Abstract
Background
Passive surveillance of malaria in health facilities remains vital for implementation of control and elimination programs. It is therefore essential understanding current age profile of clinical malaria morbidity, mortality and presentations in areas with variant infection susceptibility. This study aimed at understanding the current malaria morbidity and mortality in Western Kenya.
Methods
Surveillance of clinical and asymptomatic parasitological positivity rates of all malaria suspected patients and school children were respectively determined from June 2015 to August 2016. From 2014 to 2016, register books in hospitals were referred and the confirmed malaria cases in conjunction with total number of monthly outpatient visits (OPD) counted. All registered malaria admissions were counted together with other causes of admissions. Moreover, outcome of malaria admissions in terms of discharge or death was recorded using inpatient charts within the same time frame. Prospective surveillance of severe malaria collected information on clinical features of the disease. Giemsa stained blood slides confirmed existence of malaria parasitemia. Chi-square and analysis of variance tests were used, respectively, to compute proportions and means; then a comparison was made between different age groups, periods, and study areas.
Results
During the survey of asymptomatic infections among school children, overall blood slide positivity ranged from 6.4% at the epidemic prone site to 38.3% at the hyperendemic site. During the clinical malaria survey, school age children (5–14) presented with overall the highest (45%) blood slide positivity rate among those suspected to have the infection at the epidemic prone study site. The survey of all malaria confirmed and registered cases at OPD found 17% to 27% of all consultations among <5 children and 9.9% to 20.7% of all OPD visits among the ≥5 patients were due to malaria. Moreover, survey of all registered causes of admission in hospitals found 47% of admissions were due to malaria. The disease was a major cause of admission in epidemic prone setting where 63.4% of the <5 children and 62.8% of the ≥5 patients were admitted due to malaria (p>0.05) and 40% of all malaria admissions were school age children. Malaria related death rate was highest among <5 years at the hyperendemic site, that is 60.9 death per 1000 malaria <5 admissions. Conversely, the epidemic prone setting experienced highest malaria related death among ≥15 years (18.6 death per 1000 admissions) than the < 15 years (5.7 death per 1000 admissions of the <15 years) (p< 0.001). Surveillance of severe form of the disease found that hyperpyrexia, hyperparastemia, prostration and convulsions as common presentations of severe disease.
Conclusion
Malaria is still the major cause of hospital consultations in Western Kenya with an alarming number of severe forms of the disease among the school aged children at the epidemic prone setting. Mortalities were higher among <5 children years in high infection transmission setting and among ≥15 years in low and moderate transmission settings. Surveillance of asymptomatic and symptomatic malaria along with evaluation of current interventions in different age groups should be implemented in Kenya.
Background
In spite of the ongoing interventions, malaria remains a major public health threat to tropical and subtropical countries with more burden to sub-Saharan Africa. These interventions include case management using Artemisinin Combination Therapy (ACT) drugs and vector control through large-scale distribution of Long-Lasting Impregnated Net (LLINs), and Indoor Residual Spraying (IRS). Africa continues to shoulder the heaviest burden of all malaria cases; it registers 90% of all malaria cases and 92% of mortalities [1]. In malaria endemic areas, before the scaling up of interventions, the disease accounted for 25–35% of all outpatient consultations, 20–45% of hospital admissions, and 15–35% of all hospital deaths [2]. However, admissions due to malaria has been decreasing following the scaled up interventions in many areas of sub-Sahara Africa [3,4]. Elsewhere in Africa, resurgence of malaria infection has resulted in causing more burden among older children and adults due to a long spell of sustained malaria control [5]. However, severity of clinical malaria can be affected by a number of factors including parasite genetics and host immune factors [6–8]. While hyperparastemia, hyperpyrexia and convulsions used to be the common presenting symptoms of the severe disease among children in epidemic prone areas before intensive interventions [9,10], severe malaria anaemia, and pulmonary oedema were commonly reported features in hyperendemic areas [10]. It has been established that the introduction of LLINs has led to decrement of anaemia among children in Kenya, and therefore interventional pressure could also affect clinical disease presentations [11,12].
Currently, some areas in western Kenya are experiencing changing dynamics of malaria transmission despite the increasing use of insecticide treated nets and other interventions [13–15]. Climatic warming, vector population species shift, and insecticide resistance had been linked with this incident [14,16]. It is important to ascertain epidemiological changes associated with upsurge and sustained high malaria transmission in the context of admission age profiles, clinical presentations of severe disease and case fatality rates. Updated data on the contribution of malaria on the outpatient hospital services is also important especially in these areas that show changing risks of infection transmission. This information will provide better planning and implementation opportunities for the National malaria strategic plan to meet the 2030 Global targets. This study therefore aimed at describing the current morbidity and the related case fatality rates of malaria of three areas with different infection transmission intensity in Western Kenya.
Ethical consideration
The study was approved by the Ethical Review board of Kenya Medical Research Institute (SSC protocol No.3005) and got permission from local authorities. An informed consent was sought to human participants before they were involved in the study. The parents signed the assent form on behalf of their school children to allow them participate in the study before their assent.
Materials and methods
Study area
This study was conducted in three areas with different malaria transmission intensities. The areas included Marani (epidemic prone), Iguhu (mesoendemic) and Kombewa (hyperendemic) [17]. These areas experience long and short rainy seasons favouring vector breeding. The long rainy season starts from March to June and the shorter rainy season begins from October to November. Table 1 describes topographical, malaria endemicity and characteristics of surveyed hospitals and schools.
Table 1. Description of the study areas with different malaria transmission intensities in western Kenya.
| Category | Marani | Iguhu | Kombewa | Citation |
|---|---|---|---|---|
| Location | 34048ʹE, 00 35ʹS, | 34045ʹE, 0010ʹN, | 34030ʹE, 0007ʹN, | |
| 1520 -1700m asl in | 1430 -1580m asl | 1150 -1300m asl | ||
| Kisii | in Kakamega | in Kisumu | ||
| Topography | Hills and steep | Hilly area but has | Flat land area with | |
| valleys with fast | wider valleys | slower water | ||
| drainage | drainage | |||
| Malaria | Epidemic prone | Mesoendemic | Hyperendemic | |
| Endemicity | ||||
| Prevalence of | ||||
| asymptomatic | ||||
| parasitemia | 6% | 30% | 50% | [18] |
| among school | ||||
| Children | ||||
| Entomological | 0.4 infective bites | 16.6 infective bites | 31.1 infective bites | [19] |
| inoculation | per person per year | per person per | per person per | |
| rate | year | year | ||
| Major vectors | Anopheles funestus | Anopheles gambiae | Anopheles funestus | [20,21] |
| s.l | s.s followed by | s.l and Anopheles | ||
| Anopheles funestus | arabiensis | |||
| s.l | ||||
| Hospitals | Marani hospital the | Iguhu and Mukumu | Kombewa hospital | |
| Surveyed | level four | are level four | is also the level | |
| (The selected | government own | government and | four government | |
| health facilities | hospital in the | private owned | own hospital in the | |
| serves both | study area with a | facilities | study area with a | |
| outpatient and | catchment | respectively, | catchment | |
| inpatient | population of about | Iguhu | population of about | |
| medical | 19,000 | areas has | 23,000 | |
| services with | population of | |||
| sound malaria | 24,000 residents | |||
| diagnostic) | ||||
| Surveyed | Gesangora, Kiraeni | Ivonda and Iguhu | Akonya, Diemo, | |
| primary | and Nyasaga | Kamonye and | ||
| schools in the | Okode | |||
| study |
Despite the increased intervention scale up since 2006, previous epidemiological studies in these areas show Kombewa has a sustained high malaria transmission. While Marani experienced infection resurgence since 2012, Iguhu showed a positive response to interventions [13]. The major intervention against vectors in western Kenya is the use of long lasting mosquito nets, which are distributed for free through a mass distribution strategy. So far three rounds of free LLINs distribution have been completed. The first LLINs distribution was in 2006, which was followed by the second distribution in 2011, and the latest one was done in October to December 2015. The LLINs ownership has improved from as low as 24.6% and 65.8% in 2007 at Iguhu and Marani respectively to more than 80% in 2015 [13,18]. The coverage of indoor residual spray was as low as 38% between 2005 and 2010 with even lower over the recent years; none of the study sites were sprayed when this study was being done [22].
