Abstract
The principles of open fracture management are to manage the overall injury and specifically prevent primary contamination becoming frank infection. The surgical management of these complex injuries includes debridement & lavage of the open wound with combined bony and soft tissue reconstruction. Good results depend on early high quality definitive surgery usually with early stable internal fixation and associated soft tissue repair. While all elements of the surgical principles are very important and depend on each other for overall success the most critical element appears to be achieving very early healthy soft tissue cover. As the injuries become more complex this involves progressively more complex soft tissue reconstruction and may even requiring urgent free tissue transfer requiring close co-operative care between orthopaedic and plastic surgeons. Data suggests that the best results are obtained when the whole surgical reconstruction is completed within 48–72 h.
Keywords: Open fractures, Debridement, Bony stabilization, Early healthy soft tissue cover
Introduction
Major fractures are a massive epidemiological problem around the world, and while very severe injuries can occur in an intact soft tissue envelope, the management of an open injury is much more difficult as the wound exposes the fracture haematoma to contamination and adds a potentially complex soft tissue component to the required reconstruction. It is well established that the most serious open injuries should be dealt with by specialists but these injuries present to any surgeon providing emergency care so a universal understanding of their management essential (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
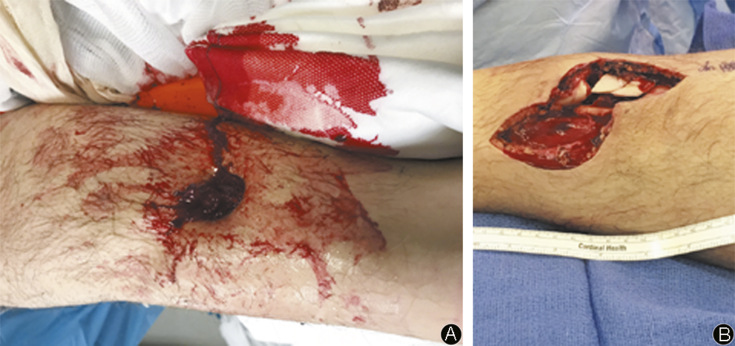
Fig. 1.
A grade IIIA tibial fracture. The initial open wound (A) is small but needs extension (B) to display the zone of injury. There is a comminuted segmental fracture with one clearly devitalised fragment requiring debridement. After debridement direct healthy closure with adequate soft tissue was possible allowing classification as IIIA.
Fig. 2.
After nailing there is a complex soft tissue defect over the distal tibia with exposed hardwear (A). This is only suitable for coverage with free tissue transfer. Here a free muscle flap was used (B) and the surface subsequently covered with a split skin graft. A grade IIIB injury. The final result is excellent (C).
Fig. 3.
The final result after a free fasciocutaneous (lateral thigh) flap to the distal leg for a grade IIIB injury.
Fig. 4.
Initial assessment of major de-gloving 3C injury (A) treated by singe stage debridement, revascularisation, internal fixation and free flap cover (B) with a latissimus dorsi flap incorporating the vascular branch to serratus anterior so the limb could be revascularized and the flap vascularized with the same micro vascular anastomosis.
Important concepts
The guiding specific principle in the management of the open fracture is the prevention of infection. The presence of a wound implies contamination but not primary infection, it is the key to treatment to prevent this contamination becoming established infection. In simple terms, bacterial multiplication will produce infection and its likelihood will be increased by the size and virulence of the inoculum and susceptibility of the host. Factors that make progression to infection more likely include the presence of shock, local haematoma, dead space, fracture instability, none viable tissue and major co-morbidities including diabetes, reduced immuno-resistance and ischaemia. Bacterial factors include the size and nature of the initial inoculum and there are specific situations where the nature of any bacterial contamination is critical. However, in the majority of situations the importance of the initial inoculum has become much reduced and today if infection develops, it is usually due to hospital acquired organisms in the more modern world and reduced or delayed access to “modern” care in the developing world.
