Abstract
Background
Sexual dysfunction is often complex and biopsychosocial. Traditional sexual health care management involves individual providers not in a multi-disciplinary setting. A multi-disciplinary team may consist of a medical provider, pelvic floor physical therapist, and sex therapist.
Aim
The aim was to explore the patient perceptions of benefit from management of their sexual dysfunction by a biopsychosocial multi-disciplinary team.
Methods
A survey was e-mailed to women patients seen by multi-disciplinary teams at 2 different settings: San Diego Sexual Medicine or Mayo Clinic Women's Health Clinic during a 27-month period. Data are reported using summary statistics for age and count for remaining survey responses. Cochran-Armitage tests for trend were used to compare pre- and post-comfort levels.
Outcomes
Main outcome measures included perceived benefit of being managed in a team-based model of care, level of benefit and satisfaction from each provider, and difference from pre-conceived level of comfort to actual comfort after each provider visit.
Results
89 of 270 e-mailed surveys were analyzed. Patient populations (mean age 47.6, range 23–77 years) were similar between sites. Overall, 82% of respondents reported moderate/great benefit from the team-based model; 72.1% reported management by all 3 providers valuable/extremely valuable; and 84.3% were somewhat/very satisfied with the model. Women endorsed specific ways in which they benefitted from the team-based model including: improved sexual function (58.1%), feeling validated (72.1%) and listened to (62.8%), that they better understood their health concerns (65.1%), that their partner better understood their health concerns (46.5%), and feeling normal (46.5%). There were no significant differences between the 2 clinics in terms of patient-perceived benefit, value, or satisfaction.
Conclusions
The team-based model of care for management of sexual dysfunction in women including a medical provider, physical therapist, and sex therapist is associated with patient-perceived benefit, satisfaction, and value.
Rullo J, Faubion S, Hartzell R, et al. Biopsychosocial Management of Female Sexual Dysfunction: A Pilot Study of Patient Perceptions From 2 Multi-Disciplinary Clinics. Sex Med 2018;6:217–223.
Key Words: Biopsychosocial, Multi-disciplinary, Satisfaction, Benefit
Introduction
The biopsychosocial model of sexual health management is often considered the gold standard because it emphasizes that sexual dysfunctions involve a complex interplay of biological, psychological, interpersonal, and sociocultural factors.1, 2, 3 This model is the foundation for clinical theories and paradigms including the sexual tipping point,4 the dual-control model,5 and systemic sex therapy.6
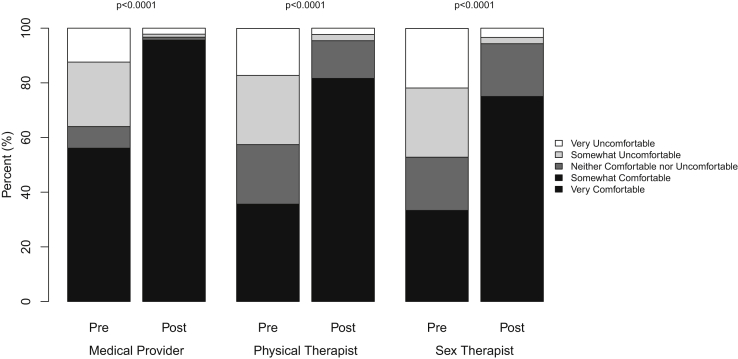
Biopsychosocial sexual health care management involves the collaboration of a medical provider, physical therapist (PT), and sex therapist (ST), who coordinate treatment between providers and patient (Figure 1). This multi-disciplinary model is not unique to sexual health care delivery, as it has been shown to be effective in other health care settings, including primary care, obesity management, and cancer survivorship.3, 7 Specifically within the field of sexual health, a number of studies have shown promising results using this multi-disciplinary framework to successfully treat various sexual health concerns, particularly female sexual dysfunction.8, 9, 10, 11, 12, 13 Despite promising clinical outcomes of multi-disciplinary treatment for sexual health, much is unknown about this model. This is, in part, due to the difficulties in integrating multiple sexual health disciplines within 1 clinic and medical record system.2, 14
Figure 1.
