Abstract
Objectives. To improve public health surveillance and response by using spatial optimization.
Methods. We identified cases of suspected nonfatal opioid overdose events in which naloxone was administered from April 2013 through December 2016 treated by the city of Pittsburgh, Pennsylvania, Bureau of Emergency Medical Services. We used spatial modeling to identify areas hardest hit to spatially optimize naloxone distribution among pharmacies in Pittsburgh.
Results. We identified 3182 opioid overdose events with our classification approach, which generated spatial patterns of opioid overdoses within Pittsburgh. We then used overdose location to spatially optimize accessibility to naloxone via pharmacies in the city. Only 24 pharmacies offered naloxone at the time, and only 3 matched with our optimized solution.
Conclusions. Our methodology rapidly identified communities hardest hit by the opioid epidemic with standard public health data. Naloxone accessibility can be optimized with established location–allocation approaches.
Public Health Implications. Our methodology can be easily implemented by public health departments for automated surveillance of the opioid epidemic and has the flexibility to optimize a variety of intervention strategies.
Amid a national public health crisis of opioid overdoses in the United States, Pennsylvania has the sixth-highest rate of drug overdose deaths (26.3 per 100 000).1 In 2015, there were 3264 overdose deaths in Pennsylvania, a 20.1% increase from 2014.1 Southwestern Pennsylvania represents one of the regions hardest hit by the opioid epidemic, with the city of Pittsburgh bearing much of the burden.2 Mitigation efforts include enhanced surveillance to identify communities at risk and enhancing accessibility to health care resources.
Many opioid overdoses in the community are encountered by emergency medical services (EMS) personnel who can administer naloxone,3 an opioid antagonist that reverses opioid overdose.4 Naloxone has been credited with countless lives saved in the opioid epidemic and use of this medication has been increasing across the country.4,5 It rapidly reverses the effects of an opioid overdose, which include unresponsiveness and respiratory depression or apnea.
Naloxone can be administered intravenously, intramuscularly, and intranasally. While naloxone has traditionally been administered by EMS personnel via intravenous or intramuscular routes, bystanders have begun to use this through intramuscular auto-injectors or intranasal spray preparations that may be available to laypersons by prescription. In a typical case, a bystander such as a family member who recognizes a victim of an opioid overdose would call 9-1-1 for an EMS response and, if naloxone were previously obtained and available, administer naloxone to the individual. Naloxone may begin to take effect even before ambulance arrival, and in the case of a patient with apnea for whom minutes count, could prevent an opioid-related death.
To increase the availability and use of naloxone by bystanders in Pennsylvania, the Secretary of Health and Physician General of the Pennsylvania Department of Health has written a standing-order prescription so that anyone in Pennsylvania can obtain naloxone through their local pharmacy without need for an individual prescription from a physician.6 However, at the time of this study, accessibility to naloxone remained limited, with many pharmacies not regularly stocking this medication,7 limiting the potential impact of a major public health intervention such as a statewide standing-order prescription, and, thus, we only used confirmed pharmacies stocking naloxone for our analysis.
Currently, there is a gap in the literature addressing the optimal distribution of naloxone. Spatial methods could vastly enhance the ability to maximize the public health benefit of naloxone accessibility. Implementation of location–allocation models in a geographic information system (GIS) can be leveraged to optimize health care accessibility.8 Specifically, location data of resource utilization (such as address level of naloxone administration) can be used to spatially refine public health policy. These models have been used to optimize prehospital services,9,10 access to health care facilities (e.g., hospitals, maternal and child health, primary care services),11,12 and access to vital medicine such as antiretroviral therapy.13,14 However, to the best of our knowledge, these spatial methods have not yet been adapted by public health departments for opioid overdose surveillance and mitigation efforts.
Neighborhood pharmacy-based naloxone distribution has the potential to provide greater accessibility to care for opioid drug users,15 reduce time to opioid overdose rescue,6 and potentially allow pharmacists to provide initial overdose prevention counseling.16 Our analysis builds on previous work in the Pittsburgh area that examined areal patterns of naloxone in pharmacies and death rates,17 whereby we used individual-level data for nonfatal opioid overdoses to provide spatially refined solutions for increasing naloxone accessibility. We used Pittsburgh and its distribution of naloxone throughout pharmacies as a case study to highlight how spatial methods can (1) optimize accessibility to naloxone by identifying deficiencies in access and (2) redistribute naloxone among pharmacies in communities with the highest incidence of opioid overdoses to more effectively mitigate the opioid epidemic. For this case study, we sought to demonstrate how location–allocation modeling can be efficiently performed by using GIS to optimize the availability of naloxone in public health systems throughout the country.
