Abstract
Objectives. To survey the spatial distribution and enteric pathogen profile of discarded human feces in the city of Atlanta, Georgia.
Methods. After defining priority search areas in central Atlanta, we conducted 5 searches of open defecation sites totaling 15 hours during the period from October 2017 to January 2018. We collected fresh stools for analysis via multiplex reverse-transcription polymerase chain reaction to identify presence of 15 common parasitic, bacterial, and viral enteric pathogens.
Results. We identified and mapped 39 open defecation sites containing 118 presumptive human stools; 23% of the 26 collected fresh stools tested positive for 1 or more pathogens. An estimated 12% of stools were positive for enterotoxigenic Escherichia coli, 7.7% for Giardia spp., 3.8% for norovirus, and 3.8% for Salmonella spp. The majority (92%) of identified open defecation sites were within 400 meters of a shelter or soup kitchen.
Conclusions. Though this study was constrained by a small sample size, results suggest that open defecation in Atlanta is common and may pose risks to public health.
Public Health Implications. Open defecation may pose health risks to people experiencing homelessness and the general public.
The association between open defecation and a wide range of health risks is well documented in low- and middle-income countries,1 as unsafely managed fecal contamination in the environment leads to potential for exposure to enteric pathogens. In high-income countries, open defecation can occur among persons experiencing homelessness who may lack ready access to sanitation facilities when and where they are needed.
An estimated 3 million people in the United States experience homelessness each year, with approximately one third of counted persons occupying unsheltered locations.2 More than 4000 people were estimated to be experiencing homelessness in Atlanta, Georgia, during the 2016 Point-in-Time Count, a national survey of people experiencing homelessness conducted by the US Department of Housing and Urban Development, with nearly 1000 occupying unsheltered locations.3 The ability of persons experiencing homelessness in the United States to maintain an adequate level of hygiene is constrained by the facilities available for their use, which may be highly variable across settings.4 A reduced availability of public toilets in high-income countries in the past 20 years and the criminalization of homelessness through antinuisance laws has worsened sanitation access for some.5,6
Despite recent disease outbreaks associated with poor sanitation among persons experiencing homelessness—notably, hepatitis A in California7—we identified no previous published studies of open defecation in the United States, either in terms of prevalence or associated microbial risks. In response to anecdotal accounts of open defecation in Atlanta by persons experiencing homelessness and references in the literature to the potential for open defecation caused by a lack of sanitation facilities serving this population,7 we conducted an observational survey to estimate the spatial distribution and enteric pathogen profile of discarded human feces in the city.
METHODS
We conducted a systematic search for open defecation sites in a predefined 2.4-square-kilometer area of central Atlanta, totaling 15 hours over 5 days during the period from October 2017 to January 2018. We mapped each site and counted all apparent human stools, also noting general site characteristics. We tracked the following indicators to distinguish between human and animal feces: presence of anal cleansing materials, makeshift latrines, presence of refuse such as paper and used condoms, presence of soiled clothing, multiple stools at an open defecation site, large-volume stools, the presence or odor of urine, and characteristic patterns of feces resulting from defecation while leaning against a surface.
When possible to do so without garnering attention from persons nearby, we collected a 2-gram sample of fecal material. We sampled only apparently fresh, unfrozen stools with moist cores, from the centermost point of the stool. Within 5 hours of collection, samples were stored at −80°C for later analysis.
We extracted total nucleic acids from 100 milligrams of stool samples by using the QIAamp 96 Virus QIAcube HT kit (Qiagen N.V., Hilden, Germany). We analyzed nucleic acid extracts through the xTAG Gastrointestinal Pathogen Panel (Luminex Molecular Diagnostics Inc, Toronto, Ontario). The Luminex Gastrointestinal Pathogen Panel is a multiplex reverse-transcriptase polymerase chain reaction–based method that detects common enteric pathogens, including Campylobacter spp., Clostridium difficile toxin A or B, Escherichia coli O157, enterotoxigenic E coli heat-labile or heat-stable enterotoxin, Shiga-like toxin 1 or 2–producing E coli, Salmonella spp., Shigella spp., Vibrio cholerae, Yersinia enterocolitica, adenovirus 40 or 41, norovirus genogroups I or II, rotavirus A, Giardia spp., Cryptosporidium spp., and Entamoeba histolytica. The method is primarily used as a stool-based diagnostic assay that has been validated in comparison with other polymerase chain reaction–based methods for direct detection of enteric infections in a range of settings.8
RESULTS
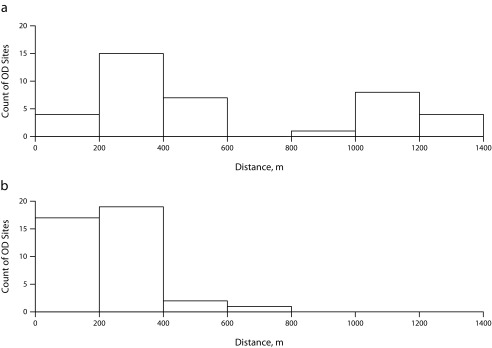
We identified 118 discarded human stools in 39 sites in the search area. Of the open defecation sites, 85% appeared to offer some privacy or shelter; typical sites included underneath overpasses (26%), adjacent to dumpsters (15%), narrow alleys with limited visibility (10%), and stairwells (8%). Other locations included parking garages, behind trees and bushes, behind buildings, in building alcoves, and along fences; the 15% of open locations were directly on or adjacent to sidewalks. We observed anal cleansing materials at 28% of open defecation sites and flies at 13% of the sites; 92% of documented open defecation sites existed within 400 meters of a shelter or soup kitchen (Figure 1). We encountered 78% of stools at 33% of the sites.