Surveillance of asymptomatic malaria among school age children
This study describes infection transmission dynamics of the study area using school children [23]. Multiple cross-sectional surveys of asymptomatic malaria infections were done among students from nine (9) primary schools in the study areas. The study involved three schools at Marani, two school from Iguhu and four schools from Kombewa. The selected primary schools represent one-third of all within a radius of ten kilometres around the selected hospitals. These schools have been sentinel sites for more than ten years. Systematic random sampling of pupils per grade using attendance list was done in three different year of study per survey with a separate list of boys and girls. Selection of participants was done from all selected schools every month with inclusion of only those without fever and without history of related complaints. Sampling of students involved grade one to six with monthly alternation while considering equal number selected participants per grade per survey. The sampling frame was adjusted to accommodate 25 boys and 25 girls per class every month at each site. Students with fever and other malaria related symptoms were taken to nearby health facility for further management. Standard finger prick method was done to obtain thin and thick smear and Giemsa stained before microscopy examination. A minimum of 400 study participants per month was sampled from June 2015 to August 2016.
Prospective surveillance of confirmed clinical malaria
Giemsa stained blood slides were used to diagnose existence of parasitemia in patients who visited the health facilities with suspected malaria and whom had to be sent to the laboratory for investigation. This was to confirm the positivity rate of clinical malaria in each site. During the survey, patients who were suspected to have malaria, and who agreed to sign a consent and/or assent (for minors under age of 18) form were included in the study between June 2015 to August 2016. Blood samples were collected by the standard finger-prick method and thick and thin smears were prepared on labelled slides. Blood smear tests were conducted in the hospitals as part of routine clinical practice and confirmed in the KEMRI laboratory in Kisumu. A clinical malaria case was defined as having fever on the day of the visit or 1 to 2 days earlier, parasitaemia, and one other symptoms of malaria [24]. Fever was defined as body temperature of above 37.5֯ C and hyperpyrexia was considered when the temperature was more or equal to 39֯ C. Blood slides collected from health facilities were examined at the Kenya Medical Research Institute (KEMRI) laboratory in Kisumu. Two different technicians examined the blood slides only to determine parasite presence while the third technician examined slides with disagreement. The KEMRI slides that confirmed positive cases were used to determine parasitemia rate. Additionally, all causes of outpatient visits for all age groups were counted (from the outpatient registries) along with specific numbers of diarrhoea and pneumonia cases among patients under five years of age.
Prospective surveillance of admissions due to severe malaria
A prospective data collection of patients with features of severe malaria was done in conveniently selected hospitals. The study included all severely ill malaria patients admitted at Mukumu, Marani, and Kombewa Hospitals from October 2015 to October 2016. Their social demographics, vital signs, and observed clinical malaria complications were recorded using a checklist which captured information on routine patient care and management [25]. Severe anaemia was considered when the haemoglobin level was below 5g/dl. Days spent in hospital, microscopy results (plus parasite density) and admission outcome were also recorded.
Review of all inpatient (IPD) malaria morbidity and mortality
Along with severe malaria surveillance, the monthly data on all causes of admission, age and the outcome (death or discharge) of admissions were also collected as from June 2015 to August 2016 for <5 children, 5–14 years and ≥15 years age groups. Data collection was done in the following hospitals: Kombewa in Kisumu county, Marani in Kisii county and Iguhu and Mukumu in Kakamega county. Iguhu and Mukumu hospitals are located in the same area close to each other (mesoendemic setting) but the former had a better OPD volume whereas the latter had a good IPD volume including all age groups.
Review of number of outpatient (OPD) malaria cases from 2014 to 2016
Number of confirmed cases were collected from the outpatient monthly reports from January 2014 to May 2015 retrospectively and from June 2015 to August 2016. Cases were counted as they were categorized giving monthly total number of <5 children and ≥5 years of age. All causes of OPD consultations were also collected on monthly basis along with malaria cases. Moreover, during the prospective survey, a number of diarrhoea and pneumonia of OPD consultations among <5 children were also collected monthly.
Household surveys of long lasting insecticides treated mosquito nets (LLINs) ownership and use
A total of 941 randomly selected households were surveyed for LLINs ownership and use using a pretested structured questionnaire. Pretesting of the questionnaire was done to the study site nearby villages and thereafter adjustments of the tools had to be effected. The specific number of surveyed village households were 294, 320, and 327 for Marani, Iguhu and Kombewa respectively. The sample size per village based on another similar study done in the same settings [26]. Three sub-locations were selected from each village using systematic random sampling from the local government household registry. About 100 households were sampled per each sub-location. Head of each household were interviewed on availability of the mosquito nets and use to every family member. Bed net ownership rate was measured as the ratio of the number of households with at least one bed net over the total number of households surveyed [27]. This study intended to identify the proportions of individuals who slept under LLINs. As a result, LLINs usage was defined as the percentage of individuals who reported using the mosquito net in the previous night over the total number of interviewees of the specific age category. Coverage was defined as the percentage of individuals potentially covered by LLINs, such that one LLINs for every two people for every household as per the World Health Organization guide [27]. With consent from the head of the household, observation and confirmation of LLINs availability and quality check were done.
Statistical analysis
Proportion of malaria at the OPD was expressed at the ratio of total number of confirmed cases basing on the specified period of time (monthly or yearly) over total number of OPD consultations. Proportion of malaria admissions was computed as a ratio of all confirmed malaria admissions over the total number of admissions on the specified period of time. Clinical and asymptomatic malaria positivity rate were determined as total number people with confirmed parasitemia over total number of people tested. This led to computation of the frequency of socio-demographic characteristics and clinical features of patients admitted with severe malaria. Thus, malaria case fatality rates were computed as the total number of patients admitted and died due to malaria with or without other comorbidity over the total number of malaria admissions over the specified period of time.