Discussion of systems of fracture care are beyond this article but the principles of clinical management involve the application of basic surgical fracture management principles to reduce the chance of infection. These are; appropriate primary assessment, wound management, gross fracture reduction and splintage, tetanus cover and early antibiotics followed by early effective surgical management. The surgical principles of open fracture care involve wound debridement to remove any dead or doubtful tissue, profuse lavage of the wound to reduce the size of the inoculum, fracture stabilisation to allow good soft tissue healing and reconstruction of the soft tissue envelope to protect the zone of injury from infection.1, 2, 3, 4
Surgical principles of open fracture management
Debridement and lavage
Fracture stabilisation
Healthy soft tissue closure
Primary assessment and management
Assessment, tetanus, antibiotics and splintage
All patients presenting after major trauma should be fully assessed following a system such as ATLS which ensures a comprehensive primary clinical assessment, identifies specific injures and allows prioritization of the care of each injury.5 Subsequent discussions in this paper will assume that there are no more significant life threatening injuries and that there are no clinical issues that will compromise management of the limb injury. In practise there are often general or local co-morbidities that complicate the decision making and additional injuries that affect prioritization. The limb injury should always be assessed on the background of general patient care but equally major open fractures are limb threatening injuries and should not be under-prioritized.
The limb should be assessed for the signs of fracture and the severity of the wound assessed visually. Distal neurovascular function and simple digit motion should be assessed and recorded. Gross contamination may be removed but probing the wound, attempts at debridement in the emergency department or partial closure should not be done. A primary photograph of the wound is very useful and should be taken if possible and the wound should be covered with a sterile dressing. The fracture should be grossly realigned and the limb splinted.1
Tetanus and antibiotics should be given urgently.6, 7 It is accepted that the earlier the antibiotics are given the better but it must be emphasised that this is an adjuvant to surgical treatment and does not provide an increased window allowing surgical treatment to be delayed. Today for minor wounds a cephalosporin is given while for more major wounds, severe crush injuries, or agricultural injuries a Penicillin, and gram negative coverage perhaps with Gentamycin and anaerobic cover with Metronidazole can be added. If must be emphasised that while the provision of early anti-biotics is essential it does not allow excessive delay in surgical management.1
Surgical management
Wound debridement and lavage
The patent should be taken promptly to the operating room for adequate wound assessment, debridement and lavage. We consider good tissue assessment and adequate debridement the most critical and most difficult element of open fracture care. The most common error is inadequate debridement. The debridement should be considered in parallel with the subsequent soft tissue reconstruction and in the most severe injuries done in conjunction with the surgeon who will perform the soft tissue reconstruction. Logically, primary assessment and debridement should be done as soon as possible after injury and traditionally within 6 h following a philosophy that the earlier the bacterial contamination is reduced the less likely it is that infection will supervene. However, wide practical experience confirms that a senior surgeon operating in daytime with an experienced consistent team is better than urgent care out of hours with a less experienced team. This has been studied in multiple recent publications8, 9, 10, 11, 12 which have considered surgical timing and concluded that unless the injury is acutely limb threatening (which means the presence of uncontrollable bleeding, compartment syndrome, vascular injury or severe high energy injury) then the primary surgery should be performed by an experienced team as an early case the next morning. This should also allow an appropriate senior plastic surgical involvement at the first surgery facilitating adequate debridement. This is our own policy, treating only the most severe limb threatening injuries emergently while all others are treated during normal hours with an experienced surgical team, if the patient presents late at night the surgery will normally be performed as first case the next morning. Higher grade injuries clearly are more at risk of infection and take higher priority for earlier debridement. This clearly implies that the treating team work in a hospital with a well organised trauma system with pre-planned access to day time operating rooms so that trauma cases do not go to the operating room late after “planned cases” are finished.
After anaesthesia, an initial wound assessment and cleaning should be performed. This involves the removal of gross contamination and is the first real opportunity to assess the injury. A formal surgical debridement should then be performed. It is essential to extend wounds adequately to explore the whole zone of injury planning these to avoid increasing the complexity of the soft tissue injury. All non-viable tissue must be removed. As the injury becomes more severe this can involve removal of significant areas of skin, subcutaneous tissue and muscle. All free bony fragments or those attached by insignificant threads of soft tissue should be removed. Bone that fails the “tug test” is removed unless it is a critical articular segment when preservation is a specialist decision. Only the neurovascular bundles are critical to preserve. If during primary surgery a very extensive debridement is required and several compartments are lost it may become clear that reconstruction may be futile and amputation the best option. In destructive injury, primary completion amputation should be performed immediately or if the nature of the problem has been confirmed at primary surgery it is reasonable to perform a life-saving debridement and temporary stabilisation with a view to discussion with the patient and family prior to early definitive surgical care as indicated.
