Abstract
It is estimated that 15% of traffic accidents cause trauma to large vessels. In about 70%–95% of cases, aortic rupture took place in the distal ligament of the left subclavian artery, whereas in the remaining cases rupture occurred in the ascending aorta above the aortic valve. Trauma to the aortic sinus and coronary arteries is rarely found in traffic accident victims. Therefore, coronary artery trauma is often misdiagnosed as coronary atherosclerotic heart disease. The present case is a 42 years old male who survived from a traffic accident. He presented with aortic sinus and left coronary artery trauma. He was misdiagnosed as having coronary atherosclerotic heart disease, and therefore wrongly given antiplatelet medicine, such as aspirin, in another hospital. Definite diagnosis was achieved in our hospital, and the patient underwent Bentall and mitral valve replacement, as well as tricuspid valvuloplasty. The aortic occlusion time during surgery was 47 min, and the total cardiopulmonary bypass time was 63 min. After surgery, transthoracic echocardiography confirmed that all the artificial valves worked sufficiently. The patient felt good and symptoms such as asthma and decreased exercise tolerance disappeared. This case taught us that acute aortic syndrome cannot be ignored when patients present with pectoralgia; antiplatelet medication should not be given before definite diagnosis.
Keywords: Acute aortic syndrome, Chest trauma, Traffic accidents
Introduction
The horizontal deceleration of a traffic accident, combined with the injuries due to vertical deceleration of the fall can cause the aorta to rupture. In about 70%–95% of cases, aortic rupture occurs in the distal ligament of the left subclavian artery, whereas in the remaining patients rupture occurs in the ascending aorta above the aortic valve.1 In patients involved in a traffic accident, trauma to the aortic sinus and coronary artery is rarely seen. Therefore, in these patients, coronary artery trauma is often misdiagnosed as coronary atherosclerotic heart disease. In this case, we focus on a male patient (age 42 years) who survived in a traffic accident that took place in Zhengzhou, China, resulting in aortic sinus and left coronary artery trauma. However, this patient was misdiagnosed as having coronary atherosclerotic heart disease in another hospital.
Aortic trauma always occurs in the arterial ligament. Acute aortic syndrome (AAS) may involve aortic dilatation, intramural aortic hematoma, penetrating atherosclerotic ulcer, aortic dissection, or aortic rupture2, 3 and requires immediate surgical correction. If untreated, the 24 h mortality rate in AAS patients is 30%.4 The diagnostic methods for thoracic aortic trauma include computed tomography (CT), magnetic resonance imaging (MRI), and transesophageal echocardiography (TEE). These diagnostic approaches have a 95% sensitivity and specificity, and the TEE method can immediately be used in patients that are unstable.2 However, due to the increase in heart rate, in patients with aortic sinus and coronary artery trauma, the CT method does not accurately diagnose type of aortic trauma. In addition, because of the extended examination time, MRI is not suitable for unstable patients. However, the TEE method is more suitable for AAS patients, although this approach is not well tolerated in several patients. Thus, it is a challenge for physicians to diagnose and treat AAS patients, especially patients with aortic trauma.
Case report
The patient was a male (42 years of age) from local province, height 175 cm, weight 120 kg, with no history of smoking, and was healthy prior to the accident. The patient was hit by a bus when he was crossing the road on August 14, 2016. His left anterior chest was impacted by the front of the bus and he fell down, about 10 m away from the site, hitting the road with his back first.
The patient was sent to the local hospital, and chest CT examination showed a fractured sternum and left clavicle. The patient showed stable vital signs, and no signs of chest distress were observed. Therefore, the patient was treated by internal fixation of the clavicular fracture, and a rib claw plate was placed to stabilize the sternal fracture. After surgery, the patient was transferred to the intensive care unit and rested for 30 days, and thereafter transferred to a general ward. When the patient was allowed for out of bed activities, symptoms such as asthma and decreased exercise tolerance were complained. Therefore, the patient was transferred to the Internal Medicine-Cardiovascular Department. After being admitted to the Department of Cardiology, the patient's troponin level, a marker of myocardial injury, was 0.4 mg/L. Clinical tests indicated clinical symptoms of acute heart failure and angina, but traumatic heart vascular injury was not considered after one month after injury. The patient was diagnosed with ischemic cardiomyopathy primarily and was highly suspected of acute myocardial infarction. Therefore, the patient was given antiplatelet drugs, including aspirin, for treatment.