METHODS
We defined an overdose event as a case involving the administration of naloxone by bystanders, first responders, or EMS personnel in the city of Pittsburgh for a nonfatal opioid overdose involving a single dose or multiple doses for an individual patient. Ultimately, we chose to focus exclusively on nonfatal cases, as these best represent opportunities for applied spatial optimization interventions for those who can access health services.
Data Acquisition
We identified cases through review of the electronic patient care records used by the Pittsburgh Bureau of Emergency Medical Services (emsCharts Inc, Warrendale, PA). Similar to other EMS systems in the United States, naloxone is available on all ambulances in Pittsburgh, and it may be available to bystanders if previously acquired, most commonly from a pharmacy. We used custom reporting software in emsCharts to obtain data including the date and time of response, the response location, amount of naloxone administered, and a record regarding whether the individual was transferred to a hospital. We first captured all records with any mention of “naloxone” or “Narcan” in the history of present illness (via text search) or in the treatment section from April 2013 through December 2016. We then manually reviewed cases in which naloxone was mentioned but not included in the treatment section to verify it was a case of suspected opioid overdose in which naloxone was administered by bystanders, first responders, or EMS personnel. We used a conservative classification and only retained events in which an individual had a nonfatal opioid overdose and received naloxone. We used GIS (Esri ArcGIS 10.5.1, Redlands, CA) to map the location and track opioid overdose events across Pittsburgh throughout the study period (2013–2016).
We separately collected data from OverdoseFreePA for all pharmacies that were offering naloxone and restricted it to those operating within the city as of January 1, 2017, to align with the EMS data. OverdoseFreePA is a Web site dedicated to disseminating critical information and data on the opioid epidemic in western Pennsylvania. In preparation of the location–allocation modeling, we converted the locations of the nonfatal opioid overdose events and the pharmacies from latitude and longitude coordinates to state plane coordinates; the location–allocation analysis necessitates the conversion of these locations to those that can be used for analysis with a projected coordinate system. In addition, we used speed limits for the Pittsburgh road network to minimize overall travel time to the closest pharmacy offering naloxone.
Data Analysis
We assessed the current availability of naloxone in pharmacies throughout the city and modeled the optimal allocation of naloxone by using each naloxone administration incident of a nonfatal opioid overdose (as specified according to our selection criteria) as the demand. Our approach assumes that improving spatial accessibility of naloxone can potentially reduce the number of deaths related to opioid overdose. An important step when one is working with sensitive, individual-level data is de-identification. A common technique for working with data of this type is to geomask the data—incorporate statistical noise into the point-level data to prevent identification of individuals.18 For this analysis, we geomasked the data and then aggregated nonfatal opioid overdoses to an average block size (approximately 310 sq ft) to visualize the intensity of nonfatal opioid overdoses throughout Pittsburgh, and then used the geomasked incident data for location–allocation analysis to improve accessibility to naloxone. The aggregated, geomasked data on nonfatal overdoses are represented with graduated circles whose areas are proportional to the number of expected demand cases.
We conducted location–allocation analysis to evaluate locational efficiency of the existing distribution of pharmacies in Pittsburgh stocking naloxone during our study period and assessed their effectiveness to provide naloxone to communities that need it most. Facility location models have been developed and applied to health care planning to describe hospital catchment areas or distribute health resources.19 In particular, location–allocation models aiming to address location and allocation decisions have been widely used in health planning by minimizing specific parameters such as travel distance or time,20 but they can also be used to assess the optimal distribution of selected facilities. During our study period, there were a total of 24 pharmacies (out of a possible 87) stocking naloxone. We solved our location–allocation problem by using the p-median model in ArcGIS 10.5.1,21,22 whereby we minimized the total distance between overdose locations (demand points) and the closest pharmacy (supply points), allowing us to select the best possible spatial configuration of 24 pharmacies to offer naloxone to the community in need (i.e., we used the entire set of possible pharmacy locations to optimize the distribution of naloxone). Specification of the p-median model is discussed in greater detail in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org.
