Abstract
Introduction
Western-constructed neuropsychological tests have been used in low and middle income countries to assess the impact of HIV/AIDS and other chronic illnesses. We explore using such instruments cross-culturally in a sub-Saharan Africa setting.
Methods
IMPAACT P1104S was a two-year observational study carried out at six clinical sites (South Africa- 3 sites, Malawi, Uganda and Zimbabwe) to assess and compare neuropsychological outcomes in three cohorts of children 5–11 years of age: HIV-infected (HIV), HIV-exposed but uninfected (HEU) and HIV unexposed and uninfected (HU). Descriptive statistics compared socio-demographic characteristics among children at sites. Instruments included the KABC-II cognitive ability, TOVA attention/impulsivity, BOT-2 motor proficiency tests, and BRIEF executive function problems. Test characteristics were assessed using intraclass and Spearman non-parametric correlations, linear regression and principal factor analyses.
Results
Of the 611 participants, 50% were male and mean age ranged from 6.6 to 8 years. In Malawi, Uganda and Zimbabwe, substantial proportions of families lived in rural settings in contrast to the South African sites. Intraclass correlation coefficients between weeks 0 and 48 were highest for the KABC scores, ranging between 0.42 to 0.71.Correlations among similar test domains were low to moderate but significant, with positive correlation between KABC Sequential and TOVA scores and negative correlation between BRIEF and KABC scores. TOVA response time scores correlated negatively with the BOT-2 Total points score. Strong and significant associations between individual measures of growth, disability and development with all test scores were observed. Performance-based measures were markedly lower for HIV compared to HEU and HU participants, even after controlling for age, sex and site. Factor analyses confirmed the underlying theoretical structure of the KABC scaled item scores.
Conclusion
The KABC, TOVA, BRIEF and BOT-2 were valid and reliable tools for assessing the neuropsychological impact of HIV in four sub-Saharan African countries.
Keywords: Pediatric HIV, Neuropsychological testing, validity, reliability, Africa
INTRODUCTION
Access to pediatric prevention and care for HIV/AIDS has expanded throughout low and middle income countries (LMIC), with reduced pediatric infection, morbidity and mortality, shifting attention to the impact of the HIV virus on neurocognitive development and other longer term outcomes. As learning and problem solving approaches may differ across cultures, researchers have questioned whether tests developed in high income settings are valid elsewhere1–6. Tests need to be reliable, consistent, and robust to challenging testing situations, simple to score and interpret and sensitive to population variability and changes in health and home environment.7–11
For this study, we chose four Western-developed standard tests, previously used in LMIC HIV/AIDS and other high burden illness settings, These measures have proven sensitive to the neuropsychological effects of pediatric HIV in the sub-Saharan African context, assessing aspects of motor development and proficiency, attention, working memory, learning, visual-spatial analysis and problem solving, and planning and reasoning11–16. The present study used the Kaufman Assessment Battery for Children, 2nd edition (KABC-II)17, the Test of Variables of Attention (TOVA; www.tovatest.com)18, the Bruininks-Oseretsky Test of Motor Proficiency, 2nd edition (BOT-2)19, and the Behavior Rating Inventory for Executive Function (BRIEF)20
Some have questioned the validity of adapting “Western-based” tests to the African context, and have recommended instead the development of altogether new neurodevelopmental assessment batteries more appropriate for such settings along with normative data specific to the target culture5. Contrary to this view, Boivin and Giordani (2009, 2013) have proposed that human neurodevelopment can be characterized within a foundational brain/behavior “omnibus”, universally accessible by neuropsychological assessment batteries (even “Western” ones) that are well designed, carefully adapted, and appropriately applied21,22. In order to substantiate this view, we evaluate the feasibility, reliability and validity of cross-cultural neuropsychological testing in a sub-Saharan Africa setting with children affected by HIV/AIDS. We hypothesize that these instruments meet adequate test construction criteria and can be used effectively and successfully in cross-cultural neuropsychological research in at-risk African children.
METHODS
Study population and design
IMPAACT P1104S was a two-year multi-site observational study carried out at six clinical sites in four sub-Sahara African countries: three in South Africa (Soweto, Tygerberg and Johannesburg); Kampala (Uganda); Harare (Zimbabwe); and Lilongwe (Malawi). The purpose was to assess and compare neuropsychological outcomes in three cohorts of young children (5 to < 11 years): HIV-infected (HIV), HIV-exposed but uninfected (HEU) and HIV-unexposed and uninfected (HU)23. HIV-infection and exposure was assumed to be perinatal or during breastfeeding. HIV-infected children were eligible if they had previously enrolled and were actively being followed in PACTG 1060, version 5.0, a longitudinal study evaluating nevirapine-based vs. lopinavir/ritonavir-based antiretroviral regimens24. The two P1104S comparison groups (HEU and HU) were recruited from similar neighborhoods as the HIV-infected participants; siblings were encouraged to co-enroll. Target sample sizes were determined based on the number of eligible P1060 children and a power computation for cross-sectional pairwise group differences. To ensure balance of the two control groups with the HIV-infected participants within sites, site and age-specific enrollment limits were imposed based on the number and age distribution of the eligible P1060 participants. Each HIV-uninfected cohort was to enroll 182 children (35 <6 years, 64 6 − <7 years and 83 7 − <11 years). Data for P1104S were collected between September 23, 2013 and December 12, 2016.
Other eligibility criteria included documented evidence of mother’s HIV status during pregnancy (if HIV-infected) and at birth or afterwards (if HIV negative). For the HU control group, exclusion criteria included history of documented brain injury, seizures, or hospitalization from CNS infection. Local institutional review boards approved the study and parental/guardian informed consents were obtained. Assent was obtained for children seven years and older. Study assessments were performed at baseline (week 0), week 48 and week 96; Data from all study weeks are included in the reliability analysis, while only baseline data are included in the validity analysis.
Measures
Socio-demographic characteristics collected included that of the caregiver (education, HIV-status, length of time child was in care of primary caregiver, family income, fuel and water sources, urban or rural living zone and employment) and child (anthropomorphic measures, illness history, and medications which may influence neuropsychological testing). Children’s neurodevelopment was assessed using performance-based measures and subjective assessments. Performance-based measures (e.g., KABC-II, TOVA, and BOT-2) are those in which there is a direct observation of the child performing a specific task using a standardized battery of tests that can include props and toys. Subjective assessments (BRIEF, Multiple Indicators Cluster Survey) generally include questionnaires with items relating to the child’s behavior that are read out loud to the informant (e.g. parent), who evaluates the extent to which those behaviors describe the child.
Kaufman Assessment Battery for Children, second edition (KABC-II)
The KABC-II17 measures neuropsychological outcomes for ages 3 – 18 years, and has been previously validated in Uganda25,26 and in South Africa6. In this study the KABC-II Luria model was used to assesses cognitive abilities in four domains: 1) Sequential Processing (short-term memory), 2) Simultaneous Processing (visual-spatial processing and problem solving), 3) Learning (immediate and delayed memory), 4) Planning (executive reasoning). All subtests were administered to all participants with instructions in local languages (the child’s preferred language). Subtests were administered even if out of age-range for the purpose of future analyses by age-band, but only scaled if within appropriate age-ranges. Subscale scores and Global scores (Mental Processing Index and Non-Verbal Index) were scaled to a US population by age. The KABC-II takes about 1.5 hours to administer. The Appendix describes the KABC-II subtests. Items of three subtests were administered in English at all sites; Rebus and Rebus delayed and Number recall (designed for one-syllable numbers). As such, the Rebus tests assessed learning in a foreign language. It is common in Anglophone Africa for English numbers to be used and translating would have complicated the subtest by introducing multisyllabic words.
Test of Variables of Attention, version 8 (TOVA)
The TOVA is a computerized test measuring key components of attention and self-control, variability (consistency), response time (speed), commissions (impulsivity), and omissions (focus and vigilance). Prior studies suggest that the visual TOVA (where a child responds rapidly by pressing a switch when a simple geometric stimulus “signal” appears on a computer screen) is a sensitive measure of persisting neurocognitive effects among African children surviving cerebral malaria27–29. Following instructions and practice trials, the TOVA takes 22 minutes for children older than 5.5 years. Scoring is based on establishing whether or not response times and attention is at the normal range for the sex and age of the child with ADHD scores more negative than −1.8 considered suggestive of ADHD for USA norms.
Bruininks-Oseretsky Test of Motor Proficiency, 2nd edition (BOT-2), Brief form
The BOT-219,30 is a standardized test comprehensively assessing gross and fine motor skills in children ages 4–21 years through eight subtests: Fine Motor Precision, Fine Motor Integration, Manual Dexterity, Bilateral Coordination, Balance, Running Speed and Agility, Upper Limb Coordination, and Strength. The Brief form of the BOT-2 has 12 items, each a game-like task, and takes about 15 minutes in all to administer. Composite scores include Fine Manual Control, Manual Coordination, Body Coordination, Strength and Agility and Total Composite Score. Total scores (0–72) are standardized to US norms by age.
