Abstract
Women involved in the criminal justice system (WICJ) are at high risk of acquiring HIV and would benefit from HIV pre-exposure prophylaxis (PrEP) but there are no studies in this population to inform PrEP implementation programs. We conducted a cross-sectional survey of HIV-uninfected, cis-gender women on probation, parole and/or recently released from prison/jail to assess PrEP awareness, eligibility, potential barriers to uptake, and the PrEP care continuum. The 125 WICJ surveyed reported high rates of HIV risk behaviors including recent transactional sex (22.4%) and unsafe injection practices (14.4%). Despite 33% (n=42) meeting eligibility criteria for PrEP, only 25% were aware of PrEP and one person was currently using it. Just 16.7% of those who were PrEP eligible perceived they were at risk for HIV. Following a brief explanation of PrEP, 90% said they would try it if recommended by their physician. Compared to those not PrEP eligible (n=83), PrEP eligible women were less likely to be stably housed or have a primary care provider, and were more likely to be violence-exposed, charged with drug possession, have lifetime substance use, or living with Hepatitis C infection. WICJ frequently engage in HIV risk behaviors that make them eligible for PrEP. Uptake may be limited by lack of PrEP awareness or underestimation of personal HIV risk. WICJ report receptiveness to PrEP and represent an important population for targeted PrEP implementation programs.
Keywords: HIV, PrEP, women, criminal justice, probation, risk
Introduction
The United States incarcerates more women than any other country worldwide (International Center for Prison Studies, 2014), though most CJ-involvement is through community-based supervision, including probation and parole (Kaeble & Glaze, 2016). Women involved in the criminal justice system (WICJ) experience disparately high rates of HIV with comorbid chronic Hepatitis C (HCV) and opioid use disorders, compared to both non-CJ involved women and men involved in the criminal justice system (MICJ) (Baillargeon et al., 2003; Meyer, Springer, & Altice, 2011). Although being in a correctional facility can precipitate risk, WICJ and MICJ more often acquire HIV outside of prison (Center for Disease Control, 2015). Compared to men, community-based WICJ have increased HIV risk related to transactional sex, injection drug and other substance use, and socioeconomic conditions, including unstable housing (Hearn, Whitehead, Khan, & Latimer, 2015).
HIV prevention for WICJ has centered on reducing risky behaviors and recidivism through psychoeducational interventions and linkage to care post-release (Lichtenstein & Malow, 2010; Meyer et al., 2011). WICJ have the most agency over condom use and injection practices, but both often require negotiation with sex and drug use partners, thereby increasing potential exposure to intimate partner violence (IPV) (El-Bassel, Terlikbaeva, & Pinkham, 2010). Pre-exposure prophylaxis (PrEP) is a critical HIV prevention strategy for WICJ because it is highly effective and fully user-controlled.
An efficacy-effectiveness gap in PrEP’s impact on women needs to be addressed by translational studies (Adimora, 2016). An estimated 468,000 U.S. women meet clinical criteria for PrEP based on sexual risk, and at least 10,000 women based on injection drug use (Iversen, Page, Madden, & Maher, 2015; Smith et al., 2015). Yet just 18,812 women have received Truvada® (TDF/FTC) as PrEP since 2012 and they were disproportionately non-Hispanic White, which poorly reflects the HIV epidemic (Mera et al., 2016). In 2016, the World Health Organization (WHO) expanded recommendations for PrEP to include all individuals “at substantial risk of HIV infection” (World Health Organization, 2016). In diverse settings, women are consistently unaware of PrEP and misestimate personal HIV risk (Auerbach, Kinsky, Brown, & Charles, 2015; Elopre, Kudroff, Westfall, Overton, & Mugavero, 2017; Garfinkel, Alexander, McDonald-Mosley, Willie, & Decker, 2017; Garnett et al., 2016; Jayakumaran, Aaron, Gracely, Schriver, & Szep, 2016; Koechlin et al., 2017).
To our knowledge, there have been no published studies on PrEP in CJ-involved populations. The purpose of this study is to characterize the PrEP care continuum among WICJ, including PrEP knowledge, eligibility, acceptance, and barriers, to inform the development of PrEP interventions for WICJ (A. S. Nunn et al., 2017).
Methods
Study Design and Setting
A cross-sectional survey of WICJ in Connecticut was conducted over six months (2016-2017.) The state has an integrated system of prisons and jails overseen by the Department of Corrections (DOC), housing approximately 1200 women in a single facility; PrEP is not available during incarceration. Another 9,000 women statewide are on probation through the Court Support Services Division (CSSD), including 750 women classified as “high risk offenders” (CT Department of Correction, 2017). Publicly available data are not disaggregated by both gender and county. Study participants were recruited from a mid-sized city in southern Connecticut with a high population of returning prisoners and jail detainees.
Study Sample and Data Collection
We purposively recruited HIV-uninfected WICJ from probation and parole offices, community-based “alternatives to incarceration” programs, clinics, transitional housing, residential drug treatment, and drug treatment centers. Site personnel were briefed on study objectives and inclusion criteria and could refer potential participants to the study coordinator. Interested individuals could also self-refer through a secured private dedicated phone line. Participants were screened by phone or in person by a single researcher (RR); all who completed screening met eligibility criteria and enrolled in the study. Surveys were administered via tablet by RR in English in a private setting on-site at partner organizations or research offices. Surveys lasted ~30 minutes and participants were compensated with a $20 gift card.