The chi-square test was used to computer the differences of outpatient and inpatient proportions of malaria morbidity between the different time periods and between different age groups in different study sites. Other categorical variables were also compared by chi-square test whereas comparison of the different means were done using one way test of ANOVA. Statistical significance was considered when the p-value was less than 0.05. Bar and line graphs were used to present the number of confirmed malaria cases as well as comparison with other causes of inpatient and outpatient morbidity over a period of time per sites.
Results
Surveillance of asymptomatic malaria among school age children
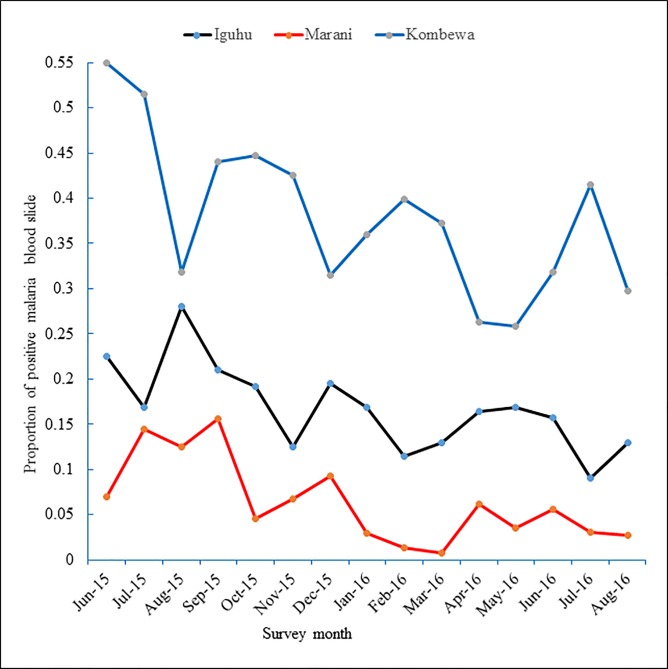
From June 2015 to August 2016, a total of 1972 and 2430 and 1759 blood slides were examined among school children living at Marani, Iguhu, and Kombewa respectively. The overall prevalence of asymptomatic malaria parasitaemia was 6.4%, 16.4% 38.3% for Marani, Iguhu, and Kombewa respectively. In June 2015, the monthly infection positivity ranged from as high as 54.9% at Kombewa while at Marani, in March 2016, the infection was as low as 0.7% (Fig 1). Of all confirmed cases, plasmodium falciparum was the dominant species with 95% followed by Plasmodium malariae (4.5%), and lastly Plasmodium ovale (0.5%).
Fig 1. Dynamics of asymptomatic malaria parasitemia among primary school students in three study sites with different infection transmission intensity in Western Kenya from June 2015 to August 2016.
Prospective surveillance of confirmed clinical malaria
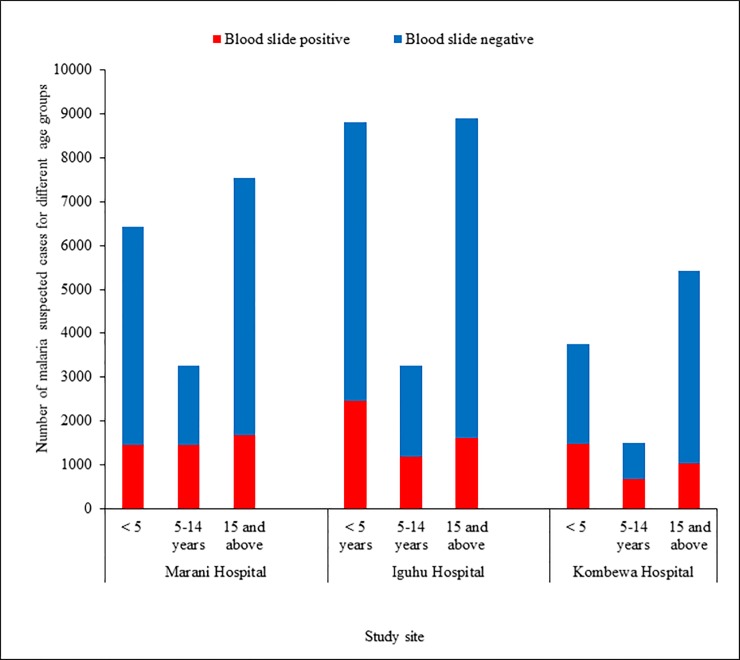
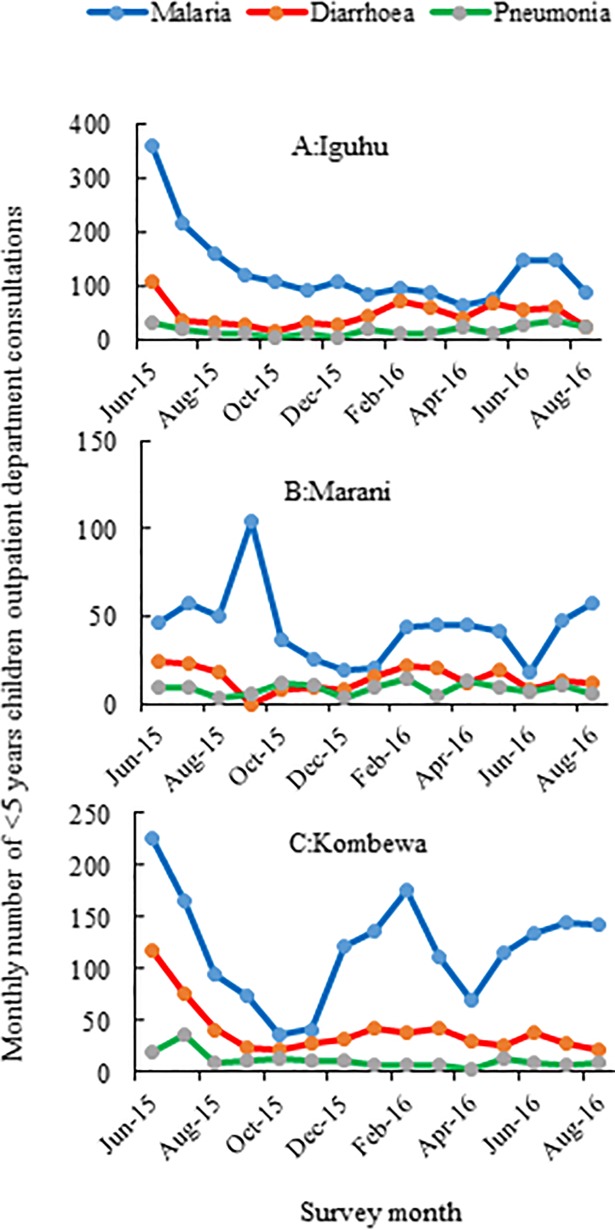
A total of 48,892 malaria suspected patients in the 3 health facilities were screened for malaria parasitaemia. Malaria positivity rates were 26.7% (4599/17231), 24.9% (5244/20985) and 29.9% (3194/10676) at Marani, Iguhu and Kombewa hospitals respectively (χ2 = 87.9, df = 2, p<0.001). The positivity rates were highest among children of 5 to 14 years of age with 44.5% (1453/3267), 45.3% (676/1493) and 36.17% (1182/3267) at Marani, Kombewa and Iguhu hospitals respectively. The positivity rates were consistently lowest among the ≥15 years in all study sites (Fig 2). Along with the laboratory parasitological surveillance, the number of malaria cases and all causes of OPD consultations were collected within the same time frame. At Marani hospital, malaria accounted for 24.06% of all < 5 year OPD consultations whilst 18% among the ≥ 5 years (p<0.001). At Iguhu hospital however, malaria consultations were higher among the ≥ 5 years (20.77%) than the < 5 years children (17.78%) p<0.001). Whereas at Kombewa Hospital, the <5 years children accounted for 27.55% of all outpatient visits as compared to only 9.9% among the ≥5 age group (p<0.001) (Table 2). Moreover, monthly data found that malaria was consistently the leading cause of OPD consultations among the <5 children in all three hospitals followed by diarrhoea and pneumonia (Fig 3).