Behavior Rating Inventory for Executive Function (BRIEF)
The BRIEF Parent form for school-age children (5–18 years) was especially designed to evaluate executive function behaviors through 86 items rated as Never=1, Sometimes=2 and Often=3, and takes about 15–30 minutes to administer31. The BRIEF has eight non-overlapping clinical scales and two statistically derived indexes: 1) Behavioral Regulation Index (BRI; sum of Inhibit, Shift and Emotional Control), and 2) Metacognition Index (MI; sum of Initiate, Working Memory, Plan/Organize, Organization of Materials and Monitor). The Global Executive Composite score (GEC) is the sum of the BRI and MI. BRIEF standardized scores are calculated based on the scores of other respondents from a standardized sample, by age and sex. Higher scores suggest a higher level of dysfunction in a specific domain. A negativity and inconsistency score is also obtained which assists with determining the validity of responses
MICS-4 Early Childhood Development and Childhood Disability Scales
We used the Early Childhood Development portion of the Questionnaire for Children Under 5 (17 items) and Questionnaire Form for Child Disability from the Multiple Indicators Cluster Survey (MICS) research program is sponsored by UNICEF32. The primary caregiver answered the questionnaire and selected questions were scored and summed to develop an overall Disability score (scale 0–100) and an overall Development score (scale 0–100), with higher values indicating better child development and worse child disability respectively.
Procedures
Standardized operating procedures were developed for each battery of tests, including test administration, scoring and quality assurance. The KABC-II, TOVA, and BOT-2 tests were designed to be readily adaptable to cross-cultural settings and instructions for the various tasks and items can be spoken by the examiner to the child in the local language or in English (the official educational language at some study sites) during administration, without the need for formal written translation or written explanation for the child. Each subtest of the KABC-II has example “teaching” items to ensure that the child understands the task required. In fact, the KABC-II has a nonverbal index score (NVI) compiled from the subtests for which language fluency is not required (even administrable by pantomime), and this global performance composite was a principal outcome for our analyses. Likewise, the BOT-2 items can be demonstrated by modeling on the part of the tester, and the TOVA relies on simple geometric figures for the signal and non-signal stimuli, not on letters or numbers or specific images as is the case in other continuous performance monitoring tests of attention.
The 86 items of the BRIEF questionnaire, read out loud to the parent or principal caregiver of the child, were formally translated by permission of the publisher. The publisher provided translated versions for Luganda, Afrikaans and Xhosa. For Shona, Zulu, Chichewa, Sesotho and Setswana, instructions and items were translated (forward and backward) and approved by the authors of the BRIEF, before being administered by trained assessors. The HSCL, MICS-4 disability and MICS-4 child development and household socio-economic questionnaires were translated into local languages by the sites and administered as interviews. Where possible, tests were administered by testers who were blinded to the child’s HIV status. The TOVA was administered first so that attention was assessed before the child was tired, and also that visual deficits for study children would immediately become evident, allowing for adaptation of subsequent assessments to limited vision capability if necessary. The battery was mostly completed in one day unless a child appeared tired, requiring a second session to complete the assessment (within one week).
Testing quality assurance procedures included a one-week training by coauthor MJB, weekly practice sessions over a one-month period by all testers, and a quality assurance plan required each month for every tester (KABC-II video evaluation, team self-video evaluation, standard operating procedures review for all tests). KABC-II testing quality was scored according to a consistent rubric and the scores were tracked monthly for every tester at every site by independent KABC-II testing experts at the Global Health Uganda assessment center in Kampala. The TOVA was automated and the BOT-2 was a straight-forward test of motor proficiency so these were not evaluated as carefully as the KABC-II, but they also had standard operating procedures that were to be reviewed by testers monthly. These will be described in depth in a separate manuscript.
Statistical analysis
Data were retrieved on May 3, 2017. Sociodemographic characteristics were summarized by site and compared using Chi-square, analysis of variance and Wilcoxon rank-sum tests. A socioeconomic index was based on seven characteristics: fuel, water, refrigerator, caregiver’s work status, social grant main source of income, caregiver education, sufficiency of household income to meet basic needs. Each item was scored from 0–10, and a mean score was computed with 10 reflecting the highest socio-economic status.
Feasibility was assessed through test completion rates and the ability to complete the tests in one day without significant interruptions. Test-retest reliability was assessed through absolute (mean difference, upper and lower limits of agreement and the coefficient of repeatability) and relative (Pearson product-moment correlation, intraclass correlation coefficient, ICC) measures33–35. Absolute and relative measures assessed the consistency and agreement of test scores from week 0 to week 48 and from week 48 to week 96 (differences were computed as the value at the most recent week minus the value at the earlier week). ICCs were computed using linear mixed models regression with participants nested within cohorts, both unadjusted and adjusted for site, participant age at entry and sex. Models used restricted maximum likelihood (REML) estimation. Test-retest analyses were repeated on the HIV-infected cohort as a sensitivity analysis to explore potential effects of change in disease status.
An exploratory principal factor analysis was performed on 13 of the 15 KABC-II week 0 items for the full sample and by HIV status (HIV-infected, HIV-uninfected), using the squared multiple correlations as initial communality estimates and varimax orthogonal rotation, with a four-factor model based on the theoretical underlying structure. Factor loadings, percent of common variance and percent of total variance were summarized. Prior to carrying out the factor analysis, we explored the data distributions graphically and tested for normality using the Shapiro-Wilk test.
Construct validity was assessed using baseline (week 0) data. First, correspondence (convergence) validity among test domains was assessed using linear regression models and generalized estimating equations (GEE) for robust error estimates. Models, adjusted just for cohort (unadjusted) and also for age, sex and site (adjusted), were run pooling all study participants and then separately by group (HIV-infected; comparison, pooling HEU and HU). Parameter estimates and 95% confidence intervals were estimated. We also computed Spearman rank correlation coefficients for the unadjusted data. Prior cross-cultural work suggests that measures of attention (e.g., TOVA D-prime), memory (e.g., KABC sequential processing) and visual spatial processing would be associated, that working memory and attention would reflect executive function (assessed in this study through the BRIEF) and that sequential processing and mental processing indices would be inversely correlated with TOVA error scores (impulsivity, inattention)5,36,37. We were also interested in assessing comparability of performance based (KABC, TOVA) with parental evaluations (BRIEF).
Second, we assessed whether neuropsychological scores correlated with HIV status, growth, quality of the home environment and caregiving (child’s development, disability; and socio-economic status). For each characteristic and test score, a linear regression model using GEE methods was fit over all cohorts and then separately for the HIV and comparison (pooling HU and HEU) cohorts. Unadjusted regressions and those adjusted for site, sex and age at study entry were performed. Parameter estimates and their standard errors and significance levels were used to indicate degree of associations. Statistical significance was determined with two-sided tests at alpha=0.05. All analyses were carried out with SAS version 9.4.
RESULTS
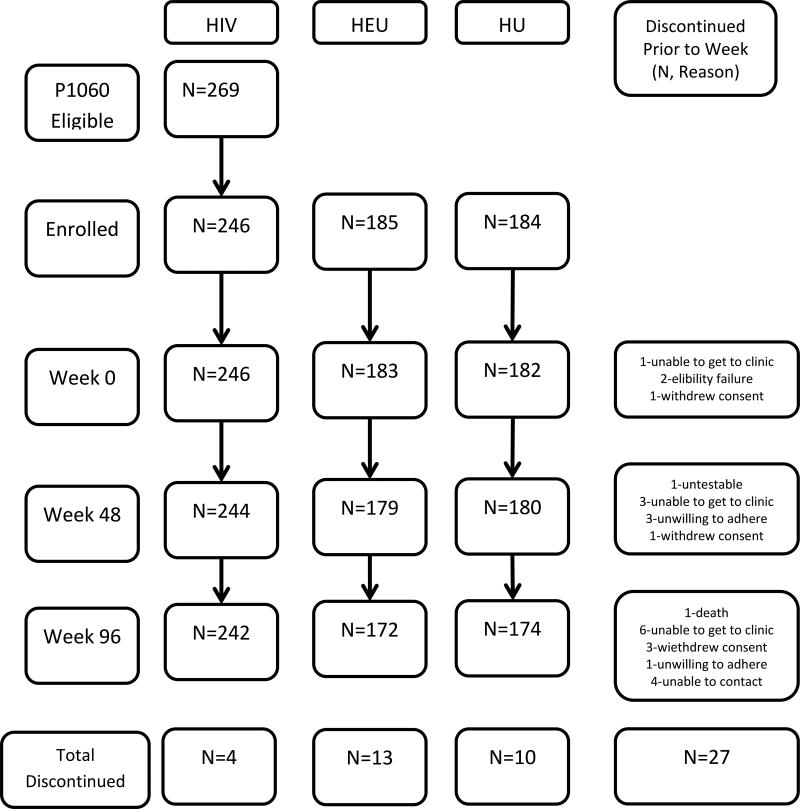
Of the original 615 enrolled, 611 participants (246 HIV, 183 HEU and 182 HU) completed the baseline study visit and were eligible for analysis (Figure 1). Of these, 603 (98.7%) completed the week 48 visit and 588 (96.2%) completed the week 96 visit; twenty three (3.8% of 611) discontinued prematurely (prior to week 96; 4 HIV-infected, 11 HEU, 8 HU). Test completion rates were 95% or higher at each study visit with over 91 percent of children completing test batteries in one day. Although only seven percent of caregivers completed the entry visit batteries in one day, on subsequent visits over 95% did so. Over 97 percent of child and caregiver tests were considered to be valid by the test administrators.