Inclusion Criteria and Informed Consent
Eligibility criteria included: 1) self-identification as a woman; 2) self-reported HIV-uninfected; 3) ≥18 years of age; 4) on probation, parole, intensive pre-trial supervision or released from prison/jail in the past 60 days; and 5) ability to provide written informed consent. All study procedures were approved by the Yale University IRB and the research advisory board at the APT Foundation, Inc.
Survey Development and Piloting
Prior to recruitment, the survey was piloted for clarity with WICJ, experts in HIV care in CJ settings, and community-based outreach workers with whom the study team has a history of collaboration. Based on feedback, the survey was revised. The final version of the survey is available in the Appendix.
Study Measures
Demographic characteristics
Demographic characteristics included age, race, ethnicity, education, employment status, and household income. Housing status was categorized as unstable if the participant answered “transitional housing or a halfway house,” “hotel, motel, or guesthouse,” or “homeless/on the streets” and stable if the participant reported living in a house or apartment with other people or by herself (Health Resources and Services Administration, 2011). Referral source was categorized as drug treatment center, transitional housing program, clinic, or other site. We assessed CJ-involvement, including lifetime incarcerations, current charges, and time since last prison- or jail-release.
Healthcare utilization
Participants were asked if they had a primary care provider (PCP) or insurance, and quantified healthcare visits in the past 6 months.
Risk behaviors
Participants were asked if they had engaged in transactional sex in the past 12 months (exchanging food, goods, housing or money for sex), drug injection in the past 6 months and shared equipment or been secondarily injected. Participants reported number and HIV serostatus of sex partners in the past 12 and 6 months, respectively. Lifetime and past 30-day substance use were determined by the NIDA Risk Behavior Assessment (Community Research Branch, 1993).
PrEP eligibility
PrEP eligibility was defined by the following criteria: 1) “high number of sex partners” in one year (≥4 partners); 2) transactional sex in the past 12 months; 3) sex with an HIV+ partner in the past 6 months; or 4) injection drug use with unsafe injecting behaviors (US Public Health Service, 2014).
PrEP awareness
After providing a brief explanation of PrEP, participants were asked, “Before today had you ever heard about PrEP or Truvada®?”
Receptiveness to PrEP
Receptiveness to PrEP was determined from three questions (Appendix; BEL_1, BEL_2, BEL_3). All affirmative responses were coded as “high PrEP receptiveness” and all “undecided” and negative responses were coded as “low PrEP receptiveness.”
Potential barriers to PrEP uptake
Potential barriers to PrEP uptake were evaluated using a novel tool informed by the Organizational Readiness for Change Model (Weiner, 2009) and the Behavioral Health Model for Vulnerable Populations (Gelberg, Andersen, & Leake, 2000), which describe enabling or disabling factors, task demands, resource availability, and situational factors drive health behaviors (PrEP use). Measures included perceptions of PrEP, HIV beliefs, and perceived safety of PrEP (Appendix; BEL_5, HR_1b). We evaluated lifetime HIV risk and other factors that might affect PrEP use: access to transportation for medical visits, lifetime and 6-month exposure to physical, sexual, or emotional IPV, and lifetime medical comorbidities including HCV and sexually transmitted infections (STIs).
HIV and STI risk perception
HIV and STI risk perception was assessed in terms of personal and partners’ HIV and STI risk in 12 months.
Data Analysis
All analyses were conducted using SPSS (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp). We performed descriptive statistics, calculating proportions for categorical variables and means (with standard deviations) or medians (with interquartile ranges) for continuous variables. We compared all characteristics stratified by PrEP eligibility, using Pearson’s chi-squared or Fisher’s exact tests for categorical variables, Student’s t-tests to compare means, and Mann-Whitney U tests to compare medians. Levene’s test confirmed homogeneity of variances.
Results
Demographic Characteristics
We enrolled 125 HIV-uninfected WICJ with a mean age of 37 years old (Table 1.) The sample was moderately racially diverse with 59% identifying as White, 22.4% identifying as Black, and 18.4% identifying as another or mixed races. Most (64.8%) completed high school or less. One-third of participants were unstably housed, 83.2% were unemployed, and the mean annual household income was $7,834. Participants were incarcerated a mean 4.4 times (SD=5.6) in their lives, and were charged with property (41.6%), drug-related (39.2%), or public disorder offenses (38.4%). Most had state or publicly funded insurance (88.8%) and a PCP (65.6%), with highly comorbid HCV (24.8%), STIs (32.8%), and depression (83.2%). Nearly half were recently exposed to IPV. Lifetime substance use rates were high.
Table 1.
