Abstract
Objectives. To understand the role of the community environment on intergenerational continuity in adverse childhood experiences (ACEs) among a rural White sample.
Methods. Parents in 12 counties in rural Iowa reported retrospectively on their own ACEs in 1989. We measured their child’s ACEs retrospectively and prospectively across adolescence (n = 451 families). We measured structural and social process–related measures of community environment (i.e., community socioeconomic status, parents’ perception of community services, perceived community social cohesion, and neighborhood alcohol vendor density) on multiple occasions during the child’s adolescence.
Results. The 4 measures of community environment were all correlated with the child’s ACEs, but only alcohol vendor density predicted ACEs after inclusion of covariates. Intergenerational continuity in ACEs was moderated by both social cohesion (b = −0.11; SE = 0.04) and alcohol vendor density (b = −0.11; SE = 0.05).
Conclusions. Efforts to increase community social cohesion and manage alcohol vendor density may assist families in breaking the cycle of maltreatment across generations.
Childhood adversity, such as abuse, neglect, and environmental instability (collectively called adverse childhood experiences, or ACEs) has been associated with poorer physical health,1 poorer mental health,2 risky health behaviors,1 and decreased life potential.3 Abuse, neglect, and other adversities in childhood show intergenerational continuity (or similarity across parents and offspring)4; and their impact on health and well-being can reverberate across generations. Therefore, reducing or preventing ACEs could produce long-lasting benefits in both health and life potential across generations. This makes the prevention of ACEs of significant interest to the public health community.
Family functioning (i.e., maintaining a safe, stable, nurturing home environment) could be negatively affected by community risks, including low community socioeconomic status (SES),5 lack of neighborhood services,6 low social control or collective efficacy,7 and high density of alcohol vendors.8 Neighborhood conditions have been linked to multiple ACEs.9–12 Understanding the effects of community-level attributes on ACEs can highlight areas in which community-level prevention efforts may be most effective at reducing exposure to ACEs. Community effects on ACEs are rarely studied among rural samples, yet almost 1 of 5 children in the United States live in rural areas,13 and rural areas have fewer child abuse resources.14 We hypothesized that a supportive community environment would be associated with fewer ACEs among a rural sample. If community environment predicts ACE score among the second generation (G2) after accounting for the ACE score of their parents (G1), it would further support the hypothesized protective role of the community context in reducing ACEs.
Factors that increase or decrease intergenerational continuity in ACEs are unknown. A supportive community environment may change the magnitude of intergenerational continuity in ACEs. Such moderating effects of community characteristics have not been previously tested on intergenerational continuity in family functioning, nor on ACEs. However, community characteristics buffer the association between family risks (e.g., harsh parenting, maternal depression) and child behavior.15 We included measures of the community environment previously linked with family functioning: SES,5 neighborhood services,6 social cohesion,7 and alcohol vendor density.8 We hypothesized that these community characteristics would change the amount of (i.e., moderate) intergenerational continuity in ACEs.
METHODS
We recruited 451 two-parent families via telephone through the cohort of all seventh-grade students (aged 12–13 years) in 8 counties in north central Iowa who were enrolled in public or private schools during winter and spring of 1989. An additional criterion for inclusion in the study was the presence of a sibling within 4 years of age of the focal seventh grader. Seventy-seven percent of the eligible families agreed to participate in the study. We first conducted interviews in 1989 with adolescents (G2) and their parents (G1) when they were in seventh grade (mean age = 13 years; 51% girls). Participants lived in 91 US census block groups across 8 rural counties in north central Iowa and were all European Americans from primarily lower-middle– and middle-class families. We found no pronounced differences in demographic indicators (e.g., education, income) using US census data to compare this sample with the surrounding families, with a single exception. The inclusion criteria of the study required a sibling who was close in age to the focal adolescent, which resulted in a slightly larger average family size than that of families in the surrounding community. More detailed information about the initial recruitment and the families involved is available in Conger and Elder.16
Procedures
We recruited G2 youths and their G1 parents from public and private schools in rural areas of Iowa during the G2’s adolescent years. We sent letters explaining the project to eligible families, who we then contacted by telephone and asked to participate. Seventy-eight percent of the families agreed to be interviewed. During each assessment period, professional interviewers made home visits to each family for approximately 2 hours on 2 occasions. At each visit, father, mother, and adolescent independently completed a set of questionnaires in separate rooms covering an array of topics related to work, finances, school, family life, mental and physical health status, and social relationships. Assessments occurred when the adolescent was in 7th, 8th, 9th, 10th, and 12th grade, as well as a year later, when the adolescents averaged 18 years of age.