Figure 1.
The number of participants at each P1104S study visit and reasons for discontinuations.
Note: HIV=HIV-infected cohort; HEU=HIV-exposed, uninfected; HU=HIV unexposed, uninfected
Socio-demographic characteristics
Table 1 shows personal and family characteristics by study site, pooling cohorts. By design, there were approximately 40% HIV and 30% each HEU and HU at each study site. About 50 percent were male. Mean age ranged from 6.6 to 8 years. Johannesburg and Soweto enrolled older participants while Malawi, Uganda and Zimbabwe enrolled younger participants (p<0.001). Weight and height z-scores were especially low at Malawi (−1.14 and −1.55, respectively, p < 0.001). MICS disability scores were highest at Uganda (10.56, p < 0.001) compared to the other sites. Development scores were lowest at Malawi (50.4; p < 0.001). Over 90% of caregivers across sites were biological mothers at entry and over 88% had been primary caregivers for five years or more at that time. Close to 70% of primary caregivers across the 3 arms were HIV-infected.
Table 1.
Child, Caregiver and Family characteristics at Study Entry by Site
| Characteristic | Joburg (N=69) |
Soweto (N=100) |
Tygerberg (N=140) |
Malawi (N=81) |
Uganda (N=89) |
Zimbabwe (N=132) |
Total (N=611) |
P-Valuea | |
|---|---|---|---|---|---|---|---|---|---|
| Design Characteristics | |||||||||
|
| |||||||||
| Cohortb | HIV | 27 (39%) | 42 (42%) | 56 (40%) | 33 (41%) | 37 (42%) | 51 (39%) | 246 (40%) | 1.000 |
| HEU | 21 (30%) | 29 (29%) | 42 (30%) | 24 (30%) | 26 (29%) | 41 (31%) | 183 (30%) | ||
| HU | 21 (30%) | 29 (29%) | 42 (30%) | 24 (30%) | 26 (29%) | 40 (30%) | 182 (30%) | ||
|
| |||||||||
| Child Characteristics | |||||||||
|
| |||||||||
| Sex | Male | 32 (46%) | 50 (50%) | 65 (46%) | 43 (53%) | 49 (55%) | 51 (39%) | 290 (47%) | 0.182 |
| Race | Black African | 69 (100%) | 100 (100%) | 97 (69%) | 81 (100%) | 89 (100%) | 132 (100%) | 568 (93%) | <.001 |
| Coloured/White/Other | 0 (0%) | 0 (0%) | 43 (31%) | 0 (0%) | 0 (0%) | 0 (0%) | 43 (7%) | ||
| Age (years) | Mean (s.d.) | 8.0 (1.6) | 7.9 (1.3) | 7.4 (1.3) | 6.6 (0.9) | 6.7 (1.2) | 6.8 (1.4) | 7.2 (1.4) | <.001 |
| <6 yrs | 8 (12%) | 8 (8%) | 11 (8%) | 18 (22%) | 22 (25%) | 45 (34%) | 112 (18%) | <.001 | |
| 6–<7 yrs | 12 (17%) | 21 (21%) | 58 (41%) | 44 (54%) | 37 (42%) | 39 (30%) | 211 (35%) | ||
| >=7 yrs | 49 (71%) | 71 (71%) | 71 (51%) | 19 (23%) | 30 (34%) | 48 (36%) | 288 (47%) | ||
| In school at time of KABC test | 58 (84%) | 84 (86%) | 94 (71%) | 55 (77%) | 41 (46%) | 74 (57%) | 406 (69%) | <.001 | |
| Unknown/NA | 0 | 2 | 8 | 10 | 0 | 3 | 23 | ||
| WHO weight z-score | Mean (s.d.) | −0.31 (1.11) | −0.19 (1.09) | −0.18 (1.06) | −1.14 (0.76) | −0.52 (0.83) | −0.48 (0.87) | −0.44 (1.01) | <.001 |
| WHO height z-score | Mean (s.d.) | −0.64 (1.04) | −0.57 (1.05) | −0.38 (0.95) | −1.55 (0.98) | −0.83 (0.96) | −0.38 (1.00) | −0.66 (1.06) | <.001 |
| WHO BMI z-score | Mean (s.d.) | 0.08 (0.91) | 0.19 (1.04) | 0.05 (0.99) | −0.20 (0.73) | 0.01 (0.82) | −0.40 (1.02) | −0.06 (0.96) | <.001 |
| MICS disability score | Mean (s.d.) | 3.77 (6.21) | 4.60 (9.37) | 4.29 (8.49) | 5.31 (10.01) | 10.56 (11.52) | 5.76 (8.02) | 5.65 (9.25) | <.001 |
| MICS development score | Mean (s.d.) | 76.35 (12.23) | 84.09 (10.89) | 86.28 (12.16) | 50.42 (13.92) | 69.25 (15.14) | 73.17 (13.13) | 74.73 (17.14) | <.001 |
|
| |||||||||
| Caregiver Characteristics | |||||||||
|
| |||||||||
| Caregiver is biological mother | 66 (96%) | 92 (92%) | 137 (98%) | 75 (93%) | 80 (90%) | 122 (92%) | 572 (94%) | 0.18 | |
| Cgv for 5 or more years | 61 (88%) | 92 (92%) | 137 (98%) | 74 (91%) | 79 (89%) | 120 (91%) | 563 (92%) | 0.09 | |
| HIV Status of primary caregiver | HIV-uninfected | 21 (31%) | 29 (30%) | 43 (31%) | 28 (35%) | 31 (35%) | 41 (31%) | 193 (32%) | 0.96 |
| HIV-infected | 47 (69%) | 67 (70%) | 97 (69%) | 53 (65%) | 57 (65%) | 91 (69%) | 412 (68%) | ||
| Not reported | 1 | 4 | 0 | 0 | 1 | 0 | 6 | ||
|
| |||||||||
| Socioeconomic Characteristics | |||||||||
|
| |||||||||
| Current residential zone | Rural | 7 (10%) | 3 (3%) | 1 (1%) | 34 (42%) | 25 (28%) | 39 (30%) | 109 (18%) | <.001 |
| Peri-urban | 30 (43%) | 10 (10%) | 138 (99%) | 27 (33%) | 60 (67%) | 3 (2%) | 268 (44%) | ||
| Urban | 32 (46%) | 87 (87%) | 1 (1%) | 20 (25%) | 4 (4%) | 90 (68%) | 234 (38%) | ||
| Major income source | Mother | 24 (35%) | 22 (22%) | 28 (20%) | 30 (37%) | 45 (51%) | 34 (26%) | 183 (30%) | <.001 |
| Father | 16 (23%) | 10 (10%) | 49 (35%) | 43 (53%) | 36 (40%) | 81 (61%) | 235 (39%) | ||
| Social grant | 23 (33%) | 64 (65%) | 43 (31%) | 0 (0%) | 0 (0%) | 0 (0%) | 130 (21%) | ||
| Other person/source | 6 (9%) | 3 (3%) | 20 (14%) | 8 (10%) | 8 (9%) | 17 (13%) | 62 (10%) | ||
| Missing | 0 | 1 | 0 | 0 | 0 | 0 | 1 | ||
| Socio-economic indexd | Median (Q1, Q3) | 7.1 (5.7, 8.3) | 5.7 (5.7, 7.1) | 6.4 (5.0, 8.6) | 3.0 (2.4, 3.9) | 5.8 (4.5, 6.8) | 6.2 (4.6, 7.6) | 6.0 (4.6, 7.6) | <.001c |
Unless indicated, differences among sites for categorical measures are tested using the Chi-Square test and for continuous measures, using the analysis of variance.
HIV=HIV-infected; HEU=HIV-exposed, uninfected; HU=HIV-unexposed, uninfected
Kruskal-Wallis Test
The socio-economic index is a composite of caregiver education, fuel and water sources, sufficiency of household income for basic needs, caregiver education and work status, major source of income and whether household has a refrigerator. Values range from 0–10.
Among the HIV cohort, several of the HIV disease characteristics differed across study sites, in particular age at ARV initiation (youngest at Soweto and Tygerberg, oldest at Malawi) and length of time on ARVs (longest at the South African sites), WHO disease stage (most severe at Johannesburg and Zimbabwe, least severe at Soweto; Supplemental Table 1)
In Malawi, Uganda and Zimbabwe, substantial proportions of families lived in rural settings in contrast to the South African sites. In Johannesburg and Malawi, non-rural families were split equally between urban and peri-urban settings while in the other sites, the non-rural families lived primarily in one setting (p < 0.001). The composite socio-economic indicator showed that participants from Johannesburg had better socio-economic circumstances than the others, with Malawi the least resourced (p < 0.001; Table 1).
