Abstract
Background:
Optimal patient selection is key to success of operative treatment for cuff tears. We assessed predictors of pain and functional outcomes in a longitudinal cohort of patients undergoing operative treatment.
Methods:
From 03/2011 to 01/2015, a cohort of patients with rotator cuff tears undergoing rotator cuff surgery was recruited. Patients completed a detailed health and demographic questionnaire, standardized shoulder questionnaires including the Shoulder Pain and Disability Index (SPADI), and underwent a MRI. Patients received follow-up questionnaires at 3, 6, 12, and 18 months. We assessed longitudinal predictors of SPADI using longitudinal mixed models. Interactions with follow-up duration after surgery were also assessed.
Results:
In our analysis (n=50), a lower fear-avoidance beliefs questionnaire physical activity score (FABQ; p=0.001) predicted a lower SPADI score (better shoulder pain and function). Those consuming alcohol 1–2 times per week or more had lower SPADI scores as compared with those consuming alcohol 2–3 times per month or less (p=0.017). Both of these variables had a significant interaction with duration of follow-up. Other variables including socio-demographic characteristics, MRI characteristics such as tear size and muscle quality, shoulder strength, and variations in surgical techniques/performance of adjuvant surgical procedures were not significant predictors of SPADI.
Conclusions:
Those with higher fear avoidance behavior and alcohol use of 1–2 times/week had worse shoulder pain and function at 18 months of follow-up. These data can be used to select optimal candidates for operative treatment of rotator cuff tears and assist with patient education and expectations prior to treatment.
Level of Evidence:
Level II; Prospective Cohort Design; Treatment Study
Keywords: Rotator cuff, surgery, predictors, outcomes, SPADI, shoulder pain, cohort
INTRODUCTION
An estimated 272,148 rotator cuff repairs were performed on an ambulatory basis in the United States in 20066, 14 There has been an increase in surgery as the initial treatment for rotator cuff tears over time30. Optimal outcomes of operative treatment for rotator cuff tears are achieved by patient selection based on characteristics that predict better pain and functional outcomes after surgery. Few studies have analyzed a limited number of factors associated with better outcomes after operative treatment3,5,8,12,18,19,21–23,26–28. A comprehensive longitudinal analysis of possible predictors of better outcomes after operative treatment in a well-defined multi-center cohort is lacking as per our assessment.
In a longitudinal multi-center cohort of patients with rotator cuff tears, we assessed predictors of better shoulder pain and function after surgery. This information can be used to guide clinicians and patients in identifying optimal candidates for surgical treatment of rotator cuff tears.
MATERIALS AND METHODS
Patient Population
Between 03/2011 and 01/2015, the Rotator Cuff Outcomes Workgroup (ROW) cohort study recruited patients 45 years and older with symptomatic (for at least 4 weeks) rotator cuff tears undergoing operative treatment. Patients were recruited from Sports/Shoulder clinics in 3 academic and 1 community setting. Exclusion criteria were a current shoulder fracture, prior shoulder surgery (on the index shoulder), and active cervical radiculopathy (elicited as neck pain radiating to shoulder/arm/hand). Patients provided informed consent and the study was approved by our Institutional Review Boards. Although this analysis was performed in patients undergoing rotator cuff surgery, the entire ROW cohort recruited patients with and without tears and also those undergoing operative and non-operative treatments.
Structured History Questionnaire and Outcome Measures
A history questionnaire and outcome questionnaires were administered to each patient at each time point. The history questionnaire was abbreviated for follow-up. The history questionnaire elicited comprehensive and structured information on patient demographics, comorbidities, symptoms, smoking/alcohol habits, and patient expectations from treatment. Performance of manual labor on a daily basis in the patient’s current job or last job (if retired) was also asked. The physical activity scale of the Fear-Avoidance and Beliefs questionnaire (FABQ) was designed by Waddell et al31 to assess fear-avoidance beliefs about physical activity in patients with low back pain. We modified the FABQ physical activity questions (4 items that contribute towards scoring) in this scale by using the term “shoulder” instead of “back”. The scale has 24 possible points with a higher score indicating worse fear-avoidance behavior with physical activity in relation to the shoulder. Mental health was assessed using the Mental Health Inventory (MHI-5)2, a component of the 36-item Short Form Health Survey32. MHI-5 scores range from 0 to 100. A score of ≤68 on the MHI-5 is indicative of a probable mood disorder (including depression)17,29.