Multi-disciplinary team-based model of care. MP = medical provider; PT = physical therapist; ST = sex therapist.
The present study is an attempt at elucidating this multi-disciplinary treatment approach for sexual health concerns, with a specific focus on women's sexual health. First, the patient flow of 2 different multi-disciplinary, integrated sexual health clinics is described. Second, patient satisfaction and perceived value and benefit of a multi-disciplinary approach from these 2 independent clinics are reported. These findings explore the benefits of the use of multi-disciplinary management for female sexual dysfunction. This is of particular interest at this time when increasing patient satisfaction is considered relevant to practice management and a determinant of provider compensation.
Methods
After approval by the Mayo Clinic Institutional Review Board, an e-mail survey was administered to women patients seen by all 3 provider types (physician, PT, ST) within a 90-day time frame at San Diego Sexual Medicine (SDSM) or Mayo Clinic Women's Health Clinic (MCWHC) between October 1, 2013, and December 31, 2015. The survey addressed such variables as perceived benefit of being managed in a team-based model of care, level of benefit from each provider, level of satisfaction from each provider, and difference in pre-conceived level of comfort and actual level comfort after the visit with each provider. This survey does not include any material from validated questionnaires.
Data are reported using summary statistics such as mean (SD) for age and count (percentage) for the remaining survey responses. Cochran-Armitage tests for trend were used to compare pre- and post-comfort levels for each type of care provider. Comparisons were made between clinics using a t test for age; χ2 or Fisher exact tests for discrete, nominal questions; and Mantel-Haenszel χ2 tests for ordinal measures. Statistical significance was set at a P value ≤.05. All analyses were conducted using software (SAS, Version 9.4; SAS Institute Inc, Cary, NC).
MCWHC is a multi-disciplinary, integrated care clinic within a larger health care organization, providing treatment for women with sexual dysfunction and menopause-related concerns. The clinic is composed of internists/family medicine specialists (MD/DO), ST, and pelvic floor PT. At MCWHC, women presenting with sexual health concerns are seen by a medical provider. If, at the time of the initial consultation, the MD/DO determines the patient would benefit from consultation with a PT and/or ST, the patient is referred, with discussion among the various providers during the episode of care, as well as coordination of care and provision of a treatment plan. Only patients seeing all 3 providers at MCWHC were included in the study.
SDSM is a stand-alone health care facility providing multi-disciplinary, integrated clinical care for men and women with sexual dysfunction. SDSM is composed of sexual medicine physicians (MD), ST, and pelvic floor PT. At SDSM, the model is somewhat different from MCWHC, in that all women patients presenting with sexual health concerns are ideally scheduled to see the MD, PT, and ST (in no specific order) on their initial visit, with discussion among the various providers throughout the visit, and a summary of pertinent findings at the end.
Results
Of 270 surveys e-mailed, 95 were returned (35.1% response rate); 6 were incomplete. A total of 89 were included in the analysis, 43 from SDSM and 46 from MCWHC. Of the 89 women who completed the survey (mean age, 47.6 years; range 20–77 years), the majority reported being white, not Hispanic (92.1%), post-menopausal (57%), married (76.4%), and employed (43.2%). The patient populations seen at MCWHC and SDSM revealed no significant differences in terms of age, menopausal status, relationship status, race/ethnicity, employment, or education status (Table 1).
Table 1.