Test-Retest reliability
Unadjusted intraclass correlation (ICC) measures between weeks 0 and 48 were highest for KABC scaled scores. Except for delayed recall, these values ranged from 0.54 to 0.73. The ICC for the BOT-2 Total points score was 0.69. BRIEF ICC measures ranged from 0.50 (Monitor), 0.52 (BRI) to 0.56 (MI) and 0.57 (GEC). The ICC values for the TOVA D-Prime and D-Prime Standard were 0.63 and .45, respectively (Table 2). Pearson correlations were very similar to the unadjusted ICCs (Table 2) while adjusted ICC measures were slightly lower (data not shown).
Table 2.
Absolute and relative measures of agreement for weeks 0 and 48
| Outcome | Week 0 N, mean (sd) |
Week 48 N, mean (sd) |
Pearsons | Unadjusted ICCb (95% CI) |
Mean Difference (95% CI) |
Limits of agreementv |
CRf | ||
|---|---|---|---|---|---|---|---|---|---|
| Kaufman Assessment Battery for Children (KABC-II), Summary Scores | |||||||||
|
| |||||||||
| Sequential | 605 | 83.32 (12.12) | 601 | 82.92 (12.44) | 0.72 | 0.71 (0.67,0.75) | −0.39 (−1.13,0.36) | −18.46,17.69 | 18.45 |
| Simultaneous | 606 | 77.72 (12.41) | 602 | 79.90 (13.20) | 0.66 | 0.65 (0.61,0.70) | 2.05 (1.20,2.89) | −18.60,22.70 | 21.07 |
| Learning | 605 | 86.69 (16.02) | 601 | 86.34 (14.75) | 0.56 | 0.54 (0.48,0.59) | −0.35 (−1.51,0.82) | −28.66,27.97 | 28.90 |
| Planning | 285 | 76.08 (11.87) | 474 | 76.59 (13.20) | 0.75 | 0.69 (0.64,0.74) | 1.92 (0.79,3.06) | −16.99,20.84 | 19.31 |
| Delayed recall | 602 | 87.39 (15.75) | 601 | 84.90 (13.88) | 0.45 | 0.42 (0.35,0.49) | −2.52 (−3.79,−1.26) | −33.29,28.25 | 31.40 |
| Nonverbal index | 608 | 76.01 (12.03) | 602 | 76.63 (12.45) | 0.75 | 0.73 (0.69,0.76) | 0.53 (−0.17,1.23) | −16.53,17.59 | 17.41 |
| Mental processing index | 607 | 77.27 (11.63) | 601 | 76.83 (11.98) | 0.73 | 0.71 (0.67,0.75) | −0.53 (−1.22,0.16) | −17.40,16.33 | 17.21 |
|
| |||||||||
| Bruininks-Oseretsky Test of Motor Proficiency (BOT-2) | |||||||||
|
| |||||||||
| Total score | 608 | 50.85 (8.42) | 603 | 51.59 (8.06) | 0.70 | 0.69 (0.64,0.73) | 0.80 (0.30,1.31) | −11.63,13.24 | 12.69 |
|
| |||||||||
| Behavior Rating Inventory for Executive Function (BRIEF) | |||||||||
|
| |||||||||
| BRI | 609 | 52.21 (12.28) | 602 | 49.81 (11.40) | 0.51 | 0.52 (0.46,0.58) | −2.31 (−3.25,−1.37) | −25.29,20.67 | 23.45 |
| MI | 609 | 51.38 (12.06) | 603 | 48.16 (11.13) | 0.56 | 0.56 (0.51,0.61) | −3.17 (−4.05,−2.29) | −24.63,18.30 | 21.90 |
| GEC | 609 | 51.92 (12.20) | 603 | 48.77 (11.17) | 0.56 | 0.57 (0.52,0.62) | −3.07 (−3.95,−2.19) | −24.59,18.44 | 21.95 |
| Monitor | 609 | 50.32 (12.91) | 603 | 47.26 (12.47) | 0.49 | 0.50 (0.44,0.56) | −2.98 (−4.00,−1.95) | −28.02,22.07 | 25.56 |
|
| |||||||||
| Test of Variables of Attention (TOVA) | |||||||||
|
| |||||||||
| ADHD | 582 | 0.03 (2.86) | 595 | 0.70 (2.96) | 0.52 | 0.53 (0.47,0.59) | 0.76 (0.53,0.99) | −4.74,6.26 | 5.61 |
| Response time variability (msec) | 582 | 247.14 (71.81) | 595 | 208.89 (66.77) | 0.66 | 0.66 (0.61,0.70) | −41.39 (−46.01,−36.76) | −151.90,69.12 | 112.77 |
| Response time (msec) | 582 | 663.05 (153.03) | 595 | 590.65 (129.70) | 0.76 | 0.74 (0.71,0.78) | −76.71 (−85.00,−68.42) | −274.71,121.29 | 202.04 |
| Commission (%) | 582 | 9.52 (6.39) | 595 | 6.94 (5.45) | 0.46 | 0.46 (0.39,0.52) | −2.71 (−3.21,−2.20) | −14.77,9.36 | 12.31 |
| Omission (%) | 582 | 15.28 (16.81) | 595 | 10.25 (13.11) | 0.57 | 0.57 (0.51,0.62) | −5.65 (−6.78,−4.52) | −32.70,21.40 | 27.60 |
| D Prime | 582 | 2.70 (0.99) | 595 | 3.25 (1.10) | 0.63 | 0.63 (0.58,0.68) | 0.58 (0.51,0.66) | −1.17,2.33 | 1.78 |
| D-prime standard score | 582 | 85.88 (13.09) | 595 | 89.22 (13.61) | 0.47 | 0.45 (0.39,0.52) | 3.71 (2.58,4.83) | −23.16,30.58 | 27.42 |
|
| |||||||||
| Selected KABC Raw Scores | |||||||||
|
| |||||||||
| Conceptual thinking | 608 | 12.07 (5.77) | 602 | 14.39 (5.26) | 0.68 | 0.66 (0.62,0.71) | 2.33 (1.97,2.68) | −6.40,11.05 | 8.90 |
| Story completion | 608 | 5.09 (4.09) | 602 | 6.59 (5.03) | 0.82 | 0.80 (0.77,0.83) | 1.48 (1.25,1.71) | −4.17,7.14 | 5.77 |
| Pattern reasoning | 608 | 5.51 (4.76) | 602 | 7.32 (5.60) | 0.75 | 0.74 (0.70,0.77) | 1.78 (1.49,2.08) | −5.49,9.06 | 7.43 |
| Face recognition | 608 | 11.09 (4.13) | 602 | 12.33 (3.67) | 0.58 | 0.57 (0.51,0.62) | 1.25 (0.96,1.53) | −5.80,8.29 | 7.19 |
| Hand movements | 608 | 6.73 (2.77) | 602 | 7.44 (2.88) | 0.64 | 0.64 (0.59,0.68) | 0.73 (0.54,0.92) | −3.93,5.39 | 4.76 |
Pearson= Pearson product moment correlation
ICC=Intraclass correlation coefficient; Unadjusted ICC values incorporate cohort and time in regression models
95% of differences should fall within lower and upper limits of agreement
CR=coefficient of repeatability (roughly half the width from lower to upper limit of agreement
Both Pearson and intraclass correlations between measures at week 48 and week 96 were slightly higher than those between weeks 0 and 48 (Supplemental Table 2). In a few cases, these differences were substantial. For example, whereas the Pearson correlation between weeks 0 and 48 for KABC learning was 0.56, the same correlation between weeks 48 and 96 was 0.82.
Mean difference scores varied by time and test. For example, mean scores were stable between weeks 0 and 48 (as indicated by the 95% CI for the mean difference including zero) for the KABC Nonverbal index and the KABC Mental processing index, while there were small but statistically significant increases for the KABC simultaneous scores and decreases for the KABC Delayed recall. During this same time frame, BRIEF scores decreased on average, indicating improved function (Table 2). Most of the KABC scores as well as the TOVA ADHD and D-Prime scores increased slightly between weeks 48 and 96 while BRIEF scores were stable (Supplemental Table 2). By definition, 95% of individual difference scores would lie between the lower and upper levels of agreement and the coefficient of repeatability is about half the width of this interval. Patterns of absolute and relative measures of test-retest reliability were similar for the analysis of data just from the HIV-infected cohort (data not shown).
Correspondence (convergent) validity – Association among neuropsychological tests
There were patterns of modest though statistically significant positive correlations between KABC Sequential scaled scores and TOVA ADHD and D-Prime baseline scores. Correlations ranged between 0.18 and 0.31 for the full sample and were slightly higher for the HIV positive group, ranging up to almost 0.4 for the TOVA D-prime (Table 3).