In parallel with debridement, a profuse wound lavage should be performed. The method and specific fluid that should be used was considered in the “Flow” study. It is now well established that a large volume of low pressure isotonic fluid should be used and that high pressure pulsatile lavage or special soaps are not required.13
It is important that a surgeon able to consider the reconstructive options performs the initial debridement as poorly planned incisions can change the nature of the defect and require a more complicated reconstruction. In general, wound extensions should be longitudinal and be sited to maximise skin viability and avoid large undermined flaps. Any flaps should be short and broad based and skin bridges kept as wide as possible. In more severe injuries the debridement should be discussed and if possible performed with the plastic surgeon who will performed the definitive reconstruction. However, despite this, the most common error in open fracture management is inadequate debridement and in many cases, adequate debridement is only possible when there is confidence that the defect can be reliably dealt with. Leaving doubtful tissue for a second look in case it survives only incorporates doubtful viability tissue in the wound and makes delay and infection more likely.
Complete wound assessment and formal classification cannot be done before exploration and debridement and in the most complex wounds this initial procedure is best done as a combined case between the orthopaedic and plastic surgeons so that the appropriate plan can be made for both hard and soft tissue reconstruction. Internationally this cooperation has been strongly recommended.
“There are many injuries in which the combination of bone and soft tissue injuries requires collaboration between Orthopaedic and Plastic surgeons from the beginning” British Orthopaedic Association & British Association of Plastic Surgeons (2,3) Complex fracture triage – “to orthopaedic traumatologist with plastic surgical support,” – care is – “highly demanding, very technical and team orientated”. S. Hansen 1991.4
Fracture stabilisation
Early stabilisation of the bony skeleton is an essential in open fracture management. Any major motion or shearing forces will continue to disrupt local soft tissues and prevent definitive soft tissue healing. A surgical philosophy avoiding fixation in open fractures is wrong, both clinical and experimental evidence confirms that even in the presence of bacterial contamination bony stability provides the best environment for healthy healing without infection and with effective early soft tissue reconstruction it is now possible to the use of any implant suitable for the fracture pattern. With the commonest considered major open fracture, the tibial shaft, the implant of choice should be an intra medullary nail if possible. If the fracture is too proximal or distal to nail, plating with maximum preservation of bone biology would be the fixation method of choice. Temporary external fixation is often used and has a role when primary definitive care is not possible. The main role of an external fixator is when the situation is not safe for definitive fixation, the patient not healthy enough or the surgeon not experienced enough to provide definitive care. External fixation may provide good temporary control but in general is a poor choice for definitive care, the presence of a frame may make plastic surgical reconstruction difficult and may lead to false confidence and delay definitive soft tissue reconstruction. Current data suggest that the outcome of major limb reconstruction with an external fixator after a severe open fracture produces poor results, indeed the LEAP study showed that the association of external fixation for bony stabilisation with soft tissue reconstruction with a flap had a worse functional outcome than amputation. It is important to remember that while a good limb salvage is the desired and can produce an excellent outcome after severe injury the consequences of failure especially with a long protracted course of reconstruction failure is disastrous for the patient who may lose many other aspects of their life investing all in salvage of a poor limb.1, 14
Wound closure, timing and techniques
The traumatic wound is the critical issue that separates open from closed fracture management. Soft tissue closure will restore the epithelial protection of the deep tissues, seal the fracture, protect against infection and lead to healthy healing. However, how and when to close the wound is a subject of intense debate and requires experienced surgical judgement as early closure is essential but must be healthy. Clearly, wound closure can only be completed after an adequate debridement and after the bony reconstruction is stable. All injured tissues will swell, and if closed too tightly additional tissue can be recruited into an area of necrosis producing wound breakdown and infection. However, leaving wounds open allows the edges to dry and may recruit additional areas of necrotic tissue into the wound. Modern wound protection with a sealed negative pressure wound dressing leaves a much tidier wound but alone does not help in preventing infection or extending the time until definitive coverage is provided.
