Abstract
Objectives. To determine the extent to which opioid prescribing rates vary across US congressional districts.
Methods. In an observational cross-sectional framework using secondary data, we constructed 2016 congressional district–level opioid prescribing rate estimates using a population-weighted methodology.
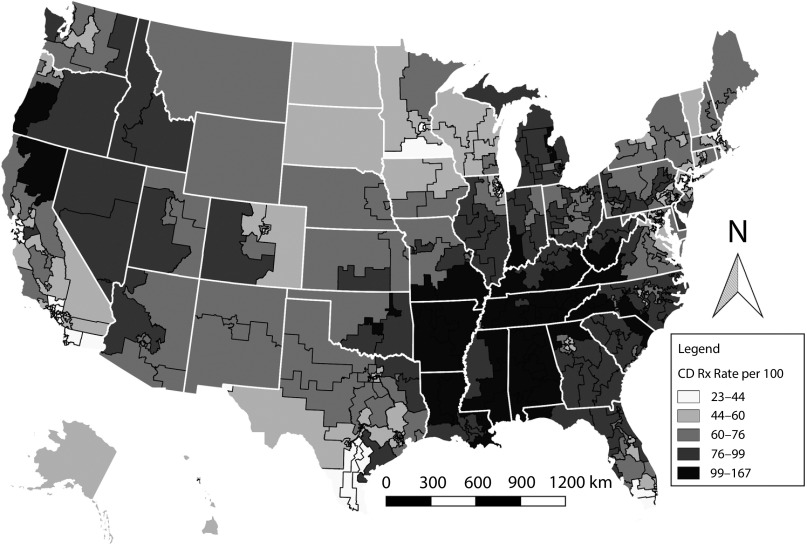
Results. High prescribing rate districts were concentrated in the South, Appalachia, and the rural West. Low-rate districts were concentrated in urban centers.
Conclusions. In the midst of an opioid overdose crisis, we identified congressional districts of particular concern for opioid prescription saturation.
Public Health Implications. The congressional district geography represents a policy-relevant boundary and a politically important level at which to monitor the crisis and determine program funding. Furthermore, in the context of the opioid crisis, knowing how congressional districts rank across the country and in states is useful in the creation of policies targeted to areas in need.
On October 26, 2017, the president of the United States officially declared the opioid epidemic a “public health emergency.” According to the Centers for Disease Control and Prevention (CDC), prescription opioid–related overdose deaths have quadrupled between 1999 and 2010.1 This large increase was matched by the quadrupling of the number of opioid prescriptions in the United States during that same period. From 2006 to 2010, opioid prescribing rates increased from 72.4 to 81.2 prescriptions per 100 persons. This rate remained constant from 2010 to 2012 and decreased to 70.6 from 2012 to 2015.1 The link between prescribing rates and overdose deaths appears to be directly related to maximum prescribed daily doses and not to regularly scheduled and as-needed doses.2,3 Thus, in understanding the nature of opioid overdose risk, it is necessary to understand how saturated a particular area is with prescription opioids.
More efficient monitoring and the development of policy that targets opioid-related mortality can be aided by knowing the geographic distribution of the opioid crisis.
Data on US opioid prescribing rates are available at the national, state, and county levels. In recent years, county- and state-level analysis has been the focus of many public health studies.1,4–6 This work has been important for characterizing wide discrepancies in opioid prescribing rates and overdose mortality rates within states and finding associations with White populations, rural areas, and Medicaid enrollment, among other variables.1 State-level analysis provides an explicit geographic link to state and federal government representation.7 We focused on congressional districts to analyze opioid prescribing rate data in states and capture a population that is represented by elected officials at a level higher than the municipality.