Table 3.
Spearman Correlations for the Association between Selected Baseline Neuropsychological Test Scores
| Test Outcome | Predictor | Full Sample | HIV Positive | HIV Uninfected | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| N | Correlation | P- Value |
N | Correlation | P- Value |
N | Correlation | P- Value |
|||||
| KABC Sequential | TOVA ADHD | 580 | 0.18 | <0.001 | * | 230 | 0.17 | 0.01 | * | 350 | 0.11 | 0.05 | * |
| TOVA D Prime | 580 | 0.31 | <0.001 | * | 230 | 0.37 | <0.001 | * | 350 | 0.18 | <0.001 | * | |
| TOVA D-prime standard score | 580 | 0.26 | <0.001 | * | 230 | 0.35 | <0.001 | * | 350 | 0.13 | 0.01 | * | |
| BRIEF BRI | TOVA Commission (%) | 580 | 0.06 | 0.18 | 230 | 0.10 | 0.13 | 350 | 0.02 | 0.74 | |||
| TOVA Omission (%) | 580 | −0.01 | 0.74 | 230 | −0.05 | 0.48 | 350 | −0.01 | 0.92 | ||||
| BRIEF MI | TOVA Commission (%) | 580 | 0.14 | <0.001 | * | 230 | 0.20 | 0.003 | * | 350 | 0.10 | 0.05 | |
| TOVA Omission (%) | 580 | 0.11 | 0.01 | * | 230 | 0.10 | 0.15 | 350 | 0.11 | 0.03 | * | ||
| KABC Planning | 285 | −0.09 | 0.15 | 120 | 0.02 | 0.82 | 165 | −0.11 | 0.17 | ||||
| KABC Mental processing index | 605 | −0.06 | 0.18 | 242 | −0.07 | 0.25 | 363 | −0.03 | 0.54 | ||||
| TOVA Response time variability (msec) | BOT-2: Total score | 582 | −0.29 | <0.001 | * | 231 | −0.36 | <0.001 | * | 351 | −0.21 | <0.001 | * |
| TOVA Response time (msec) | BOT-2: Total score | 582 | −0.24 | <0.001 | * | 231 | −0.26 | <0.001 | * | 351 | −0.20 | <0.001 | * |
| BRIEF Monitor | TOVA Commission (%) | 580 | 0.14 | <0.001 | * | 230 | 0.22 | <0.001 | * | 350 | 0.08 | 0.15 | |
| TOVA Omission (%) | 580 | 0.11 | 0.01 | * | 230 | 0.15 | 0.02 | * | 350 | 0.09 | 0.10 | ||
indicates p-value < 0.05
TOVA response time scores correlated negatively with the BOT-2 Total points score. The BRIEF global scales and TOVA error measures were either not significantly correlated or correlations were very low. The other pairwise correlations were low but significant and in the expected directions. Subgroup analyses of HIV-infected and uninfected children followed similar patterns. These relationships were supported by the adjusted regression parameter estimates, most of which were all significantly different from zero in the expected directions (Supplemental Table 3).
Construct validity – Association with predictors of neuropsychological functioning
TOVA and KABC scores were markedly lower for the HIV cohort in comparison to HEU and HUU (Table 4). There were strong and significant adjusted associations between individual measures of growth, disability and development with baseline KABC global scores (non-verbal, mental processing index; Table 4). Although these measures were also associated with the BRIEF GEC score, only the child development and disability scores were consistently associated in the expected directions. Strong and significant linear associations also held between individual indicators of socio-economic status and KABC global domains but largely not with BRIEF global scores (Supplemental Table 4). For the KABC non-verbal test, associations with growth measures were largely driven by the HIV uninfected study group (HEU/HU) (Supplemental Table 5) and this held true also for the associations between both KABC measures and socioeconomic indicators (data not shown).. TOVA D-prime and ADHD scores were associated with child development and disability when all participants were analyzed (Table 4) but in subgroup analyses, only child developmental scores were associated with these outcomes (Supplemental Table 5).
Table 4.
The Association between Selected Baseline Neuropsychological Test Scores and Participant Growth and Development Characteristics a
| KABC GLOBAL DOMAINS | BRIEF GLOBAL DOMAINS |
TOVA SELECTED TEST DOMAINS | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Predictor | Covariate/ Level |
NVI | MPI | GEC | ADHD | DPRIME-Standard | ||||||||||
|
| ||||||||||||||||
| Estim(SE) | P- Value |
Estim(SE) | P- Value |
Estim(SE) | P- Value |
Estim(SE) | P- Value |
Estim(SE) | P- Value |
|||||||
| Cohortb | HEU | 6.56 (1.08) | <0.001 | * | 6.29 (0.99) | <0.001 | * | −1.43 (1.15) | 0.21 | 1.09 (0.26) | <0.001 | * | 5.58 (1.26) | <0.001 | * | |
| HU | 7.14 (1.05) | <0.001 | * | 7.92 (1.00) | <0.001 | * | −2.35 (1.11) | 0.03 | * | 0.84 (0.26) | <0.001 | * | 5.31 (1.24) | <0.001 | * | |
| HIV | REF | REF | REF | REF | REF | |||||||||||
| HIV Status | HIV-infected | −6.85 (0.90) | <0.001 | * | −7.10 (0.83) | <0.001 | * | 1.89 (0.98) | 0.05 | −0.96 (0.22) | <0.001 | * | −5.44 (1.09) | <0.001 | * | |
| HIV-uninfect. | REF | REF | REF | REF | REF | |||||||||||
| WHO-BMI Z-score | continuousc | 0.77 (0.49) | 0.12 | 1.22 (0.47) | 0.01 | * | 0.98 (0.46) | 0.03 | * | −0.03 (0.12) | 0.82 | −0.70 (0.56) | 0.21 | |||
| WHO-Height Z-score | continuous | 2.60 (0.44) | <0.001 | * | 2.63 (0.42) | <0.001 | * | −1.09 (0.44) | 0.01 | * | 0.15 (0.11) | 0.16 | 1.57 (0.54) | 0.003 | * | |
| WHO-Weight Z-score | continuous | 2.39 (0.47) | <0.001 | * | 2.67 (0.46) | <0.001 | * | −0.22 (0.46) | 0.64 | 0.13 (0.12) | 0.27 | 0.70 (0.55) | 0.20 | |||
| Biological mom | No | −2.23 (1.70) | 0.19 | −3.12 (1.47) | 0.03 | * | 0.35 (2.41) | 0.89 | −0.95 (0.46) | 0.04 | * | −2.00 (1.99) | 0.31 | |||
| Yes | REF | REF | REF | REF | REF | |||||||||||
| Cgv less than 5 yrs | No | 0.22 (1.53) | 0.89 | 0.18 (1.47) | 0.90 | −1.15 (1.67) | 0.49 | 0.18 (0.34) | 0.59 | −2.23 (1.42) | 0.12 | |||||
| Yes | REF | REF | REF | REF | REF | |||||||||||
| Child, disability score | continuous | −0.25 (0.05) | <0.001 | * | −0.31 (0.04) | <0.001 | * | 0.41 (0.05) | <0.001 | * | −0.04 (0.01) | 0.002 | * | −0.14 (0.06) | 0.02 | * |
| Child, developmental score | continuous | 0.19 (0.04) | <0.001 | * | 0.18 (0.04) | <0.001 | * | −0.24 (0.04) | <0.001 | * | 0.03 (0.01) | 0.01 | * | 0.19 (0.04) | <0.001 | * |
Regression models adjusted for site, sex and age at entry; Each cell of the table represents results from a separate analysis
HIV=HIV-exposed and infected; HEU=HIV-exposed and uninfected; HU=HIV-unexposed and uninfected.
Continuous measure, parameter estimates change per additional unit.
indicates p-value < 0.05
Factor analyses
Distributional analysis indicated item-scores were not normally distributed (all Shapiro-Wilk p-values < 0.001). However, except for Gestalt closure, graphical analysis indicated approximate normality with slight kurtosis and skewness (Supplemental Figure 1a and Figure 1b). When we analyzed KABC-II baseline scores of all participants together, 47% of the total variance was explained by the four-factor solution. Factor 1 largely loaded on measures reflecting learning (Atlantis, Atlantis delay, Rebus, Rebus delay), factor 2 loaded on simultaneous processing (Block count, Rover) and planning (Pattern reasoning, Story completion); factor 3 loaded on sequential processing (Number recall, Word order) and factor 4 loaded on simultaneous processing (Triangles and Gestalt closure; Figure 2). These results also held for the analysis of HIV-infected participants alone and for the analysis of the uninfected group (HEU and HU combined; Table 5).
Figure 2.