Shoulder outcomes were assessed using the Shoulder Pain and Disability Index (SPADI)24, a standardized 13-item questionnaire. SPADI has a pain scale (5 items) and a disability scale (8 items). SPADI scores range from 0 to 100 with lower scores reflecting better shoulder pain and function.
Strength Testing
Strength testing was performed using a hand-held dynamometer in abduction, external rotation, and internal rotation by trained research assistants. Both the affected and contralateral shoulders were assessed and a mean of two consecutive measurements that were at least 10 seconds apart was used in our analysis. Our detailed protocol for standardized strength testing has been previously described15, 20. Strength testing using a dynamometer has good intra-rater and inter-rater reliability11. We used a ratio of the affected shoulder versus the contralateral shoulder strength in the analysis.
Surgical Characteristics
A surgery report form was used to determine whether a biceps tenodesis or tenotomy was performed and the technique used when performing the rotator cuff repair. The technique was classified into single row, double row, and other (open repair or transosseous equivalent). The surgery report form was completed by the attending surgeon.
Diagnostic Imaging
Shoulder MRI images were read in a blinded fashion by consensus by two shoulder experts (L.D.H. and N.B.J., or J.E.K. and N.B.J.). Our previous work has shown good inter-rater and intra-rater reliability for these MRI readings as compared with a reading by a musculoskeletal radiologist13. Kappa values ranged from 0.75 to 0.90 for tear presence, tear size, and tear thickness13. MRI features including tear thickness, tear size in longitudinal and transverse planes, fatty infiltration of the rotator cuff muscles, tendon retraction, and rotator cuff muscle atrophy were assessed. Criteria for each of these measurements follows standard nomenclature and has been previously described13.
Diagnosis of Rotator Cuff Tear
Rotator cuff tears were diagnosed based on the clinical impression of a sports/shoulder fellowship trained attending physician and evidence of structural deficit on MRI. Biceps tendon pathology was diagnosed based on the clinician’s impression since imaging can be negative even if the patient has symptoms corresponding to biceps pathology or vice versa. A MRI was unavailable for 2 patients in the cohort.
Longitudinal Follow-Up
Patients were followed at approximately 3, 6, 12, and 18 months after completion of baseline visit. Patients were mailed follow-up questionnaires with a prestamped envelope. Patients received phone or email reminders if they did not return the questionnaires, and eventually a call from the study Principal Investigator if questionnaires were still not returned. All 50 patients had at least 1 follow-up from baseline. At 18 months 35 patients were available for analysis.
Statistical Analysis
Potential factors associated with treatment outcomes (SPADI) were assessed over 18 months of follow-up. Since variable effects can change over time, a total of 27 variables and their interactions with time were assessed. An a priori sample size calculation was not performed for this analysis. Variables included in our analysis were categorized into demographics, patient symptoms, comorbidities, personal habits, shoulder strength, and patient expectations. For partial-thickness tears, size of tear was given a value of 0 for the analysis since there is no accepted standard methodology to calculate size in partial-thickness tears. Race and patient expectations after treatment could not be used in the analysis due to very few patients in one of the categories. Prediction models were estimated using a linear mixed model incorporating an AR(1) covariance structure. Our statistical model uses all available follow-up time points (3, 6, 12, and 18 months) for a given patient. Resulting standard goodness-of-fit and residual analyses were unremarkable. The full model, including interactions regardless of statistical significance, was used to estimate least square mean differences between groups for significant variables for ease of clinical interpretation. Univariate p-values are presented for each variable based on the global test for the variable and interactions with time. If desired, the 26 univariate models can be interpreted, adjusting for multiplicity, by the reader using the Bonferroni p-value adjustment (0.05/26 = 0.0019).
RESULTS
There were 50 patients in the operative cohort who met the eligibility criteria for this analysis. A majority of patients undergoing surgery were male (62%; n=31; Table I). The mean age of patients having surgery was 59 years (Standard Deviation=9 years). Most patients were engaged in light or no manual labor for their current or last (in case of retirees or those not working) job (74%; n=37). An equal number of patients were never smokers or past/current smokers (n=24 in each group). Biceps pathology was diagnosed in 30% (n=15) of patients.