Characteristics of survey respondents
| Total N = 89 |
San Diego Sexual Medicine N = 43 |
Mayo Clinic Women's Health Clinic N = 46 |
P value | |
|---|---|---|---|---|
| Age at visit, y | .84 | |||
| Mean (SD) | 47.6 (14.2) | 47.8 (15.1) | 47.3 (13.5) | |
| Range | 20.0–77.0 | 20.0–72.0 | 23.0–77.0 | |
| Race/ethnicity | .29 | |||
| White, not Hispanic | 82 (92.1%) | 39 (90.7%) | 43 (93.5%) | |
| Black, not Hispanic | 2 (2.2%) | 2 (4.7%) | 0 (0.0%) | |
| Asian/Pacific Islander | 2 (2.2%) | 1 (2.3%) | 1 (2.2%) | |
| White, Native American, and Asian/Pacific Islander | 1 (1.1%) | 1 (2.3%) | 0 (0.0%) | |
| Prefer not to answer | 2 (2.2%) | 0 (0.0%) | 2 (4.3%) | |
| Menstrual status | .52 | |||
| Premenopause | 29 (33.7%) | 15 (36.6%) | 14 (31.1%) | |
| Perimenopause | 8 (9.3%) | 5 (12.2%) | 3 (6.7%) | |
| Postmenopausal | 49 (57.0%) | 21 (51.2%) | 28 (62.2%) | |
| Relationship status | .18 | |||
| Single | 6 (6.7%) | 5 (11.6%) | 1 (2.2%) | |
| In a relationship | 10 (11.2%) | 6 (14.0%) | 4 (8.7%) | |
| Domestic partnership/civil union | 1 (1.1%) | 1 (2.3%) | 0 (0.0%) | |
| Married | 68 (76.4%) | 29 (67.4%) | 39 (84.8%) | |
| Separated from spouse/partner | 3 (3.4%) | 1 (2.3%) | 2 (4.3%) | |
| Other | 1 (1.1%) | 1 (2.3%) | 0 (0.0%) | |
| Education | .09 | |||
| High school graduate or GED | 5 (5.7%) | 3 (7.1%) | 2 (4.3%) | |
| Some college or 2-y degree | 23 (26.1%) | 8 (19.0%) | 15 (32.6%) | |
| 4-y College graduate | 29 (33.0%) | 11 (26.2%) | 18 (39.1%) | |
| Post-graduate studies | 31 (35.2%) | 20 (47.6%) | 11 (23.9%) | |
| Employment status | .29 | |||
| Employed | 38 (43.2%) | 17 (39.5%) | 21 (46.7%) | |
| Self-employed | 19 (21.6%) | 12 (27.9%) | 7 (15.6%) | |
| Full-time homemaker | 8 (9.1%) | 6 (14.0%) | 2 (4.4%) | |
| Retired | 14 (15.9%) | 6 (14.0%) | 8 (17.8%) | |
| Student | 3 (3.4%) | 1 (2.3%) | 2 (4.4%) | |
| Work disabled | 4 (4.5%) | 1 (2.3%) | 3 (6.7%) | |
| Unemployed | 2 (2.3%) | 0 (0.0%) | 2 (4.4%) |
GED = General Equivalency Development.
Values are n (%) unless otherwise specified.
Compared to MCWHC, significantly more patients from SDSM reported being previously seen by another provider for a sexual health concern (85.4% SDSM vs 26.1% MCWHC, P < .0001). Significantly more patients at MCWHC presented with a symptom of sexual pain compared with those at SDSM (93.5% vs 72.1%, P = .0099).
With regard to the findings of this study that explored the patient-perceived benefits of multi-disciplinary management for female sexual dysfunction, 82.1% of the respondents reported moderate or great benefit from the team-based model of care. A total of 77.6% reported that seeing all 3 providers was valuable or extremely valuable, and 84.3% were somewhat or very satisfied with the model. There were no significant differences between the 2 clinics in terms of patient-perceived benefit, value, or satisfaction (P = .53; P = .12; and P = .60, respectively) (Table 2).
Table 2.