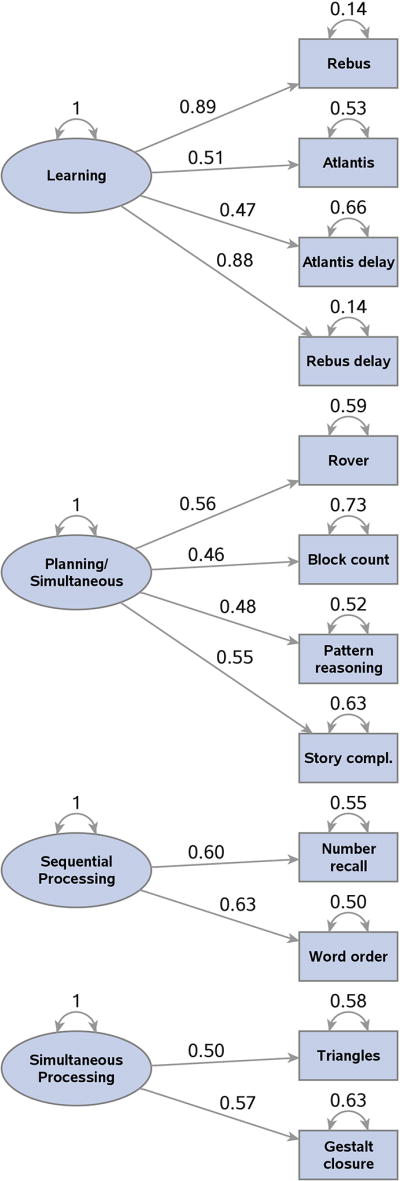
Factors and factor loadings for the exploratory factor analysis of scaled KABC items for all study participants.
Note: Factor loadings are only shown if 0.40 or over. The values by the curved arrowed lines indicate factor and error variance estimates. Factor variances are scaled to the value “1”. Factor interpretations are noted in the oval shapes; in order of the amount of total variance explained, they are: Learning, Planning (with Simultaneous), Sequential and Simultaneous processing. Values by the straight arrowed lines indicate factor loadings, which represents the correlation of the specific factor with the indicated KABC item. The square of the factor loading indicates the proportion of variance for that item accounted for by the specific factor. For example, the correlation between the factor representing Learning and Rebus is 0.89. The amount of variance of Rebus accounted for by the Learning factor is (.89)2= 79%. Error variances for the item scores indicate the proportion of total variance that is unique and not explained by the four common factors. For example, for Block count, 73% of the total variance is unique to that variable while 27% is common to the four factors (refer to manuscript Table 5 for the communalities).
Table 5.
Factor Analysis Results of Baseline KABC-II Scores, Overall and by Cohort (HIV-infected; HIV-uninfected)a
| Data Group | Variable | Factors | Communalityb | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | Factor1 | Factor2 | Factor3 | Factor4 | |||
| All Cohorts | 603 | Number recall | 0.03 | 0.03 | 0.60 | 0.29 | 0.45 |
| Word order | 0.20 | 0.21 | 0.63 | 0.13 | 0.50 | ||
| Hand movements | 0.11 | 0.26 | 0.39 | 0.17 | 0.26 | ||
| Block count | 0.14 | 0.46 | 0.16 | 0.11 | 0.27 | ||
| Rover | 0.29 | 0.56 | 0.10 | −0.06 | 0.41 | ||
| Triangles | 0.11 | 0.29 | 0.28 | 0.50 | 0.42 | ||
| Gestalt closure | 0.06 | 0.01 | 0.20 | 0.57 | 0.37 | ||
| Pattern reasoning | 0.28 | 0.48 | 0.23 | 0.34 | 0.48 | ||
| Story completion. | 0.22 | 0.55 | 0.08 | 0.12 | 0.37 | ||
| Atlantis | 0.51 | 0.31 | 0.31 | 0.14 | 0.47 | ||
| Rebus | 0.89 | 0.22 | 0.11 | 0.13 | 0.86 | ||
| Atlantis delay | 0.47 | 0.32 | 0.11 | −0.01 | 0.34 | ||
| Rebus delay | 0.88 | 0.25 | 0.08 | 0.13 | 0.86 | ||
|
|
|||||||
| % Common Variance | 38.78 | 25.77 | 20.66 | 14.79 | . | ||
| % Total Variance | 18.06 | 12.00 | 9.62 | 6.89 | 46.57 | ||
| Eigenvalue | 2.35 | 1.56 | 1.25 | 0.90 | 6.05 | ||
|
|
|||||||
| HIV-infected | 241 | Number recall | 0.01 | 0.04 | 0.61 | 0.38 | 0.52 |
| Word order | 0.22 | 0.15 | 0.67 | 0.12 | 0.54 | ||
| Hand movements | 0.14 | 0.32 | 0.33 | −0.01 | 0.23 | ||
| Block count | 0.13 | 0.53 | 0.16 | 0.22 | 0.37 | ||
| Rover | 0.35 | 0.61 | 0.17 | −0.05 | 0.52 | ||
| Triangles | 0.09 | 0.32 | 0.22 | 0.49 | 0.40 | ||
| Gestalt closure | −0.00 | −0.02 | 0.09 | 0.57 | 0.34 | ||
| Pattern reasoning | 0.29 | 0.51 | 0.13 | 0.27 | 0.43 | ||
| Story completion. | 0.19 | 0.64 | −0.00 | −0.04 | 0.45 | ||
| Atlantis | 0.48 | 0.24 | 0.31 | 0.15 | 0.41 | ||
| Rebus | 0.91 | 0.19 | 0.11 | −0.03 | 0.88 | ||
| Atlantis delay | 0.45 | 0.20 | 0.11 | 0.08 | 0.26 | ||
| Rebus delay | 0.90 | 0.25 | 0.07 | −0.01 | 0.88 | ||
|
|
|||||||
| % Common Variance | 38.71 | 28.03 | 19.10 | 14.16 | . | ||
| % Total Variance | 18.50 | 13.40 | 9.13 | 6.77 | 47.80 | ||
| Eigenvalue | 2.41 | 1.74 | 1.19 | 0.88 | 6.21 | ||
|
|
|||||||
| HIV-uninfected a (combined) | 362 | Number recall | 0.03 | −0.04 | 0.58 | 0.20 | 0.38 |
| Word order | 0.17 | 0.22 | 0.60 | 0.12 | 0.45 | ||
| Hand movements | 0.06 | 0.20 | 0.44 | 0.20 | 0.28 | ||
| Block count | 0.13 | 0.41 | 0.10 | 0.04 | 0.19 | ||
| Rover | 0.24 | 0.53 | 0.04 | −0.04 | 0.34 | ||
| Triangles | 0.12 | 0.25 | 0.30 | 0.52 | 0.44 | ||
| Gestalt closure | 0.09 | −0.04 | 0.23 | 0.56 | 0.38 | ||
| Pattern reasoning | 0.27 | 0.44 | 0.29 | 0.36 | 0.48 | ||
| Story completion. | 0.20 | 0.48 | 0.10 | 0.19 | 0.32 | ||
| Atlantis | 0.52 | 0.34 | 0.24 | 0.14 | 0.47 | ||
| Rebus | 0.87 | 0.24 | 0.12 | 0.18 | 0.86 | ||
| Atlantis delay | 0.48 | 0.40 | 0.05 | −0.05 | 0.39 | ||
| Rebus delay | 0.86 | 0.26 | 0.08 | 0.16 | 0.83 | ||
|
|
|||||||
| % Common Variance | 38.41 | 24.61 | 21.02 | 15.96 | . | ||
| % Total Variance | 17.12 | 10.97 | 9.37 | 7.11 | 44.57 | ||
| Eigenvalue | 2.23 | 1.43 | 1.22 | 0.92 | 5.79 | ||
HIV-uninfected combines HIV-exposed and uninfected (HEU) with HIV-unexposed and uninfected (HU)
The last two entries in the Communality column represent the percent of total variance and the total variance accounted for by all four factors
DISCUSSION
Despite demographic differences across six research sites in four countries speaking nine languages (including English), we were able to use a Western-based set of neuropsychological tests successfully in an African context with psychometrically valid and reliable outcomes yielding consistent findings across all study sites. Previously, we have shown that scores on these tests were lower in the HIV-infected cohort38 and these results were confirmed in this study. These results demonstrated acceptable testing consistency across 96 weeks for the KABC, TOVA, BRIEF and BOT-2.
Other researchers have noted moderate to high test-retest correlations at two to three weeks in three LMIC countries for KABC learning, sequential processing and planning subtests and tests equivalent to KABC simultaneous processing and TOVA measures of inattention and error rates5. In that study testing was repeated at two to three weeks, whereas in this study we repeated testing at 48 and 96 weeks. Although time intervals for the retesting differed, the test-retest reliability measures were comparable.
The lowest KABC intraclass correlations corresponded to subtests that have differing age bands. For example, among the KABC raw scores, Delayed recall is not usually administered to children if their original scores (Rebus and Atlantis) were low (< 4); but we administered these scores to all participants, which could have affected correlations with their scores when they were one year older (at week 48). It is also possible that their school status changed between the two study visits, which could also have influenced their learning and delayed recall abilities. On the other hand, conceptual thinking and face recognition were designed for children 7 years and under; these children may have reached a ceiling one year later (at the second study visit).