For our case study, ultimately, the p-median model is a more practical choice for improving overall accessibility to naloxone through pharmacies because it reduces the overall distance traveled—that is, people who need naloxone (demand points) must travel to the closest pharmacy (supply point[s]) to acquire it, as opposed to choosing the maximize coverage model, which would focus on pharmacies delivering naloxone to those who need it at the location of overdose. Here, the selection of the current pharmacies to stock naloxone minimized overall travel time by taking into consideration both distance and time to closest pharmacy. This was done by using the road network in Pittsburgh (which accounts for both travel distance and speed). This can be solved efficiently by using GIS to generate a near-optimal solution22 and generates computational savings, which allow for efficient analysis.
RESULTS
There were 3270 cases identified via naloxone administration or mention of naloxone in the medical records obtained through emsCharts. For the analyses, we excluded 88 cases that did not receive naloxone because of improvement in mental status (n = 84), nonopioid ingestion suspected (n = 2), or death pronouncement on scene (n = 2). This resulted in 3182 patients who received naloxone in the field and were included in the final analysis. Most patients receiving naloxone in the field were transported to the emergency department; only 4% refused either care or transport.
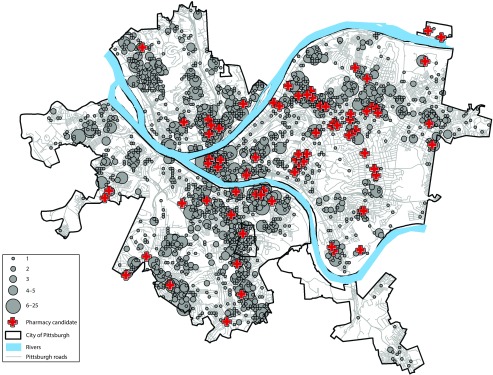
The spatial pattern of naloxone administration in Pittsburgh and where it occurred are displayed in Figure 1. We used the quantiles to represent the graduated number of incidents (derived statistically) to visualize the intensity of naloxone use. Communities where the opioid epidemic is most entrenched are noted throughout the city (note: the small rectangular area that appears as an “island” in Pittsburgh is technically outside the city limits—Mt Oliver).
FIGURE 1—
Spatial Distribution of Naloxone Administration Events: Pittsburgh, PA, April 2013–December 2016
In Figure 1, the locations of all pharmacies (candidate pharmacies) are marked as red crosses throughout the city. Of the 87 pharmacies in Pittsburgh, only 24 were identified on OverdoseFreePA as stocking naloxone during our study period. The 87 pharmacies in Pittsburgh are used to represent the full set of candidate locations where naloxone could be stocked, which could be used to reallocate naloxone to improve accessibility by minimizing the travel cost of obtaining it.
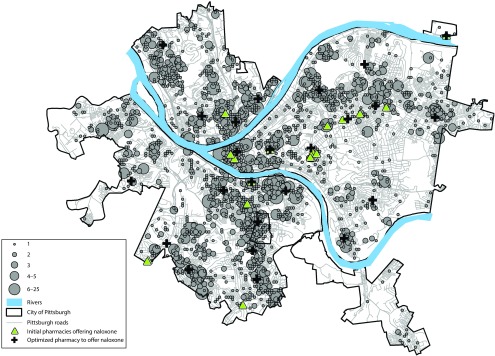
Figure 2 provides both the initial configuration of pharmacies carrying naloxone (green triangles) and the optimal solution that improves accessibility by minimizing travel according to the locations where people are overdosing (black crosses)
FIGURE 2—
Spatially Optimized Pharmacies That Should Stock Naloxone: Pittsburgh, PA, April 2013–December 2016
Out of the original 24 pharmacies offering naloxone, only 3 agreed between the current and optimized model. We chose 21 pharmacies from the candidate set of pharmacies that were in operation during our study period and represented a spatially optimized solution that minimized travel cost and increased accessibility for communities hardest hit. This reconfiguration shaved roughly more than two tenths of a mile off the average distance to the closest pharmacy offering naloxone, which may not sound like much, but provides crucial minutes for acquisition and administration. Conversely, the existing configuration of pharmacies has 21 that currently stock naloxone in areas that do not need it as much as other communities.
DISCUSSION
This study demonstrated how accessibility to an essential opioid antagonist can be optimized by using EMS data of previous opioid overdoses and spatial analytics. Our analyses were guided by an underlying assumption that improvement in the spatial accessibility of naloxone could reduce the number of deaths related to opioid overdose. It relied on established methods that can be implemented by using GIS, allowed extrapolation to other settings, and provided a framework that any public health department can implement. End users could use similar analyses for community surveillance to inform policy development and implementation.