Demographic Characteristics of Study Sample, by PrEP Eligibility (N=125)
| Characteristic | Total (N=125) | PrEP eligible (n=42) | Not PrEP eligible (n=83) | p-value |
|---|---|---|---|---|
| Age (mean, SD, SE) | (37.1, 11.0, 1.0) | (35.1, 8.4, 1.3) | (38.1, 12.1, 1.3) | 0.16 |
| Race, n (%) | 0.28 | |||
| White | 74 (59.2) | 29 (69.0) | 45 (54.2) | |
| Black | 28 (22.4) | 7 (16.6) | 21 (25.3) | |
| Other | 23 (18.4) | 6 (14.3) | 17 (20.5) | |
| Education, n (%) | 0.38 | |||
| High school | 81 (64.8) | 25 (59.5) | 56 (67.5) | |
| Post-secondary education | 44 (35.2) | 17 (40.5) | 27 (32.5) | |
| Housing Status, n (%) | 0.024 | |||
| Unstable | 47 (37.6) | 32 (76.2) | 46 (55.4) | |
| Stable | 78 (62.4) | 10 (23.8) | 37 (44.6) | |
| Referral Source, n (%) | 0.887 | |||
| Drug Treatment | 75 (60.0) | 24 (57.1) | 51 (61.4) | |
| Transitional Housing | 34 (27.2) | 12 (28.6) | 22 (26.5) | |
| Clinic /Other | 16 (12.8) | 6 (14.3) | 10 (12.0) | |
| Employment status, n (%) | 0.285 | |||
| Unemployed | 104 (83.2) | 37 (88.1) | 66 (79.5) | |
| Employed | 21 (16.8) | 5 (11.9) | 16 (19.3) | |
| Annual household Income (mean, median, IQR) | (7834.2, 2352, 10,200) | (5116, 2328, 8748) | (9244, 2400, 10164) | 0.165 |
| Lifetime # incarcerations (mean, SD) | (4.37, 5.6) | (5.07, 6.5) | (4.01, 5.0) | 0.317 |
| Current charges, n (%) | ||||
| Person Crimes | 28 (22.4) | 10 (23.8) | 18 (21.7) | 0.788 |
| Property Crimes | 52 (41.6) | 17 (40.5) | 35 (42.2) | 0.856 |
| Drug Possession | 49 (39.2) | 22 (52.4) | 27 (32.5) | 0.032 |
| Public Disorder | 48 (38.4) | 20 (47.6) | 28 (33.7) | 0.132 |
| Domestic Violence | 22 (17.6) | 5 (11.9) | 17 (20.5) | 0.234 |
| Other | 43 (34.4) | 10 (23.8) | 33 (39.8) | 0.076 |
| Months since last prison-release (mean, SD) | n=91 (14.9, 26.9) | n=65 (17.4, 30.6) | n=26 (8.7, 12.2) | 0.161 |
| Health insurance status, n (%) | 0.455 | |||
| Medicaid/Medicare only | 111 (88.8) | 38 (90.5) | 73 (88.0) | |
| Other Insurance | 11 (8.8) | 4 (9.5) | 7 (8.4) | |
| No Insurance | 3 (2.4) | 0 (0) | 3 (3.6) | |
| Has a primary care provider | 82 (65.6) | 23 (54.8) | 59 (71.2) | 0.07 |
| Comorbidities, n (%) | ||||
| STIs | 41 (32.8) | 15 (35.7) | 26 (31.3) | 0.622 |
| HCV | 31 (24.8) | 16 (38.1) | 15 (18.1) | 0.014 |
| Depression | 104 (83.2) | 37 (88.1) | 67 (80.7) | 0.298 |
| Recent IPV exposure, n (%) | 50 (40) | 25 (59.5) | 25 (30.1) | 0.002 |
PrEP=pre-exposure prophylaxis; STIs= sexually transmitted infections; HCV= Hepatitis C; IPV= intimate partner violence
PrEP and HIV-related beliefs and behaviors
Many (46.4%) WICJ had received ≥1 HIV test within the past 6 months. Only 8% perceived personal risk for HIV, 9.6% perceived partner risk for HIV, and 9.6% perceived personal STI risk in the next 12 months.
One-quarter of participants were familiar with PrEP and one was taking PrEP in a clinical trial. After receiving brief information about PrEP, 90.4% were receptive to taking it if recommended by their doctor. Primary concerns about PrEP were side effects (70.4%), drug interactions (57.6%) and fear about incomplete effectiveness (57.6%). In terms of PrEP eligibility, 22.4% had engaged in transactional sex in the past 12 months, 14.4% had engaged in unsafe injection practices in the past 6 months, 16.8% had had ≥4 sex partners in the past 12 months and 0.8% had had an HIV+ sex partner in the past 6 months, resulting in 33.6% (n=42) meeting criteria for PrEP eligibility.
Characteristics by PrEP Eligibility
There were no significant differences between those who were (n=42) and were not PrEP eligible (n=83) in terms of race, education, employment status, median income, time since last prison release, or insurance status (Tables 1 and 2). Compared to those ineligible, PrEP eligible women were significantly less often stably housed (23.8 vs. 44.6%; p=0.024) and more likely to: have a current drug charge (52.4% vs. 32.5%; p=0.032), have HCV (38.1 vs. 18.1%; p=0.014), be recently IPV-exposed (59.5 vs. 30.1% ; p=0.002), perceive HIV risk (16.6 vs. 3.6%; p=0.011), perceive STI risk (16.6 vs. 6.0%; p=0.011), and have lifetime substance use.
Table 2.