Fig 2. Total blood slide confirmed malaria cases among suspected patients attending outpatient departments from three hospitals located in different transmission settings of Western Kenya from June 2015 to August 2016.
Table 2. Comparison of under-fives and over-fives proportions of confirmed malaria consultations among all outpatients (OPD) of three hospitals located in three areas with different transmission intensity of western Kenya from June 2015 to August 2016.
| Hospital | Age group | OPD visits of | 95% CI | p-value |
|---|---|---|---|---|
| (years) | Confirmed malaria | (p1–p2) | ||
| Marani | < 5 | 1457/6057 (24.06%) | ||
| ≥5 | 3142/16691 (18.82%) | 0.04–0.06 | <0.001 | |
| Iguhu | <5 | 1979/11129 (17.78%) | ||
| ≥5 | 2666/12835 (20.77%) | 0.02–0.04 | <0.001 | |
| Kombewa | <5 | 1785/6480 (27.55%) | ||
| ≥5 | 1994/20127 (9.9%) | 0.16–0.19 | <0.001 |
p1 = proportion among the <5; p2 = proportion among the ≥5
Fig 3. Monthly cases of confirmed malaria and other common diseases (diarrhoea and pneumonia) among under five children attending outpatient clinics from June 2015 to August 2016 in three hospital of Western Kenya.
Prospective surveillance of admissions due to severe malaria
Clinical presentations of 1244 of severely ill malaria patients varied from site to site. For example, persistent vomiting accounted for 60.7% while prostration registered 60.6%; these were the commonest presentations at the hyperendemic site area, at Kombewa hospital. Similarly, at Marani Hospital hyperparastemia registered 40.4% and signs of prostration had 39.1%; this record emerged common at Marani epidemic prone study site. Severe anaemia malaria at the hyperendemic site was witness to only 14.3% of admissions and as low as 3% in other study areas. The number of severe malaria cases was highest among the ≥15 years old at Mukumu hospital (mesoendemic) with 51.5% and the lowest among the <5 years old with only 17.3%. Moreover, Marani hospital had approximately 70% of all severe malaria admission from the ≥5 years old with equal contribution between the 5 and 14 and ≥15 age groups. Around 63% of all severe malaria admissions at Kombewa were from <5 year old children and was lowest among children aged 5 to 14 years with only 16%. The mean length of hospital stay (days) was the longest at Kombewa (4.59±1.9) and the shortest was at Marani (2.1±2.25) (f179.07, df = 2, p<0.001) (Table 3).
Table 3. Clinical presentations of severe malaria among patients admitted in three hospitals in Western Kenya from August 2015 to October 2016.
| Clinical | Variable | Hospital name | P-value | ||
|---|---|---|---|---|---|
| category | Marani | Mukumu | Kombewa | ||
| (n = 578) | (n = 254) | (n = 412) | |||
| Age group | <5 | 169 (29.2%) | 44 (17.3%) | 259 (62.8%) | |
| 5–14 | 206 (35.6%) | 79 (31.1%) | 65 (15.8%) | ||
| ≥15 | 203 (35.1%) | 131 (51.5%) | 88 (21.4%) | <0.001 | |
| Sex | Female | 304 (52.6%) | 130 (51.2%) | 215 (52.2%) | |
| Male | 274 (47.4%) | 124 (48.8%) | 197 (47.8) | >0.05 | |
| Treatment before | Yes | 254 (43.9%) | 74 (29.1%) | 23 (5.6%) | <0.001 |
| admission | |||||
| Comorbidity | Yes | 53 (9.2%) | 09 (3.6%) | 46 (11.2%) | <0.05 |
| Admission | Mean | 2.1 ± 2.25 | 2.7 ± 1.36 | 4.59 ± 1.90 | <0.001 |
| length (days) | |||||
| Clinical | Hyperpyrexia | 127 (21.9%) | 120 (47.2%) | 118 (28.6%) | <0.001 |
| features | Respiratory | ||||
| Distress | 26 (4.5%) | 41 (16.1%) | 26 (6.3%) | <0.001 | |
| Hypoglycaemia | 1 (0.1%) | 2 (0.78%) | 2 (0.49%) | * | |
| Severe anaemia | 18 (3.1%) | 9 (3.5%) | 58 (14.3%) | <0.001 | |
| Signs of shock | 30 (5.2%) | 27 (10.6%) | 60 (14.1) | <0.001 | |
| Coma | 2 (0.3%) | 5 (1.9%) | 4 (0.9%) | * | |
| Prostration | 226 (39.1%) | 140 (55.1%) | 249 (60.6%) | <0.001 | |
| Convulsions | 52 (8.9%) | 9 (3.5%) | 89 (21.6%) | <0.001 | |
| Persistent | |||||
| Vomiting | 100 (17.3%) | 65 (25.6%) | 251 (60.7%) | <0.001 | |
| Jaundice | 13 (2.2%) | 6 (2.3%) | 3 (0.7%) | >0.05 | |
| Hyperparastemia | 234 (40.4%) | 101 (39.8%) | 127 (30.8%) | <0.05 |
*Not compared because of small number of observations
Review of inpatient malaria morbidities
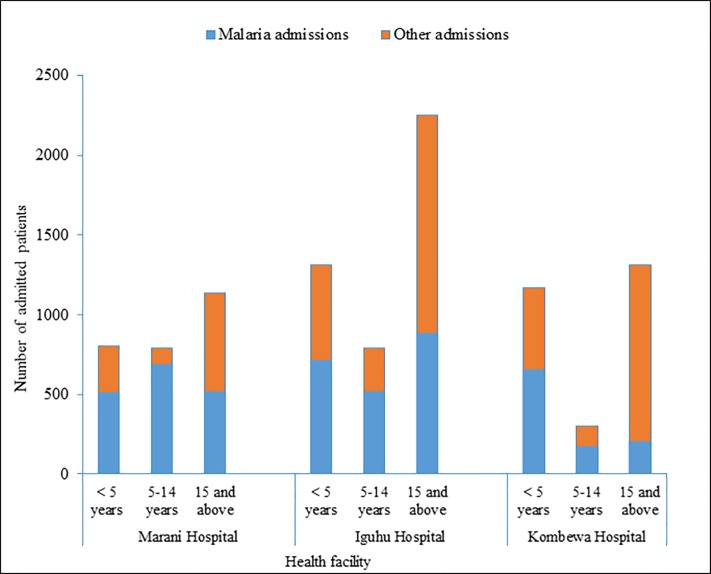
A total of 2732, 4353 and 2782 patients with different causes were admitted at Marani, Mukumu/Iguhu, and Kombewa hospitals respectively. Out of those numbers, malaria admissions accounted for 62.7%, 48.59% and 36.9% at Marani, Iguhu/Mukumu and Kombewa hospitals respectively. Generally, malaria accounted for 47% (4876/10481) of all admissions for all surveyed health facilities. Marani hospital admitted the highest proportion of patients with malaria, accounting for 63.4% of all <5 children admissions and 62.8% of all ≥5 years old inpatients (p>0.05). Malaria constituted 54.62% (721/1320), and 56.15% (657/1170) of all under-fives admissions at Iguhu/Mukumu and Kombewa hospitals respectively (p>0.05). Whereas only 38.52% (1403/3642) and 23.06% (372/1613) of all over-fives admissions were due to malaria at Iguhu/Mukumu and Kombewa hospitals respectively (p<0.001) (Table 4).