By transforming discrete point-level data into a geovisualization that highlights areas in the study region with greater frequency of nonfatal opioid overdoses, we demonstrated a method for rapid assessment of the opioid epidemic by using first-responder data. Although we used Pittsburgh as our case study and our results identified that 5 neighborhoods were at highest risk, this analysis focused on demonstrating the application of established spatial methods to help maximize limited resources for mitigating the opioid epidemic, an approach that can be easily adapted for rural and urban communities elsewhere.
Residents in these communities may suffer from depressed local economies and limited accessibility to health care already. For example, in Pittsburgh there are no hospitals south of the rivers that are technically in city limits. This may result in longer transport times to an emergency department given the physical distance to hospitals south of the city, or the need to cross tunnels and bridges to access the city’s hospitals. Using proportional graduated circles to represent the incident locations, we identified these at-risk communities and can target health care interventions such as making naloxone available in the community, bridging the gap between communities and hospital-based resources.
Improving accessibility to naloxone that is not reliant on EMS or hospital-based resources could take many forms. For example, overdose education and naloxone distribution programs have trained bystanders to help assist in the administration of naloxone in opioid overdose events.23 Public health advocacy organizations have also made progress by combining naloxone distribution with clean needle exchange.24 Considering a statewide standing-order prescription for naloxone is available in Pennsylvania, as well as increasing emphasis of physicians in our city to provide instructions on obtaining naloxone upon discharge following an opioid overdose, we focused on the availability of naloxone through community pharmacies. We found that out of 87 pharmacies in operation in Pittsburgh during our study period, only 24 offered naloxone and a mere 3 pharmacies were in an optimal location per our model of at-risk communities. Although it could be expected that all pharmacies stock naloxone or that new pharmacies open in areas where it is currently not available, these are costly interventions for an already costly public health crisis. In addition, shortages of auto-injectors and emergency medications including naloxone may make availability at all pharmacies unfeasible. Instead, the current stock of naloxone could be redistributed among existing pharmacies to better serve those areas that need it most. Similar analyses could be utilized to inform other potentially costly public health interventions to address the opioid epidemic, such as spatially optimizing the distribution of naloxone through public health advocacy groups, a peer support program, and warm hand-off via a community paramedicine initiative.
Data from EMS are unique in nature and have played a critical role in targeting public health interventions. The uniqueness of these data is ultimately what allows for spatially optimized interventions. For example, EMS data have been used to improve accessibility to trauma centers, helping redistribute the burden of care and maximize patient outcomes25,26; to optimize access to primary care stroke centers to help stroke victims recover faster27,28; and to help optimize care for opioid abuse in rural locations.29 Our research contributes to the growing literature on leveraging EMS data for public health interventions. Furthermore, because these data are ubiquitous throughout the United States, our approach can be easily implemented in a variety of urban and rural settings.
Limitations
We identified cases of suspected opioid overdose with naloxone administration on the basis of documentation of naloxone use in EMS patient care records. This may have missed cases that were incorrectly documented within the electronic record. Our manual review and classification of the EMS data took a conservative approach and may not have captured all opioid overdoses. We may have also missed cases of opioid overdose in which bystanders had naloxone available, appropriately treated the overdose, and never called 9-1-1. Although these missing cases in our analysis may underrepresent the true incidence of opioid overdoses, it is common practice in Pittsburgh for citizens to call 9-1-1 for an EMS response even when naloxone is used by bystanders, and it is unlikely that this would substantially bias the distribution of cases resulting in EMS response.
Furthermore, the data on pharmacies throughout Pittsburgh that offered naloxone during our study period may suffer from a lag when naloxone is reported as being stocked, as well as implications of pharmacy supply chain policy affecting the availability of naloxone. However, OverdoseFreePA seeks to minimize this lag by employing staff to call and confirm drug availability with local pharmacies.
Finally, our descriptive analysis only captured areas that were purely spatial in nature and did not consider temporal dynamics. Although including temporal data in our analysis would have improved the estimates of how overdose events evolved over our study period, our approach captures the chronic hot spots throughout the city. Future work should expand the purely spatial approach to a spatiotemporal one by using scan statistics to better understand how nonfatal opioid overdoses may fluctuate temporally across the city. In addition, data on utilization rates would be beneficial for assessing the impact of improved accessibility on a reduction in opioid overdoses.