Table I:
Baseline Characteristics of Patients with Rotator Cuff Tears Having Surgery: The ROW Cohort (n=50)
| Characteristics | Percent of Patients* | (Number of Patients)** |
|---|---|---|
| Demographics | ||
| Sex | ||
| Female | 38% | (19) |
| Male | 62% | (31) |
| Age | 52 59 65 | (59 ± 9) |
| Race/Ethnicity | ||
| Non-Hispanic White | 92% | (46) |
| Other | 6% | (3) |
| Missing | 2% | (1) |
| Highest level of education | ||
| Less than college | 32% | (16) |
| College or above | 64% | (32) |
| Missing | 4% | (2) |
| Marital Status | ||
| Single/Divorced/Widowed | 22% | (11) |
| Married | 78% | 39 |
| Symptoms and Shoulder Strength | ||
| Duration of symptoms (months) | 2 6 18 | (23 ± 41) |
| Daily shoulder use at work | ||
| Heavy/Moderate manual labor | 24% | (12) |
| Light/No manual labor | 74% | (37) |
| Missing | 2% | (1) |
| Dominant Shoulder Affected | ||
| No | 22% | (11) |
| Yes | 74% | (37) |
| Missing | 4% | (2) |
| Tear as a result of trauma | ||
| No | 46% | (23) |
| Yes | 54% | (27) |
| External Rotation Strength Ratio¶ | 0.3 0.5 0.7 | (0.5 ± 0.3) |
| Isolated Abduction Strength Ratio¶ | 0.8 0.9 1.0 | (0.9 ± 0.2) |
| Comorbidities and Personal Habits | ||
| Number of comorbidities | ||
| ≤1 | 58% | (29) |
| >1 | 42% | (21) |
| Smoking | ||
| Never | 48% | (24) |
| Past/current | 48% | (24) |
| Missing | 4% | (2) |
| Alcohol Use | ||
| 2–3 times per month or less | 36% | (18) |
| 1–2 times per week or more | 60% | (30) |
| Missing | 4% | (2) |
| Fear Avoidance and Behavior Physical Activity (FABQ) Score | 17.0 19.0 23.0 | (19.0 ± 4.0) |
| Mental Health Inventory (MHI-5) | 76.0 85.0 90.0 | (80.0 ± 17.0) |
| Patient Expectations After Treatment | ||
| A great improvement | 94% | (47) |
| Moderate/little/no improvement, or Quality of my life will be worse | 6% | (3) |
| Associated Disorders | ||
| Presence of biceps tendon pathology | ||
| No | 70% | (35) |
| Yes | 30% | (15) |
n for missing for continuous variables: External rotation strength ratio=4; Isolated abduction strength ratio=7;
a b c represent the lower quartile a, the median b, and the upper quartile c for continuous variables
X ± Standard Deviation for continuous variables
Strength ratio is measured as affected shoulder versus unaffected shoulder
A majority of patients had a full-thickness tear (90%; n=43; Table II). The median longitudinal size of the tendon with the largest tear was 2 centimeters (25th percentile=1 centimeter; 75th percentile=6 centimeters) and median transverse size was 2 centimeters (25th percentile=1 centimeter; 75th percentile=3 centimeters). Grade 0 fatty infiltration was present in 48% of patients (n=23).
Table II:
MRI and Surgical Characteristics of Rotator Cuff Tear in Patients Having Surgery: The ROW Cohort
| Rotator cuff tear characteristics | Percent of Patients* | (Number of Patients)** |
|---|---|---|
| MRI Characteristics | ||
| Longitudinal size of tear# | 1 2 6 | (4 ±3) |
| Transverse size of tear# | 1 2 3 | (2 ±2) |
| Cross-sectional area of tear# | 2 3 21 | (14 ±19) |
| Thickness of tear∏ | ||
| Partial-thickness | 10% | (5) |
| Full-thickness | 90% | (43) |
| Fatty infiltration± | ||
| Grade 0 | 48% | (23) |
| Grade 1 or more | 40% | (19) |
| Missing | 12% | (6) |
| Muscle Atrophy± | ||
| None/Mild | 62% | (30) |
| Moderate/Severe | 25% | (12) |
| Missing | 12% | (6) |
| Number of tendons torn | ||
| 0 or 1 | 60% | (29) |
| 2 or 3 | 40% | (19) |
| Tendon retraction | ||
| Stage I or not applicable¶ | 60% | (29) |
| Stage II or more | 40% | (19) |
| Surgical Characteristics | ||
| Biceps tenodesis/tenotomy | ||
| Yes | 60% | (30) |
| No | 36% | (18) |
| Missing | 4% | (2) |