PrEP perception, HIV beliefs and testing behaviors and substance use, by PreP Eligibility (N=125)
| Characteristic | Total (N=125) | PrEP eligible (n=42) | Not PrEP eligible (n=83) | p-value |
|---|---|---|---|---|
| Time Since Last HIV Test n (%) | 0.05 | |||
| 0–6 months | 87 (69.6) | 34 (81.0) | 53 (63.9) | |
| 6+ months | 38 (30.4) | 8 (19.0) | 30 (36.1) | |
| Perceive HIV risk in next 12 months, n (%) | 0.011 | |||
| Yes | 10 (8.0) | 7 (16.7) | 3 (3.6) | |
| No | 115 (92.0) | 35 (83.3) | 80 (96.4) | |
| Perceive partner’s HIV risk in next 12 months | 12 (9.6) | 5 (11.9) | 7 (8.4) | 0.534 |
| Perceive STI risk, n (%) | 0.056 | |||
| Yes | 12 (9.6) | 7 (16.6) | 5 (6.0) | |
| No | 113 (90.4) | 35 (83.3) | 78 (94.0) | |
| Agree HIV is a serious risk to health/well-being, n (%) | 121 (96.8) | 41 (97.6) | 80 (96.4) | 0.711 |
| Agree one can tell if a person has HIV, n (%) | 4 (3.2) | 1 (2.4) | 3 (3.6) | 0.711 |
| Agree condom use after condomless sex is “pointless”, n (%) | 8 (6.4) | 2 (4.8) | 6 (7.2) | 0.595 |
| Believe HIV can be cured, n (%) | 24 (19.2) | 6 (14.3) | 18 (21.7) | 0.321 |
| Familiar with PrEP, n (%) | 32 (25.6) | 13 (31.0) | 19 (22.9) | 0.329 |
| Currently taking PrEP, n (%) | 1 (0.8) | 0 | 0 | --- |
| PrEP Receptiveness, n (%) | 113 (90.4) | 39 (92.9) | 74 (89.2) | 0.507 |
| Lifetime Substance use | N=100 | n=29 | n=71 | |
| Cocaine* | 83 (83) | 28 (96.6) | 55 (77.5) | 0.020 |
| Amphetamine | 22 (22) | 12 (41.4) | 10 (14.1) | 0.003 |
| Hallucinogens | 49 (49) | 19 (65.5) | 30 (42.3) | 0.035 |
| Opiates | 64 (64) | 22 (75.9) | 42 (59.2) | 0.114 |
| Heroin* | 70 (70) | 25 (86.2) | 45 (63.4) | 0.030 |
| Barbiturates* | 6 (6) | 1 (3.4) | 5 (7.0) | 0.669 |
| Benzodiazepines | 56 (56) | 20 (69.0) | 36 (50.7) | 0.095 |
| Sleep Medications | 16 (16) | 6 (20.7) | 10 (14.1) | 0.414 |
| Cannabis* | 92 (92) | 27 (93.1) | 65 (91.5) | 1.0 |
| Inhalants | 9 (9) | 5 (17.2) | 4 (5.6) | 0.066 |
| Other* | 15 (15) | 4 (15.4) | 11 (15.5) | 1.0 |
Fisher’s Exact Ratio
Figure 1 demonstrates the PrEP care continuum in the study sample. Of participants who were eligible to take PrEP (n=42), all were insured but only 55% had a PCP; 31% were aware of PrEP; 93% were receptive to PrEP; and none were currently taking PrEP.
Figure 1.
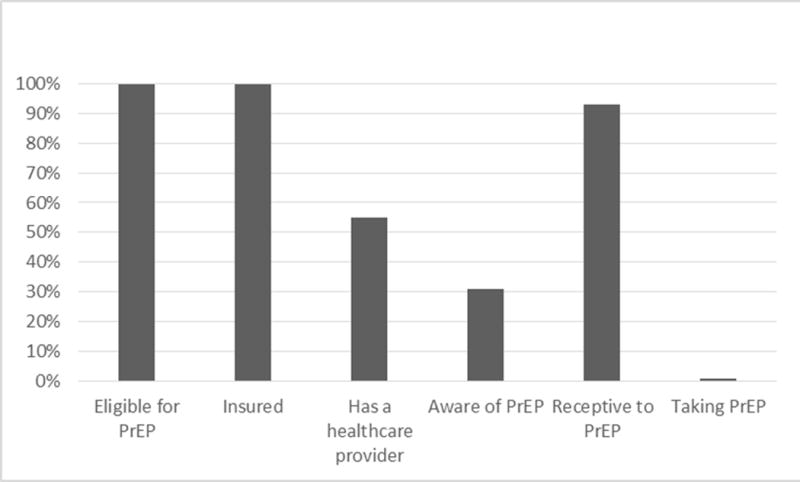
PrEP Care Continuum
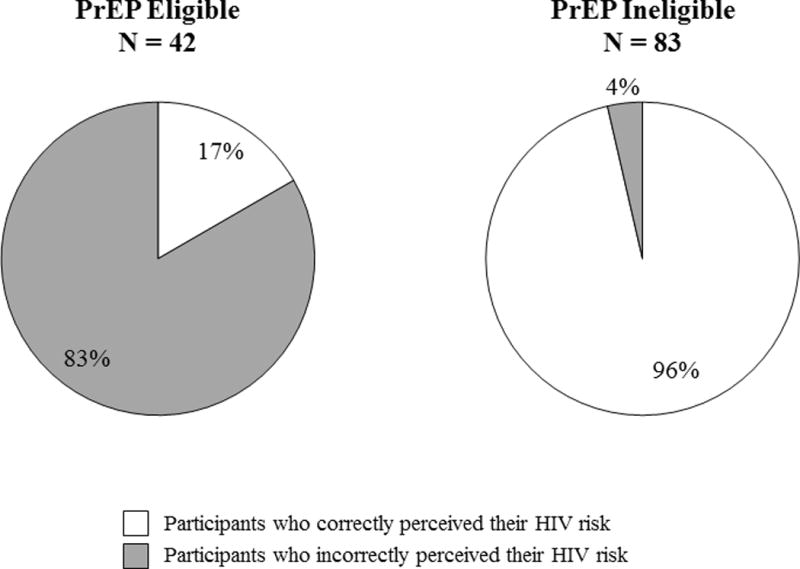
Figure 2 depicts concordance between PrEP eligibility and perception of HIV risk. Of those PrEP ineligible (n=83), 96.4% perceived they had low HIV risk. Conversely, of those who who were PrEP eligible (n=42), only 16.6% accurately perceived their high HIV risk.