The congressional district in the United States is “a territorial division of a state from which a member of the U.S. House of Representatives is elected.”8 Districts tend to be of similar population size; as of the 2010 Census reapportionment, congressional districts have 710 767 people on average.9 This geography is a policy-relevant boundary and a politically important level at which to monitor the crisis and determine program funding. Using our analysis, policymakers can understand how their districts are faring relative to other districts across the country and within their state using a single measure instead of using several different county measures. In the context of the opioid crisis, knowing how congressional districts rank across the country and within states is useful in the creation of policies targeted to areas in need. Furthermore, previous literature has shown that the administrative level of the county may not be an appropriate primary unit of analysis, especially when developing policy and implementing programs that do not operate at the administrative level of the county.10 Even with the clear connection between geography and political representation, relatively few studies on health indicators perform analysis at this level, with some notable exceptions.11,12
Although previous literature has focused on the county, leaders in Congress are typically more familiar and concerned with constituents in their own districts, which are often composed of many different counties and portions of counties. Thus, there is value in constructing district-level rates that incorporate the spatial relationship between districts and counties. The aggregation of county-level opioid prescribing rates may accurately capture congressional district–level prescribing rates when counties are fully nested in districts; however, this is only the case for 16 districts out of 436. The spatial relationship between county and congressional district boundaries for the remaining districts varies a great deal. Fifty-six urban districts are each entirely contained in a single large county, and the remaining districts contain portions of multiple counties. When only portions of counties lie in a district, it is not a simple exercise to appropriate county rates to the congressional district, as these portions may be quite irregular in size and shape because of the overall gerrymandering of a district.
Complicating matters further is the degree to which a district’s boundaries have been drawn along racial or political lines (racial or political gerrymandering). This has the potential to distort the relationship between the demographics of the congressional district and the intersecting county-level opioid prescribing rates that are associated with county average demographics. Although we do not explicitly present a solution for the potential demographic distortions created by heavily gerrymandered districts, we do propose a possible methodology in the Discussion section.
We analyzed congressional district–level variation in opioid prescribing rates both between and within states by creating estimates based on a population-weighting methodology. Our study design was a cross-sectional observational analysis of secondary data.
METHODS
We obtained county-level opioid prescribing rates data from the QuintilesIMS Transactional Data Warehouse via the CDC.13 QuintilesIMS tracks all prescribing patterns nationally to provide accurate data for economic and statistical analysis. We focused on 2016 prescribing rates that are measured per 100 people. We identified opioid prescriptions using the National Drug Code and included Butrans (buprenorphine), codeine, fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, propoxyphene, tapentadol, and tramadol.
The construction of congressional district–level opioid prescribing rate estimates requires census block population data from the US Census Bureau’s 2010 decennial census. We retrieved this data set from the National Historical Geographic Information System (NHGIS), which provides high-quality demographic, economic, agricultural, and housing information at various spatial scales dating back to the first census in 1790.14 To estimate the congressional district prescribing rates from the county rates, we used a population-weighting method.11,12 This approach identifies an intermediary geographic level that nests both to the source zone (county) and the target zone (congressional district) and is conceptually similar to a dasymetric approach. A dasymetric approach is a method that accounts for the underlying population distribution when calculating rates for an area.15 Because census blocks nest into both counties and congressional districts, they provide the optimal cross between the 2 and do not require additional areal weighting techniques. Specific steps taken are as follows. First, we assigned county rates to block rates in an unweighted manner. Next, we summed the collection of block-level rates in a particular district using census block to congressional district population weights where we calculated the congressional district population as the population sum of the contained census blocks.
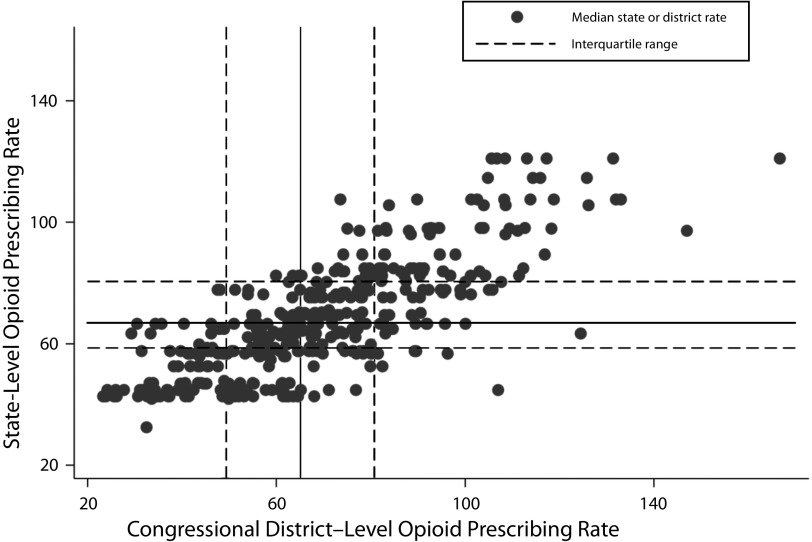
We performed the initial analysis of opioid prescribing rates with descriptive statistics across all congressional districts nationally and within each state. A boxplot is provided for visual interpretation of the national distribution rates. Congressional districts with the top 10 and bottom 10 rates are presented for discussion along with the ranking of state-level congressional district prescribing rate means. To identify congressional district prescribing rate outliers with respect to own-state prescribing rate distributions across districts, we identified high-rate districts in high-rate states, high-rate districts in low-rate states, low-rate districts in high-rate states, and low-rate districts in low-rate states. We did this by plotting congressional district rates against their state rates. We identified the various categories of district to state pairings as the points that lie outside the interquartile ranges of both district and state opioid prescribing rates.