Patient responses by clinic
| Overall, how satisfied were you with your visit(s) with… | SDSM | MCWHC | Combined | P value |
|---|---|---|---|---|
| …a team-based model of care? | .6023 | |||
| Very Satisfied | 33 (76.7%) | 34 (73.9%) | 67 (75.3%) | |
| Somewhat Satisfied | 6 (14.0%) | 2 (4.3%) | 8 (9.0%) | |
| Neutral | 1 (2.3%) | 6 (13.0%) | 7 (7.9%) | |
| Somewhat Dissatisfied | 2 (4.7%) | 2 (4.3%) | 4 (4.5%) | |
| Very Dissatisfied | 1 (2.3%) | 2 (4.3%) | 3 (3.4%) | |
| Rate the level of benefit you received from our team-based model of care | .8925 | |||
| Great Benefit | 25 (58.1%) | 28 (60.9%) | 53 (59.6%) | |
| Moderate Benefit | 10 (23.3%) | 10 (21.7%) | 20 (22.5%) | |
| Unsure | 4 (9.3%) | 1 (2.2%) | 5 (5.6%) | |
| Very Little Benefit | 3 (7.0%) | 5 (10.9%) | 8 (9.0%) | |
| No Benefit at All | 1 (2.3%) | 2 (4.3%) | 3 (3.4%) | |
| In what ways did you benefit? | ||||
| Sexual Function Improved | 25 (58.1%) | 21 (45.7%) | 46 (51.7%) | .2388 |
| Felt Validated | 31 (72.1%) | 28 (60.9%) | 59 (66.3%) | .2630 |
| Felt Listened To | 27 (62.8%) | 33 (71.7%) | 60 (67.4%) | .3681 |
| Helped you feel normal | 20 (46.5%) | 21 (45.7%) | 41 (46.1%) | .9352 |
| Helped you better understand your health concerns | 28 (65.1%) | 33 (71.7%) | 61 (68.5%) | .5013 |
| Helped your partner understand your health concerns | 20 (46.5%) | 22 (47.8%) | 42 (47.2%) | .9012 |
| Other | 9 (20.9%) | 4 (8.7%) | 13 (14.6%) | .1024 |
| How valuable was it to see all three types of providers at our clinic? | .1170 | |||
| Extremely Valuable | 18 (41.9%) | 27 (58.7%) | 45 (50.6%) | |
| Valuable | 13 (30.2%) | 11 (23.9%) | 24 (27.0%) | |
| Moderately Valuable | 6 (14.0%) | 3 (6.5%) | 9 (10.1%) | |
| Slightly Valuable | 3 (7.0%) | 3 (6.5%) | 6 (6.7%) | |
| Not at all Valuable | 3 (7.0%) | 2 (4.3%) | 5 (5.6%) | |
| If you had not come to our clinic, how likely or unlikely would you have been to see a… | ||||
| …medical provider specializing in sexual health? | .0004 | |||
| Very Likely | 19 (44.2%) | 8 (17.4%) | 27 (30.3%) | |
| Somewhat Likely | 11 (25.6%) | 8 (17.4%) | 19 (21.3%) | |
| Unsure | 5 (11.6%) | 9 (19.6%) | 14 (15.7%) | |
| Somewhat Unlikely | 6 (14.0%) | 9 (19.6%) | 15 (16.9%) | |
| Very Unlikely | 2 (4.7%) | 12 (26.1%) | 14 (15.7%) | |
| …physical therapist specializing in sexual health? | .2679 | |||
| Missing | 1 | 1 | 2 | |
| Very Likely | 7 (16.7%) | 5 (11.1%) | 12 (13.8%) | |
| Somewhat Likely | 6 (14.3%) | 6 (13.3%) | 12 (13.8%) | |
| Unsure | 4 (9.5%) | 3 (6.7%) | 7 (8.0%) | |
| Somewhat Unlikely | 11 (26.2%) | 11 (24.4%) | 22 (25.3%) | |
| Very Unlikely | 14 (33.3%) | 20 (44.4%) | 34 (39.1%) | |
| …sex therapist? | .4163 | |||
| Very Likely | 10 (23.3%) | 3 (6.5%) | 13 (14.6%) | |
| Somewhat Likely | 2 (4.7%) | 9 (19.6%) | 11 (12.4%) | |
| Unsure | 4 (9.3%) | 6 (13.0%) | 10 (11.2%) | |
| Somewhat Unlikely | 9 (20.9%) | 5 (10.9%) | 14 (15.7%) | |
| Very Unlikely | 18 (41.9%) | 23 (50.0%) | 41 (46.1%) | |
| Before visiting our clinic, what was your comfort level with being seen by a … |