The test-retest analysis of just the HIV-infected cohort demonstrated substantially similar measures of relative agreement (correlations) as on the full set of study participants and absolute measures largely followed the same patterns, mitigating the concern that change in disease status might influence these results.
A recent study of rural, HIV-unexposed isi-Zulu-speaking South African children from seven to 11 years of age validated the factor structure of the KABC-II, focusing on eight subtests, two each from the learning, sequential, simultaneous and planning scales6. Factor analyses of the KABC scaled scores in our study discriminated the theoretical constructs, though explaining less of the total variation than in two previous African studies (over 50% of total variability), one study in healthy Zairian children, and a second in healthy South African children primarily from Soweto.3,39. A third study in Uganda, testing children with cerebral malaria, used the same subtests as in the current study, but analyzed raw scores, finding a five-factor solution discriminated among learning, simultaneous processing, sequential processing and planning26. In our four-factor analysis of all study participants, we found similar interpretations for the first three factors. Whereas Bangirana’s fourth factor loaded on planning, in our analysis, planning loaded on the second factor.. In all of these cited studies, staff administered the KABC in local languages. Modifications to account for cultural differences varied, including omitting certain test items which participants may not have been familiar with, omitting whole subtests and considering whether to modify time-based administration rules. These studies also reviewed important factors which could influence test-taking: children’s prior exposure to individualized testing, culturally distinct learning styles, differences in perceptual discrimination, and whether children are encouraged to complete tasks accurately rather than quickly.
As a measure of convergent validity, test results for similar domains correlated and regression analyses showed there were statistically significant associations in the expected directions. However, Spearman correlations were low. Since the regression analyses were adjusted for site, sex and age, we can only posit the unadjusted correlations might have been affected by measured or unmeasured cultural differences such as noted above.
Test results were correlated with expected health, growth, development, disability, and, for the KABC, socio-economic indicators. BRIEF scores were associated with child development and disability. Subgroup analyses did not show the same strength of association for the HIV-infected group as for the HIV-uninfected. This could have been due to loss of power resulting from smaller samples and or from actual differences between the groups.
In this study, tests and task and item instructions were spoken to the children as needed in their local language. Despite the manner in which the standardized administration of the tests could have been undermined by speaking the instructions in the local languages, the measures themselves were sensitive enough in their design, and proved highly adaptable to the various cultural and language contests in the present study. This may have been because of the ability to administer the evaluation with the provision of teaching sample items (KABC-II) for all of the subtests, a short practice session prior to testing (TOVA), and the modeling of motor tasks for all of the items (BOT-2). We acknowledge questions of cross-cultural validity in neuropsychological testing remain difficult ones in light of potential differences in social and learning experiences, understanding of test content and familiarity with test-taking2,3,11,12.
Our study was not without limitations. At the entry visit, the test battery for caregivers proved too lengthy to be completed in one day. Several of our analyses were of HIV-status subgroups, for which smaller sample sizes may have reduced the statistical power to distinguish significant effects. There were several conditions that could have influenced test scores for the same children across time: In some cases (fewer than 5%) the caregiver completing the BRIEF at week 0 differed from that completing it at week 48 and 96; there may have been practice effects of repeated tests; HIV-infected children’s changes in health or stability could have influenced their test-taking abilities differently at different study visits. In our factor analysis of KABC scores, we used item scores which were normed to the US population. Since data on the 13 KABC items were not strictly normally distributed, we should treat our results as exploratory findings. The BRIEF instrument may be especially susceptible to bias derived from using non-local scoring norms. Further analyses are planned to develop local norms in these four African countries using the P1104S HU cohort data, recognizing these analyses may still yield tentative results due to the small sample sizes of population subgroups categorized by age, sex at birth and ethnicity/language.
CONCLUSIONS AND IMPLICATIONS
We found the KABC, TOVA, BRIEF and BOT-2 to be valid and reliable when using standardized scores from high-income countries in a study of HIV infected and uninfected perinatally exposed and unexposed children at six research sites in four sub-Saharan African countries. Yet, further research into adapting tests developed in high income Western settings for LMIC contexts is also warranted.
Boivin and Giordani (2009) proposed the concept of a brain/behavior omnibus as a way to conceptually interface foundational neuropsychological functions21. This approach suggests that foundational brain/behavior functions are universal to human neurodevelopment, and therefore, consistent across cultures. However, this approach also recognizes that the neuropsychological assessment of these functions must be sensitive to how such foundational brain/behavior domains are shaped by ecological necessity and cultural experience. The robust validity and reliability of our application of a Western-based neuropsychological assessment battery to evaluate the brain/behavior effects of pediatric HIV across six different study sites representing nine different local languages in four different countries supports this premise.
Neuropsychological measurement can be used to evaluate the extent to which the integrity of the foundational brain/behavior domains is consistently compromised across settings in a given manner for a given disease (for example, HIV). Likewise, these measures can also be used to evaluate improvement in function, given health interventions.
We need to continue to develop more sensitive and innovative technologies within the cross-cultural neuropsychology of African children, As these technologies become increasingly accessible to resource-constrained settings such as those represented in the present study, we will gain a wealth of information that lends interpretive power for a dynamic biocultural co-constructivist paradigm (demonstrating biocultural reciprocity and plasticity) as applied to the neuropsychology of African children. Western-based tests, which have been adapted for use in culturally sensitive, effective, and appropriate manners, will yield valuable results and will, along with dynamic testing, neuroimaging and genomic analyses, help us characterize the foundational universal brain/behavior domains.
Supplementary Material
Supplementary Figure 1a and Figure 1b. Frequency distributions for the 13 KABC-II scaled item scores used in the factor analysis. Normal density curves overlay the frequency histograms. Mean and standard deviations are indicated. The cells in Figure 1a illustrate the first eight KABC-II items (Number recall, Word order, Hand movements, Block count, Rover, Triangles, Gestalt closure and Pattern reasoning) and the cells in Figure 1b illustrate the remaining five items (Story completion, Atlantis, Rebus, Atlantis delay, Rebus delay).
Acknowledgments
Overall support for the International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT) Network was provided by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health (NIH) under Award Numbers UM1AI068632 (IMPAACT LOC), UM1AI068616 (IMPAACT SDMC) and UM1AI106716 (IMPAACT LC), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We would like to thank Meredith Warshaw and Stan Morse for carefully reading the manuscript and reviewer comments, Katie McCarthy and J.L. Ariansen for clinical trials support. We would like to thank the protocol medical officers, Pim Brouwers and Sonia Lee for their contributions. The following institutions and individuals participated in IMPAACT P1104S: 8051, Wits Reproductive Health and HIV Institute (Wits RHI) Shandukani Research Center CRS, University of the Witwatersrand, Johannesburg: South Africa: Janet Grab, Gurpreet Kindra; 8052, Soweto IMPAACT CRS, Perinatal HIV Research Unit (PHRU), Chris Hani Baragwanath Hospital, Johannesburg, South Africa: Given Leshabane, Hilda Ndiweni; 8950, Family Clinical Research Unit (FAM-CRU) Clinical Research Site (CRS), Tygerberg Hospital, Tygerberg, South Africa: Joan du Plessis, Marisa Groenewald; 30293, Makerere University – Johns Hopkins University (MU-JHU) Research Collaboration (MUHJU CARE LTD) CRS, Kampala, Uganda: Linda Barlow-Mosha; Mary Nyakato; 31890 (30313), Harare Family Care CRS, Parirenyatwa Hospital, Harare, Zimbabwe:; Mary N Tichareva, Petronella Matibe; 12001, University of North Carolina (UNC) Project, Tidziwe Centre, Kamuzu Central Hospital, Lilongwe, Malawi: Mary Chiunda, Tionge Kamvaunamwali,
References
- 1.Boivin MJ, Giordani B. Neuropsychological assessment of African children: evidence for a universal brain/behavior omnibus within a coconstructivist paradigm. Progress in brain research. 2009;178:113–135. doi: 10.1016/S0079-6123(09)17808-1. [DOI] [PubMed] [Google Scholar]
- 2.Sternberg RJ. Culture and intelligence. American Psychologist. 2004;59:325–338. doi: 10.1037/0003-066x.59.5.325. [DOI] [PubMed] [Google Scholar]
- 3.Giordani B, Boivin MJ, Opel B, Dia Nseyila DN, Lauer RE. Use of the K-ABC with children in Zaire, Africa: An evaluation of the sequential-simultaneous processing distinction within an intercultural context. International Journal of Disability, Development and Education. 1996;43(1):5–24. [Google Scholar]
- 4.Abubakar A, van de Vijver FJR. How to adapt tests for Sub-Saharan Africa. van de Vijver FJR, editor. Handbook of Applied Developmental Science in Sub-Saharan Africa Abubakar, A. 2017;Chapter 11:197–212. XVIII; http://www.springer.com/978-1-4939-7326-2.