| Type of repair | ||
| Single row | 58% | (29) |
| Double row | 24% | (12) |
| Other | 12% | (6) |
| Missing | 6% | (3) |
2 patients did not have a MRI available for review so total n for MRI variables in the table is 48
a b c represent the lower quartile a, the median b, and the upper quartile c for continuous variables
X ± Standard Deviation for continuous variables
Tear size determined by sum of supraspinatus and infraspinatus tear size in longitudinal or transverse planes for full-thickness tears only; n for missing: transverse size=5; longitudinal size=4; cross-sectional area=5
If any of the tendons had a full-thickness tear, the tear was classified as full-thickness
Grading reported for muscle most severely affected
Since tear was partial-thickness
In unadjusted multiple comparisons among variables without a significant interaction with time, none of the structural, demographic, symptom, comorbidities, personal habits, shoulder strength, surgical technique, or patient expectation characteristics were significant predictors of SPADI score during follow-up (Table III). When interactions were assessed, FABQ physical activity score and alcohol use were significant predictors of SPADI scores with a differential effect over time. Alcohol use predicted SPADI score in that those consuming alcohol 1–2 times per week or more had lower SPADI scores (better shoulder pain and function) as compared with those consuming alcohol 2–3 times per month or less. The effect size was greatest at 3 months of follow-up and then diminished during subsequent follow-up time points (Figure 1). FABQ physical activity score predicted SPADI such that those with higher FABQ physical activity scores (more fear avoidance behavior) had higher SPADI scores (worse shoulder pain and function). This difference was most pronounced at 3 months of follow-up (Figure 2).
Table III:
Predictors of SPADI Score at 18 months in Patients with Rotator Cuff Tears Having Surgery
| Variable | p-value of variable | p-value for interaction of variable with duration of follow-up* |
|---|---|---|
| Demographics | ||
| Highest level of education | 0.79 | 0.38 |
| Marital status | 0.22 | 0.92 |
| Sex | 0.40 | 0.99 |
| Age | 0.76 | 0.70 |
| Symptoms and Shoulder Strength | ||
| Duration of symptoms | 0.62 | 0.74 |
| Daily shoulder use at work | 0.12 | 0.69 |
| Tear as a result of trauma | 0.74 | 0.34 |
| Dominant shoulder affected | 0.91 | 0.09 |
| External rotation strength ratio | 0.27 | 0.46 |
| Isolated abduction strength ratio | 0.17 | 0.43 |
| Comorbidities and Personal Habits | ||
| Alcohol use | - | 0.02 |
| Fear avoidance and behavior (FABQ) physical activity | - | 0.001 |
| Number of Comorbidities | 0.98 | 0.54 |
| Smoking | 0.73 | 0.70 |
| Mental Health Inventory (MHI-5) | 0.11 | 0.28 |
| Associated Disorders | ||
| Presence of biceps tendon pathology | 0.49 | 0.60 |
| Rotator Cuff Tear Characteristics | ||
| Longitudinal size of tear | 0.14 | 0.67 |
| Transverse size of tear | 0.30 | 0.20 |
| Cross-sectional area of tear | 0.16 | 0.42 |
| Number of torn tendons | 0.68 | 0.14 |
| Fatty infiltration | 0.18 | 0.25 |
| Tendon retraction | 0.38 | 0.92 |
| Muscle atrophy | 0.48 | 0.64 |
| Surgical Characteristics | ||
| Biceps tenodesis/tenotomy | 0.78 | 0.32 |
| Type of repair | 0.91 | 0.74 |
SPADI=Shoulder Pain and Disability Index
Variables significant at p<0.05 are reported in italics
If interaction is significant, p-value for variable is not reported
Figure 1: Estimated differences with 95% confidence intervals in SPADI for patients with alcohol consumption of 2–3 times per month or less versus those with 1–2 times per week or more.