||||
| …medical provider specializing in sexual health? | .0902 | |||
| Very Comfortable | 15 (34.9%) | 8 (17.4%) | 23 (25.8%) | |
| Somewhat Comfortable | 11 (25.6%) | 16 (34.8%) | 27 (30.3%) | |
| Neither Comfortable nor Uncomfortable | 4 (9.3%) | 3 (6.5%) | 7 (7.9%) | |
| Somewhat Uncomfortable | 10 (23.3%) | 11 (23.9%) | 21 (23.6%) | |
| Very Uncomfortable | 3 (7.0%) | 8 (17.4%) | 11 (12.4%) | |
| …physical therapist specializing in sexual health? | .1259 | |||
| Missing | 1 | 1 | 2 | |
| Very Comfortable | 5 (11.9%) | 6 (13.3%) | 11 (12.6%) | |
| Somewhat Comfortable | 10 (23.8%) | 10 (22.2%) | 20 (23.0%) | |
| Neither Comfortable nor Uncomfortable | 15 (35.7%) | 4 (8.9%) | 19 (21.8%) | |
| Somewhat Uncomfortable | 8 (19.0%) | 14 (31.1%) | 22 (25.3%) | |
| Very Uncomfortable | 4 (9.5%) | 11 (24.4%) | 15 (17.2%) | |
| …sex therapist? | .2000 | |||
| Missing | 1 | 1 | 2 | |
| Very Comfortable | 4 (9.5%) | 3 (6.7%) | 7 (8.0%) | |
| Somewhat Comfortable | 10 (23.8%) | 12 (26.7%) | 22 (25.3%) | |
| Neither Comfortable nor Uncomfortable | 13 (31.0%) | 4 (8.9%) | 17 (19.5%) | |
| Somewhat Uncomfortable | 8 (19.0%) | 14 (31.1%) | 22 (25.3%) | |
| Very Uncomfortable | 7 (16.7%) | 12 (26.7%) | 19 (21.8%) | |
| After visiting our clinic, what was your comfort level with being seen by a… | ||||
| …medical provider specializing in sexual health? | .1230 | |||
| Very Comfortable | 37 (86.0%) | 33 (71.7%) | 70 (78.7%) | |
| Somewhat Comfortable | 4 (9.3%) | 11 (23.9%) | 15 (16.9%) | |
| Neither Comfortable nor Uncomfortable | 0 (0.0%) | 1 (2.2%) | 1 (1.1%) | |
| Somewhat Uncomfortable | 1 (2.3%) | 0 (0.0%) | 1 (1.1%) | |
| Very Uncomfortable | 1 (2.3%) | 1 (2.2%) | 2 (2.2%) | |
| …physical therapist specializing in sexual health? | .4837 | |||
| Missing | 1 | 1 | 2 | |
| Very Comfortable | 24 (57.1%) | 27 (60.0%) | 51 (58.6%) | |
| Somewhat Comfortable | 7 (16.7%) | 13 (28.9%) | 20 (23.0%) | |
| Neither Comfortable nor Uncomfortable | 9 (21.4%) | 3 (6.7%) | 12 (13.8%) | |
| Somewhat Uncomfortable | 2 (4.8%) | 0 (0.0%) | 2 (2.3%) | |
| Very Uncomfortable | 0 (0.0%) | 2 (4.4%) | 2 (2.3%) | |
| …sex therapist? | .0618 | |||
| Missing | 0 | 1 | 1 | |
| Very Comfortable | 17 (39.5%) | 22 (48.9%) | 39 (44.3%) | |
| Somewhat Comfortable | 9 (20.9%) | 18 (40.0%) | 27 (30.7%) | |
| Neither Comfortable nor Uncomfortable | 14 (32.6%) | 3 (6.7%) | 17 (19.3%) | |
| Somewhat Uncomfortable | 2 (4.7%) | 0 (0.0%) | 2 (2.3%) | |
| Very Uncomfortable | 1 (2.3%) | 2 (4.4%) | 3 (3.4%) |
Women endorsed specific ways in which they benefitted from the team-based model, including improved sexual function (58.1%), feeling validated (72.1%), feeling listened to (62.8%), feeling that they better understood their health concerns (65.1%), feeling that their partner better understood their health concerns (46.5%), and feeling normal (46.5%). There were no significant differences between the 2 clinics in terms of these benefits (all P values >.2).