Public Health Implications
Accessibility to health care resources has been broadly defined in the form of either nonspatial or spatial accessibility.30 Accessibility can also refer to the societal factors that may impede accessibility to health care.30 The gold standard is to ensure that all members of society have equal accessibility to health care,31 a goal that is often not achieved. New approaches to public health surveillance and mitigation of the opioid crisis must consider this inequality by accounting for demographic and economic factors, distance and time to treatment (physical accessibility), and ways to improve accessibility to immediate treatment that is not reliant on existing hospital and EMS systems.8,9
Methods similar to those employed in this study are essential to target and maximize limited health care resources in the fight against the opioid epidemic and are critical to identify communities at greatest risk. Policy designed to mitigate the opioid epidemic is only as strong as the detection of the event; otherwise, suboptimal policy may be implemented and not overly effective. This is demonstrated by the current allocation of naloxone within pharmacies in Pittsburgh that are not located in the communities where chronic hot spots of opioid overdose occur. Future efforts to deploy opioid overdose interventions should be informed by similar analyses at the local, regional, or state level.
Conclusions
Our analysis demonstrated how accessibility to naloxone in the community can be improved through spatial modeling of opioid overdoses in relation to existing health care resources. Although it focused on the availability of naloxone at community pharmacies, similar methods could be used to target other public health interventions amid the opioid crisis, including the positioning of emergency responder units, public accessibility to naloxone, and targeted education interventions. Identifying how these spatial modeling methods can have an impact on multiple interventions could also address overdoses of nonresidents who would not likely have access to naloxone from community-based pharmacies.
ACKNOWLEDGMENTS
The authors thank the dedicated emergency medical services first responders for the city of Pittsburgh. In addition, we are grateful for the expert advice received from the anonymous reviewers.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval from the University of Pittsburgh was obtained for this study.
Footnotes
See also Dasgupta, p. 1122.
REFERENCES
- 1.Injury Prevention and Control. Opioid overdose. Drug overdose death data. Centers for Disease Control and Prevention. 2016. Available at: https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed October 20, 2017.
- 2. 2015 overdose data for Allegheny County. Allegheny County Medical Examiner’s Office. Available at: https://www.overdosefreepa.pitt.edu/know-the-facts/view-overdose-death-data. Accessed October 15, 2017.
- 3.Nielsen K, Nielsen SL, Siersma V, Rasmussen LS. Treatment of opioid overdose in a physician-based prehospital EMS: frequency and long-term prognosis. Resuscitation. 2011;82(11):1410–1413. doi: 10.1016/j.resuscitation.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 4.Davis CS, Ruiz S, Glynn P, Picariello G, Walley AY. Expanded access to naloxone among firefighters, police officers, and emergency medical technicians in Massachusetts. Am J Public Health. 2014;104(8):e7–e9. doi: 10.2105/AJPH.2014.302062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyon S, Aks SE, Schaeffer S. Expanding access to naloxone in the United States. J Med Toxicol. 2014;10(4):431–434. doi: 10.1007/s13181-014-0432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pennsylvania Department of Health. Standing Order DOH-002–2016: Naloxone prescription for overdose prevention. Available at: http://www.dos.pa.gov/ProfessionalLicensing/BoardsCommissions/Documents/SN%20-%20Naloxone%20Prescription%20for%20Overdose%20Prevention%20(Standing%20Order%20DOH-002-2016).pdf. Accessed June 13, 2018.