Measures
ACEs items included indicators of abuse (physical, sexual, emotional), emotional neglect, and other household challenges (parent treated violently by spouse, household substance abuse, household mental illness, and parental separation or divorce). Specific items included for each ACE are available from the first author (T. J. S.). We calculated an ACE score for each G1 parent and each G2 adolescent by summing the 8 ACE category variables that we assessed. G1 parents reported ACEs retrospectively in adulthood. G2 adolescents and both G1 parents reported ACEs retrospectively at the first assessment. Then all 3 reporters prospectively reported ACEs over time at later assessments (until the assessment at age 18 years).
We collected US census block group data (percentage of households on public assistance, percentage of residents older than 25 years who were unemployed, and percentage of households living below the poverty line) at each assessment and averaged them. We collected US census reports of block group population density at each assessment and averaged it.
Mothers and fathers both completed a 9-item scale assessing the degree to which there was a lack of social services (e.g., medical services, good schools, police and fire protection, successful businesses, and other educational, social, and medical services) in their area at 2 assessments. Parent reports were correlated at 0.45 and combined into a single scale (α = 0.79).
Mothers and fathers both reported at 2 of the assessments (eighth grade and ninth grade) on the “ability of community members to control the behavior of individuals in the community.”17(p920) Seven items addressed the residents’ respect for rules and laws, friendliness, and helpfulness; parents’ supervision of their children; absence of drugs and crime; and residents’ overall efforts to make the area a nice place to live. Parent reports were correlated at 0.32 and combined into a single scale (α = 0.68).
We defined alcohol vendor density as the number of onsite and offsite alcohol vendors (i.e., off sales, on sales, and both on and off sales) within 1 kilometer (0.62 miles) of the family’s residence (on the basis of network distance using Esri Business Analyst [Esri, Redlands, CA]). We estimated densities at each assessment and then averaged them (α = 0.86).
Mothers and fathers reported the degree to which they had problems related to their alcohol use (e.g., trouble getting work done, problems with family because of alcohol use, health problems and accidents, and feeling guilty or a need to reduce drinking) at 4 of the 5 assessments. We averaged mother and father alcohol responses across assessments into composite scales for each parent (α = 0.79 for fathers; α = 0.85 for mothers).
Mothers and fathers both completed the neuroticism scale from the Neuroticism–Extraversion–Openness Five Factor Inventory18 at the second assessment. We calculated family income to needs ratio from parent-reported information at each assessment. We averaged responses across assessments (α = 0.88).
Analyses
We operationalized intergenerational continuity as the magnitude of prediction from G1 ACE exposure to G2 ACE exposure. We first tested hypotheses separately for G1 mothers and G1 fathers, for G2 boys and G2 girls, and then we applied equality constraints and combined them across gender if the pattern of results was not significantly different. We tested each community attribute as a moderator of the association from G1 ACEs to G2 ACEs by centering G1 ACE score and the community attribute, then creating a product term between G1 ACEs and the community attribute, and then entering all 3 terms as predictors of G2 ACE exposure.
We first tested the main and moderating effects of each community attribute separately and then combined them into a single model. We included repeated measures of community characteristics taken throughout G2’s adolescence to produce an estimate of chronic or cumulative exposure to area characteristics.9 Missingness was less than 10% for all variables and was not related to any of the baseline variables in the model. We performed analyses on the basis of restricted maximum-likelihood estimation, with sandwich estimation of SEs to account for some families sharing the same blockgroup.19 Residents select into particular neighborhoods by preexisting traits,20 including personality.21
As a robustness check, we included parent neuroticism and alcohol problems as covariates because they show spatial autocorrelation,20,21 have been linked with ACEs in previous studies,22 and were significantly related to G2 ACEs in this sample. We also included parent income as a covariate. Because of the rural nature of this sample, we also controlled for population density. We did not employ sample weights.