A total of 17.9% of patients reported that they did not benefit from the team-based model, 22.4% did not find if valuable, and 15.7% were not satisfied with the model. Compared to those who reported value, benefit, and satisfaction with the team-based model, those who did not were significantly more likely to be single (P < .05) or unmarried (P ≤ .05), and significantly less likely to report an increase in post-visit comfort level with any of the providers (all P values < .01). Additionally, those who did not perceive value from the team-based model were significantly more likely to be employed (P = .01).
The level of benefit from the visits with each of the 3 providers was assessed separately. A total of 86.5% of respondents reported great or moderate benefit with regard to the MD/DO, with no significant differences between clinics (P = .53). There were significant differences between clinics with regard to patient-perceived benefit from the visit with the PT (56.1% great or moderate benefit at SDSM vs 82.2% at MCWHC, P = .03) and ST (46.5% great or moderate benefit at SDSM vs 78.3% at MCWHC, P = .001).
The level of satisfaction from the visits with each of the 3 providers was also assessed separately. A total of 88.8% of patients were satisfied with their visit with the MD/DO and 86.2% were satisfied with their visit with the PT. Satisfaction with these providers was not significantly different between the 2 clinics (P = .49 and P = .26, respectively). Satisfaction with the ST was significantly different between clinics (74.4% very or somewhat satisfied at SDSM vs 86.9% at MCWHC, P = .03).
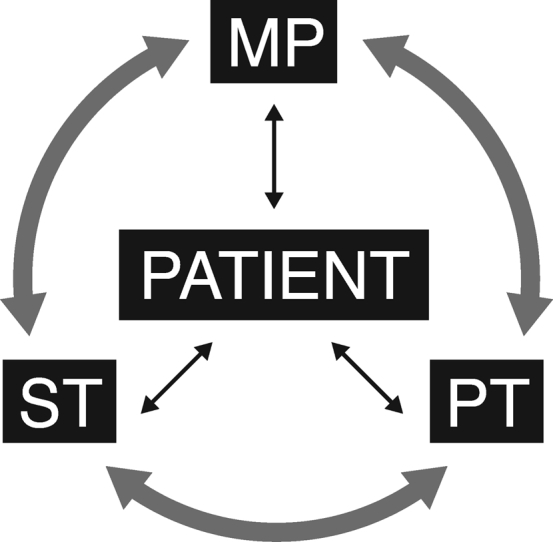
The pre-conceived level of patient comfort with each of the 3 providers was compared to the actual level of patient comfort experienced after the visit. Concerning the medical provider, patients' level of comfort increased significantly at both clinics from 56.1–95.6% somewhat or very comfortable after the visit (P < .0001), with no significant differences between the clinics (pre, P = .09 and post, P = .12). Concerning the PT, patients' level of comfort increased from 35.6–81.6% being somewhat or very comfortable after the visit (P < .0001), with no significant differences between the clinics (pre, P = .13 and post, P = .48). Concerning the ST, patients' level of comfort increased from 33.3–75% being somewhat or very comfortable after the visit (P < .0001), with no significant differences between clinics (pre, P = .20 and post, P = .06) (Figure 2).
Figure 2.
Comfort level with seeing team members before vs after visit.
Discussion
A multi-disciplinary clinic is uniquely equipped to address sexual health problems, which are considered to be complex and biopsychosocial. However, the vast majority of sexual health care providers do not practice in a multi-disciplinary setting. Only 6.8% of patients in this study had been assessed within a team-based model prior to presentation at SDSM or MCWHC.2, 15 The purpose of this study was to assess whether the multi-disciplinary model demonstrated benefits in the form of enhanced patient satisfaction. At a time when provider reimbursement is based on Hospital Consumer Assessment of Healthcare Providers and Systems scores, patient satisfaction becomes the leading metric for compensation.16
The present study assessed patient perceived value, benefit, and satisfaction of 2 multi-disciplinary treatment models for sexual health concerns. 2 sites were included in this study to determine whether or not there would be generalizability of this concept across sites and specific models. 1 model (MCWHC) is a referral-based integrated sexual health clinic (ie, patients begin their care with a medical provider and are referred to a PT and/or ST if deemed medically necessary). The other model (SDSM) is a compulsory integrated sexual health clinic (ie, patients see every provider on the team). Overall, despite differences between the 2 team-based approaches, over 80% of respondents reported benefit and satisfaction with the team-based approach, and over 70% reported that seeing all 3 providers was valuable. There were no significant differences in these outcomes between the 2 clinics. These findings show high patient perceived benefit, comfort, and satisfaction, and therefore support the implementation of multi-disciplinary management for female sexual dysfunction.