Table 4. Contribution of confirmed malaria cases to the inpatient admissions from three hospitals located in different malaria transmission settings of Western Kenya from June 2015 to August 2016.
| Hospital | Age group | Admissions (IPD) of | 95% CI | p-value |
|---|---|---|---|---|
| name | (years) | Confirmed malaria | (p1-p2) | (χ2) |
| Marani | < 5 | 513/809 (63.41%) | ||
| ≥5 | 1210/1927 (62.79%) | -0.03–0.04 | >0.05 | |
| Iguhu and Mukumu |
<5 | 721/1320 (54.62%) | ||
| ≥5 | 1403/3642 (38.52%) | 0.13–0.19 | <0.001 | |
| Kombewa | <5 | 657/1170 (56.15%) | ||
| ≥5 | 372/1613 (23.06%) | 0.29–0.37 | <0.001 |
p1 = Proportion among <5; p2 = Proportion among ≥5
Furthermore, out of all patients admitted due to malaria at Marani hospital, most of them were from the 5 to 14 age group with approximately 40% (684/1713) of all malaria admissions (χ2 = 51.45, df = 1, p<0.001). Conversely, at Iguhu/Mukumu hospital, the highest number of all malaria admissions (42% (885/2115) were from the ≥15 age group (χ2 = 11.47, df = 1, p<0.001). Kombewa hospital on contrary observed a highest number of malaria admissions (63.8% (656/1028) among the ≤5 children (p<0.001) (Fig 4).
Fig 4. Malaria admissions and total number of admissions hospitals located in three areas with malaria transmission intensity and interventions responses in Western Kenya from June 2015 to August 2016.
Review of malaria related mortalities
Lowest overall malaria related mortalities were observed at the study site with mesoendemic transmission setting (Iguhu/Mukumu) with 10 deaths per 1000 malaria admissions. However, this site observed highest death rate among the ≥15 patients (19.2 deaths per 1000 ≥15 malaria admissions) and lowest among the 5–14 with 2 death per 1000 of 5–14 years malaria admissions. Marani hospital observed 11 deaths per 1000 of all age groups of malaria admissions. Similar to Iguhu/Mukumu, Marani noted highest fatality rate among the ≥15 age group (17 deaths per 1000 ≥15 years malaria admissions); and on contrary lowest among the ≤5 children (5.8 deaths per 1000 malaria admissions of the 5–14 age group). Kombewa hospital registered the highest overall case fatality rate with 52 deaths per 1000 of all malaria admissions. This hospital, which is located in the hyperendemic setting, had the lowest fatality rate among the 5–14 age group (18 deaths per 1000 admissions of the 5–14 age group). Moreover, Kombewa showed no significant difference between the <5 children (60.9 death per 1000 admission of <5 years) and ≥5 age group (35 death per 1000 admissions (p>0.05)) fatality rates.
In comparison, malaria related death rate was higher among the <5 years old at the high transmission site of Kombewa (60.9 death per 1000 malaria <5 admissions) than the low and moderate transmission settings of Marani and Iguhu/Mukumu respectively (p<0.001). Hospitals located in the low and moderate malaria transmission settings (Marani, Iguhu and Mukumu) experienced highest malaria related death among ≥15 years old (18.6 death per 1000 admissions) than the < 15 years age group (5.7 death per 1000 admissions of the <15 years) (p< 0.001). There was no significant difference between the overall malaria related case fatality rates between Marani and Iguhu/Mukumu. Nevertheless, a higher age specific fatality rate among the 5–14 was noted at Marani when compared with Iguhu and Mukumu together (Table 5).
Table 5. Malaria related case fatality rates from three hospitals located in different infections transmission intensity in Western Kenya from June 2015 to August 2016.
| Fatality rate | Name of the Health facility | Comparison | |||
|---|---|---|---|---|---|
| (per 1000 | Marani | Mukumu | Kombewa | “a” and “b” | a” and “c” |
| malaria | “a” | Iguhu “b” | “c” | p-value | p-value |
| Admissions) | |||||
| < 5 case fatality rate | (3/513) | (3/721) | (40/657) | >0.05 | <0.001 |
| 5.8 | 4.1 | 60.9 | |||
| 5–14 case fatality | (7/684) | (1/518) | (3/169) | <0.05 | >0.05 |
| rate | 10 | 2 | 17.6 | ||
| ≥15 case fatality | (9/516) | (17/885) | (10/203) | >0.05 | <0.05 |
| rate | 17 | 19.2 | 49.3 | ||
| Overall malaria | (19/1713) | (21/2124) | 53/1029 | >0.05 | <0.001 |
| related case | 11 | 10 | 52 | ||
| fatality rate | |||||
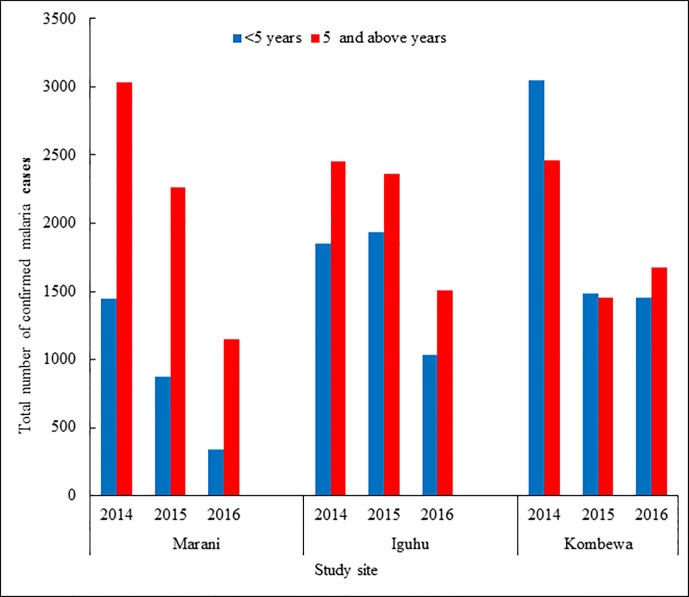
Review of number of outpatient (OPD) malaria cases from 2014 to 2016
The number of Confirmed Malaria cases in three hospitals (Iguhu, Marani and Kombewa County Hospitals) was fewer by approximately 50% from 14,300 cases in 2014 to 7130 in 2016. On the contrary, Kombewa hospital showed more cases in the year just after LLINs distribution (Fig 5). There was a significant reduction of proportions of confirmed malaria out of all OPD consultation among under-fives observed between 2014 and 2016. Morbidity decline from 22.3% to 7.9% at Marani, from 23.5% to 13.2% at Iguhu, and from 32.5% to 29.5% at Kombewa (p< 0.001) was noted. Similarly, a significant reduction of OPD morbidities was observed (p<0.001) among over-fives at Marani and Kombewa. Contrarily, Iguhu experienced a significant increase of OPD malaria consultations among over-fives between 2014 (11.5% (2454/7871) and 2016 (14.8% (1510/10177) (p<0.001) (Table 6).