RESULTS
Characteristics of the sample are presented in Table 1. The number of ACEs experienced by G1 parents (mean = 1.3; interquartile range [IQR] = 2) was positively associated with the number of ACEs experienced by G2 offspring (mean = 2.2; IQR = 2; r = 0.25). In raw units, a 1-point increase in G1 ACE exposure was associated with a 0.34 unit increase in G2 ACE exposure (P < .001). Although all measures of the neighborhood environment (except population density) were significantly correlated with the G2 ACE exposure, most were not significant once we included the G1 ACE score as a predictor of G2 ACE exposure. Preliminary analyses showed no difference in the pattern of results between G1 mother ACE exposure and G1 father ACE exposure, nor were the results moderated by G2 gender.
TABLE 1—
Characteristics of Study Sample in Rural Iowa: 1989–1994
| Characteristic | Mean (SD) or % |
| Maternal age, y | 37.70 (4.10) |
| Paternal age, y | 39.70 (4.90) |
| Maternal educational attainment | 13.40 (2.90) |
| Paternal educational attainment | 13.50 (2.10) |
| Family per capita income | 7.94 (5.65) |
| Parent alcohol problems (scale 1–4) | 4.24 (0.47) |
| Parent neuroticism (scale 1–5) | 2.58 (0.41) |
| Adolescent G1 mother | 6.0 |
| G2 major health problems as infant | 11.5 |
| G2 is a girl | 52.0 |
| G2 age, y | 13.20 (0.42) |
| G2 is White | 100.0 |
| Community characteristics (block group level) | |
| Low socioeconomic status | 6.42 (3.07) |
| Population density (people per mi2) | 227.93 (493.49) |
| Perceived lack of community services (scale 1–4) | 3.09 (0.29) |
| Perceived community social cohesion (scale 1–4) | 3.00 (0.27) |
| Alcohol vendor density (vendors per km2) | 4.13 (7.76) |
| No. ACEs | |
| G1 mother | 1.53 (1.79) |
| G1 father | 1.12 (1.42) |
| G2 adolescent | 2.21 (1.38) |
Note. ACEs = adverse childhood experiences; G1 = first generation; G2 = second generation. Sample size was n = 451. G1 ACE scores are not directly comparable with G2 ACE scores.
After accounting for G1 ACE score, community SES did not show a main or moderating effect on intergenerational continuity in ACE score. These results were the same whether community SES was the only community predictor or whether it was included along with the other community attributes. Higher perception of community services was associated with lower G2 ACE scores (b = −0.18; SE = 0.06; P < .01) although this main effect was not significant once the other community variables were added to the model. Perception of community resources did not change the amount of intergenerational continuity.
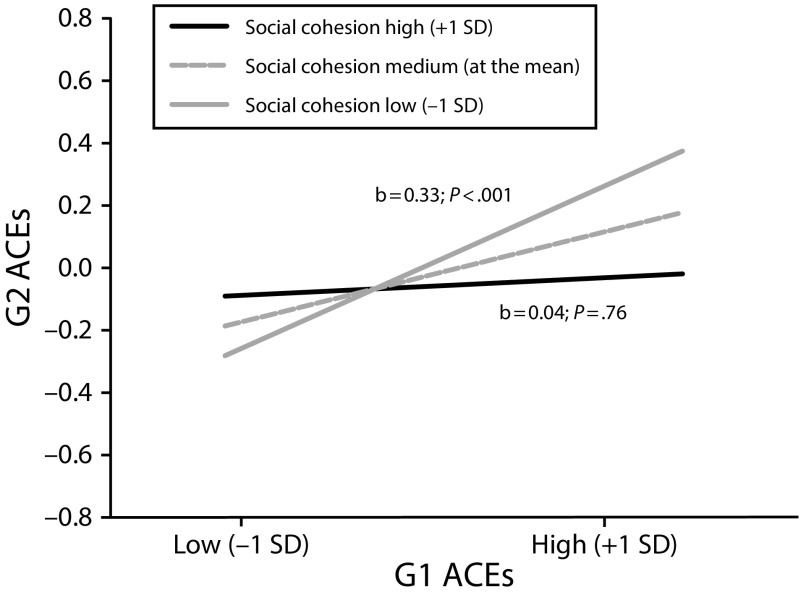
Perceived community social cohesion reduced the intergenerational continuity in ACEs (b = −0.14; SE = 0.06; P = .02). Among families living in communities with social cohesion 1 SD above the mean, the intergenerational continuity in ACEs was reduced to 0.04 (P = .76; Figure 1). The intergenerational continuity in ACE score was not statistically significant for families living in communities above the 60th percentile on social cohesion. This effect remained significant when we included the other community attributes as covariates.