Figure 2.
Discussion
This study is the first to describe PrEP eligibility, awareness, acceptability, beliefs and barriers to PrEP uptake in WICJ. Although similar questions have been addressed in other high risk populations (Chan et al., 2016; Peitzmeier et al., 2017; Shrestha et al., 2017), the unique social and structural issues contributing to women’s CJ-involvement required focused study. We found high rates of risk behaviors and significant markers for economic and social instability. These factors contribute to CJ-involvement, which in turn is destabilizing and further compounds HIV risk (Håkansson & Berglund, 2012; Schilling et al., 1994). High risk behaviors suggests all WICJ should at least be screened for HIV risk and PrEP eligibility. PrEP eligibility criteria is based on sex and drug-related HIV risk behaviors, but many of the variables associated with PrEP eligibility among WICJ in this study were markers of social instability. These findings support the need for PrEP eligibility screening that encompasses environmental and health-related indicators of HIV risk. Efforts to expand PrEP should focus on WICJ who are IPV-exposed, unstably housed, disengaged from healthcare, or who use drugs, factors associated with PrEP eligibility in our study. These are also potentially modifiable factors that could be addressed to reduce HIV risk, in addition to improving quality of life and CJ and health outcomes.
This is also the first study to characterize the PrEP care continuum among WICJ. Although access to a healthcare provider is essential for PrEP initiation and an area for targeted intervention, our PrEP continuum illustrates that having a PCP alone is insufficient for PrEP awareness or uptake, suggesting PrEP has not entered the provider-patient conversation. Low rates of PrEP awareness in our sample (25%) are similar to findings among non-CJ-involved Black and Latina women (Collier, Colarossi, & Sanders, 2017), Black men and trans-women who have sex with men (Eaton et al., 2017), and people who inject drugs (Escudero et al., 2015). PrEP scale-up will require a multifaceted approach, including expanding the network of PrEP prescribers or referrers through provider education and outreach. Since nearly all (97.6%) participants in our study had health insurance but only 65.6% had a PCP, linking women to providers who can provide PrEP is a necessary next step.
Many WICJ interface with healthcare systems less frequently than with CJ settings, so public health strategies should consider PrEP outreach in non-traditional venues. Prisons, jails, probation and parole offices, and courts have been successfully used to access women for other types of HIV interventions (Meyer, Muthulingam, El-Bassel, & Altice, 2017; Underhill, Dumont, & Operario, 2014). To our knowledge, no prior HIV interventions in CJ settings have involved PrEP, though data is emerging. There is limited data on the feasibility and effectiveness of providing PrEP in prisons (and it is not a consistently recommended strategy), but prisons and jails could provide linkages to HIV prevention services for women returning to communities (United Nations Office on Drugs and Crime, 2013).
The majority (83.3%) of women in our sample who were PrEP eligible did not perceive personal risk of HIV. In other studies, low perceived risk correlates with lower rates of HIV testing (Earnshaw VA, Smith LR, Chaudoir SR, Lee IC & MM., 2013) and PrEP adherence (Corneli et al., 2014). Discordance between perceived and actual risk has been reported in other at-risk populations including MSM (Kesler et al., 2016), African-Americans (A. Nunn et al., 2011) and incarcerated men (Golin, Barkley, Biddell, Wohl, & Rosen, 2017). Correlation between perceived and actual HIV risk varies, with some studies indicating moderate perception accuracy (Khawcharoenporn, Chunloy, & Apisarnthanarak, 2016; Mgbere et al., 2013) and others showing more extreme rates of risk underestimation (Clifton et al., 2016; Fan et al., 2014; Mumtaz et al., 2014). Discrepancies between perceived and actual risk are a significant public health challenge because it indicates that those who are most vulnerable to HIV (and thus PrEP eligible) may not recognize their risk or seek out services and are in need of targeted outreach.
Women’s personal perception of HIV risk was associated with PrEP eligibility although most PrEP eligible participants were unaware of their risk, perhaps because substance use can increase disinhibition or impair cognitive functioning (Pfaus et al., 2010; Volkow et al., 2007). Rationalization (denial) and underestimation of the risks of drug use and transactional sex is also common among people chronically exposed to risk (Ladouceur, Mayrand, & Tourigny, 1987). Social desirability biases may have led to under-reporting of global risk but not specific risk behaviors. Importantly, all study participants would likely meet “substantial risk” criteria for PrEP related to community- and network-level factors and many participants engaged in ongoing risk behaviors even if they did not meet PrEP eligibility criteria.