Fig 5. Trend of confirmed outpatient department malaria cases from 2014 through 2016 from three Hospitals in Western Kenya before and after LLINs mass distribution.
Table 6. Proportions of confirmed malaria to all outpatient department (OPD) visits from three hospitals located in areas with different transmission intensity of Western Kenya as from 2014 to 2016.
| Hospital | Age group | Proportion of Confirmed malaria visits | p-value | ||
|---|---|---|---|---|---|
| (years) | 2014 | 2015 | 2016 | Difference | |
| (LLINs) | 2014 and 2016 | ||||
| Marani | < 5 | 1446/6496 | 872/6153 | 344/4313 | <0.001 |
| (22.3%) | (14.2%) | (7.9%) | |||
| ≥5 | 3033/14007 | 2162/14390 | 1153/11738 | <0.001 | |
| (21.7%) | (15%) | (9.8%) | |||
| Iguhu | <5 | 1851/7871 | 1935/8461 | 1032/7790 | <0.001 |
| (23.5%) | (22.9%) | (13.2%) | |||
| ≥5 | 2454/21394 | 2364/11188 | 1510/10177 | <0.001 | |
| (11.5%) | (21.1%) | (14.8%) | |||
| Kombewa | <5 | 3062/9422 | 1483/5769 | 1454/4923 | <0.001 |
| (32.5%) | (25.7%) | (29.5%) | |||
| ≥5 | 2464/14795 | 1452/12966 | 1564/11504 | <0.001 | |
| (16.7%) | (11.2%) | (13.6%) | |||
(Note: Mass distribution of LLINs to all sites was done in 2015)
Household surveys of long lasting insecticides treated mosquito nets (LLINs) ownership and use
A total of 941 households were surveyed where 85% of them had at least one mosquito net while 43% had a net for every two individuals. The highest use of LLINs was observed among the <5 children with 90.5% (134/148), 88.9% (104/117) and 85.3% (116/136) at Marani, Iguhu and Kombewa respectively (χ2 = 0.01, df = 1, p>0.05). The lowest use of LLINs was witnessed among the 5–14 age group with 71.5% (168/235), 49.3% (105/213) and 57.6% (113/196) (Marani) at Marani, Iguhu and Kombewa respectively (χ2 = 15.03, df = 1, p<0.001). Among the ≥15 age group, the lowest use of mosquito nets was noted at Iguhu with 59.7% (191/320) whereas Marani and Kombewa had 86.7% (225/294) and 82.35 (269/327) respectively (Table 7).
Table 7. Household long lasting insecticide treated mosquito nets (LLINs) use and ownership survey in December 2016 in Western Kenya.
| Household category | Study site | p-value | ||
|---|---|---|---|---|
| Marani | Iguhu | Kombewa | ||
| LLINs ownership | 274/294 | 234/320 | 292/327 | |
| (93.19%) | (73.12%) | (89.29%) | <0.001 | |
| LLINs coverage | 131/294 | 113/320 | 161/327 | |
| (44.56%) | (35.31%) | (49.23%) | <0.001 | |
| Any <5 child slept under | 134/148 | 104/117 | 116/136 | |
| LLINs | (90.54%) | (88.89%) | (85.29%) | 0.379 |
| Any 5–14 child slept under | 168/235 | 105/213 | 113/196 | |
| LLINs | (71.49%) | (49.3%) | (57.64%) | <0.001 |
| Any ≥15 slept under LLINs | 255/294 | 191/320 | 269/327 | |
| (86.73%) | (59.69%) | (82.26%) | <0.001 | |
Discussion
The present study investigated the current infection, morbidity and related case fatality rates of malaria in three areas with different infection transmission intensity in Western Kenya. Even though these three sites have different transmission intensity due to their different topography, altitude and climates, it is expected that with the roll out of malaria intervention through the use of LLINs, malaria infections, morbidity and mortality will drop drastically and even register no more transmission. However, the results of this study shows that the different sites have responded to the intervention differently. Whilst the intervention has reduced transmission in some sites, other sites have remained the same. This has happened despite the country’s investment in malaria strategic (2009–2018) plan of reducing morbidity and mortality by two-third between 2009 and 2018 through increase of uptake of appropriate intervention by 80% among people at risk and 100% coverage of case management among other strategic interventions [28]. Therefore enhanced monitoring of focal malaria transmission and appropriate interventions should be performed.
There was higher malaria positivity rate during surveillance of confirmed clinical cases in the hyperendemic site of Kombewa, where transmission is more perennial than in the other two sites. Transmission is mesoendemic in Iguhu/Mukumu site and epidemic prone in Marani, which has experienced epidemics in the past [29]. Higher, positivity rate among the 5–14 age group that was observed in all study sites has been as well noted in the malaria indicator surveys, in East Africa [17,30]. This could be due to increased exposure to mosquito bite as they start sleeping alone or with other children, a practice that lead to improper utilization of LLINs as observed in the current study. Monitoring clinical malaria blood slide positivity with accurate documentation and diagnosis is therefore vital to intervention evaluation.
The higher positivity rate of asymptomatic infection during the school surveys in the hyperendemic area of Kombewa did not translate into more clinical cases compared with the epidemic prone area of Marani. Malaria transmission in Marani has been historically very low [18] and therefore the people may not have enough functional immunity to malaria and with the infection of Plasmodium parasite, easily get sick. However the population in hyperendemic Kombewa and Iguhu have much exposure to sporozoites and therefore are able to tolerate carriage of Plasmodium without necessarily getting sick.