FIGURE 1—
Moderation of Intergenerational Continuity in ACEs by Parents’ Perception of Community Social Cohesion Among Rural Iowa Families: 1989–1994
Note. ACEs = adverse childhood experiences; G1 = first generation; G2 = second generation.
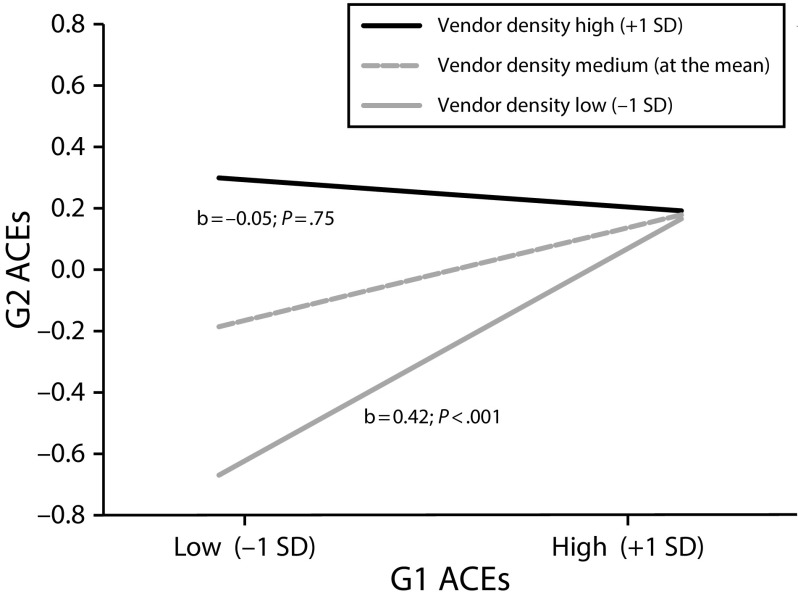
Alcohol vendor density reduced the intergenerational continuity in ACEs (b = −0.17; SE = 0.06; P < .01). G2 adolescents were likely to have a relatively higher ACE score if they resided in an area with a high density of alcohol vendors, regardless of whether their G1 parents had a relatively high ACE score (Figure 2). G2 adolescents tended to have low ACE scores (0–1 ACEs) only when they resided in an area with a low density of alcohol vendors and had parents who did not experience many ACEs themselves. The intergenerational continuity in ACEs was not statistically significant in communities rated below the 45th percentile on alcohol vendor density. This effect remained significant when we included the other community attributes as covariates.
FIGURE 2—
Moderation of Intergenerational Continuity in ACEs by Density of Alcohol Vendors Among Rural Iowa Families: 1989–1994
Note. ACEs = adverse childhood experiences; G1 = first generation; G2 = second generation.
These findings remained significant after we included parent neuroticism and parent alcohol problems as additional covariates.
DISCUSSION
Among these rural White families, children of parents who experienced ACEs were more likely to also experience ACEs. Such continuity across generations is consistent with other work on childhood abuse, neglect, and household challenges as well as the emerging literature on intergenerational continuity in ACEs.23 The mechanism behind such continuity and the degree to which this continuity is a causal effect of parent ACE exposure on offspring ACE exposure remain unknown. These questions must also be answered to adequately inform policies intended to reduce ACEs.
In these White, rural, lower SES communities, high perceived community social cohesion was associated with a reduction in ACEs across generations. This is consistent with cross-sectional work showing a negative correlation between collective efficacy and child maltreatment24 and points to the importance of social cohesion for health and well-being among rural populations. In addition, the moderation effect shows that social cohesion reduces intergenerational continuity in ACEs. These effects of community social cohesion on G2 ACEs remained after controlling for the G1 ACE score, income, personality, and alcohol problems. Interventions that increase neighborhood social cohesion may reduce ACE exposure and are likely to have the greatest impact on families in which the parents themselves had high ACE exposure as children.
The moderation of intergenerational continuity by alcohol outlet density did not conform to our expectation that high vendor density would exacerbate intergenerational continuity. The only adolescents who experienced relatively fewer ACEs were those who simultaneously lived in a low vendor density area and had parents who reported experiencing relatively fewer ACEs. In other words, this study found that either (1) high parent exposure to ACEs or (2) high alcohol vendor density was sufficient to put children at risk for exposure to adverse childhood experiences. Alcohol vendor density has been shown to correlate with several individual elements of the overall ACE score, including domestic violence,25 sexual assault,26 child abuse, and child neglect.27 Alcohol problems of the G1 parent did not account for the association between vendor density and G2 ACEs, supporting the interpretation of this finding as evidence for a community effect and not a selection effect.