Traditionally, debridement is staged and wound closure delayed to allow doubtful tissue to declare itself. However, given the risk of hospital acquired infection, many have advocated a more radical initial debridement and early wound closure. This more radical approach was first attributed to Godina15 and has now been well documented to provide the best results.16, 17, 18, 19 However, providing consistent, successful immediate or very early complex soft tissue reconstruction requires the availability of an extremely experienced combined orthopaedic and plastic surgical team and is hard to achieve. A staged approach is used by many surgeons but does not provide comparable results. The evidence strongly confirms Godina's opinion that debridement is best completed at the primary procedure and early closure limits the risk of infection.1, 2, 3, 16, 17, 18, 19 Each delay incorporates additional dead tissue as superficial layers desiccate and are damaged by exposure. Earlier wound closure prevents additional tissue damage and prevents hospital acquired infection. This has now been studied with both lower and higher grade injuries. In simpler injuries Jenkinson19 has shown better results with initial wound closure and in major injuries the best results, with infection rates as low as 3%16, 17, 18 are seen when the surgery including debridement, bony and soft tissue reconstruction (including free flap cover if required) is completed at the first and only visit to the operating room. Clearly the case must be suitable for single stage surgery but infection rates close to that expected after surgical management of closed fractures can be achieved. The more common staged approach does not achieve this and is documented to produce infection rates between 20 and 50%.20
“Wide, early, experienced debridement to clearly healthy tissue and early rotational or free muscle flap cover may be better in experienced hands than sequential debridement and delayed closure” Marco Godina 1986.
Wound assessment and classification
Wounds are graded after debridement, and although more comprehensive systems are available the Gustillo and Andersen open fracture classification is in common usage and has stood the test of time.21
Open Fracture Classification after Gustilo 1982–421
O-I low energy, minimal soft tissue damage, wound <1 m
O-II Higher energy, laceration 1–10 cm but no flaps/crushing/gross contamination
O-IIIA High energy comminution/segmental/contaminated but adequate soft tissue cover
O-IIIB High energy comminution/segmental/contaminated but inadequate soft tissue cover
O-IIIC Open fracture complicated by vascular injury requiring repair for limb viability
Specific soft tissue injury patterns
Grade I wounds are low energy, tiny puncture wounds with a minimal zone of injury. After wound extension, the required debridement is minimal and after fracture stabilisation the surgical extensions can be directly closed with little risk of swelling and wound necrosis, with a tiny wound this essentially implies primary wound closure.
Grade II wounds are also low energy but the wound is a laceration, usually less than 10 cm in length but over healthy deep tissues, with minimal devitalisation, no gross contamination, no large zone of injury and no degloving. Surgically the laceration should be extended, the zone of injury displayed and the bone and soft tissues debrided and lavaged as required. In a low energy wound significant amounts of tissue will not be required to be removed and after fracture stabilisation the surgical extensions and wound can be closed. While it is often recommended that primary open wound should be left open for a second assessment and delayed primary closure after 2–3 days, current data has shown that primary closure of healthy grade II wounds is not only safe but associated with a lower infection rate than delayed closure.19 However, the closure must be healthy and not be under tension. The decision needs experience and careful postoperative monitoring.
Grade III injuries are all high energy, beyond this the injury is then defined by the soft tissue reconstruction needed for closure or the presence of an associated limb threatening vascular injury. All are limb threatening but the limb is most at risk in III-C injuries which is any open fracture with a vascular injury that requires repair for limb viability. Clearly this is a major surgical emergency and limb survival depends on a rapid combined orthopaedic & vascular surgical procedure. A variety of techniques are available for the vascular repair sometimes after primary intra-vascular shunting to provide temporary blood supply to the extremity prior to a formal repair often with a reversed vein graft. A short ischaemia time is of paramount importance but combining bony and vascular reconstruction is always difficult as the vascular repair will fail if there is no bony stability but delaying the vascular repair while the skeleton is definitively stabilised may produce unacceptable delay. A potential sequence can be primary and wound assessment/lavage/debridement, vascular shunting, temporary external fixation or definitive fixation if the fracture is suitable for a rapid stabilisation procedure followed by definitive vascular reconstruction and usually early, but delayed soft tissue reconstruction if the limb is viable. Overall establishing bony stability and re-vascularization are essential, each one needs the other to be successful and direct co-operation and communication between the vascular and orthopaedic surgeons is essential.