The proportion of malaria consultations at the OPD among under-fives at the epidemic prone study site was by far higher than previously reported when compared with other similar settings in Kenya [31]. This could be due to the observed infection transmission resurgence that has occurred over the recent years in this area [14]. Higher proportion of malaria consultations at the OPD among the less immune under-fives than over-fives in hyperendemic areas has been also reported in other areas [1,31–33]. On the contrary, the mesoendemic study site had higher proportion of OPD visits due to malaria among over-fives than under-fives. Studies have shown malaria burden shift from under-fives to older children and adults when the transmission intensity decreases [34,35]. The mesoendemic study site is currently also experiencing a decreasing transmission intensity [14,15].
Monthly number of OPD visits due to malaria among the under-fives was consistently higher than diarrhoea or pneumonia throughout the 15 month observations. Having higher number of OPD malaria cases increases chances of having higher cases of fatality rates than that of other childhood killer diseases. Other studies from sub-Sahara Africa also describe malaria as still an important cause of inpatient and outpatient medical consultation [31,36,37].
Severe malaria in hyperendemic settings presented mainly by life threatening persistent vomiting, convulsions and prostration. Patients presenting with severe malaria anaemia in the hyperendemic study site were less than 15% and this shows a decrease of cases when compared to the period before the intensive interventions [10,38]. Pooled data from demographic health surveys from multiple countries showed more risk of anaemia in areas with low coverage and use of mosquito bed nets [39]. The decreased severe malaria anaemia admissions in Western Kenya could be attributed to the ongoing improving bed net coverage and use [13,20,40,41].
The reported changing infection dynamics in the midst of improving LLINs coverage could potentially be catastrophic especially in the epidemic prone setting. This is consistent with other studies in the same settings, which found increasing symptomatic and asymptomatic infections in spite of expanding LLINs ownership and coverage [13,14,31].
The use of hospital records in reporting some of the results in this study may be a limitation in making some of the comparisons. Change in diagnostic and reporting accuracy, case management rate, and health seeking behaviour may also affect the comparisons. Moreover, the selected health facilities in different infection endemicity might be unrepresentative of the study area as they are few. Moreover, the current study present malaria morbidity and mortality at the level four hospitals. Therefore findings from this study may not be generalized to represent all levels of health facilities in Western Kenya.
Conclusion
Malaria is still the major cause of admission in Western Kenya with a slight decrease of the outpatient visits. On one hand, an alarming number of the severe form of the disease among the school age children was observed in the epidemic prone setting. On the other hand, there was decreased proportion of severe malaria anaemia in hyperendemic setting of Kombewa. Mortalities were the highest among under-fives in the hyperendemic study area and among over-fifteen year olds in the mesoendemic and epidemic prone transmission settings. The case related fatality rates are comparable with the previously documented in other areas of sub Saharan Africa. Surveillance of malaria in health facilities as well as asymptomatic infections should be done and interpreted locally for better planning of interventions.
Acknowledgments
Authors are grateful to community members from each study site for their participation in this study during the household survey. Authors would also like to extend their appreciation to schools for their time and patience during data collection. We also acknowledge the Hospital administration at Kombewa, Iguhu and Marani as well as Mukumu for their support during the whole process of data collection. We acknowledge the contribution of all field research assistants throughout the time of data collection.
Data Availability
All relevant data are within the manuscript in terms of tables and figures.
Funding Statement
Funders had no any role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. This study was funded by the National Institutes of Health through grant number RO1 AI050243, U19 AI129326 and D43 TW001505. Dr. Guiyun Yan was a recipient.
References
- 1.WHO (2017) World malaria report 2016 Geneva: World Health Organization [Google Scholar]
- 2.Breman JG (2001) The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. The American journal of tropical medicine and hygiene 64: 1–11. [DOI] [PubMed] [Google Scholar]
- 3.Mogeni P, Williams TN, Fegan G, Nyundo C, Bauni E, Mwai K, et al. (2016) Age, Spatial, and Temporal variations in hospital admissions with malaria in Kilifi County, Kenya: a 25-year longitudinal observational study. PLoS Med 13: e1002047 10.1371/journal.pmed.1002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Meara WP, Mangeni JN, Steketee R, Greenwood B (2010) Changes in the burden of malaria in sub-Saharan Africa. The Lancet infectious diseases 10: 545–555. 10.1016/S1473-3099(10)70096-7 [DOI] [PubMed] [Google Scholar]
- 5.Trape J-F, Tall A, Diagne N, Ndiath O, Ly AB, Faye J, et al. (2011) Malaria morbidity and pyrethroid resistance after the introduction of insecticide-treated bednets and artemisinin-based combination therapies: a longitudinal study. The Lancet infectious diseases 11: 925–932. 10.1016/S1473-3099(11)70194-3 [DOI] [PubMed] [Google Scholar]
- 6.Snow RW, Omumbo JA, Lowe B, Molyneux CS, Obiero J-O, Palmer A, et al. (1997) Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. The Lancet 349: 1650–1654. [DOI] [PubMed] [Google Scholar]
- 7.Kiwuwa MS, Ribacke U, Moll K, Byarugaba J, Lundblom K, Färnert A, et al. (2013) Genetic diversity of Plasmodium falciparum infections in mild and severe malaria of children from Kampala, Uganda. Parasitology research 112: 1691–1700. 10.1007/s00436-013-3325-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ariey F, Hommel D, Le Scanf C, Duchemin JB, Peneau C, Hulin A, et al. (2001) Association of severe malaria with a specific Plasmodium falciparum genotype in French Guiana. Journal of Infectious Diseases 184: 237–241. 10.1086/322012 [DOI] [PubMed] [Google Scholar]
- 9.Esamai F, Nabakwe E, Mining S, Forsberg P, Lewis DH (1999) Clinical presentation and diagnosis of cerebral malaria in children in the highlands of western Kenya. East African medical journal 76: 89–92. [PubMed] [Google Scholar]
- 10.Okach D, Ayisi J, Onyango R (2014) Severe malaria in western Kenya: Analysis of hospital records to determine the influence of transmission level on clinical presentation. Sky Journal of Medicine and Medical Sciences 2: 073–078. [Google Scholar]