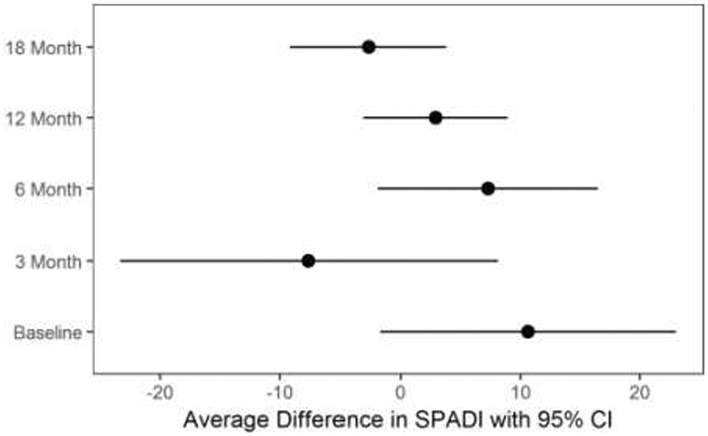
Note: Estimated differences at each of the time points is presented given the significant interaction of alcohol use with time. SPADI=Shoulder Pain and Disability Index
Figure 2: Estimated differences with 95% confidence intervals in SPADI for FABQ physical activity score.
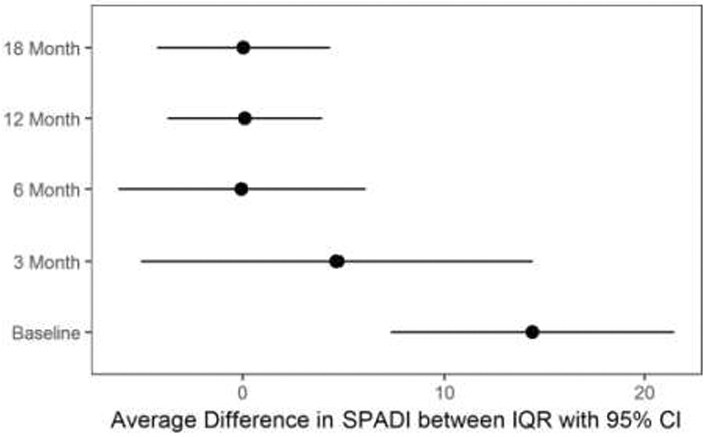
Note: Estimated differences for 75th percentile (23 points) versus 25th percentile (17 points) at each of the time points are presented given the significant interaction of FABQ physical activity with time. SPADI=Shoulder Pain and Disability Index
DISCUSSION
We assessed predictors of better outcomes of operative treatment for rotator cuff tears. In a longitudinal analysis, FABQ physical activity score and alcohol use were significant predictors of SPADI score and had an interaction with duration of follow-up. These variables showed a greater effect size during the initial duration of follow-up and the magnitude of their estimates diminished during longer follow-up time points.
Operative treatment is routinely offered to patients with rotator cuff tears. Assessment of better prognostic indicators after operative treatment can help to optimize patient selection and educate patients on expectations of treatment outcomes. Thus, this information can be useful to patients and clinicians.
Castagna et al4 studied 54 patients undergoing a transtendinous arthroscopic rotator cuff repair for partial-thickness tears. Although this study only assessed partial-thickness tears, less tendon retraction, younger age, and history of trauma were associated with better outcomes. Kamath et al16 reported on results of arthroscopic repair of high grade partial-thickness rotator cuff tears. Although this study was not specifically designed to assess prognostic factors associated with outcomes, the authors found that the average age of patients with an intact repair at follow-up was significantly lower than those with a persistent defect. Nho et al21 reported that shoulder strength predicted the American Shoulder and Elbow Surgeons (ASES) score after rotator cuff repair. Gladstone et al10 assessed 38 patients and reported that muscle atrophy and fatty infiltration were independent predictors of Constant and American Shoulder and Elbow Surgeons scores. In our study, none of the structural characteristics of the rotator cuff including fatty infiltration and muscle atrophy were significant predictors of outcomes. However, there were very few patients with Grade 3 or 4 fatty infiltration in our study because such patients are usually not recommended surgery. Longitudinal size of tear, although not statistically significant in our sample, was the closest measure to achieving significance and potentially could be significant in a larger sample of patients (p=0.14). Prior studies have reported that a larger tear size is related to worse shoulder outcomes of pain and function22, 25. A higher number of comorbidities was not a significant predictor of rotator cuff surgery outcomes in our study. Tashjian et al28 reported in 151 patients that those with a greater number of comorbidities had worse general health status after a rotator cuff repair but also had a greater improvement in overall shoulder pain, function, and quality of life scores.
Differences in surgical techniques such as single row repair versus double row repair versus transosseous/open repair, and whether or not a biceps tenodesis or tenotomy was performed were not significant predictors of surgical outcomes in our study. There is debate in the literature on whether differences in surgical techniques or adjuvant procedures with rotator cuff surgery impact treatment outcomes. A review from the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) concluded that double row repair has not been proven to be more effective than single row in full-thickness tears1. Prior literature has also found no significant difference in outcomes in patients that underwent a rotator cuff repair with a tenotomy/tenodesis versus without tenotomy/tenodesis7,9.
