2007). These two issues may be overcome by eCBT-I interventions because first, stigma associated with face-to-face help-seeking may be protected by the anonymity offered by receiving interventions digitally. Second, the preference for self-reliance is exemplified by the fact that young people are increasingly using the internet to access information and services about mental health (Horgan and Sweeney, 2010). This assertion is also supported by empirical data from one of the studies included in this review whereby adolescents who were originally assigned to the waitlist control group were given the option to receive either internet-delivered or face-to-face group CBT-I after the trial had finished. Participants overwhelmingly (97%) opted to receive the eCBT-I program, suggesting that this format may be more appealing to adolescents (de Bruin et al., 2015).
The scarcity of relevant literature to review is a key limitation of the current paper, which prevents strong conclusions being made about the effect of eCBT-I delivered to young people. However, this lack of literature simultaneously highlights the importance of continued work in this field, based on the promising findings both from this review and the adult literature, and the seemingly appropriate fit between digitally-delivered programs and young people's preferences. Questions arising from the current study that require further investigation include the investigation of: the differential effect of eCBT-I in treatment-seeking clinical groups as compared to sub-clinical and non-treatment seeking groups; the potential for eCBT-I to prevent the development of more severe insomnia symptoms by employing controlled designs with follow-up; the impact of therapist support in youth samples, the relative effectiveness of different formats of CBT-I, and whether there are secondary effects on broader mental health symptoms that go beyond sleep outcomes.
The last ten years has seen increased interest in using eCBT-I to target sleep problems in adults. Studies are now beginning to address younger age groups and this review draws attention to the promise of such approaches, while simultaneously highlighting the need for further research.
Role of funding sources
Funding for this study was provided by the Black Dog Institute, in the form of a National Health and Medical Research Council (NHMRC) John Cade Fellowship (APP1056964) awarded to Professor Helen Christensen. The NHMRC had no role in the study design, collection, data analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Contributors
Dr. Werner-Seidler designed the study in consultation with Ms. Johnson and Professor Christensen. Dr. Werner-Seidler and Ms. Johnson performed the database search and screened articles for eligibility. Professor Christensen was consulted in instances of disagreement. Dr. Werner-Seidler conducted data extraction, which was checked by Ms. Johnson. All authors contributed to the final manuscript.
Conflict of interest
We declare no conflict of interest with respect to this submission or publication of this manuscript.
Contributor Information
Aliza Werner-Seidler, Email: a.wernerseidler@blackdog.org.
Lara Johnston, Email: l.johnston@blackdog.org.au.
References
- Baglioni C., Battagliese G., Feige B., Spiegelhalder K., Nissen C., Voderholzer U., Lombardo C., Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; San Antonio, TX: 1996. Manual for the Beck Depression Inventory—II. [Google Scholar]
- Blom K., Jernelov S., Lindefors N., Kaldo V. Internet Interventions, Part 1. Vol. 4. 2016. Facilitating and hindering factors in internet-delivered treatment for insomnia and depression; pp. 51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin E.J., Oort F.J., Bogels S.M., Meijer A.M. Efficacy of internet and group-administered cognitive behavioral therapy for insomnia in adolescents: a pilot study. Behav. Sleep Med. 2014;12:235–254. doi: 10.1080/15402002.2013.784703. [DOI] [PubMed] [Google Scholar]
- de Bruin E.J., Bogels S.M., Oort F.J., Meijer A.M. Efficacy of cognitive behavioral therapy for insomnia in adolescents: a randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep. 2015;38:1913–1926. doi: 10.5665/sleep.5240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Christensen H., Batterham P.J., Gosling J.A., Ritterband L.M., Griffiths K.M., Thorndike F.P., Glozier N., O'Dea B., Hickie I.B., Mackinnon A.J. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry. 2016;3:333–341. doi: 10.1016/S2215-0366(15)00536-2. [DOI] [PubMed] [Google Scholar]
- Clarke G., Harvey A.G. The complex role of sleep in adolescent depression. Child Adolesc. Psychiatr. Clin. N. Am. 2012;21:385–400. doi: 10.1016/j.chc.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Quantitative methods in psychology: a power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Dewald J.F., Meijer A.M., Oort F.J., Kerkhof G.A., Bögels S.M. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med. Rev. 2010;14:179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- Espie C.A., Kyle S.D., Williams C., Ong J.C., Douglas N.J., Hames P., Brown J.S. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35:769–781. doi: 10.5665/sleep.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford D.E., Kamerow D.B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Franzen P.L., Buysse D.J. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin. Neurosci. 2008;10:473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths F., Lindenmeyer A., Powell J., Lowe P., Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J. Med. Internet Res. 2006;8 doi: 10.2196/jmir.8.2.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A., Griffiths K.M., Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey A.G. Insomnia: symtpom or diagnosis? Clin. Psychol. Rev. 2001;21:1037–1059. doi: 10.1016/s0272-7358(00)00083-0. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savović J., Schulz K.F., Weeks L., Sterne J.A.C. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoare E., Milton K., Foster C., Allender S. Depression, psychological distress and internet use among community-based Australian adolescents: a cross-sectional study. BMC Public Health. 2017;17 doi: 10.1186/s12889-017-4272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook A.M., Crowther R., Lotter A., Cheng C., King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. Can. Med. Assoc. J. 2000;162:225–233. [PMC free article] [PubMed] [Google Scholar]