- 7.Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Wang F. Measurement, optimization, and impact of health care accessibility: a methodological review. Ann Assoc Am Geogr. 2012;102(5):1104–1112. doi: 10.1080/00045608.2012.657146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chanta S, Mayorga ME, McLay LA. Improving emergency service in rural areas: a bi-objective covering location model for EMS systems. Ann Oper Res. 2014;221(1):133–159. [Google Scholar]
- 10.Khodaparasti S, Maleki H, Bruni ME, Jahedi S, Beraldi P, Conforti D. Balancing efficiency and equity in location-allocation models with an application to strategic EMS design. Optim Lett. 2016;10(5):1053–1070. [Google Scholar]
- 11.Polo G, Acosta CM, Ferreira F, Dias RA. Location-allocation and accessibility models for improving the spatial planning of public health services. PLoS One. 2015;10(3):e0119190. doi: 10.1371/journal.pone.0119190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmadi-Javid A, Seyedi P, Syam SS. A survey of healthcare facility location. Comput Oper Res. 2017;79:223–263. [Google Scholar]
- 13.Gerberry DJ, Wagner BG, Garcia-Lerma JG, Heneine W, Blower S. Using geospatial modeling to optimize the rollout of antiretroviral-based pre-exposure HIV interventions in sub-Saharan Africa. Nat Commun. 2014;5:5454. doi: 10.1038/ncomms6454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dodson ZM, Agadjanian V, Driessen J. How to allocate limited healthcare resources: lessons from the introduction of antiretroviral therapy in rural Mozambique. Appl Geogr. 2017;78:45–54. doi: 10.1016/j.apgeog.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaller ND, Yokell MA, Green TC, Gaggin J, Case P. The feasibility of pharmacy-based naloxone distribution interventions: a qualitative study with injection drug users and pharmacy staff in Rhode Island. Subst Use Misuse. 2013;48(8):590–599. doi: 10.3109/10826084.2013.793355. [DOI] [PubMed] [Google Scholar]
- 16.Green TC, Dauria EF, Bratberg J, Davis CS, Walley AY. Orienting patients to greater opioid safety: models of community pharmacy-based naloxone. Harm Reduct J. 2015;12(1):25. doi: 10.1186/s12954-015-0058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burrell A, Ethun L, Fawcett JA et al. The pharmacist’s role in overdose: using mapping technologies to analyze naloxone and pharmacy distribution. J Am Pharm Assoc (2003) 2017;57(2S):S73–S77.e1. doi: 10.1016/j.japh.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Leitner M, Curtis A. A first step towards a framework for presenting the location of confidential point data on maps—results of an empirical perceptual study. Int J Geogr Inf Sci. 2006;20(7):813–822. [Google Scholar]
- 19. Church RL. Location modelling and GIS. In: Longley PA, Goodchild MF, Maguire DJ, Rhind DW, eds. Geographical Information Systems: Principles, Techniques, Management and Applications. 2nd ed, abridged. Hoboken, NJ: John Wiley & Sons; 2005:293–303.
- 20.Murray AT, Grubesic TH. Locational Planning of Health Care Facilities. Spatial Analysis in Health Geography. New York, NY: Ashgate; 2016. pp. 243–259. [Google Scholar]
- 21.Hakimi SL. Optimum locations of switching centers and the absolute centers and medians of a graph. Oper Res. 1964;12(3):450–459. [Google Scholar]
- 22.Environmental Systems Research Institute. Algorithms used by the ArcGIS Network Analyst extension. Available at: http://resources.arcgis.com/en/help/main/10.2/index.html#/algorithms_used_by_the_arcgis_network_analyst_extension/004700000053000000. Accessed September 5, 2017.
- 23.Walley AY, Doe-Simkins M, Quinn E, Pierce C, Xuan Z, Ozonoff A. Opioid overdose prevention with intranasal naloxone among people who take methadone. J Subst Abuse Treat. 2013;44(2):241–247. doi: 10.1016/j.jsat.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 24.Bennett AS, Bell A, Tomedi L, Hulsey EG, Kral AH. Characteristics of an overdose prevention, response, and naloxone distribution program in Pittsburgh and Allegheny County, Pennsylvania. J Urban Health. 2011;88(6):1020–1030. doi: 10.1007/s11524-011-9600-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nance ML, Carr BG, Branas CC. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med. 2009;163(6):512–518. doi: 10.1001/archpediatrics.2009.65. [DOI] [PubMed] [Google Scholar]
- 26.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Distance matters: effect of geographic trauma system resource organization on fatal motor vehicle collisions. J Trauma Acute Care Surg. 2017;83(1):111–118. doi: 10.1097/TA.0000000000001508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mullen MT, Wiebe DJ, Bowman A et al. Disparities in accessibility of certified primary stroke centers. Stroke. 2014;45(11):3381–3388. doi: 10.1161/STROKEAHA.114.006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullen MT, Branas CC, Kasner SE et al. Optimization modeling to maximize population access to comprehensive stroke centers. Neurology. 2015;84(12):1196–1205. doi: 10.1212/WNL.0000000000001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA. Access to emergency care in the United States. Ann Emerg Med. 2009;54(2):261–269. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donabedian A. Aspects of Medical Care Administration: Specifying Requirements for Health Care. Cambridge, MA: Harvard University Press; 1973. pp. 72–110. [Google Scholar]
- 31.Ricketts TC. Geographic Methods for Health Services Research: A Focus on the Rural–Urban Continuum. Lanham, MD: University Press of America; 1994. pp. 103–128. [Google Scholar]