In our analysis, alcohol use and psychosocial factors such as fear avoidance behavior were significant predictors of surgical outcomes. Patients who had a greater fear of physical activity causing increased shoulder pain had worse shoulder pain and functional outcomes after surgery. Most of the effect was seen in the immediate postoperative period at 3 months of follow-up in our analysis. There is increasing literature on the role of psychosocial factors in treatment outcomes of musculoskeletal disorders. Woollard et al33 assessed factors associated with shoulder disability in 46 patients undergoing surgery for rotator cuff pathology at 6 months of follow-up. Patients underwent either a subacromial decompression or subacromial decompression with a rotator cuff repair. Surgery on the dominant arm and FABQ score were associated with treatment outcomes in the Woollard et al study. It is difficult to explain the association of greater alcohol use with treatment outcomes in our study. However, it is possible that greater alcohol use is a proxy for another variable that was not captured or controlled for in our data and univariate analysis.
Limitations of our study include a relatively small sample size and unavailability of complete data at all of the outcome time points. However, this is one of the few studies to longitudinally assess prognostic factors in patients undergoing operative treatment with a comprehensive set of potential predictor variables.
CONCLUSIONS
Longitudinal predictors of pain and functional outcomes after operative treatment for rotator cuff tears included alcohol use, and those with higher fear avoidance behavior had worse shoulder pain and function at 18 months of follow-up. The greatest effect of these variables was seen in the immediate 3 months follow-up after surgery. These data can be used to select optimal candidates for operative treatment of rotator cuff tears and assist with patient education and expectations prior to treatment.
ACKNOWLEDGMENTS
We thank the entire ROW team for their efforts. We also thank our clinical staff at the Orthopedic and Arthritis Center at Brigham and Women’s Hospital, Shoulder Service at Massachusetts General Hospital, and clinical staff at Vanderbilt Orthopaedic Institute for their efforts and cooperation.
FUNDING: Dr. Jain is/was supported by funding from National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) 1K23AR059199 and 1U34AR069201.
The project described was supported by CTSA award Number UL1TR000445 from the National Center for Advancing Translational Sciences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arce G, Bak K, Bain G, Calvo E, Ejnisman B, Di Giacomo G et al. Management of disorders of the rotator cuff: proceedings of the ISAKOS upper extremity committee consensus meeting. Arthroscopy 2013;29:1840–1850. 10.1016/j.arthro.2013.07.265 [DOI] [PubMed] [Google Scholar]
- 2.Berwick DM, Murphy JM, Goldman PA, Ware JE Jr., Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care 1991;29:169–176. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy 2007;23:347–354. 10.1016/j.arthro.2006.12.012 [DOI] [PubMed] [Google Scholar]
- 4.Castagna A, Delle Rose G, Conti M, Snyder SJ, Borroni M, Garofalo R. Predictive factors of subtle residual shoulder symptoms after transtendinous arthroscopic cuff repair: a clinical study. Am J Sports Med 2009;37:103–108. 10.1177/0363546508324178 [DOI] [PubMed] [Google Scholar]
- 5.Chen AL, Shapiro JA, Ahn AK, Zuckerman JD, Cuomo F. Rotator cuff repair in patients with type I diabetes mellitus. J Shoulder Elbow Surg 2003;12:416–421. 10.1016/S1058274603001721 [DOI] [PubMed] [Google Scholar]
- 6.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am 2012;94:227–233. 10.2106/JBJSJ.00739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Carli A, Vadala A, Zanzotto E, Zampar G, Vetrano M, Iorio R et al. Reparable rotator cuff tears with concomitant long-head biceps lesions: tenotomy or tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc 2012;20:2553–2558. 10.1007/s00167-012-1918-5 [DOI] [PubMed] [Google Scholar]
- 8.Feng S, Guo S, Nobuhara K, Hashimoto J, Mimori K. Prognostic indicators for outcome following rotator cuff tear repair. J Orthop Surg 2003;11:110–116. 10.1177/230949900301100202 [DOI] [PubMed] [Google Scholar]