A total of 19% of patients, on average, did not report benefit, value, or satisfaction from the team-based model; however, the reason was not queried. These patients were significantly more likely to be single or unmarried and significantly less likely to report an increase in comfort post-visit, with any of the providers. It is unknown whether or not this same patient cohort would benefit from a different provider model or from seeing different providers (ie, they were not comfortable or did not connect with the team members) or if they transferred treatment dissatisfaction to visit dissatisfaction. These findings may also suggest that women who are most uncomfortable with sexual health treatment will likely benefit the least.
Differences between the 2 models did appear in visits with the PT and ST. Patients reported greater benefit and satisfaction with the ST and PT in the referral-based model (MCWHC) as compared to the compulsory model (SDSM). Reasons for this are purely speculative. It is possible that the PT was perceived with greater benefit in the referral-based model because nearly all patients in this model were women with sexual pain, and physical therapy is a well-established, evidenced-based treatment for sexual pain,8, 10, 11, 12 more so than any other female sexual health concern (eg, desire, arousal, orgasm). However, post-hoc analyses revealed no significant difference between women with and without pain in their level of benefit, value, and satisfaction with PT (all P > .6). Alternatively, it may be that patients simply prefer the autonomy to choose whether to see providers beyond the MD/DO, and this autonomy led to higher perceived benefit. Or perhaps the temporal relationship of visits may explain the differences in perceived benefit between the 2 models. Future research comparing these models is needed.
There are several limitations of this study. The patient populations were not representative of the general population, as the majority of participants were English speaking, white, non-Hispanic, postmenopausal, married, and employed. Only 33% of the population sample returned a completed survey, thus it is unclear how those who did not complete the surveys may have differed. The survey was retrospectively obtained, not an exit survey, and relied on patient recall. In addition, the survey items assessing perceived value, benefit, and satisfaction were not obtained from previously validated instruments. Finally, this was a proof of principle study, with only 2 sites assessed, thus limiting the generalizability of the findings.
Conclusion
Multi-disciplinary, integrated sexual health treatment teams are uncommon despite the fact that sexual health problems are considered to be biopsychosocial. This study shows that the team-based model of care including a medical provider, PT, and ST for management of sexual dysfunction in women is associated with high patient-perceived benefit, satisfaction, and value. Future research on treatment outcomes is needed to support the effectiveness of this integrated care model.
Statement of authorship
Category 1
-
(a)Conception and Design
- Jordan Rullo; Stephanie Faubion; Rose Hartzell; Sue Goldstein; Deborah Cohen; Irwin Goldstein
-
(b)Acquisition of Data
- Karla Frohmader
-
(c)Analysis and Interpretation of Data
- Jordan Rullo; Stephanie Faubion; Rose Hartzell; Sue Goldstein; Deborah Cohen; Karla Frohmader; Ashley Winter; Kristin Mara; Darrell Schroeder; Irwin Goldstein
Category 2
-
(a)Drafting the Article
- Jordan Rullo; Stephanie Faubion; Rose Hartzell; Sue Goldstein; Deborah Cohen
-
(b)Revising It for Intellectual Content
- Jordan Rullo; Stephanie Faubion; Rose Hartzell; Sue Goldstein; Deborah Cohen; Karla Frohmader; Ashley Winter; Kristin Mara; Darrell Schroeder; Irwin Goldstein