Our study fills an important gap in the PrEP care continuum by focusing on community-based WICJ. There may be issues specific to CJ settings in Connecticut, though convenience sampling suggests broader generalizability. Our sample had relatively high rates of publicly funded insurance, which may be less applicable to areas without expanded Medicaid. A pharmaceutical sponsored patient assistance plan, however, covers medication cost and can partially overcomes un- or under-insurance; a larger barrier to PrEP access is finding a willing prescriber and linked HIV prevention services. Many variables, including HIV status and risk behaviors, were self-reported, potentially reflecting recall or social desirability biases. We may have misclassified people as stably housed when they were unstably “doubling up” with friends or family, though this definition is inconsistently used across federal housing agencies. We found high rates of recent HIV testing, which may reflect involvement in residential or other structured drug treatment programs. We applied CDC criteria for PrEP eligibility for women. Other criteria, such as “infrequent condom usage,” are ill-defined and specific to heterosexual penetrative sex which does not apply to all WICJ. Past 6-month incident bacterial STIs are also a potential marker of risk, though this is not listed as a clear indication for PrEP for women (US Public Health Service, 2014). WICJ and their risk networks experience high HIV prevalence and may all be potential candidates for PrEP, though logistically wide dissemination is not feasible. In light of these constraints, we applied the most stringent interpretation of PrEP eligibility criteria to help prioritize WICJ for intervention.
This study focused on PrEP eligibility in a community-based population of WICJ. Future directions will focus on expanding to WICJ who are currently incarcerated and determining how PrEP eligibility and perceptions vary across the CJ spectrum. The highly structured nature of CJ systems can provide access women who may benefit from HIV prevention interventions, including PrEP (Meyer, Muthulingam, El-Bassel & Altice, 2017). Our results suggest that WICJ are receptive to and in need of PrEP counseling. Future research should intervene along the PrEP continuum for WICJ, including facilitating PrEP uptake, adherence, and linking to other HIV prevention services.
Conclusion
WICJ experience high rates of HIV risk and associated PrEP eligibility but uptake is limited. A PrEP care continuum shows the largest barriers to uptake are personal awareness and access. Interventions should be directed at increasing provider knowledge and proficiency in prescribing PrEP, encouraging providers to screen for PrEP eligibility, and empowering WICJ as PrEP consumers.
Supplementary Material
Acknowledgments
Funding: This research was supported by grants from the Infectious Disease Society of America Medical Scholars Program, Yale School of Medicine Medical Student Fellowship, The G.D. Hsiung PhD Student Research Fellowship, and career development funding from the National Institute on Drug Abuse (K23 DA033858 for JPM). Funding sources had no impact on data collection or interpretation or the decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest: None to report.
References
- Adimora AA. Preventing HIV among Women — A Step Forward, but Much Farther to Go. New England Journal of Medicine. 2016;375(22):2195–2196. doi: 10.1056/NEJMe1613661. [DOI] [PubMed] [Google Scholar]
- Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, Attitudes, and Likelihood of Pre-Exposure Prophylaxis (PrEP) Use Among US Women at Risk of Acquiring HIV. AIDS Patient Care and STDs. 2015;29(2):102–110. doi: 10.1089/apc.2014.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillargeon J, Wu H, Kelley MJ, Grady J, Linthicum L, Dunn K. Hepatitis C seroprevalence among newly incarcerated inmates in the Texas correctional system. Public Health. 2003;117(1):43–48. doi: 10.1016/S0033-3506(02)00009-4. [DOI] [PubMed] [Google Scholar]
- Bureau of Justice Statistics. HIV in Prisons, 2004. Bureau of Justice Statistics Bulletin. 2006:1–12. Retrieved from http://bjs.ojp.usdoj.gov/content/pub/pdf/hivp04.pdf.
- Center for Disease Control. HIV Among Incarcerated Populations. 2015:1–2. [Google Scholar]
- Chan PA, Glynn TR, Oldenburg CE, Montgomery MC, Robinette AE, Almonte A, Nunn AS. Implementation of Preexposure Prophylaxis for Human Immunodeficiency Virus Prevention Among Men Who Have Sex With Men at a New England Sexually Transmitted Diseases Clinic. Sexually Transmitted Diseases. 2016;43(11):717–723. doi: 10.1097/OLQ.0000000000000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifton S, Nardone A, Field N, Mercer CH, Tanton C, Macdowall W, Sonnenberg P. HIV testing, risk perception, and behaviour in the British population. Aids. 2016;30(6):943–952. doi: 10.1097/QAD.0000000000001006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier KL, Colarossi LG, Sanders K. Raising Awareness of Pre-Exposure Prophylaxis (PrEP) among Women in New York City: Community and Provider Perspectives. Journal of Health Communication. 2017 doi: 10.1080/10810730.2016.1261969. [DOI] [PubMed]
- Corneli A, Wang M, Agot K, Ahmed K, Lombaard J, Van Damme L. Perception of HIV Risk and Adherence to a Daily, Investigational Pill for HIV Prevention in FEM-PrEP. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2014;67(5):555–563. doi: 10.1097/QAI.0000000000000362. [DOI] [PubMed] [Google Scholar]
- Smith Dawn K, Van Handel Michelle, Wolitski Richard J, Stryker Jo Ellen, Hall H Irene, Prejean Joseph, Koenig Linda J, V LA. Vital Signs: Estimated Percentages and Numbers of Adults with Indications for Preexposure Prophylaxis to Prevent HIV Acquisition. Morbidity and Mortality Weekly Report. 2015;64(46):2012–2015. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- Department of Correction: York Correctional Institution. 2017 Retrieved July 6, 2017, from http://www.ct.gov/doc/cwp/view.asp?q=265454.