To complement the descriptive statistics, a choropleth map is presented using national, state, and congressional district shapefiles available online through NHGIS.16 The map highlights the variability of opioid prescribing rates both between and within states. Prescribing rates per 100 persons are categorized by quantiles for each district. Quantiles classify the data such that each category has an equal number of observations (i.e., an equal number of congressional districts).
Quantiles have been identified in previous research as the most appropriate classification scheme when presenting epidemiological rate data.17
RESULTS
The 2016 mean and median rates for opioid prescriptions per 100 people across all congressional districts were 66.96 and 65.14, respectively, with a range of 23.30 to 166.69 (Table A available as a supplement to the online version of this article at http://www.ajph.org). Districts with the 10 highest rates were overwhelmingly contained in the Southeastern states, whereas districts with the 10 lowest rates were entirely contained in California, New York City, and Virginia (Table 1). Interestingly, the state of Virginia contained both a top and bottom 10 prescribing rate district. However, these extremes within the state may be expected, as the low-rate district contains Arlington County, which is near Washington, DC, whereas the high-rate district covers the far western part of the state along the border with West Virginia.
TABLE 1—
Top 10 and Bottom 10 Opioid Prescribing Rates by Congressional District: United States, 2016
| Rank | State | Congressional District | Opioid Prescribing Rate per 100 |
| 1 | Alabama | 4 | 166.69 |
| 2 | Kentucky | 5 | 147.00 |
| 3 | Tennessee | 3 | 133.00 |
| 4 | Tennessee | 1 | 131.95 |
| 5 | Alabama | 1 | 131.35 |
| 6 | Mississippi | 4 | 126.14 |
| 7 | Arkansas | 1 | 125.79 |
| 8 | Virginia | 9 | 124.49 |
| 9 | Tennessee | 6 | 118.79 |
| 10 | Oklahoma | 1 | 118.28 |
| 427 | Virginia | 8 | 29.29 |
| 428 | California | 18 | 27.73 |
| 429 | New York | 14 | 26.16 |
| 430 | California | 17 | 25.96 |
| 431 | New York | 5 | 25.83 |
| 432 | New York | 7 | 25.58 |
| 433 | California | 19 | 24.20 |
| 434 | New York | 6 | 23.90 |
| 435 | New York | 8 | 23.34 |
| 436 | New York | 9 | 23.30 |
Note. Table G (available as a supplement to the online version of this article at http://www.ajph.org) provides a full ranking of all congressional districts.
Of the top 10 rates shown in Table 1, Alabama’s 4th district, Kentucky’s 5th district, Tennessee’s 1st and 3rd districts, and Alabama’s 1st district were outliers with respect to the overall distribution of prescribing rates (Figure A, available as a supplement to the online version of this article at http://www.ajph.org, contains a boxplot). There were no outliers at the lower end of the distribution. The interquartile range was relatively narrow compared with the minimum and maximum values, running from 49.40 to 80.80.
With respect to geographic patterns of prescribing rates across congressional districts (Figure 1), there was a concentration of high prescribing rates throughout the South and along Appalachia. These areas have been highlighted as the most at-risk regions in terms of opioid-related mortality.4 Eastern Arizona, northern California, and Nevada along with the more rural portions of the states of Oregon and Washington had relatively high levels of opioid prescribing rates. Major urban districts like San Francisco and Los Angeles, California; Chicago, Illinois; Atlanta, Georgia; New York City; and Boston, Massachusetts, displayed rates well below the average. These spatial patterns represent the relationship between prescribing rates and the spatial sorting patterns of individuals and households with socioeconomic characteristics that directly correlate to opioid prescribing rates. However, several rural areas of the country, including the Texas border counties, northern Wisconsin, and the Dakotas, had prescribing rates well below the national average. For example, there was a stark contrast between the prescribing rates in northern Wisconsin and the upper peninsula of Michigan, suggesting a possible difference in state policy regarding opioid prescriptions.