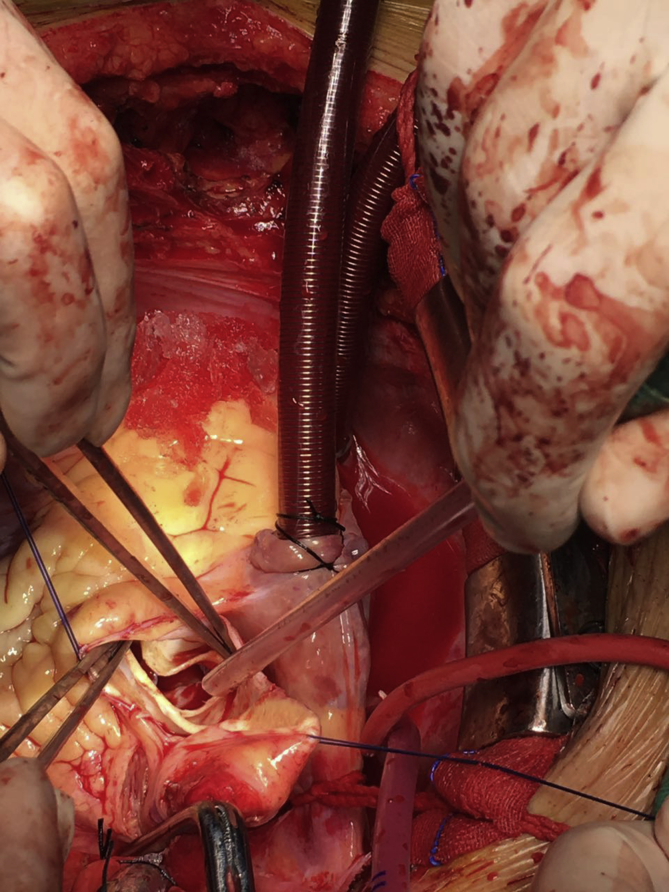
A coronary angiography (CAG) procedure showed that the left main coronary artery was blocked. To correct this defect, the patient was admitted to our hospital for treatment. Because the patient did not present with risk factors of coronary arteries arteriosclerosis such as hypertension or diabetes, physicians considered the diagnosis of trauma-associated aortic lesions involving coronary artery.5 Aortic CTA and TEE were performed, however CTA analysis did not identify aortic dissection. The patient did not tolerate TEE, however, transthoracic echocardiography demonstrated a floating intima in the aorta, severe aortic insufficiency, severe incompetence of the mitral valve, severe tricuspid regurgitation, and severe pulmonary hypertension (Fig. 1). Therefore, antiplatelet medication was immediately terminated and 3 days later the patient underwent exploratory thoracotomy. During surgery, aortic sinus circumferential transection and blockage of the left main coronary artery were observed, and the patient underwent Bentall and mitral valve replacement, as well as three tricuspid valvuloplasty (Fig. 2). The aortic occlusion time during surgery was 47 min, and the cardiopulmonary bypass time was 63 min. After surgery, transthoracic echocardiography confirmed that all artificial valves worked sufficiently. The patient felt good; symptoms such as asthma and decreased exercise tolerance disappeared.
Fig. 1.
Ultrasound image demonstrating a floating intima in the aorta prior to surgery.
Fig. 2.
Dissection in the aortic sinus during surgery.
Half a year after treatment, the patient recovered well and symptoms such as asthma and chest distress were no longer observed. During CT examination, no abnormalities in the aortaorcoronary artery were observed.
Discussion
In thoracic injuries, mitral valve prolapse and trauma to the aorta may occur, and in many cases (about 25%), these are caused due to motor vehicle fatalities.6 Both CT and TEE methods have a high sensitivity and specificity in thoracic injury.1 Patients with aortic sinus and coronary artery trauma have an increased heart rate which is a challenge for accurately diagnosing aortic trauma by CT analysis. Although severe aortic insufficiency can be identified with TEE, limitations still exist when diagnosing aortic sinus trauma.7
Aortic sinus injuries occur during percutaneous coronary intervention surgery. In 1999, Ishibashi et al8 reported aortic sinus injuries during percutaneous coronary intervention operation. Moreover, in 2007, Vianna et al9 reported that spontaneous aortic dissection was limited to the sinus of Valsalva, and involved the left main coronary artery during catheterization interventions. The incidence rate of this complication was 0%–0.008% for diagnostic catheterization, and 0.15%–0.06% for angioplasty procedures.9 This complication always occurred in the right coronary artery.10
During surgery of our patient, we noticed that instead of only the right aortic sinus, all aortic valve leaflets and sinuses were damaged. This indicated that the patients' aortic dissection could not be caused by coronary angiography. On the other hand, aortic dissection is associated with hypertension (high blood pressure) and other connective tissue disorders. Most individuals (72%–80%) who present with aortic dissection have a previous history of hypertension.11 However, our patient did not have any prior history of hypertension, autoimmune disease, or smoking. Moreover, prior to the traffic accident, our patient tolerated heavy physical labor.
We highly suspected that our patient suffered from coronary artery trauma instead of coronary atherosclerotic heart disease. During surgery, we identified aortic sinus circumferential transection and blockage of the left main coronary artery. Aortic sinus lesion often causes coronary injury. Ischemic cardiomyopathy caused by coronary injury following trauma is rare while coronary arteries arteriosclerosis heart disease is more common, and can be easily misdiagnosed as coronary disease.