Category 3
-
(a)Final Approval of the Completed Article
- Jordan Rullo; Stephanie Faubion; Rose Hartzell; Sue Goldstein; Deborah Cohen; Karla Frohmader; Ashley Winter; Kristin Mara; Darrell Schroeder; Irwin Goldstein
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Basson R., Wierman M.E., Van Lankveld J., Brotto L. Recommendations for women's sexual dysfunction. In: Montorsi F., Basson R., Adaikan G., editors. Sexual medicine: sexual dysfunctions in men and women. 3rd International consultation on sexual medicine. Health Publication Ltd; Paris, France: 2010. [Google Scholar]
- 2.Berry M.D., Berry P.D. Contemporary treatment of sexual dysfunction: reexamining the biopsychosocial model. J Sex Med. 2013;10:2627–2643. doi: 10.1111/jsm.12273. [DOI] [PubMed] [Google Scholar]
- 3.Perelman M. Advocating for a transdisciplinary perspective in sexual medicine. Curr Sex Health Rep. 2015;7:1. [Google Scholar]
- 4.Perelman M.A. The sexual tipping point: a mind/body model for sexual medicine. J Sex Med. 2009;6:629–632. doi: 10.1111/j.1743-6109.2008.01177.x. [DOI] [PubMed] [Google Scholar]
- 5.Janssen E., Bancroft J. Indiana University Press; Bloomington, IN: 2007. The psychophysiology of sex. [Google Scholar]
- 6.Bakker R.M., Vermeer W.M., Creutzberg C.L. Qualitative accounts of patients' determinants of vaginal dilator use after pelvic radiotherapy. J Sex Med. 2015;12:764–773. doi: 10.1111/jsm.12776. [DOI] [PubMed] [Google Scholar]
- 7.Reiss-Brennan B., Brunisholz K.D., Dredge C. Association of integrated team-based care with health care quality, utilization, and cost. JAMA. 2016;316:826–834. doi: 10.1001/jama.2016.11232. [DOI] [PubMed] [Google Scholar]
- 8.Bergeron S., Lord M.J. The integration of pelvi-perineal re-education and cognitive-behavioral therapy in the multidisciplinary treatment of the sexual pain disorders. Sex Relationsh Ther. 2003;18:135–141. [Google Scholar]
- 9.Carvalho J., Nobre P. Biopsychosocial determinants of men's sexual desire: testing an integrative model. J Sex Med. 2011;8:754–763. doi: 10.1111/j.1743-6109.2010.02156.x. [DOI] [PubMed] [Google Scholar]
- 10.Pacik P.T. Understanding and treating vaginismus: a multimodal approach. Int Urogynecol J. 2014;25:1613–1620. doi: 10.1007/s00192-014-2421-y. [DOI] [PubMed] [Google Scholar]
- 11.Sadownik L.A., Seal B.N., Brotto L.A. Provoked vestibulodynia-women's experience of participating in a multidisciplinary vulvodynia program. J Sex Med. 2012;9:1086–1093. doi: 10.1111/j.1743-6109.2011.02641.x. [DOI] [PubMed] [Google Scholar]
- 12.Spoelstra S.K., Dijkstra J.R., va Driel M.F. Long-term results of an individualized, multifaceted, and multidisciplinary therapeutic approach to provoked vestibulodynia. J Sex Med. 2011;8:489–496. doi: 10.1111/j.1743-6109.2010.01941.x. [DOI] [PubMed] [Google Scholar]
- 13.Walker L., Beck A.M., Hamptom A.J. A biopsychosocial approach to sexual recovery after prostate cancer treatment: suggestions for oncology nursing practice. Can Oncol Nurs J. 2014;Fall:256–263. [Google Scholar]
- 14.Goldstein I. Sexual medicine reflects the light of knowledge. J Sex Med. 2012;9:2733–2735. doi: 10.1111/j.1743-6109.2012.02991.x. [DOI] [PubMed] [Google Scholar]
- 15.Hartzell R., Cohen D., Goldstein S. Perceived patient benefits when sexual health assessment is performed at a single site using a multidisciplinary approach: integrating sex therapy, physical therapy, and sexual medicine. J Sex Med. 2014;11:230. [Google Scholar]
- 16.Stanowski A.C., Simpson K., White A. Pay for performance: are hospitals becoming more efficient in improving their patient experience? J Health Manag. 2015;60:268–285. [PubMed] [Google Scholar]