Grade IIIA injuries are high energy injuries where there is still adequate healthy soft tissue for direct reconstruction after debridement while in a Grade III- B injury the soft tissue cover is inadequate. The adequacy of local tissues for simple soft tissue reconstruction critically depends on the site with a major wound. For example, wounds over the mid femur commonly have adequate soft tissue cover while a more minor wound over the distal tibia will not and may require a major flap for soft tissue reconstruction. All high-energy injuries are difficult to assess and should be treated by a team experienced in bony and soft tissue reconstruction from the start.2, 3, 5
Despite the grade of injury early HEALTHY soft tissue closure after an adequate debridement and fracture stabilisation is still the rule. In III-A injuries this is straight forward but in a III-B injury the situation is much more complex and a complex soft tissue reconstruction is required by definition. In these wounds, after debridement there is a soft tissue defect that will not close but can be of varying size and complex three-dimensional nature. The reconstruction should be tailored to the wound but is of increasing complexity depending on the wound site and size.
The reconstructive ladder for soft tissue defects in open fractures.
Split skin graft (SSG)
Fascio-cutaneous flap
Rotational muscle flap (with SSG)
Free muscle flap with SSG or free Fascial flap
Grade III-B wounds include a wide spectrum of injury from small awkward wounds in places where there is just not enough local cover (typically the distal medial tibia), to devastating injuries where all the compartments are widely open with significant soft tissue loss and possibly an associated bony defect. The plastic surgeon must be involved from the outset as the infection rate is specifically related to the delay in obtaining healthy soft tissue cover. The techniques required involve a progressive increase in complexity as the needs of the wound increases. Individual surgeons will favour specific reconstructive techniques but the following options are a reasonable selection for the common scenarios that present.
In the simplest IIIB defects, soft tissue coverage over a healthy muscle bed can be achieved by split thickness skin grafting. However, the reconstructive surgeon must understand the whole wound, the expectations for range of motion and the need for soft tissue (i.e. tendon) gliding and durable coverage particularly over joints which may require a more complex reconstruction.
A small defect of skin and subcutaneous tissue over bone or implant, without a significant underlying zone of injury (commonly over the proximal tibia), may be amenable to coverage with a local or regional flap, commonly a muscle flap with skin graft. These may be proximally or distally based, however the zone of injury and microperfusion of the limb must be evaluated to ensure that the resultant perfusion of the flap will be adequate. Common pedicle, rotational flaps in the lower extremity include the gastrocnemius flap (medial or lateral), the soleus flap (medial or lateral), or propeller perforator flaps which are often distally based. For proximal defects around the tibial tubercle Gastrocnemius flaps may be adequate, this muscle (especially the larger medial head) is useful as it has a specific blood supply from the superior popliteal artery and is consistently undamaged in fractures of the tibia. In the most devastating tibial fractures often this is all that is alive below the knee and it may be useful to cover a short below knee amputation stump. For smaller mid tibial defects a soleus flap (medial or lateral), or fascio-cutaneous flap including propeller perforator flaps may be able to be used. However local rotation flaps should only be used if the donor area has not been involved in the primary trauma. It is not advisable to rotate flaps within a significant zone of injury as this then carries a significant risk of flap necrosis and failure.
Larger soft tissue defects and those injuries with a wide zone of injury require coverage with healthy tissue with a reliable blood supply. Rotational options are limited in major injuries and in the distal leg so free flaps are usually the most optimal reconstructive solution. These flaps bring in healthy, vascularized tissue that help healing and provide excellent cover but require specialist skills in microvascular reconstruction and should only be done by surgeons experienced in the technique. The choice of muscle vs. fasciocutaneous free flap has been a matter of debate amongst reconstructive surgeons over the past ∼30 years, recent studies have demonstrated relative equivalency of these flap types for limb salvage, flap success, and prevention of infection. Early healthy soft tissue cover is the rule.