To treat coronary arteries arteriosclerosis heart disease, coronary artery bypass grafting can be performed under cardiac arrest or in a heart beating state. Because coronary arteries are located on the surface of the heart, the heart will not be opened during surgery to examine the internal structure of the heart. However, during traumatic aortic disease, the site of injury is in the ascending aorta, therefore, surgery must be performed under extracorporeal circulation and the heart must be opened to examine the internal structure. If aortic lesions are only present in the ascending aorta and aortic valve, Bentall surgery may be considered for treatment. In this case, artificial blood vessels are placed and damaged aortic valves and coronary arteries repaired. Coronary artery bypass grafting for coronary disease as well as Bentall operations for aortic lesions are very different in nature, therefore, the clinical diagnosis of patients is of utmost importance.
Aortic sinus injuries are associated with acute aortic syndrome, such as Stanford type A aortic dissection.12 These patients present with symptoms such as a tearing pain in the anterior thoracic. However, several AAS patients who presented with typical symptoms of coronary heart disease were not diagnosed until CAG was performed. AAS patients were given antiplatelet medication, such as aspirin, however this type of medication is fatal to these patients.13 In recent years, physicians have realized that an increasing number of AAS patients are at a higher risk of diagnosis and treatment than others. In general, AAS should be considered when patients present with pectoralgia. Since TEE can identify changes in cardiac structure and function, it is a very useful tool in patients with AAS.14, 15 Moreover, patients should never be recommended to take antiplatelet medication before the diagnosis is final.
In conclusions, AAS should be considered when patients present with pectoralgia, and patients should never be given antiplatelet medication before definite diagnosis.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Atanasijevic T.C., Popovic V.M., Nikolic S.D. Characteristics of chest injury in falls from heights. Leg Med (Tokyo) 2009;11(suppl 1):S315–S317. doi: 10.1016/j.legalmed.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein S.A., Evangelista A., Abbara S. Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2015;28(2):119–182. doi: 10.1016/j.echo.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 3.Meredith E.L., Masani N.D. Echocardiography in the emergency assessment of acute aortic syndromes. Eur J Echocardiogr. 2009;10(1):i31–i39. doi: 10.1093/ejechocard/jen251. [DOI] [PubMed] [Google Scholar]
- 4.Vignon P., Guéret P., Vedrinne J.M. Role of transesophageal echocardiography in the diagnosis and management of traumatic aortic disruption. Circulation. 1995;92(10):2959–2968. doi: 10.1161/01.cir.92.10.2959. [DOI] [PubMed] [Google Scholar]
- 5.Erbel R., Aboyans V., Boileau C. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the European Society of Cardiology (ESC) Eur Heart J. 2014;35(41):2873–2926. doi: 10.1093/eurheartj/ehu281. [DOI] [PubMed] [Google Scholar]
- 6.Williams J.S., Graff J.A., Uku J.M. Aortic injury in vehicular trauma. Ann Thorac Surg. 1994;57(3):726–730. doi: 10.1016/0003-4975(94)90576-2. [DOI] [PubMed] [Google Scholar]
- 7.Nabati M., Bagheri B., Eslami S. Spontaneous aortic dissection limited to the sinus of valsalva: report of two cases. J Tehran Heart Cent. 2016;11(1):34–37. PMCID: PMC4939254. [PMC free article] [PubMed] [Google Scholar]
- 8.Ishibashi Y., Myojin K., Ishii K. Chronic dissecting aneurysm of the sinus of valsalva: report of a case. Kyobu Geka. 1999;52(12):988–992. PMID:10554482. [PubMed] [Google Scholar]
- 9.Vianna C.B., Puig L.B., Vieira M.L. Spontaneous aortic dissection limited to sinus of Valsalva and involving the left main coronary artery. Int J Cardiovasc Imag. 2007;23(4):455–458. doi: 10.1007/s10554-006-9164-x. [DOI] [PubMed] [Google Scholar]
- 10.Li L., Cao Y. Extensive dissection to the coronary sinus of valsalva during percutaneous intervention in right coronary artery-a case report and literature review. Clin Med Insights Cardiol. 2011;5:41–44. doi: 10.4137/CMC.S6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nienaber C.A., Eagle K.A. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation. 2003;108(5):628–635. doi: 10.1161/01.CIR.0000087009.16755.E4. [DOI] [PubMed] [Google Scholar]
- 12.Huang F., Li L., Qin W. Partial aortic root remodeling for root reconstruction in patients with acute type A dissection. J Biomed Res. 2016;30(5):411–418. doi: 10.7555/JBR.30.20150097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu Q.Y., Tai S., Tang L. ST-segment elevation myocardial infarction could be the primary presentation of acute aortic dissection. Am J Emerg Med. 2017;10:1–5. doi: 10.1016/j.ajem.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Patel P.A., Bavaria J.E., Ghadimi K. Aortic regurgitation in acute type-A aortic dissection: a clinical classification for the perioperative echocardiographer in the era of the functional aortic annulus. J Cardiothorac Vasc Anesth. 2018;32(1):586–597. doi: 10.1053/j.jvca.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 15.Cinnella G., Dambrosio M., Brienza N. Transesophageal echocardiography for diagnosis of traumatic aortic injury: an appraisal of the evidence. J Trauma. 2004;57(6):1246–1255. doi: 10.1097/01.ta.0000133576.35999.00. PMID:15625457. [DOI] [PubMed] [Google Scholar]