- 9.Franceschi F, Longo UG, Ruzzini L, Papalia R, Rizzello G, Denaro V. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop 2007;31:537–545. 10.1007/s00264-006-0206-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719–728. 10.1177/0363546506297539 [DOI] [PubMed] [Google Scholar]
- 11.Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg 2002;11:33–39. 10.1067/mse.2002.119852 [DOI] [PubMed] [Google Scholar]
- 12.Henn RF 3rd, Kang L, Tashjian RZ, Green A. Patients’ preoperative expectations predict the outcome of rotator cuff repair. J Bone Joint Surg Am 2007;89:1913–1919. 10.2106/JBJS.F.00358 [DOI] [PubMed] [Google Scholar]
- 13.Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R 2014. 10.1016/j.pmrj.2014.08.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord 2014;15:4 10.1186/1471-2474-15-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain NB, Wilcox RB 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R 2013;5:45–56. 10.1016/j.pmrj.2012.08.019 Epub 2013/01/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am 2009;91:1055–1062. 10.2106/JBJS.G.00118 [DOI] [PubMed] [Google Scholar]
- 17.Kelly MJ, Dunstan FD, Lloyd K, Fone DL. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry 2008;8:10 10.1186/1471-244X-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klinger HM, Steckel H, Ernstberger T, Baums MH. Arthroscopic debridement of massive rotator cuff tears: negative prognostic factors. Arch Orthop Trauma Surg 2005;125:261–266. 10.1007/s00402-004-0738-6 [DOI] [PubMed] [Google Scholar]
- 19.Mallon WJ, Misamore G, Snead DS, Denton P. The impact of preoperative smoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg 2004;13:129–132. 10.1016/S1058274603002805 [DOI] [PubMed] [Google Scholar]
- 20.Miller JE, Higgins LD, Dong Y, Collins JE, Bean JF, Seitz AL et al. Association of strength measurement with rotator cuff tear in patients with shoulder pain: the rotator cuff outcomes workgroup study. Am J Phys Med Rehabil 2016;95:47–56. 10.1097/PHM.0000000000000329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg 2009;18:13–20. 10.1016/jjse.2008.05.045 [DOI] [PubMed] [Google Scholar]
- 22.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 2009;25:30–39. 10.1016/j.arthro.2008.08.010 [DOI] [PubMed] [Google Scholar]
- 23.Prasad N, Odumala A, Elias F, Jenkins T. Outcome of open rotator cuff repair. An analysis of risk factors. Acta Orthop Belg 2005;71:662–666. [PubMed] [Google Scholar]
- 24.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res 1991;4:143–149. [PubMed] [Google Scholar]
- 25.Romeo AA, Hang DW, Bach BR Jr., Shott S. Repair of full thickness rotator cuff tears. Gender, age, and other factors affecting outcome. Clin Orthop Relat Res 1999:243–255. [PubMed] [Google Scholar]
- 26.Sherman SL, Lyman S, Koulouvaris P, Willis A, Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res 2008;466:608–613. 10.1007/s11999-008-0116-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tashjian RZ, Bradley MP, Tocci S, Rey J, Henn RF, Green A. Factors influencing patient satisfaction after rotator cuff repair. J Shoulder Elbow Surg 2007;16:752–758. 10.1016/jjse.2007.02.136 [DOI] [PubMed] [Google Scholar]
- 28.Tashjian RZ, Henn RF, Kang L, Green A. Effect of medical comorbidity on self-assessed pain, function, and general health status after rotator cuff repair. J Bone Joint Surg Am 2006;88:536–540. 10.2106/JBJS.EO0418 [DOI] [PubMed] [Google Scholar]
- 29.Thorsen SV, Rugulies R, Hjarsbech PU, Bjorner JB. The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared. BMC Med Res Methodol 2013;13:115 10.1186/1471-2288-13-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Varkey DT, Patterson BM, Creighton RA, Spang JT, Kamath GV. Initial medical management of rotator cuff tears: a demographic analysis of surgical and nonsurgical treatment in the United States Medicare population. J Shoulder Elbow Surg 2016. (Epub). 10.1016/jjse.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 31.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52:157–168. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care 1992;30:473–483. [PubMed] [Google Scholar]
- 33.Woollard JD, Bost JE, Piva SR, Kelley Fitzgerald G, Rodosky MW, Irrgang JJ. The ability of preoperative factors to predict patient-reported disability following surgery for rotator cuff pathology. Disabil Rehabil 2017;39:2087–2096. 10.1080/09638288.2016.1219396 [DOI] [PubMed] [Google Scholar]