- 11.Gitonga CW, Edwards T, Karanja PN, Noor AM, Snow RW, Brooker SJ, et al. (2012) Plasmodium infection, anaemia and mosquito net use among school children across different settings in Kenya. Tropical Medicine & International Health 17: 858–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frosch AE, Ondigo BN, Ayodo GA, Vulule JM, John CC, Cusick SE, et al. (2014) Decline in childhood iron deficiency after interruption of malaria transmission in highland Kenya. The American journal of clinical nutrition 100: 968–973. 10.3945/ajcn.114.087114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou G, Lee M-C, Githeko AK, Atieli HE, Yan G (2016) insecticide-Treated net campaign and Malaria Transmission in Western Kenya: 2003–2015. Frontiers in Public Health 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapesa A, Kweka EJ, Atieli H, Kamugisha E, Zhou G, Githeko AK, et al. (2017) Why some sites are responding better to anti-malarial interventions? A case study from western Kenya. Malaria Journal 16: 498 10.1186/s12936-017-2145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ototo EN, Zhou G, Kamau L, Mbugi JP, Wanjala CL, Machani M, et al. (2017) Age-specific Plasmodium parasite profile in pre and post ITN intervention period at a highland site in western Kenya. Malaria journal 16: 466 10.1186/s12936-017-2119-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wanjala CL, Kweka E (2018) Malaria vectors insecticides resistance in different agro-ecosystems in western Kenya. Frontiers in Public Health 6: 55 10.3389/fpubh.2018.00055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Malaria Control Programme(NMCP), Kenya National Bureau of Statistics (NBoSK), ICF International (2016) Kenya Malaria indicator Survey 2015 Nairobi, Kenya, and Rockville, Maryland, USA: NMCP, KNBS, and ICF International. [Google Scholar]
- 18.Zhou G, Afrane YA, Vardo-Zalik AM, Atieli H, Zhong D, Wamae P, et al. (2011) Changing patterns of malaria epidemiology between 2002 and 2010 in Western Kenya: the fall and rise of malaria. PLoS One 6: e20318 10.1371/journal.pone.0020318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndenga B, Githeko A, Omukunda E, Munyekenye G, Atieli H, Wamai P, et al. (2006) Population dynamics of malaria vectors in western Kenya highlands. Journal of medical entomology 43: 200–206. [DOI] [PubMed] [Google Scholar]
- 20.Ototo EN, Mbugi JP, Wanjala CL, Zhou G, Githeko AK, Yan G (2015) Surveillance of malaria vector population density and biting behaviour in western Kenya. Malaria Journal 14: 1 10.1186/1475-2875-14-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Degefa T, Yewhalaw D, Zhou G, Lee M-c, Atieli H, Githeko AK, et al. (2017) Indoor and outdoor malaria vector surveillance in western Kenya: implications for better understanding of residual transmission. Malaria journal 16: 443 10.1186/s12936-017-2098-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CDC (2016) President's Malaria initiave, Kenya Malaria Operational Plan FY 2016 Atlanta: Department of health and human service, Department of state USA; http://www.pmi.gov/docs/default-source/default-document-library/malaria-operational accesed 21st of September 2016. [Google Scholar]
- 23.Stevenson JC, Stresman GH, Gitonga CW, Gillig J, Owaga C, Marube E, et al. (2013) Reliability of school surveys in estimating geographic variation in malaria transmission in the western Kenyan highlands. PloS one 8: e77641 10.1371/journal.pone.0077641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afrane YA, Zhou G, Githeko AK, Yan G (2014) Clinical malaria case definition and malaria attributable fraction in the highlands of western Kenya. Malaria journal 13: 405 10.1186/1475-2875-13-405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Public Health and Sanitation (2010) National Guideline for diagnosis, treatment and prevention of malaria in Kenya, Third edition edition. Nairobi: Ministry of Health and Sanitation. [Google Scholar]
- 26.Atieli HE, Zhou G, Afrane Y, Lee M-C, Mwanzo I, Githeko AK, et al. (2011) Insecticide-treated net (ITN) ownership, usage, and malaria transmission in the highlands of western Kenya. Parasites & vectors 4: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO (2013) Methods for achieving universal coverage with long-lasting insecticidal nets in malaria control Geneva: World Health Orgnization. [Google Scholar]
- 28.Kenya Ministry of Health (2014) Kenya Malaria strategy 2009–2018 Nairobi: Kenya Ministry of Health. [Google Scholar]
- 29.Malakooti M, Biomndo K, Shanks G (1998) Reemergence of epidemic malaria in the highlands of western Kenya. Emerging infectious diseases 4: 671 10.3201/eid0404.980422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferede G, Worku A, Getaneh A, Ahmed A, Haile T, Abdu Y, et al. (2013) Prevalence of malaria from blood smears examination: a seven-year retrospective study from Metema Hospital, Northwest Ethiopia. Malaria research and treatment 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Machini B, Waqo E, Kizito W, Edwards J, Owiti P, Takarinda K (2016) Trends in outpatient malaria cases, following Mass Long Lasting Insecticidal Nets (LLIN) distribution in epidemic prone and endemic areas of Kenya. East African Medical Journal 93: 10–15. [Google Scholar]
- 32.Guinovart C, Bassat Q, Sigaúque B, Aide P, Sacarlal J, Nhampossa T, et al. (2008) Malaria in rural Mozambique. Part I: Children attending the outpatient clinic. Malaria Journal 7: 36 10.1186/1475-2875-7-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oguttu DW, Matovu JKB, Okumu DC, Ario AR, Okullo AE, Opigo J, et al. (2017) Rapid reduction of malaria following introduction of vector control interventions in Tororo District, Uganda: a descriptive study. Malaria Journal 16: 227 10.1186/s12936-017-1871-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ursing J, Rombo L, Rodrigues A, Aaby P, Kofoed P-E (2014) Malaria transmission in Bissau, Guinea-Bissau between 1995 and 2012: malaria resurgence did not negatively affect mortality. PloS one 9: e101167 10.1371/journal.pone.0101167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mawili-Mboumba DP, Akotet MKB, Kendjo E, Nzamba J, Medang MO, Mbina J-RM, et al. (2013) Increase in malaria prevalence and age of at risk population in different areas of Gabon. Malaria journal 12: 3 10.1186/1475-2875-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jagannathan P, Muhindo MK, Kakuru A, Arinaitwe E, Greenhouse B, Tappero J, et al. (2012) Increasing incidence of malaria in children despite insecticide-treated bed nets and prompt anti-malarial therapy in Tororo, Uganda. Malaria journal 11: 435 10.1186/1475-2875-11-435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mutsigiri F, Mafaune PT, Mungati M, Shambira G, Bangure D, Juru T, et al. (2017) Malaria morbidity and mortality trends in Manicaland province, Zimbabwe, 2005–2014. Pan African Medical Journal 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okiro EA, Al-Taiar A, Reyburn H, Idro R, Berkley JA, Snow RW, et al. (2009) Age patterns of severe paediatric malaria and their relationship to Plasmodium falciparum transmission intensity. Malaria journal 8: 4 10.1186/1475-2875-8-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Florey L (2012) Anemia as an impact measure of ITN use among young children Calverton, Maryland USA: ICF International. [Google Scholar]
- 40.Aregawi MW, Ali AS, Al-Mafazy A-W, Molteni F, Katikiti S, Warsame M, et al. (2011) Reductions in malaria and anaemia case and death burden at hospitals following scale-up of malaria control in Zanzibar, 1999–2008. Malaria journal 10: 46 10.1186/1475-2875-10-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smithson P, Florey L, Salgado SR, Hershey CL, Masanja H, Bhattarai A, et al. (2015) Impact of malaria control on mortality and anemia among Tanzanian children less than five years of age, 1999–2010. PLoS One 10: e0141112 10.1371/journal.pone.0141112 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript in terms of tables and figures.