FIGURE 1—
Histograms Showing Distances From Open Defecation (OD) Sites to (a) the Nearest Public Restroom and (b) the Nearest Shelter or Soup Kitchen: Atlanta, GA, October 2017–January 2018
Note. We omitted specific data on the location of open defecation sites because of concerns that this information could result in enforcement actions against persons experiencing homelessness.
Of the 118 stools identified in the survey area, we analyzed the 26 stools with moist cores indicating recent disposal; 23% of these tested positive for 1 or more enteric pathogens: 12% tested positive for enterotoxigenic E coli, 7.7% for Giardia spp., 3.8% for norovirus, and 3.8% for Salmonella spp. Stool samples contained an average water content of 73% (SD = 10%), which is within the range of established values for fresh human stool.9 We excluded 1 sample from analysis following inconclusive reverse-transcriptase polymerase chain reaction results. Random duplicate samples (n = 6) yielded fully consistent results.
DISCUSSION
This study provides evidence that open defecation is relatively common in the urban core of a major American city, despite global statistics that suggest universal access to sanitation.10 Although it was not a comprehensive survey of open defecation in Atlanta, we identified 39 open defecation sites containing 118 stools in a rapid search that was limited to 15 hours over 5 days. The number of stools encountered in this survey was limited by the presence of other persons: we purposefully avoided contact with people in the search areas because of concerns about causing embarrassment. It is possible that not all stool was of human origin or from persons experiencing homelessness. Also, we cannot estimate the population of persons resorting to open defecation because multiple stools in this study may have been from the same individual.
It is likely that open defecation in Atlanta is not limited to the small area we surveyed. We did not search areas surrounding any apparent homeless camp, identified by the presence of tents or bedding, or any area marked “no trespassing.” Excluding these sites introduces a potential bias in our counts of open defecation sites in the search area.
The proximity of open defecation sites to shelters and soup kitchens suggests that those facilities are not meeting the sanitary needs of persons experiencing homelessness. As 78% of the stools in this study were found at only 33% of the open defecation sites, we suspect that localized sanitation interventions might be effective at reducing open defecation. However, the use of sanitation facilities by persons experiencing homelessness is a complex issue that may be limited by systematic challenges such as safety, privacy, and accessibility.4
Furthermore, molecular analysis of stools indicated presence of enteric pathogens, suggesting both that persons experiencing homelessness may be at relatively high risk of enteric infection and that there may be risks associated with exposure to discarded feces. An estimated 8.2% of the US population are infected annually with norovirus, 0.7% with Giardia, 0.5% with Salmonella, and 0.03% with enterotoxigenic E coli,11 though prevalence in stools outside clinical settings has not been characterized in a comparable population. Molecular analyses in this study did not capture viability or infectivity of enteric pathogens identified, so estimates of exposure risks are not possible from our data.
For persons experiencing homelessness, limited access to sanitation facilities and resource constraints at existing facilities may present challenges to maintaining dignity, health, and privacy4; these basic human needs are among the reasons sanitation has been declared a human right.12 Achieving universal sanitation access in the United States will require consideration of “invisible” populations whose needs are unmet and whose rights have not yet been realized.
HUMAN PARTICIPANT PROTECTION
Human participant protection was not required because no human participants were involved in this study.
REFERENCES
- 1.Prüss-Üstün A, Bos R, Gore F, Bartram J. Safer water, better health. Geneva, Switzerland: World Health Organization; 2008. p. 53. [Google Scholar]
- 2.Henry M, Watt R, Rosenthal L, Shivji A. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. US Department of Housing and Urban Development. 2016. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed January 26, 2018.
- 3. 2016 Homeless Point-in-Time Count. Atlanta, GA: Partners for Home; 2016.
- 4.Leibler JH, Nguyen DD. Personal hygiene practices among urban homeless. Int J Environ Res Public Health. 2017;14(8):pii:E928. doi: 10.3390/ijerph14080928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stanwell-Smith R. Public toilets down the drain? Why privies are a public health concern. Public Health. 2010;124(11):613–616. doi: 10.1016/j.puhe.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Saelinger D. Nowhere to go: the impacts of city ordinances criminalizing homelessness. Georgetown J Poverty Law Policy. 2006;13(3):545–566. [Google Scholar]
- 7.Kushel M. Hepatitis A outbreak in California—addressing the root cause. N Engl J Med. 2018;378(3):211–213. doi: 10.1056/NEJMp1714134. [DOI] [PubMed] [Google Scholar]
- 8.Albert MJ, Rotimi VO, Iqbal J, Chehadeh W. Evaluation of the xTAG gastrointestinal pathogen panel assay for the detection of enteric pathogens in Kuwait. Med Princ Pract. 2016;25(5):472–476. doi: 10.1159/000447698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose C, Parker A, Jefferson B, Cartmell E. The characterization of feces and urine: a review of the literature to inform advanced treatment technology. Crit Rev Environ Sci Technol. 2015;45(17):1827–1879. doi: 10.1080/10643389.2014.1000761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Global Health Observatory Data Repository. Open defecation: data by country. 2015. Available at: http://apps.who.int/gho/data/node.main.WSHOPENDEFECATION?lang=en. Accessed January 26, 2018.
- 11.Mead PS, Slutsker L, Dietz V et al. Food-related illness and death in the United States. Emerg Infect Dis. 1999;5(5):607–625. doi: 10.3201/eid0505.990502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United Nations General Assembly. 64/292. The Human Right to Water and Sanitation. 2010:9–11. Available at: http://www.un.org/es/comun/docs/?symbol=A/RES/64/292&lang=E. Accessed June 18, 2018.