FIGURE 1—
Map of Congressional District Opioid Prescribing (Rx) Rates (Quantiles): United States, 2016
Note. CD = congressional district.
State vs Congressional District Analysis
States that contained congressional districts with the highest 10 prescribing rates also contained some of the highest state congressional district rate averages, with the exception of Virginia (Table B). Louisiana, West Virginia, South Carolina, and Michigan had high congressional district averages but did not contain districts with rates in the top 10. An examination of actual state rates (not district rates averaged at the state level) using the previously defined high–high, high–low, low–high, and low–low categories once again highlighted the Southeastern hotspot. High–high districts contained district rates above the third quartile of 80.80 and state rates above the third quartile of 80.55 (Figure 2). These districts were predominately in the South, with the exception of Michigan and Indiana (Tables C–E, available as a supplement to the online version of this article at http://www.ajph.org, list all congressional districts in each outlier quadrant). Low–low districts contained district rates below the first quartile of 49.4 and state rates below the first quartile of 58.65. The majority of low–low districts were contained in New York City and the Los Angeles area. Although there were no districts with low rates in high-rate states, 6 districts with high rates in low-rate states were identified; namely, the 12th and 13th districts of Illinois, the 1st district of New Jersey, the 1st and 4th districts of Texas, and the 1st district of California.
FIGURE 2—
State vs Congressional District Opioid Prescribing Rates: United States, 2016
Sensitivity Analysis
We tested the accuracy of the population-weighted methodology by constructing congressional district estimates of a related socioeconomic characteristic that is observed at both the county and the congressional district levels. Specifically, we applied the population-weighting methodology to construct congressional district–level estimates and then compared these estimates to actual observed values. We selected White population proportion as the comparable socioeconomic characteristic because of its correlation with opioid prescribing rates.1,3,4 We retrieved White proportion at the county and congressional district levels from the 2011 through 2015 American Community Survey.16 Summary statistics of the actual proportions versus estimated proportions showed high similarity in the mean and maximum (Table F, available as a supplement to the online version of this article at http://www.ajph.org). However, the estimated proportions displayed a lower SD and larger minimum value, resulting in a slightly lower median value than the true median.
To assess variation in estimation strength that might occur as a result of how completely counties are nested in the congressional districts, we calculated fit statistics on the basis of nesting degree quartiles. Specifically, for each county intersecting with a congressional district, we calculated the county population proportion that is contained in the congressional district on the basis of census block population counts. We equated the degree of nesting for a particular congressional district to the mean of the contained population proportions of all counties intersecting with the district. Perfect nesting (mean = 1), districts that contain only full counties, produced perfect estimates, which we expected. We did not include these districts in the calculation of nesting degree quartiles. We calculated a root mean square error (RMSE) for each nesting degree quartile. The 25th, 50th, and 75th percentiles for nesting degree were 0.43, 0.75, and 0.93, respectively. Estimation accuracy increased as the degree of nesting increased.
The poorest performing estimates came from districts in the first quartile (RMSE = 0.1523). These districts tend to be densely populated urban areas, with many of these districts contained in a much larger single county. The second quartile estimates produced a RMSE of 0.079, which is nearly one half the size of the first quartile RMSE. The accuracy of the estimates improved further for the third and fourth quartile (RMSEs of 0.037 and 0.007, respectively). We plotted actual versus estimated proportions by degree of nesting for an additional visual interpretation of the sensitivity analysis (Figure 3). With the exception of first quartile, all quartiles display good to excellent visual clustering around the 45-degree line. These findings were robust across various other socioeconomic variables that are related to opioid prescribing rates, including poverty rate and proportion of college graduates.
FIGURE 3—
Congressional District (CD) White Population Proportion Estimate vs Actual by County Nesting Degree: United States, 2016
Note. Q = quartile. We equated the degree of nesting for a particular CD to the mean of the contained population proportions of all counties intersecting with the district. Low nesting degree implies that only small portions of counties (or a single county) are contained in a district. High nesting degree implies that an overall large proportion of intersecting counties are contained in the district. Districts containing perfectly nested counties are not included.