Over the last few years' evidence has gathered supporting Godina's philosophy15, 16, 17 that radical wound debridement and early healthy flap cover leads to better results than sequential debridement and delayed cover. The “fix and flap” approach gives the best results with results achieving very high (93%) limb salvage rate with lower risk of infection. However, few hospitals have the experience or staff availability to provide such high quality ortho-plastic care with access to an immediate free flap service, and many plastic surgeons prefer to evaluate the remaining perfusion to the limb with angiogram, CTA or MRA. It is also appropriate to be able to discuss the complexity of the situation with the patient before definitive care and describe any donor site issues prior to flap surgery. However, it remains essential to avoid protracted repeated debridements and delay as this produces bad results. The best practical option is probably to complete the debridement, bony stabilisation and wound assessment with a combined team at presentation and then perform the definitive soft tissue reconstruction at the second visit to the operating room at 48 h.
Over the last few years negative pressure dressings (Vacuum assisted closure - VAC) has become a popular method of wound dressing for severe wounds. While certainly very useful in chronic wounds, the place of the VAC system in acute wound care has not been shown to reduce infection although it does provide a better sealed soft tissue dressing. Specifically, it has been shown that use of a VAC dressing does not to allow the soft tissue cover to be delayed. Occasionally in patients unable to have complex early soft tissue cover and smaller acute wounds, management with a negative pressure dressing may avoid more complex treatment and lead to adequate granulations and enable a simple SSG or even gradual wound epithelisation.22, 23, 24, 25
Summary
Major open fracture care is complex and requires early access to specialist surgical techniques for early bony and soft tissue reconstruction. The aim of treatment is to prevent contamination becoming infection which can become disastrous with extremely severe consequences for the patient.20, 26 Obtaining an excellent result and avoiding major complications requires high levels of surgical skill and often teamwork between orthopaedic and plastic surgery that employs basic surgical principles of good debridement, provision of bony stability and early healthy soft tissue reconstruction and closure. With high quality early care excellent results can be achieved.15, 16, 17, 18
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Smith R.M. Greenfield's Surgery: Scientific Principles and Practice, Sixth Edition, Chapter 28. 2017. The principles of orthopedic surgery for trauma. [Google Scholar]
- 2.The Management of Open Tibial Fractures. British Orthopaedic Association and British Association of Plastic Surgeons; September 1997. a working party report. Please make sure this item, is it a book? [Google Scholar]
- 3.BOAST4 The Management of Severe Open Lower Limb Fractures. British Orthopaedic Assoc; 2009. https://www.boa.ac.uk/wp-content/uploads/2014/05/BOAST-4-The-Management-of-Severe-Open-Lower-Limb-Fractures.pdf [Google Scholar]
- 4.Hansen S.T., Jr. Open fractures. In: Hansen & Swinotowski, editor. Orthopaedic Trauma Protocols. Raven press; New York: 1993. [Google Scholar]
- 5.ATLS program American college of Surgeons, https://www.facs.org/quality-programs/trauma/atls.