- Earnshaw VA, Smith LR, Chaudoir SR, Lee IC, C MM. Implications for Perceptions of HIV Risk and Testing Frequency among at risk populations. AIDS Education and Prevention. 2013;24(6):574–581. doi: 10.1521/aeap.2012.24.6.574.STEREOTYPES. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Matthews DD, Driffin DD, Bukowski L, Wilson PA, Stall RD, The Power Study Team A Multi-US City Assessment of Awareness and Uptake of Pre-exposure Prophylaxis (PrEP) for HIV Prevention Among Black Men and Transgender Women Who Have Sex with Men. Prevention Science. 2017:1–12. doi: 10.1007/s11121-017-0756-6. [DOI] [PMC free article] [PubMed]
- El-Bassel N, Terlikbaeva A, Pinkham S. HIV and women who use drugs: Double neglect, double risk. The Lancet. 2010;376(9738):312–314. doi: 10.1016/S0140-6736(10)61026-4. [DOI] [PubMed] [Google Scholar]
- Elopre L, Kudroff K, Westfall AO, Overton ET, Mugavero MJ. The Right People, Right Places, and Right Practices: Disparities in PrEP Access among African American Men, Women, and MSM in the Deep South. Journal of Acquired Immune Deficiency Syndromes. 2017;74 doi: 10.1097/QAI.0000000000001165. Retrieved from http://journals.lww.com/jaids/pages/default.aspx http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emex&AN=611815261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escudero DJ, Kerr T, Wood E, Nguyen P, Lurie MN, Sued O, Marshall BDL. Acceptability of HIV Pre-exposure Prophylaxis (PrEP) Among People Who Inject Drugs (PWID) in a Canadian Setting. AIDS and Behavior. 2015;19(5):752–757. doi: 10.1007/s10461-014-0867-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan W, Yin L, Qian HZ, Li D, Shao Y, Vermund SH, Zhang Z. HIV risk perception among HIV negative or status-unknown men who have sex with men in China. BioMed Research International. 2014;2014 doi: 10.1155/2014/232451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, Decker MR. Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care. 2017;29(6):751–758. doi: 10.1080/09540121.2016.1234679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett GP, Hallett TB, Takaruza A, Hargreaves J, Rhead R, Warren M, Gregson S. Providing a conceptual framework for HIV prevention cascades and assessing feasibility of empirical measurement with data from east Zimbabwe: a case study. The Lancet HIV. 2016;3(7):e297–e306. doi: 10.1016/S2352-3018(16)30039-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen RM, Leake BD. Healthcare Access and Utilization The Behavioral Model for Vulnerable Populations : Application to Medical Care Use and Outcomes for Homeless People. Health Services Research. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Golin CE, Barkley BG, Biddell C, Wohl DA, Rosen DL. Great Expectations: HIV Risk Behaviors and Misperceptions of Low HIV Risk among Incarcerated Men. AIDS and Behavior. 2017 doi: 10.1007/s10461-017-1748-z. [DOI] [PMC free article] [PubMed]
- Håkansson A, Berglund M. Risk factors for criminal recidivism – a prospective follow-up study in prisoners with substance abuse. BMC Psychiatry. 2012;12(1):111. doi: 10.1186/1471-244X-12-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration. Frequently Asked Questions About Health Care for the Homeless 2011 [Google Scholar]
- Hearn LE, Whitehead NE, Khan MR, Latimer WW. Time Since Release from Incarceration and HIV Risk Behaviors Among Women: The Potential Protective Role of Committed Partners During Re-entry. AIDS and Behavior. 2015;19(6):1070–1077. doi: 10.1007/s10461-014-0886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIV prevention, diagnosis, treatment and care for key populations. 2016 [Google Scholar]
- Jayakumaran JS, Aaron E, Gracely EJ, Schriver E, Szep Z. Knowledge, attitudes, and acceptability of pre-exposure prophylaxis among individuals living with HIV in an urban HIV clinic. PLoS ONE. 2016;11(2):1–10. doi: 10.1371/journal.pone.0145670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen Jenny, Page Kimberly, M A, M L. HIV, HCV and health-related harms among women who inject drugs: Implications for prevention and treatment. Journal of Acquired Immune Deficiency Syndromes. 2015;69(0 1):1–14. doi: 10.1016/j.chc.2010.03.003.Neurobiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaeble D, Glaze L. Correctional Populations in the United States, 2015. 2016 Retrieved from https://www.bjs.gov/content/pub/pdf/cpus15.pdf.