- Horgan Á., Sweeney J. Young students' use of the internet for mental health information and support. J. Psychiatr. Ment. Health Nurs. 2010;17:117–123. doi: 10.1111/j.1365-2850.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- Lancee J., van den Bout J., van Straten A., Spoormaker V.I. Internet-delivered or mailed self-help treatment for insomnia? A randomized waiting-list controlled trial. Behav. Res. Ther. 2012;50:22–29. doi: 10.1016/j.brat.2011.09.012. [DOI] [PubMed] [Google Scholar]
- Lancee J., van Straten A., Morina N., Kaldo V., Kamphuis J.H. Guided online or face-to-face cognitive behavioral treatment for insomnia: a randomized wait-list controlled trial. Sleep. 2016;39:183–191. doi: 10.5665/sleep.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A., Duggan M., Perrin A., Stepler R., Rainie H., Parker K. Pew Research Centre; Washington, DC: 2015. Teens, Social Media and Technology Overview. [Google Scholar]
- Manber R., Carney C., Edinger J., Epstein D., Friedman L., Haynes P.L., Karlin B.E., Pigeon W., Siebern A.T., Trockel M. Dissemination of CBTI to the non-sleep specialist: protocol development and training issues. J. Clin. Sleep Med. 2012;8:209–218. doi: 10.5664/jcsm.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell M.D., Gehrman P., Perlis M., Umscheid C.A. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam. Pract. 2012;13 doi: 10.1186/1471-2296-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int. J. Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Morris J., Firkins A., Millings A., Mohr C., Redford P., Rowe A. Internet-delivered cognitive behavior therapy for anxiety and insomnia in a higher education context. Anxiety Stress Coping. 2016;29:415–431. doi: 10.1080/10615806.2015.1058924. [DOI] [PubMed] [Google Scholar]
- Ohayon M.M., Roberts R.E., Zulley J., Smirne S., Priest R.G. Prevalence and patterns of problematic sleep among older adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 2000;39:1549–1556. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- Palmqvist B., Carlbring P., Andersson G. Internet-delivered treatments with or without therapist input: does the therapist factor have implications for efficacy and cost? Expert Rev. Pharmacoecon. Outcomes Res. 2007;7:291–297. doi: 10.1586/14737167.7.3.291. [DOI] [PubMed] [Google Scholar]
- Qaseem A., Kansagara D., Forciea M., Cooke M., Denberg T.D. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2016;165:125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- Reed M.D., Findling R.L. Overview of current management of sleep disturbances in children: I pharmacotherapy. Curr. Ther. Res. 2002;63:B18–B37. [Google Scholar]
- Rickwood D.J., Deane F.P., Wilson C.J. When and how do young people seek professional help for mental health problems. Med. J. Aust. 2007;187:S35–S39. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- Riemann D., Perlis M.L. The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med. Rev. 2009;13:205–214. doi: 10.1016/j.smrv.2008.06.001. [DOI] [PubMed] [Google Scholar]
- Riemann D., Voderholzer U. Primary insomnia: a risk factor to develop depression? J. Affect. Disord. 2003;76:255–259. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- Roane B.M., Taylor D.J. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–1356. [PMC free article] [PubMed] [Google Scholar]
- Roberts R.E., Roberts C.R., Chen I.G. Functioning of adolescents with symptoms of disturbed sleep. J. Youth Adolesc. 2001;30:1–18. [Google Scholar]
- Seyffert M., Lagisetty P., Landgraf J., Chopra V., Pfeiffer P.N., Conte M.L., Rogers M.A. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0149139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M.P., Andrade C. Behavioral interventions for insomnia: theory and practice. Indian J. Psychiatry. 2012;54:359–366. doi: 10.4103/0019-5545.104825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shochat T., Cohen-Zion M., Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med. Rev. 2014;18:75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Smith M.T., Perlis M.L., Park A., Smith M.S., Pennington J., Giles D.E., Buysse D.J. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am. J. Psychiatr. 2002;159:5–11. doi: 10.1176/appi.ajp.159.1.5. [DOI] [PubMed] [Google Scholar]
- Spek V., Cuijpers P., Nyklicek I., Riper H., Keyzer J., Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol. Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R., Vagg P.R., Jacobs G.A. Consulting Psychologists Press; Palo Alto, CA: 1983. Manual for the State-Trait Anxiety Inventory. [Google Scholar]
- Taylor D.J., Lichstein K.L., Durrence H.H. Insomnia as a health risk factor. Behav. Sleep Med. 2003;1:227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- Younes N., Chollet A., Menard E., Melchior M. E-mental health care among young adults and help-seeking behaviors: a transversal study in a community sample. J. Med. Internet Res. 2015;17 doi: 10.2196/jmir.4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariae R., Lyby M.S., Ritterband L.M., O'Toole M.S. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia - a systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2016;30:1–10. doi: 10.1016/j.smrv.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Zingg W., Castro-Sanchez E., Secci F.V., Edwards R., Drumiright L.N., Sevdalis N., Holmes A.H. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS) Public Health. 2016;133:19–37. doi: 10.1016/j.puhe.2015.10.012. [DOI] [PubMed] [Google Scholar]