- 5.Holding P, Anum A, van de Vijver FJ, et al. Can we measure cognitive constructs consistently within and across cultures? Evidence from a test battery in Bangladesh, Ghana, and Tanzania. Applied neuropsychology Child. 2016:1–13. doi: 10.1080/21622965.2016.1206823. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell JM, Tomlinson M, Bland RM, Houle B, Stein A, Rochat TJ. Confirmatory factor analysis of the Kaufman assessment battery in a sample of primary school-aged children in rural South Africa. South African Journal of Psychology. 2017 Nov 17; doi: 10.1177/0081246317741822. Article first published online, [DOI]
- 7.Paper presented at: Cognition Workshop. Institute of Education; London: Jul 23–24, 2013. Save-the-children. Cognition Workshop Report. 2013. [Google Scholar]
- 8.Bangirana P, John CC, Idro R, et al. Socioeconomic predictors of cognition in Ugandan children: implications for community interventions. PloS one. 2009;4(11):e7898. doi: 10.1371/journal.pone.0007898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brahmbhatt H, Boivin M, Ssempijja V, et al. Impact of HIV and Atiretroviral Therapy on Neurocognitive Outcomes Among School Aged Children. Journal of acquired immune deficiency syndromes (1999) 2017 doi: 10.1097/QAI.0000000000001305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogunlade AO, Kruger HS, Jerling JC, et al. Point-of-use micronutrient fortification: lessons learned in implementing a preschool-based pilot trial in South Africa. International journal of food sciences and nutrition. 2010:1–16. doi: 10.3109/09637486.2010.495710. [DOI] [PubMed] [Google Scholar]
- 11.Semrud-Clikeman M, Romero RA, Prado EL, Shapiro EG, Bangirana P, John CC. Selecting measures for the neurodevelopmental assessment of children in low- and middle-income countries. Child neuropsychology. 2017 Oct;23(7):761–802. doi: 10.1080/09297049.2016.1216536. Epub 2016 Sep 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Wyhe KS, van de Water T, Bouivin MJ, Cotton MF, Thomas KGF. Cross-cultural assessment of HIV-associated neurocognitive impairment using the Kaufman Assessment Battery for Children: A systematic review. J Int AIDS Society. 2017;20(1):1–11. doi: 10.7448/IAS.20.1.21412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bangirana P, Allebeck P, Boivin MJ, et al. Cognition, behaviour and academic skills after cognitive rehabilitation in Ugandan children surviving severe malaria: a randomised trial. BMC neurology. 2011;11:96. doi: 10.1186/1471-2377-11-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bangirana P, Sikorskii A, Giordani B, Nakasujja N, Boivin MJ. Validation of the CogState battery for rapid neurocognitive assessment in Ugandan school age children. Child and adolescent psychiatry and mental health. 2015;9:38. doi: 10.1186/s13034-015-0063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boivin MJ, Busman RA, Parikh SM, et al. A pilot study of the neuropsychological benefits of computerized cognitive rehabilitation in Ugandan children with HIV. Neuropsychology. 2010;24(5):667–673. doi: 10.1037/a0019312. [DOI] [PubMed] [Google Scholar]
- 16.Familiar I, Ruisenor-Escudero H, Giordani B, et al. Use of the Behavior Rating Inventory of Executive Function and Child Behavior Checklist in Ugandan Children with HIV or a History of Severe Malaria. Journal of developmental and behavioral pediatrics : JDBP. 2015;36(4):277–284. doi: 10.1097/DBP.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaufman AS, Kaufman NL. Kaufman Assessment Battery for Chidlren. Second. San Antonio Tx: Pearson Inc NCS Pearson; 2004. [Google Scholar]
- 18.The T.O.V.A. (Version 6.X) (Computer Program) [computer program] Los Alamitos, CA: 1993. [Google Scholar]
- 19.Bruininks RH, Bruininks BD. BOT2: Bruininks-Oseretsky Test of Motor Proficiency. Second. Minneapolis, MN: Pearson Assessments; 2005. [Google Scholar]
- 20.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function® (BRIEF®) Lutz, FL: Psychological Assessment Resources (PAR); 2003. [Google Scholar]
- 21.Boivin MJ, Giordani B. Neuropsychological assessment of African children: evidence for a universal basis to cognitive ability. In: Chiao JY, editor. Cultural Neuroscience: Cultural Influences on Brain Function. Vol. 178. New York, NY: Elsevier Publications; 2009. pp. 113–135. [DOI] [PubMed] [Google Scholar]
- 22.Neuropsychology of Children in Africa: Perspectives on Risk and Resilience. In: Boivin MJ, Giordani B, editors; Fletcher-Janzen E, editor. Specialty Topics in Pediatric Neuropsychology. 1 New York, NY: Springer; 2013. [Google Scholar]
- 23.Boivin MJ, Barlow-Mosha L, Chernoff MC, et al. Neuropsychological performance in African children with HIV enrolled in a multisite antiretroviral clinical trial. Aids. 2018;32(2):189–204. doi: 10.1097/QAD.0000000000001683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barlow-Mosha L, Angelidou K, Lindsey J, et al. Nevirapine- Versus Lopinavir/Ritonavir-Based Antiretroviral Therapy in HIV-Infected Infants and Young Children: Long-term Follow-up of the IMPAACT P1060 Randomized Trial. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2016;63(8):1113–1121. doi: 10.1093/cid/ciw488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bangirana P, Giordani B, John CC, Page C, Opoka RO, Boivin MJ. Immediate neuropsychological and behavioral benefits of computerized cognitive rehabilitation in Ugandan pediatric cerebral malaria survivors. Journal of developmental and behavioral pediatrics : JDBP. 2009;30(4):310–318. doi: 10.1097/DBP.0b013e3181b0f01b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bangirana P, Seggane M, Allebeck P, et al. A preliminary examination of the construct validity of the KABC-II in Ugandan children with a history of cerebral malaria. African health sciences. 2009;9(3):186–192. [PMC free article] [PubMed] [Google Scholar]
- 27.Bergemann TL, Bangirana P, Boivin MJ, Connett JE, Giordani BJ, John CC. Statistical approaches to assess the effects of disease on neurocognitive function over time. J Biomet Biostat. 2012;(S7:016):1–8. doi: 10.4172/2155-6180.S7-016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boivin MJ, Bangirana P, Byarugaba J, et al. Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics. 2007;119(2):e360–366. doi: 10.1542/peds.2006-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.John CC, Bangirana P, Byarugaba J, et al. Cerebral malaria in children is associated with long-term cognitive impairment. Pediatrics. 2008;122(1):e92–99. doi: 10.1542/peds.2007-3709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deitz JC, Kartin D, Kopp K. Review of the Bruininks-Oseretsky Test of Motor Proficiency, Second Edition (BOT-2) Physical & occupational therapy in pediatrics. 2007;27(4):87–102. [PubMed] [Google Scholar]
- 31.Gioia GA, Isquith PK, Retzlaff PD, Espy KA. Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function (BRIEF) in a clinical sample. Child neuropsychology : a journal on normal and abnormal development in childhood and adolescence. 2002;8(4):249–257. doi: 10.1076/chin.8.4.249.13513. [DOI] [PubMed] [Google Scholar]
- 32.UNICEF. [Accessed March 14, 2017];Multiple Indicator Cluster Surveys. 2017 http://mics.unicef.org/
- 33.Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21(9):1331–1335. doi: 10.1002/sim.1108. [DOI] [PubMed] [Google Scholar]
- 34.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 35.Vaz S, Falkmer T, Passmore AE, Parsons R, Andreou P. The case for using the repeatability coefficient when calculating test-retest reliability. PloS one. 2013;8(9):e73990. doi: 10.1371/journal.pone.0073990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boivin MJ, Chounramany C, Giordani B, Xaisida S, Choulamountry L. Validating a cognitive ability testing protocol with Lao children for community development applications. Neuropsychology. 1996;10(4):588–599. [Google Scholar]
- 37.Holding P, Boivin MJ. The Assessment of neuropsychological outcomes in pediatric severe malaria. In: Boivin MJ, Giordani B, editors. Neuropsychology of Children in Africa: Perspectives on Risk and Resilience. NY: Springer Science+Business; 2013. [Google Scholar]
- 38.Boivin M, Chernoff M, Laughton B, et al. Neuropsychological outcomes in a two year African-based pediatric observational study; Conference on Retroviruses and Opportunistic Infections (CROI); Feb 13–16, 2017; Seattle, Washington. 2017. 2017. [Google Scholar]
- 39.Jansen P, Greenop K. Factor analyses of the Kaufman Assessment Battery for Children assessed longitudinally at 5 and 10 years. South African Journal of Psychology. 2008;38(2):335–365. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1a and Figure 1b. Frequency distributions for the 13 KABC-II scaled item scores used in the factor analysis. Normal density curves overlay the frequency histograms. Mean and standard deviations are indicated. The cells in Figure 1a illustrate the first eight KABC-II items (Number recall, Word order, Hand movements, Block count, Rover, Triangles, Gestalt closure and Pattern reasoning) and the cells in Figure 1b illustrate the remaining five items (Story completion, Atlantis, Rebus, Atlantis delay, Rebus delay).