- Kajstura BA, Immarigeon R. States of Women ’ s Incarceration : The Global Context. 2015 Retrieved from https://www.prisonpolicy.org/global/women/
- Kesler MA, Kaul R, Myers T, Liu J, Loutfy M, Remis RS, Gesink D. Perceived HIV risk, actual sexual HIV risk and willingness to take pre-exposure prophylaxis among men who have sex with men in Toronto, Canada. AIDS Care. 2016;28(11):1378–1385. doi: 10.1080/09540121.2016.1178703. [DOI] [PubMed] [Google Scholar]
- Khawcharoenporn T, Chunloy K, Apisarnthanarak A. Uptake of HIV testing and counseling, risk perception and linkage to HIV care among Thai university students. BMC Public Health. 2016;16(1):556. doi: 10.1186/s12889-016-3274-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koechlin FM, Fonner VA, Dalglish SL, O’Reilly KR, Baggaley R, Grant RM, Kennedy CE. Values and Preferences on the Use of Oral Pre-exposure Prophylaxis (PrEP) for HIV Prevention Among Multiple Populations: A Systematic Review of the Literature. AIDS and Behavior. 2017;21(5):1325–1335. doi: 10.1007/s10461-016-1627-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladouceur R, Mayrand M, Tourigny Y. Risk-taking behavior in gamblers and non-gamblers during prolonged exposure. Journal of Gambling Behavior. 1987;3(2):115–122. doi: 10.1007/BF01043450. [DOI] [Google Scholar]
- Lichtenstein B, Malow R. A Critical Review of HIV-Related Interventions for Women Prisoners in the United States. Journal of the Association of Nurses in AIDS Care. 2010;21(5):380–394. doi: 10.1016/j.jana.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mera R, McCallister S, Palmer B, Mayer G, Mangnuson D, Rawlings K. Abstract: TUAX0105LB: FTC/TDF (Truvada) for HIV pre-exposure prophylaxis (PrEP) utilization in the United States: 2013–2015. 21st International AIDS Conference; Durban, South Africa. 2016. [Google Scholar]
- Meyer Jaimie, El-Bassel N, Muthulingam D, Altice FL. Leveraging the U. S. Criminal Justice System to Access Women for HIV Interventions. AIDS and Behavior. 2017 doi: 10.1007/s10461-017-1778-6. [DOI] [PMC free article] [PubMed]
- Meyer JP, Cepeda J, Taxman FS, Altice FL. Sex-Related Disparities in Criminal Justice and HIV Treatment Outcomes: A Retrospective Cohort Study of HIV-Infected Inmates. Am J Public Health. 2015;105(9):1901–1910. doi: 10.2105/ajph.2015.302687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. Journal of Women’s Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mgbere O, Monjok E, Abughosh S, Ekong E, Holstad MM, James Essien E. Modeling covariates of self-perceived and epidemiologic notions of risk for acquiring STIs/HIV among military personnel: A comparative analysis. AIDS and Behavior. 2013;17(3):1159–1175. doi: 10.1007/s10461-011-0126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumtaz GR, Weiss HA, Thomas SL, Riome S, Setayesh H, Riedner G, Abu-Raddad LJ. HIV among people who inject drugs in the Middle East and North Africa: systematic review and data synthesis. PLoS Medicine. 2014;11(6):e1001663. doi: 10.1371/journal.pmed.1001663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIDA Risk Behavior Assessment. Rockville, MD: 1993. [Google Scholar]
- Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, Mayer KH, Mimiaga M, Patel R, Chan PA. Defining the HIV Pre-Exposure Prophylaxis Care Continuum. Aids. 2017;0:1. doi: 10.1097/QAD.0000000000001385. (December 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn A, Zaller N, Cornwall A, Mayer KH, Moore E, Dickman S, Kwakwa H. Low Perceived Risk and High HIV Prevalence Among a Predominantly African American Population Participating in Philadelphia’s Rapid HIV Testing Program. AIDS Patient Care and STDs. 2011;25(4):229–235. doi: 10.1089/apc.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peitzmeier SM, Tomko C, Wingo E, Sawyer A, Sherman SG, Glass N, Decker MR. Acceptability of microbicidal vaginal rings and oral pre-exposure prophylaxis for HIV prevention among female sex workers in a high-prevalence US city. AIDS Care. 2017;121:1–5. doi: 10.1080/09540121.2017.1300628. (May) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaus JG, Wilkins MF, DiPietro N, Benibgui M, Toledano R, Rowe A, Couch MC. Inhibitory and disinhibitory effects of psychomotor stimulants and depressants on the sexual behavior of male and female rats. Hormones and Behavior. 2010;58(1):163–176. doi: 10.1016/j.yhbeh.2009.10.004. [DOI] [PubMed] [Google Scholar]
- Schilling R, el-Bassel N, Ivanoff A, Gilbert L, Su KH, Safyer SM. Sexual risk behavior of incarcerated, drug-using women, 1992. Public Health Reports (Washington, DC: 1974) 1994;109(4):539–547. [PMC free article] [PubMed] [Google Scholar]
- Shrestha R, Karki P, Altice FL, Huedo-Medina TB, Meyer JP, Madden L, Copenhaver M. Correlates of willingness to initiate pre-exposure prophylaxis and anticipation of practicing safer drug- and sex-related behaviors among high-risk drug users on methadone treatment. Drug and Alcohol Dependence. 2017;173:107–116. doi: 10.1016/j.drugalcdep.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon L, Flynn C, Muck K, Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and hepatitis C among entrants to Maryland correctional facilities. Journal of Urban Health : Bulletin of the New York Academy of Medicine. 2004;81(1):25–37. doi: 10.1093/jurban/jth085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underhill K, Dumont D, Operario D. HIV prevention for adults with criminal justice involvement: A systematic review of HIV risk-reduction interventions in incarceration and community settings. American Journal of Public Health. 2014;104(11):e27–e53. doi: 10.2105/AJPH.2014.302152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNODC, ILO, UNDP, WHO, & UNAIDS. Policy Brief: HIV prevention, treatment and care in prisons and other closed settings: a coprehensive package of interventions. 2013 Retrieved from https://www.unodc.org/documents/hiv-aids/HIV_comprehensive_package_prison_2013_eBook.pdf.
- US Public Health Service. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States – 2014 Clinical Practice Guideline. Center for Disease Control. 2014:1–67. [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Telang F, Jayne M, Wong C. Stimulant-induced enhanced sexual desire as a potential contributing factor in HIV transmission. American Journal of Psychiatry. 2007;164(1):157–160. doi: 10.1176/appi.ajp.164.1.157. [DOI] [PubMed] [Google Scholar]
- Weiner BJ. A theory of organizational readiness for change. 2009;9:1–9. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Prison Brief: United States of America. 2014 Retrieved from http://www.prisonstudies.org/country/united-states-america.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