DISCUSSION
The United States experienced a declining life expectancy for a second straight year in 2016.18 Increasing age-specific death rates among those aged 15 to 44 years are attributable to increases in unintentional injuries that are largely driven by opioid overdose mortality.18 In 2016, 42 200 deaths were attributed to opioids,19 which is staggering by itself but may even be a vast underestimate.20 However, beyond the toll on American lives, the opioid epidemic bears large economic costs. The opioid epidemic was estimated to cost the United States $78.5 billion in 2013, with about a third going to increased health care and treatment costs.21 With these alarming facts in mind, understanding the opioid epidemic at policy-relevant geographies is important.
To the best of our knowledge, this is the first study to focus on congressional district–level opioid prescribing rates. We have identified the following salient findings. First, at-risk districts were concentrated in the Southeastern states with clear rural versus urban variation. Although these geographical patterns have been previously identified in county-level analysis, our contribution here is in the identification of additional variation between district and state rates and in the creation of congressional district rankings. Second, we identified how our population-weighting technique was affected by the spatial relationship between congressional districts and counties.
Variation in opioid prescribing rates both across and within states has potential policy implications, especially in terms of identifying which level of government should monitor prescribing rates and develop policies. Members of Congress are most concerned about the issues directly affecting their own constituents. By knowing opioid prescribing rates by congressional district, instead of at the state level, which may be very different, representatives may be able to advocate more strongly for federal policy. Additionally, county-level rates provide members of Congress important information on how rates vary within a state at a relatively small geography. However, because of the spatial relationship between a member’s district and intersecting counties, the county rates may provide a poor approximation for the district rate. We took a first step in estimating congressional district–level opioid prescribing rates and in identifying locations of variability, but we did not isolate the contributing components.
Variability between congressional district opioid prescribing rates can be generated in 3 ways. First, rates may depend on socioeconomic composition in a district. Second, variation in rates may be endogenously generated because people may demand more in certain areas for reasons the researcher does not observe. Third, rates may vary as a result of deliberate policy actions or a lack of action, which may influence prescribing rates over time. Disentangling these 3 sources is of priority for future research. With this knowledge, we would increase our ability to learn why certain districts are more successful in achieving more appropriate opioid prescribing rates.
Our analysis was limited in the following ways. On the basis of the sensitivity analysis using White population proportion, our population-weighting methodology proved reasonably robust for most congressional districts. However, for districts that exhibit low levels of nesting with counties, that is, contain only small portions of counties, the estimation was poor. These districts tend to contain dense urban geographies with average socioeconomic characteristics that deviate from the averages for counties with which they intersect. In this setting, population weighting does not accurately capture the underlying variation. Future research will seek to develop weighting methods that consider socioeconomic variables, such as poverty, race, and population density, that are associated with opioid prescribing rates.1,3,4 Specifically, census block socioeconomic variables can potentially be used to adjust the population weighting up or down. The development of this methodology will also address traditional concerns with population-weighting techniques, namely that the source zone (county) data are distributed down to the geographic intermediary (census blocks) in a uniform manner.
There are 3 caveats related to the data we used. First, census block data are available for 2010; however, the opioid prescription rate data are from 2016. Thus, we constructed population weights on the basis of 2010 census block and congressional district population ratios.
Second, opioid prescribing rate data were missing for 180 counties. In these instances, population weights were constructed with respect to the total number of census blocks in a district that contained county-level prescribing rate data. The impact of the missing rate data on the estimation was assumed to be minimal because missing counties contain very small proportions of congressional district total populations. The average district population proportion associated with a missing county was 0.01. The singular congressional district of Alaska was an outlier, where 0.12 of its population was contained in counties with missing opioid prescribing rate data. The estimated congressional district prescribing rate should be interpreted with caution here.
Lastly, the modifiable areal unit problem is a potential issue because 3 different scales were used within our analyses: census block, county, and congressional district. Had we selected a different set of scales, results may have varied. However, we chose to use the finest resolutions possible to preserve the greatest amount of information in the data. Furthermore, we were restricted by the need to find a spatial unit that nests both within counties and congressional districts. This is true only for census blocks.