Low neighborhood SES and lack of community services were both correlated with G2 ACEs, yet neither predicted G2 ACEs after accounting for G1 parents’ exposure to ACEs. This finding suggests that, among this rural sample, these community elements are not causes of ACEs and supports other work showing null effects for neighborhood SES after accounting for covariates.28 Efforts to reduce exposure to ACEs that focus on enhancing community SES or improving community services to rural residents may be less effective than are efforts to increase perceived social cohesion or reduce alcohol vendor density.
Limitations
These nonexperimental data cannot support strong causal inference. Although this rural sample showed variation in most neighborhood characteristics, it remains possible that other samples designed specifically to study high-risk neighborhoods could provide a different pattern of results. Any omission of personal characteristics that could have caused selection into communities and exposure to ACEs would result in a misspecified model, invalidating the observed results. These community characteristics may be markers of preexisting parent characteristics that affect intergenerational continuity in ACEs or drive selection into neighborhoods29 instead of causal moderators.
Children show different responses to the community environment across different ages,30 and shifting social mores may change how community factors relate to ACEs. Finally, although many models of behavior indicate that it is one’s perception of a stimulus (and not the stimulus itself) that creates a response,31 and this has been found in some studies of community effects,32,33 several of our measures of community resources and neighborhood structure were reported by parents (e.g., perceived social cohesion), which can conflate the objective reality of the community with the parents’ perception of the community.
Conclusions
Exposure to early adversity is associated with a host of health problems, interferes with successful relationship formation, and reduces productivity and success in the workplace. Exposure to these risk factors (collectively called ACEs) shows continuity across generations among families in this rural sample. However, that cycle may be disrupted in White, rural, lower SES communities when adolescents are living in a community with low alcohol vendor density or in a community that their parents characterize as high in social cohesion. If replicated, these findings suggest that efforts to foster social cohesion and limit the density of alcohol vendors may help families break the cycle of exposure to adverse experiences during childhood and adolescence.
ACKNOWLEDGMENTS
This study was funded in part by the National Institute of Mental Health (grant MH43270), the Centers for Disease Control and Prevention ([CDC] grant 200-2012-M-53706V), and the Iowa State University College of Human Sciences (internal grant).
The authors thank the project staff, participating families, and Rand Conger for his permission to access the data. We extend our gratitude to the many families who participated in these important research projects. These analyses could not have been conducted without their help and willingness to share their lives with study investigators.
Note. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
HUMAN PARTICIPANT PROTECTION
The Iowa State University institutional review board approved this study.
Footnotes
REFERENCES
- 1.Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- 3.Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: shifting the narrative. Child Youth Serv Rev. 2017;72:141–149. doi: 10.1016/j.childyouth.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 suppl):S32–S38. doi: 10.1016/j.jadohealth.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coulton CJ, Korbin JE, Su M. Neighborhoods and child maltreatment: a multi-level study. Child Abuse Negl. 1999;23(11):1019–1040. doi: 10.1016/s0145-2134(99)00076-9. [DOI] [PubMed] [Google Scholar]
- 6.Maguire-Jack K, Negash T. Parenting stress and child maltreatment: the buffering effect of neighborhood social service availability and accessibility. Child Youth Serv Rev. 2016;60:27–33. [Google Scholar]
- 7.Molnar BE, Goerge RM, Gilsanz P et al. Neighborhood-level social processes and substantiated cases of child maltreatment. Child Abuse Negl. 2016;51:41–53. doi: 10.1016/j.chiabu.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freisthler B, Maguire-Jack K. Understanding the interplay between neighborhood structural factors, social processes, and alcohol outlets on child physical abuse. Child Maltreat. 2015;20(4):268–277. doi: 10.1177/1077559515598000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuellar J, Jones DJ, Sterrett E. Examining parenting in the neighborhood context: a review. J Child Fam Stud. 2015;24(1):195–219. doi: 10.1007/s10826-013-9826-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Downey L, van Willigen M. Environmental stressors: the mental health impacts of living near industrial activity. J Health Soc Behav. 2005;46(3):289–305. doi: 10.1177/002214650504600306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spiker S, Sorrelgreen E, Williams J. Liquor Outlet Report: A Preliminary Analysis of the Relationship Between Off-Sale Liquor Outlets and Crime in Oakland for 2007. Oakland, CA: Urban Strategies Council; 2007. [Google Scholar]
- 12.Valentino K, Nuttall AK, Comas M, Borkowski JG, Akai CE. Intergenerational continuity of child abuse among adolescent mothers: authoritarian parenting, community violence, and race. Child Maltreat. 2012;17(2):172–181. doi: 10.1177/1077559511434945. [DOI] [PubMed] [Google Scholar]
- 13.US Census Bureau. B11001: household type (including living alone). 2007–2011 American Community Survey. Available at: http://factfinder2.census.gov. Accessed January 1, 2018.