- 6.Collinge C.A., McWilliam-Ross K., Kelly K.C., Dombroski D. Substantial improvement in prophylactic antibiotic administration for open fracture patients: results of a performance improvement program. J Orthop Trauma. 2014;28:620–625. doi: 10.1097/BOT.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 7.Lack W.D., Karunakar M.A., Angerame M.R. Type III open tibia fractures: immediate antibiotic prophylaxis minimizes infection. J Orthop Trauma. 2015;29:1–6. doi: 10.1097/BOT.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 8.Skaggs D.L., Friend L., Alman B. The effect of surgical delay on acute infection following 554 open fractures in children. J Bone Joint Surg Am. 2005;87:8–12. doi: 10.2106/JBJS.C.01561. [DOI] [PubMed] [Google Scholar]
- 9.Weber D., Dulai S.K., Bergman J. Time to initial operative treatment following open fracture does not impact development of deep infection: a prospective cohort study of 736 subjects. JOT. 2014;28(11):613–619. doi: 10.1097/BOT.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 10.Schenker M.L., Yannascoli S., Baldwin K.D. Does timing to operative debridement affect infectious complications in open long-bone Fractures? A systematic review. J Bone Joint Surg Am. 2012;94:1057–1064. doi: 10.2106/JBJS.K.00582. [DOI] [PubMed] [Google Scholar]
- 11.Hull P.D., Johnson S.C., Stephen D.J. Delayed debridement of severe open fractures is associated with a higher rate of deep infection. Bone Joint J. 2014;96-B:379–384. doi: 10.1302/0301-620X.96B3.32380. [DOI] [PubMed] [Google Scholar]
- 12.Schenker M.L., Ahn J., Donegan D. The cost of after-hours operative debridement of open tibia fractures. J Orthop Trauma. 2014;28:626–631. doi: 10.1097/BOT.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 13.FLOW Investigators, Bhandari M., Jeray K.J. A trial of wound irrigation in the initial management of open fracture wounds. N Engl J Med. 2015;373:2629–2641. doi: 10.1056/NEJMoa1508502. [DOI] [PubMed] [Google Scholar]
- 14.Worlock P., Slack R., Harvey L. The prevention of infection in open fractures: an experimental study of the effect of fracture stability. Injury. 1994;25:31–38. doi: 10.1016/0020-1383(94)90181-3. [DOI] [PubMed] [Google Scholar]
- 15.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;76:719–728. doi: 10.1097/00006534-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Gopal S., Majumder S., Batchelor A.G. Fix and Flap, the radical treatment of open tibial fractures. J Bone Joint Surg Br. 2000;82-B:959–966. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 17.Hertel R., Lambert S.M., Muller S. Rebuilding severe open fractures of the leg: immediate is better than early soft tissue reconstruction for open fractures of the leg. Injury. 1998;29:154–155. [Google Scholar]
- 18.Vermaak P.V., Parsons L., Liggins F. Impact of Management: Reoperation Rates and Gustilo Anderson Grade 3 Open Fractures of the Lower Limb. OTA Annual Meeting. 2017. paper 124. [Google Scholar]
- 19.Jenkinson R.J., Kiss A., Johnson S. Delayed wound closure increases deep-infection rate associated with lower-grade open fractures: a propensity-matched cohort study. J Bone Joint Surg Am. 2014;96:380–386. doi: 10.2106/JBJS.L.00545. [DOI] [PubMed] [Google Scholar]
- 20.Webb L.X., Bosse M.J., Castillo R.C., LEAP Study Group Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg Am. 2007;89:923–928. doi: 10.2106/JBJS.F.00776. [DOI] [PubMed] [Google Scholar]
- 21.Gustilo R.B., Anderson J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analysis. J Bone Joint Surg Am. 1976;58-A:453–458. [PubMed] [Google Scholar]
- 22.Steiert A.E., Partenheimer A., Schreiber T. The VAC system as a bridging between primary Osteosynthesis in conjunction with functional reconstruction of soft tissue in open fractures type 2 and type 3. Zentralbl Chir. 2004;129(supp 1):S98–S100. doi: 10.1055/s-2004-822658. [DOI] [PubMed] [Google Scholar]
- 23.DeFranzo A.J., Argenta L.C., Marks M.W. The use of vacuum assisted closure therapy for the treatment of lower extremity wounds with exposed bone. Plas Reconstr Surg. 2001;108:1184–1191. doi: 10.1097/00006534-200110000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Bhattacharyya T., Mehta P., Smith R.M. Routine use of wound vacuum-assisted closure does not allow coverage delay for open tibia fractures. Plast Reconstr Surg. 2008;121:1263–1266. doi: 10.1097/01.prs.0000305536.09242.a6. [DOI] [PubMed] [Google Scholar]
- 25.Masters J., Bruce J., Parsons N., Costa M.L. Rates of Surgical Site Infection after Open Fractures: Findings of the UK Wound Management of Lower Limb Fractures (UK WOLLF) Trial. OTA Annual Meeting. 2017. paper 123. [Google Scholar]
- 26.Ram G.G., Anil Chander V.C., Rajappa S. Amputees have better quality of life than who had limb salvaged in grade iii B and grade iii C crush injury. Indian J Orthop Surg. 2015;1:146–148. [Google Scholar]