In summary, our results emphasize the value in analyzing health and clinical outcomes at the congressional district level. In the opioid crisis context, a major driver has been prescription opioid abuse, and it is important to understand the amount of saturation in particular congressional districts to drive both federal and local policy efforts. Our results indicate areas of priority for reducing prescription opioid saturation, particularly in the Southeast.
ACKNOWLEDGMENTS
We thank the editor and anonymous reviewers for their helpful comments and suggestions; the article benefited greatly from the review process.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary as data were obtained from secondary sources.
Footnotes
See also Wykoff et al., p. 1124.
REFERENCES
- 1.Centers for Disease Control and Prevention. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. doi: 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunn KM, Saunders KW, Rutter CM et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohnert AS, Valenstein M, Bair MJ et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 4.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13(10):988–996. doi: 10.1016/j.jpain.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caines K, Shoff C, Bott DM, Pines JM. County-level variation in emergency department admission rates among US Medicare beneficiaries. Ann Emerg Med. 2016;68(4):456–460. doi: 10.1016/j.annemergmed.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Koh K, Grady SC, Darden JT, Vojnovic I. Adult obesity prevalence at the county level in the United States, 2000–2010: downscaling public health survey data using a spatial microsimulation approach. Spat Spatiotemporal Epidemiol. doi: 10.1016/j.sste.2017.10.001. In press. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 8.Congressional district. Merriam-Webster. 2018. Available at: https://www.merriam-webster.com/dictionary/congressional%20district. Accessed April 10, 2018.
- 9.Burnett KD. Congressional Apportionment: 2010 Census Briefs. Suitland, MD: US Census Bureau; 2011. [Google Scholar]
- 10.Kim R, Subramanian SV. What’s wrong with understanding variation using a single-geographic scale? A multilevel geographic assessment of life expectancy in the United States. Procedia Environ Sci. 2016;36:4–11. [Google Scholar]
- 11.Hao Y, Ward EM, Jemal A, Pickle LW, Thun MJ. US congressional district cancer death rates. Int J Health Geogr. 2006;5(1):28. doi: 10.1186/1476-072X-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson JL, Mansfield CJ. Disease, death, and the body politic: an areal interpolation example for political epidemiology. Int J Appl Geospat Res. 2010;1(3):49–68. [Google Scholar]
- 13.Centers for Disease Control and Prevention. U.S. county prescribing rates. 2016:2017. Available at: https://www.cdc.gov/drugoverdose/maps/rxcounty2016.html. Accessed November 18, 2017. [Google Scholar]
- 14.Manson S, Schroeder J, Van Riper D, Ruggles S. IPUMS National Historical Geographic Information System. Minneapolis: University of Minnesota; 2017. Version 12.0 [2010 Decennial Census] [Google Scholar]
- 15.Eicher CL, Brewer CA. Dasymetric mapping and areal interpolation: implementation and evaluation. Cartogr Geogr Inf Sci. 2001;28(2):125–138. [Google Scholar]
- 16.Manson S, Schroeder J, Van Riper D, Ruggles S. IPUMS National Historical Geographic Information System. Minneapolis, MN: University of Minnesota; 2017. Version 12.0 [2011–2015 American Community Survey 5-Year Estimate] [Google Scholar]
- 17.Brewer CA, Pickle L. Evaluation of methods for classifying epidemiological data on choropleth maps in series. Ann Assoc Am Geogr. 2002;92(4):662–681. [Google Scholar]
- 18.Kochanek K, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. Hyattsville, MD: National Center for Health Statistics; 2017. NCHS data brief no. 293. [PubMed] [Google Scholar]
- 19.Hedegaard H, Warner M, Miniño A. Drug Overdose Deaths in the United States, 1999–2016. Hyattsville, MD: National Center for Health Statistics; 2017. NCHS data brief no. 294. [PubMed] [Google Scholar]
- 20.Bernstein L, Ingraham C. Fueled by drug crisis, US life expectancy declines for a second straight year. 2017. Available at: https://www.washingtonpost.com/national/health-science/fueled-by-drug-crisis-us-life-expectancy-declines-for-a-second-straight-year/2017/12/20/2e3f8dea-e596-11e7-ab50-621fe0588340_story.html?utm_term=.94d18c42fe89. Accessed December 21, 2017.
- 21.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–906. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]