- 14.Choo EK, Spiro DM, Lowe RA, Newgard CD, Hall MK, McConnell KJ. Rural–urban disparities in child abuse management resources in the emergency department. J Rural Health. 2010;26(4):361–365. doi: 10.1111/j.1748-0361.2010.00307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delany-Brumsey A, Mays VM, Cochran D. Does neighborhood social capital buffer the effects of maternal depression on adolescent behavior problems? Am J Community Psychol. 2014;53(3–4):275–285. doi: 10.1007/s10464-014-9640-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conger RD, Elder GH. Families in Troubled Times: Adapting to Change in Rural America. Hawthorne, NY: Aldine de Gruyter; 1994. [Google Scholar]
- 17.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 18.Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 19.Muthén LK, Muthén BO. Mplus User’s Guide. 7th ed. Los Angeles: Muthén & Muthén; 2012. [Google Scholar]
- 20.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Jokela M, Bleidorn W, Lamb ME, Gosling SD, Rentfrow PJ. Geographically varying associations between personality and life satisfaction in the London metropolitan area. Proc Natl Acad Sci USA. 2015;112(3):725–730. doi: 10.1073/pnas.1415800112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spinhoven P, Elzinga BM, Van Hemert AM, de Rooij M, Penninx BW. Childhood maltreatment, maladaptive personality types and level and course of psychological distress: a six-year longitudinal study. J Affect Disord. 2016;191:100–108. doi: 10.1016/j.jad.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 23.Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry. 2016;87(1):3–14. doi: 10.1037/ort0000133. [DOI] [PubMed] [Google Scholar]
- 24.Emery CR, Tung HN, Wu S. Neighborhood informal social control and child maltreatment: a comparison of protective and punitive approaches. Child Abuse Negl. 2015;41:158–169. doi: 10.1016/j.chiabu.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Livingston M. Alcohol outlet density and harm: comparing the impacts on violence and chronic harms. Drug Alcohol Rev. 2011;30(5):515–523. doi: 10.1111/j.1465-3362.2010.00251.x. [DOI] [PubMed] [Google Scholar]
- 26.Abbey A. Alcohol’s role in sexual violence perpetration: theoretical explanations, existing evidence, and future direction. Drug Alcohol Rev. 2011;30(5):481–489. doi: 10.1111/j.1465-3362.2011.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freisthler B, Midanik LT, Gruenewald PJ. Alcohol outlets and child physical abuse and neglect: applying routine activities theory to the study of child maltreatment. J Stud Alcohol. 2004;65(5):586–592. doi: 10.15288/jsa.2004.65.586. [DOI] [PubMed] [Google Scholar]
- 28.Pinderhughes EE, Nix R, Foster EM, Jones D. Parenting in context: impact of neighborhood poverty, residential stability, public services, social networks, and danger on parental behaviors. J Marriage Fam. 2007;63(4):941–953. doi: 10.1111/j.1741-3737.2001.00941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schofield TJ, Merrick M, Chen CF. Reciprocal Associations Between Neighborhood Context and Parent Investments: Selection Effects in Two Longitudinal Samples. Princeton, NJ: Princeton University; 2016. Working Paper No. 16–08–ff.
- 30.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52(1):1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 32.Chung HL, Steinberg L. Relations between neighborhood factors, parenting behaviors, peer deviance, and delinquency among serious juvenile offenders. Dev Psychol. 2006;42(2):319–331. doi: 10.1037/0012-1649.42.2.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schofield TJ, Conger RD, Conger KJ. Neighborhood disorder and children’s antisocial behavior: the protective effect of family support among Mexican American and African American families. Am J Community Psychol. 2012;50(1–2):101–113. doi: 10.1007/s10464-011-9481-7. [DOI] [PMC free article] [PubMed] [Google Scholar]